Abstract
Organophosphorus and carbamate Insectiside is common in Asia–Pacific region consisting of 63% of the Global death. Organophosphorus and Carbamate poisoning can lead into different complications in the respiratory,digestive,neurological aspects and maybe fatal in certain cases.Besides medical management of the same,early rehabilitation is also required to manage different kinds of neurological aspects caused due to Organophosphorus and carbamate poisoning. The study was done to introspect the early intervention in swallowing and speech therapy in organophosphorus and carbamate poisoning individual,as a part of management besides medical intervention. A 19 years old female reported to the hospital with history of consuming organophos and carbamate insecticide with the intention of self harming causing cardiac arrest and as diagnosed as Flaccid Dysarthria with Oro-Pharyngeal Dysphagia when assessed with diagnostic tools respectively. Early speech and swallowing intervention was provided and introspected using MASA which showed improvement in scores during the therapeutic intervention and was statistically analysed using linear regression analysis. The result showed the improvement in MASA scores (the slope of the best fit) and proved that MASA scores improved significantly (slope = 14.3, p < 0.05) over time as the therapy sessions proceeded. The regression model was also significant (p < 0.05). The motor-speech therapeutic intervention provided improvement in the kinematics of oro-motor skills along with improvement in intelligibility of speech. This study concludes that early intervention in managing speech and swallowing abilities in Dysarthria and Dysphagia is helpful besides medical intervention in such cases.
Keywords: MASA, Speech and swallowing therapy, Organophosphorus poisoning, Dysphagia, Dysarthria
Background
Organophosphorus and Carbamate are toxic insectisides used in agricultural practise to control the pests and mammals by inactiviting the enzyme acetylcholinesterase (AchE),that results in accumulation of Acetylcholine(AChE) at the autonomic and central synapses of the nervous system causing neuromuscular blockages effecting humans in both prolonged and transient durations [1].Organophosphorus and Carbamate are toxins that are used medically to reverse neuromuscular blockages and also in the treatment of Alzheimers disease(tacrine and donepezil), glaucoma (echothiopate), myasthenia gravis (pyridostigmine) [2].When considering the principles of poisoning,mostly the poisoning are dose related,which is again dependent on the concentration over time.Poisoning is usually caused due to direct consumption of toxins and also from prolonged exposure to the toxins,inhalation and injections from the same [3].The symptoms of toxin consumption can occur soon after consumtion of the same or might be delayed because the parenttoxin is less toxic than the metabolite.Organophosphorus(OP) and Carbamate can be absorbed through the mucosas of the gastrointestinal tract,lungs and skins and thus inhibiting plasma and RBCs resulting in inhibition of the acetylcholine causing muscarine cholinergic symtoms(bradycardia,myosis,bronchorrhea,salivation,lacrimation) and nicotinic cholinergic symptoms (tachykardia,sweating,abdominal pain). The intermediate syndrome is a recurrence of cholinergic symptoms that appears to have resolved after using OP pesticides. This occurs between 24 and 96 h after OP exposure and is frequently linked to the development of respiratory failure. It entails the onset of muscle paralysis, primarily affecting upper-limb muscles, neck flexors, and cranial nerves [4].
Because of their biochemical mode of action, anticholinesterase drugs can cause signs and symptoms of acute poisoning that are directly correlated with AChE activity levels General acute signs of peripheral nicotinic and muscarinic intoxication are readily noticeable in Human Intoxication Cases(World Health Organisation,1986).Miosis(inability to react to light) is one of the primary symptoms.Other symtoms includes sweating,rhinorrhea,lacrimation and salivation, abdominal cramps and other gastroinstestinal symptoms;coughing and respiratory difficulties;dyspnea,wheezing and constriction in the chest;twitching of the tongue and facial muscles;tremors and fasiculations;pallor and changes in EEG;cyanosis;anorexia;nausea,vomitting,diarrhoea and involuntary urination and defecation [5]. Central effects include headache, fatigue, paresthesia, ataxia, tremulousness, dizziness, and disorientation accompany these signs and symptoms.Eventually, a coma, respiratory failure, twitching, seizures, and convulsions may happen.If the patient lives past the day of poisoning, there will be psychotic episodes, aggressive incidents, mood swings, and personality changes [6].
According to a WHO study,self harm is depicted as one of the major problem in Asia Pasific region which accounts 63% of the global death [7].Organophosphorus and carabamate agent exposure is caused in 3,000,000 individuals with upto 300,000 fatalities [2].
This study was done to introspect the early intervention in swallowing and speech therapy in organophosphorus and carbamate poisoning individual,as a part of management besides medical intervention.
Case Presentation
A 19 years old female reported to the hospital with history of consuming organophosphorus and carbamate insecticide with the intention of self harming. This caused cardiac arrest and in unconscious state and thus intubation, ventilation and central –venous catheterisation was performed. Active management for the same was imposed on the patient and was shifted to ICU where the routine tests showed raised Total Count (TC) and hypertnatraemia. The metabolite value of Serum Lactate showed value of 9.5 mmol/L which was above the reference range and serum Sodium as 152 mmol/L and Serum Potassium was 3.3 mmol/L; which was not within the referenced range.
NECT Head revealed absence of any abnormality in brain parenchyma and USG of whole abdomen showed grossly normal study.In Liver Function test, SGOT and SGPT result showed 51 U/L which was above the normal range. In the Renal Function Test(RFT),serum urea showed an increased range of 32 mg/dL and Serum Sodium was 152 mmol/L.In haematology the WBC count was 26,700 cu mm and ESR was 32 mm/hr which was significantly higher. Patient was kept in ICU for a fortnight and was shifted to general ward when the patient was stable.
The psychiatric evaluation reported of Hypnagogic Hallucinations, which might have resulted due to altered sensorium in the patient disturbed sleep but with stable response and was prescribed clonazepam for relieving anxiety. The poisoning resulted, in experiencing of Hypnagogic Hallucinations.
Physiotherapy management included was bronchial hygiene and as the cough reflex was poor in the patient; so lung expansion therapy, spirometry, range of motion exercises was included in the management plan. She was presented to the Otolaryngologist and Speech Language Pathologist with complaints of slurring of speech and swallowing difficulty (unable to swallow semi-solids and solid food).
The patient was evaluated for speech with N-DAT (Newcastle’s Dysarthria Assessment)and was diagnosed with Flaccid Dysarthria as the persistent clinical symptoms for the same was monopitch, monoloudness, mild hypernasality, slow rate of speech with abnormal MPD (Maximum Phonation Duration), S/Z ratio and abnormal pitch glide and slow and irregular DDK (diadochokinetic) rates w.r.t. AMR(Alternate Motion Rate) and SMR(Slow Motion Rate) and poor breathing patterns. Tongue function test revealed the Level 3 with presence of fasciculations of the tongue. The kinematics of the tongue, lip, jaw and soft palate was affected mildly when assessed with Frenchay’s Dysarthria Assessment(FDA) at motion and during speech.
The patient could not be evaluated for linguistic skills as she was unwilling to talk or answer to spontaneous questions and was having poor attention. But after few sessions of Interaction the linguistic skills were found to be intact and clinically normal.
The swallowing assessment was done using MASA (Mann Assessment of Swallowing Ability) and pre therapy score suggested was 150, suggestive of Moderate Oro-Pharyngeal Dysphagia with prolonged Oral Transit Time, inadequate hyolaryngeal movement and impaired bolus capture with spilling of bolus and inadequate volunteer oral movements with poor cough reflex. The patient was diagnosed with Oro-Pharyngeal Dysphagia as the chief complaints of the patient was difficulty in initiation of swallowing along with nasopharyngeal regurgitation.
Result
The intervention was initiated after the patient was shifted from ICU to the general ward after a fortnight and was able to comprehend simple step commands and was responding with gestures.The intervention in case of swallowing was initiated in three perspectives that is rehabilitation that involved swallowing exercises and maneuvers and compensatory strategies that is modification of the diet(according to Nation Dysphagia Diet) Posture correction and prevention from dysphasia, for at risk populations, which involves further deterioration in swallowing mechanism like food and liquid restrictions (intake of semi-liquid,liquids and semi-solid food) in supine position was also implemented.
The initial MASA score suggested Moderate Oro-Pharyngeal Dysphagia and was fed using Ryle’s Tube and was provided with oral feeds. Then gradually with the initiation of speech and swallowing therapy the prognosis was observed with the help of interventional strategies used in dysphagia therapy and the speech therapy.In speech therapy, the primary goal was to improve the lingual,labial kinematics and strengthening the same at rest or at motion and during production of speech. SOVT (Semi-occluded Vocal Tract exercises) was also incorporated during the therapy sessions to improve the monopitch and monoloudness and to relax the vocal fold musculature. Vocal warm up exercises such as humming and yawn sigh were also included. The voice therapy was also included in the interventional starategies to improve the quality and reduce the hypernasality of the voice.
The patient showed a drastic change in swallowing within 5 sessions of therapy. The MASA scores and N-DAT result (pre and post swallowing therapy) with diet modifications are given below (Table 1).
Table 1.
Overall Summary of MASA scores, Diet Modifications and Therapeutic Techniques used for Dysphagia Intervention, dysphagia modifiet diet and Oro-motor exercises in the 1st, 2nd, 3rd, 4th and 5th day of therapeutic intervention provided
| Days | Diet modifications | Masa scores/N-Dat results | Swallowing therapy strategies | Speech therapy strategies |
|---|---|---|---|---|
| Day 1 |
L1-dysphagia pureed(during therapy) General feeding procedure(post therapy)-RT (Ryles’s Tube) |
MASA score-150 N-DAT-monopitch,monoloudness, Mild hypernasality,poor lip closure TFT-Level 3 |
Chin tug,Mutipleswallows,Head Lift Mandelson maneuver,head and body positioning |
-Tongue protrusion and extension in anti clockwise and clockwise direction in buccal cavity,protrusion and extension of lips using phonation -SOVT,Breathing exercises |
| Day 2 |
L2- Dysphagia mechanically altered (during therapy) General feeding procedure-RT and L1(post therapy) |
MASA Score-155 N-DAT monopitch,monoloudness, Mild hypernasality,poor lip closure TFT-Level 3 Tongue fasciculation seen |
Chin tug,Mutipleswallows,Head Lift Mandelson maneuver,head and body positioning |
-Tongue protrusion and extension in left and right w.r.t opposite forces -SOVT,breathing exercises |
| Day 3 |
L3-Dysphagia Advanced(during therapy) General feeding procedure- RT with L2(post therapy) |
MASA Score-187 N-DAT: Improved resonance,loudness and pitch improved,improved lip closure,TFT-Level 4 Tongue fasiculations improved |
Chin tug,Mutipleswallows,Head Lift Mandelson maneuver,head and body positioning |
-Tongue protrusion and extension in left and right w.r.t opposite forces -Tongue protrusion and extension in anti clockwise and clockwise direction in buccal cavity,protrusion and extension of lips using phonation -SOVT,breathing exercises |
| Day 4 |
L3- Dysphagia Advanced(during Therapy) General Feeding Procedure- RT with L3(post therapy) |
MASA Score:198 N-DAT: no hypernasality, loudness and pitch improved, improved lip closure,TFT-Level 4, tongue fasiculationsimproved |
Chin tug, Mutipleswallows, Head Lift Mandelson maneuver, head and body positioning |
-Tongue protrusion and extension in anti clockwise and clockwise direction in buccal cavity, protrusion and extension of lips using phonation -Tongue protrusion and extension in left and right w.r.t opposite forces -SOVT,breathing exercises |
| Day 5 | L4 –Regular RT removed post therapy |
MASA Score:200 N-DAT: no hypernasality,loudness and pitch improved,improved lip closure,TFT-Level 4 Absence of tongue fasiculations |
RT Removed | Advised to continue oro-motor exercises, voice parameters like Pitch and loudness improved |
From the table, MASA scores improved over time duration, the same is visually depicted in the following figure (Fig. 1).
Fig. 1.
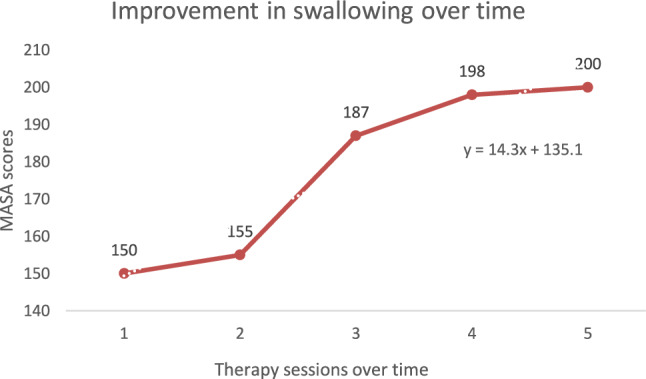
Improvement of MASA scores w.r.t number of days of swallowing therapy provided. When MASA scores were obtained from the patient on the 1st, 2nd, 3rd, 4th and 5th day of therapeutic intervention,it was seen that the scores gradually improved from 150, i.e. moderate dysphagia to 200 i.e.no dysphagia
This improvement was statistically explored using regression analysis to check if the improvement was significant over the number of therapy sessions. The pre-requisites of performing a regression analysis are that the variables should be continuous and normally distributed. Although the MASA scores are discrete data, true ability to swallow falls through a continuum and can therefore be used in a regression analysis (Donald and Morrison, 1972). The MASA scores were explored to obtain information on the distribution pattern. The MASA scores were found to be normally distributed (Shapiro–Wilk test statistic = 0.835, p > 0.05). The linear regression analysis, done to check if the improvement in MASA scores (the slope of the best fit) was significant or not, proved that MASA scores improved significantly (slope = 14.3, p < 0.05) over time as the therapy sessions were imparted. The regression model was significant (p < 0.05) (Tables A–C) (Table 2).
Table 2.
As the therapy sessions progressed, MASA scores considerably improved (slope = 14.3, p < 0.05), according to the results of the linear regression analysis, which was performed to determine whether the improvement in MASA scores (the slope of the best fit) was significant or not
| A. Model summaryb | ||||
|---|---|---|---|---|
| Model | R | R square | Adjusted R square | Std. error of the estimate |
| 1 | 0.947a | 0.898 | 0.864 | 8.81476 |
| B. Anovab | ||||||
|---|---|---|---|---|---|---|
| Model | Sum of squares | df | Mean square | F | Sig | |
| 1 | Regression | 2044.900 | 1 | 2044.900 | 26.318 | 0.014a |
| Residual | 233.100 | 3 | 77.700 | |||
| Total | 2278.000 | 4 | ||||
| C. Coefficientsb | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | Unstandardized coefficients | Standardized coefficients | 95.0% Confidence interval for B | |||||
| B | Std. error | Beta | t | Sig. | Lower bound | Upper bound | ||
| 1 | (Constant) | 135.100 | 9.245 | 14.613 | 0.001 | 105.678 | 164.522 | |
| Therapy sessions over time | 14.300 | 2.787 | 0.947 | 5.130 | 0.014 | 5.429 | 23.171 | |
Discussion
The different kinds of oro-pharyngeal weakness and difficulties can be observed in oro-pharyngeal dysphagia. This includes decrease in crio-pharyngeal dysfunction, reduction in cricopharyngeal opening,prolong hyolaryngeal excursion and effortful swallows resulting in difficulty in swallowing, prolonged oral –transit time, nasopharyngeal regurgitation and residues of bolus remaining in the oral cavity. The inclusion of Swallowing exercises in the Dysphagia Interventional Strategy, such as chin tuck (head flexion and neck flexion) helps in changing the pharyngeal dimensions in directing the bolus smoothly with the help of gravity into the pharynx and the oesophagus so that the bolus residue cannot be stuck in the valeculae and thereby, strengthening the initiation of swallow reflex [8].The mandelson maneuver helps in activation of suprahyoid muscles. Further with effortful swallow, mandelson maneuver helps in the activation of the hyoid bone thereby expanding the dynamics of strengthening the suprahyoid and the pulling of hyoid bone in anterior–superior direction resulting in the protection of the airway and effortlessly leading the bolus by enlarging the passage of the esophagus [9].Head and body positioning can help in changing the dimensions of cervical range of motion. The Head Lift exercise helps in the improved anterior movement of the hyoid bone, opening of the UES (Upper Esophageal Sphincter) and thyrohyoid shortening [10].
Oro-motor exercises mostly involves in improving the kinematics of the oral articulators such as tongue and lips. It mainly focuses on improving the biomechanics and kinematics of the lips like maintaining lip closure, maintaining intraoral pressure, range of motion of lips along with making various lip positions that is used during production of the speech. Additionally, the oro-motor exercises also helps in improving dynamics of the tongue, such as range of motion during speech production,directionality and also to strengthen the tongue for propulsion of the bolus. The kinematics of the tongue can be improved by moving of the tongue in anti-clockwise and clock-wise direction in the buccal cavity. Puckering and lip extension by producing the sounds/oooo/and/eee/, as well as the extension and protrusion of the tongue in accordance with and without resistance from the opposite directions, can all be beneficial in enhancing the dynamics of the tongue movements by positively impacting speech production.
When post-therapy N-DAT and FDA were assessed the kinematics of the tongue, jaw and lips improved both w.r.t. motion and during speech movements. Hypernasality improved with adequate resonatory and phonatory functioning. The suprasegmental aspects of the speech was perceived to be improved with normal rate of speech. The variability in the pitch glide was perceived to be improved following the speech therapy.
As there had been few studies directly pointing the effects of organophosphorus and carbamate poisoning on the humans when consumed and only few literatures show the effect of different toxins effect on humans. There are very few studies which highlights the speech and swallowing symptoms in organophosphorus and carbamate poisoning patients.
Stein et. al (2002) conducted a study on the developmental disabilities on children which reveals that lead, mercury and polychlorinated biphenyl’s(PCBs) poisoning can cause catastrophic developmental effects on the children like mental retardation, CP, impaired sensory-motor functions, decreased verbal ability, decrease processing [11].
Sikka et. al (2006) concluded that organophos can cause reproductive toxicity in human males by interferencing with the androgen hormone leading to low sperm count [12].
Vale et. al (2015) conducted a study to observe the impact of organophosphorus and carbamate insecticide and found that the Ach is blocked in autonomic and central synapses causing symptoms like muscle paralysis affecting upper limbs, neck flexors and cranial nerves from or within 24 to 96 h exposure in humans [13].
Leung et. al (2019) cited that organophos and carbamate can cause mitochondrial poisoning as developmental defects in humans and animal studies also showed exposure to gthe same can cause oxidative stress [14].
Omwenga et. al (2020) conducted a study to examine the level of organophosphorus and carbanomates in Kenya to find the possible health risk and residue of acephate, chlorpyrifos, methamidophos, omethoate and profenofos. These toxic chemicals were found in French beans, kales, spinach and tomatoes respectively. Chlorpyrifos in spinach had an acute Hazard Quotient (HQ) of 3.3 and 2.2 for children and adults, respectively, implying that potential health risks with respect to acute dietary exposure cannot be excluded [15].
There has been report of reduced overall IQ and verbal IQ persisting into middle and late childhood due to prenatal and early exposure to certain chemicals both artificial and naturally occurring toxins, effecting the linguistic developments in children [16].
In the present study, the patient presented with the speech and swallowing symptoms which was diagnosed as Flaccid Dysarthria with Oropharyngeal Dysphagia with the help of diagnostic tools like N-DAT, FDA and MASA respectively. The flaccid dysarthria which is usually caused due to affect in the Lower Motor Neurons,was gradually seemed to improve following therapeutic process through the hierarchy of motor–speech exercises. Oropharyngeal Dysphagia was reported in the present study in which the patient had prolonged Oral Transit Time, inadequate hyolaryngeal movement and impaired bolus capture with spilling of bolus and inadequate volunteer oral movements with poor cough reflex.With extensive Swallowing for 5 days MASA scores improved and RT was removed.This study further highlights the fact that the toxicity mostly affected the Lower Motor Neurons(LMN) and the prevalent dysphasia symptoms was caused due to affect in motor-neuron and musculature involved in swallowing [17].The alpha motor neurons contribute in the final common pathway and any kind of damage can cause variable symptoms of LMN. Spinal interneurons and motor neuron projections from the motor cortex via descending corticospinal fibers have a direct impact on alpha motor neurons. Muscle atrophy, fasiculations, fibrillations and weakness are some of the symptoms that occur due to damage of the alpha motor neurons in LMN. Thus, it can be further inferred that in such cases of organophosphorus and carbamate poisoning,alpha motor neurons can be affected resulting in speech and swallowing disorders. The severity of the symptoms were not profound, otherwise it could have been fatal for the patient. However, as a result of the cardiac arrest, dysphagia and dysarthria were noted as clinical symptoms manifested in this study. A case study reported about “cardiovascular dysphagia” and concluded that as left atrium is situated anatomically in front of the oesophagus. Therefore, mechanical compression due to left atrial enlargement may result in dysphagia, particularly when fluid overload in decompensated heart failure causes dilatation of the left atrium [18]. Another notion could be proposed that, the cardiac arrest would have caused ischemic stroke due to presence of pathological pathway connecting these two disorders [19].Thus, it could have further resulted in lesions in insular, internal capsular, and pontine regions of the brain causing dysarthria and dysphagia [20].
There are studies that concludes that the severity of dysarthria is correlated with dysphagia severity, suggesting that dysarthria is a significant clinical predictor of dysphagia. The prevalence of dysphagia appears lower than it actually is because of compensatory swallowing techniques and dysarthria is easier to detect than dysphagia [21].
The early intervention for speech and swallowing therapy provides fruitful results in managing dysarthria and dysphagia in such cases caused due to poisoning.
The limitation of the study is that to observe other clinical symptoms of dysarthria and dysphagia, large number of samples and different age groups with the effectiveness of early and late therapeutic intervention should be studied in such cases of poisoning. It is also recommended to adopt toxicological reports with various toxicological parameters, concentrations of chemicals and poisons, and effects on various organs, accompanied by the opinions of forensic analysts in such cases of poisoning.
Conclusion
This study was basically carried out to understand the impact of different kinds of speech and swallowing symptoms in a organophosphorus and carbamate poisoning cases and the possible management using speech and swallowing therapy and maneuvers for the same. The implementation of Speech and Swallowing rehabilitation as earlier as possible in a patient with exposure to toxins can help in prognosis besides medical intervention.The linguistic skills might need prolonged duration of language therapy but speech and swallowing therapy has been quite effective in positively improving the swallowing in a patient with toxin consumptions. Further studies should be carried out in large number of samples in understanding the kind of dysphagia and dysarthria persisting in the patients with toxins effect. MASA can be an effective tool in monitoring the prognosis in swallowing in the patient with toxins consumption.
Author Contributions
Koyel Das: Conceptualization, Methodology, Writing Original Draft preparation; Henry Benson Nongrum: Project Administration, Supervision, Writing Original Draft, Resources; Ruchira Mukherjee: Formal Analysis, Validation; Soubhik Bhattacharjee; Resources; Dinesh Bhatia; Writing, Review & Editing.
Funding
None.
Data Availability
Data related to the study can be availed from the corresponding author (Koyel Das) on request.
Declarations
Conflict of interest
None.
Ethical Approval
Not applicable.
Concent to Participate
The subject/participant gave her concent to participate in the study.Concent form is enclosed.
Consent for Publication
The author and co-authors give their consent for publication of the article in the respective journal.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rowe C, Gunier R, Bradman A, Harley KG, Kogut K, Parra K et al (2016) Residential proximity to organophosphate and carbamate pesticide use during pregnancy, poverty during childhood, and cognitive functioning in 10-year-old children. Environ Res 150:128–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Organophosphate and carbamate poisoning [Internet]. [cited 2024 Feb 13]. Available from: https://medilib.ir/uptodate/show/339
- 3.MSD Manual Professional Edition [Internet]. [cited 2024 Feb 13]. General Principles of Poisoning - Injuries; Poisoning. Available from: https://www.msdmanuals.com/en-in/professional/injuries-poisoning/poisoning/general-principles-of-poisoning
- 4.Abdollahi M, Karami-Mohajeri S (2012) A comprehensive review on experimental and clinical findings in intermediate syndrome caused by organophosphate poisoning. Toxicol Appl Pharmacol 258(3):309–314 [DOI] [PubMed] [Google Scholar]
- 5.Jokanović M (2009) Medical treatment of acute poisoning with organophosphorus and carbamate pesticides. Toxicol Lett 190(2):107–115 [DOI] [PubMed] [Google Scholar]
- 6.Eddleston M, Buckley NA, Eyer P, Dawson AH (2008) Management of acute organophosphorus pesticide poisoning. Lancet 371(9612):597–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eddleston M, Phillips MR (2004) Self poisoning with pesticides. BMJ 328(7430):42–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kagaya H, Inamoto Y, Okada S, Saitoh E (2011) Body positions and functional training to reduce aspiration in patients with dysphagia. JMAJ 54(1):35–8 [Google Scholar]
- 9.Kim JH, Kim YA, Lee HJ, Kim KS, Kim ST, Kim TS et al (2017) Effect of the combination of mendelsohn maneuver and effortful swallowing on aspiration in patients with dysphagia after stroke. J Phys Ther Sci 29(11):1967–1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuomi L, Dotevall H, Bergquist H, Petersson K, Andersson M, Finizia C (2022) The effect of the shaker head-lift exercise on swallowing function following treatment for head and neck cancer: results from a randomized, controlled trial with videofluoroscopic evaluation. Head Neck 44(4):862–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stein J, Schettler T, Wallinga D, Valenti M (2002) In harm’s way: toxic threats to child development. J Dev Behav Pediatr JDBP 23(1 Suppl):S13-22 [DOI] [PubMed] [Google Scholar]
- 12.Assessment UENC for E. Reproductive toxicity of organophosphate and carbamate pesticides [Internet]. 2009 [cited 2024 Feb 13]. Available from: https://hero.epa.gov/hero/index.cfm/reference/details/reference_id/7494091
- 13.Vale A, Lotti M (2015) Organophosphorus and carbamate insecticide poisoning. Handb Clin Neurol 131:149–68 [DOI] [PubMed] [Google Scholar]
- 14.Leung MCK, Meyer JN (2019) Mitochondria as a target of organophosphate and carbamate pesticides: revisiting common mechanisms of action with new approach methodologies. Reprod Toxicol Elmsford N 89:83–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omwenga I, Kanja L, Zomer P, Louisse J, Rietjens IMCM, Mol H (2021) Organophosphate and carbamate pesticide residues and accompanying risks in commonly consumed vegetables in Kenya. Food Addit Contam Part B Surveill 14(1):48–58 [DOI] [PubMed] [Google Scholar]
- 16.Dzwilewski KL, Schantz SL (2015) Prenatal chemical exposures and child language development. J Commun Disord 57:41–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waito AA, Valenzano TJ, Peladeau-Pigeon M, Steele CM (2017) Trends in research literature describing dysphagia in motor neuron diseases (MND): a scoping review. Dysphagia 32(6):734–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matta A, Elenizi K, Carrié D, Roncalli J (2020) Dysphagia as an early sign of cardiac decompensation in elderly: case report. Eur Heart J—Case Rep 4(4):1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghanekar S, Corey S, Lippert T, Borlongan CV (2016) Pathological links between stroke and cardiac arrest. Chin Neurosurg J 2(1):40 [Google Scholar]
- 20.Flowers HL, Al Harbi MA, Mikulis D, Silver FL, Rochon E, Streiner D et al (2017) MRI-based neuroanatomical predictors of dysphagia, dysarthria, and aphasia in patients with first acute ischemic stroke. Cerebrovasc Dis Extra 7(1):21–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang BJ, Carter FL, Altman KW (2020) Relationship between dysarthria and oral-oropharyngeal dysphagia: the present evidence. Ear Nose Throat J 12:0145561320951647 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data related to the study can be availed from the corresponding author (Koyel Das) on request.


