Abstract
Since 1952, myringoplasty has evolved with various surgical techniques, including overlay, underlay, sandwich, pegging, rosette, and plugging. Overlay and underlay methods are most commonly used. In 1998, Eavey introduced the cartilage and perichondrium butterfly inlay myringoplasty, designed for small to medium-sized perforation closure, offering practical advantages such as reduced surgical time and improved hearing outcomes. A one-year prospective study (September 2022 to September 2023) in a tertiary care hospital in India involved 30 patients aged 9–52 years with inactive small central perforations. Pre-operative pure tone audiometry (PTA) results were required to be no higher than 35 dB conductive hearing loss. General or local anesthesia was used based on the patient’s age. The surgical technique involved visualizing the perforation, graft preparation, and transcanal insertion. Among the 30 patients, the graft uptake rate was 100% at 3 months and 93.33% at 6 months. Pre-operative mean PTA was 29.76 dB, which decreased to 25.03 dB post-operatively, with a statistically significant air-bone gap closure of 4.73 dB. Cartilage rosette inlay-onlay myringoplasty offers an effective solution for small to medium-sized perforations, achieving high success rates (93.33%). This technique is associated with reduced surgical time, suitability for day care surgery, and minimal scarring, making it a valuable addition to routine clinical practice.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-024-04831-4.
Keywords: Myringoplasty, Cartilage rosette, Endoscopic ear surgery
Introduction
Since 1952, myringoplasty surgery has witnessed the evolution and adoption of various surgical methods [1, 2]. These techniques encompass overlay, underlay, sandwich, pegging, rosette, and plugging approaches, each with its own set of proponents. Among these methods, overlay and underlay techniques stand out as the most widely practiced.
In the year 1998, Eavey introduced an innovative approach to myringoplasty known as the cartilage and perichondrium butterfly inlay myringoplasty, primarily designed for the closure of small to medium-sized perforations [3]. This transcanal endoscopic procedure utilizes a composite graft composed of tragal perichondrium and cartilage, cleverly fashioned in the shape of a rosette to seamlessly fill the perforation, requiring no additional support within the middle ear or external auditory canal.
The technique boasts several practical advantages, including reduced surgical duration, enhanced patient comfort, minimal scarring for improved cosmesis, superior hearing outcomes, and a dry ear post-surgery.
Materials and Methods
This was a 1 year prospective study done in a tertiary care hospital in India from September 2022 to September 2023. 30 patients between the age group of 9–52 years with an inactive small central perforation were included in the study. All ears were dry for atleast 3 weeks before the surgery. Pre-operative pure tone audiometry(PTA) for all the patients should not be more than 35 db CHL(conductive hearing loss). Patients with revision surgery, squamosal disease and sensory neural/mixed hearing loss component on PTA were excluded from the study.
Pure tone audiometry was done preoperatively and postoperatively at 6th month during regular follow-up of patient’s up till 6 months. General anaesthesia was used for children and for rest of patients local anaesthesia (ropivacaine with adrenaline 1:80,000) was used.
Technique
Perforation is visualized under 0 degree 3 mm otoendoscope and margins are freshened with a sickle knife. Squamous epithelium from under and over surface of tympanic membrane is scraped off with circular knife. Dimensions and shape of perforation are measured using right angled pick. Tragal cartilage with perichondrium attached on one side is harvested by a small incision on inner aspect of tragus, taking care that the dome of tragus is maintained and incision site sutured with 4 − 0 non absorbable suture. Graft is cut in same shape as the perforation but 2 mm larger than the size of perforation. Perichondrium is elevated on one side of the cartilage from periphery till the centre circumferentially leaving just a pedicle in the centre. The final shape becomes like a disc of cartilage with perichondrium folded on it like a rose.(Fig. 1).
Fig. 1.
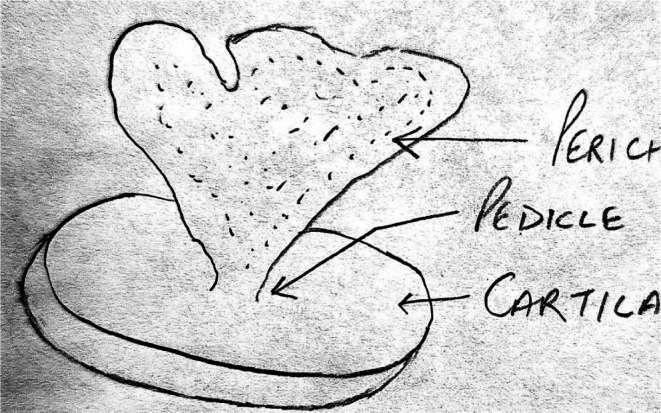
Preparation of a cartilage rosette
The middle ear is filled with medicated gelforam. The graft is then inserted in a transcanal fashion, endoscopically, in such a way that the cartilage rests under the edges of perforation and the perichondrium is reposited over the epithelial edge of the perforation. It becomes a modified inlay overlay type of myringoplasty. The external auditory canal is not packed with gelfoam but left as it is to dry. The patient has immediate hearing improvement and is discharged same day. On follow-up within 7 days the perichondrium swells up and becomes pink. On 3 month follow-up the perichondrium gets necrosed and sloughs off leaving behind an intact neotympanum with cartilage.(Fig. 2).
Fig. 2.

Pre-operative small central perforation in left tympanic membrane and post-operative cartilage graft seen at 1 month
Results
Total patients included in the study were 30. Males were 18 and females were 12. Mean age was 26.33 years. Graft take-up rate on 3 month follow-up was 100% (30/30) and on 6 month follow-up was 93.33% (30/30). Pre-operative mean PTA was 29.76 db CHL. Post-operative mean PTA was 25.03 db CHL. The post-operative air bone gap closure was 4.73 db. Both the graft uptake and post-operative air bone gap closure was statistically significant (p < 0.001). (Table 1)
Table 1.
Tabulated data showing mean hearing gain and graft uptake in the study subjects
| S.No. | Age/Sex | Pre op PTA (db) | Post op PTA (db) | Graft uptake | Hearing gain (db) |
|---|---|---|---|---|---|
| 1 | 15/M | 30 | 25 | + | 5 |
| 2 | 22/F | 25 | 20 | + | 5 |
| 3 | 18/F | 35 | 20 | + | 15 |
| 4 | 16/M | 28 | 23 | + | 5 |
| 5 | 20/F | 30 | 18 | + | 12 |
| 6 | 17/F | 26 | 20 | + | 6 |
| 7 | 19/M | 35 | 18 | + | 17 |
| 8 | 26/F | 30 | 20 | + | 10 |
| 9 | 18/M | 25 | 20 | + | 5 |
| 10 | 13/M | 33 | 19 | + | 14 |
| 11 | 20/M | 35 | 29 | + | 6 |
| 12 | 45/F | 20 | 23 | + | -3 |
| 13 | 35/M | 30 | 35 | + | -5 |
| 14 | 42/M | 25 | 25 | + | 0 |
| 15 | 38/F | 30 | 28 | + | 2 |
| 16 | 40/M | 30 | 28 | + | 2 |
| 17 | 42/M | 35 | 40 | - | -5 |
| 18 | 14/F | 26 | 25 | + | 1 |
| 19 | 52/M | 34 | 25 | + | 9 |
| 20 | 9/M | 28 | 25 | + | 3 |
| 21 | 11/F | 30 | 28 | + | 2 |
| 22 | 27/F | 33 | 28 | + | 5 |
| 23 | 10/M | 25 | 30 | - | -5 |
| 24 | 16/F | 32 | 28 | + | 4 |
| 25 | 32/M | 30 | 25 | + | 5 |
| 26 | 44/M | 32 | 30 | + | 2 |
| 27 | 14/M | 28 | 25 | + | 3 |
| 28 | 32/M | 30 | 20 | + | 10 |
| 29 | 39/F | 28 | 26 | + | 2 |
| 30 | 41/M | 35 | 25 | + | 10 |
| Mean | 26.33 | 29.76 | 25.03 | 93.33 | 4.73 |
Discussion
The pursuit of closing tympanic membrane perforations to enhance auditory function dates back centuries. In the 1640s, Banzer ingeniously employed pig’s bladder membrane to cover an ivory tube, marking one of the earliest attempts at myringoplasty [1]. Subsequent innovations emerged in the late 19th century, with Roosa in 1876 noting the use of cautery to treat perforation rims and Berthold in 1878 introducing myringoplasty involving the utilization of a thick skin graft [2, 3].
Significant advancements in the field continued into the 20th century, exemplified by Wullstein in 1952 and Heerman in 1958, who employed split-thickness skin and temporalis fascia grafts, respectively [4, 5]. In 1964, Goodhill and colleagues introduced the use of tragal perichondrium for myringoplasty, providing the groundwork for cartilage-based techniques [6]. The year 1982 saw the introduction of the plugging technique by Gibb and Chang [7].
Myringoplasty techniques have continued to evolve, embracing contemporary innovations to cater to diverse patient needs. These innovations encompass total endoscopic perichondrium reinforced cartilage myringoplasty, as pioneered by Shakya and Nepal in 2022 [8], ultrathin cartilage-perichondrium complex graft myringoplasty, investigated by Huang et al. in 2021 [9], endoscopic butterfly cartilage myringoplasty, as introduced by Özgür et al. in 2016 [10], and the comparative analysis of endoscopic versus microscopic cartilage myringoplasty, as explored by Daneshi et al. in 2020 [11].
It is essential to assess these diverse techniques and their respective outcomes, as each offers distinctive advantages and considerations. For example, Daneshi et al. reported that endoscopic myringoplasty is a safe and effective method for improving hearing, offering reduced recovery time and post-operative pain, making it a preferable choice for myringoplasty [11].
These modern refinements, including those by Shakya and Nepal [8], Huang et al. [9], Özgür et al. [10], and Daneshi et al. [11], contribute to the ever-evolving landscape of myringoplasty, providing tailored solutions for a variety of clinical scenarios and patient profiles.
In our study, we employed the inlay-onlay tympanoplasty technique, conducting a comprehensive analysis in 30 patients (21 males, 9 females) aged between 9 and 52 years. The selection criteria included patients with small-sized safe perforations in the tympanic membrane, excluding those with sensory neural hearing loss or a history of revision surgery.
The results were promising, with a graft take-up rate of 93.3%, except for 2 failures due to infection. Additionally, 3 cases developed otomycosis 1–2 weeks postoperatively, effectively managed with antifungal ear drops while preserving graft integrity. Hearing improvement was observed in the majority of patients, with 15 experiencing a 1–5 dB improvement, 3 achieving a 6–9 dB enhancement, 6 demonstrating a 10–15 dB gain, and 1 patient showing a remarkable 16–20 dB improvement. However, a subset of 5 patients did not experience hearing improvement.
Our procedure exhibits several notable advantages. It can be swiftly completed in the hands of an experienced surgeon, often within 30 min. The technique lends itself well to day care surgery, reducing patient inconvenience, post-operative discomfort, and morbidity. The use of a cartilage-perichondrium graft, though seemingly rigid, facilitates effective sound conduction and yields highly satisfactory post-operative hearing outcomes. Moreover, the graft displays resilience during the initial phase of nutritional compromise, ultimately forming a stable neotympanic membrane above the cartilage graft.
However, it is important to acknowledge that these innovative techniques may not be suitable for addressing extensive perforations or patients with significant conductive hearing loss. In such cases, the preferred approach would involve tympanoplasty, allowing for comprehensive exploration of the middle ear and ossicles to address specific issues associated with these conditions.
Conclusion
Cartilage rosette inlay-onlay myringoplasty stands out as a straightforward and effective method for mending small to medium-sized perforations, yielding highly satisfactory results and success rates of up to 93%. This approach offers clear benefits, including reduced surgical duration, suitability for day care surgery, and minimal scarring, making it a viable candidate for routine application in everyday clinical practice.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Funding
Not applicable.
Declarations
Ethical Approval
Obtained from institution ethics committee.
Conflict of Interest
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Banzer F (1640s) Early attempts at myringoplasty. Unpublished
- 2.Roosa AD (1876) Cautery for the treatment of perforated tympanic membranes. Arch Otolaryngol 5(3):196–204 [Google Scholar]
- 3.Berthold (1878) Myringoplasty with a thick skin graft. Arch Otolaryngol 7(2):51–54 [Google Scholar]
- 4.Wullstein H (1952) Skin myringoplasty. Arch Otolaryngol 56(2):184–189 [Google Scholar]
- 5.Heerman CE (1958) Temporalis fascia graft for myringoplasty. Arch Otolaryngol 67(3):330–334 [Google Scholar]
- 6.Goodhill V et al (1964) Tragal perichondrium for myringoplasty. Otolaryngol Clin N Am 35(5):927–936 [Google Scholar]
- 7.Gibb AG, Chang SK (1982) The plugging technique in myringoplasty. J Laryngol Otol 96(1):15–18 [Google Scholar]
- 8.Shakya R, Nepal A (2022) Total endoscopic perichondrium reinforced cartilage myringoplasty. Otolaryngol Res Online J 4(1):16–21 [DOI] [PubMed] [Google Scholar]
- 9.Huang Y et al (2021) Ultrathin cartilage-perichondrium complex graft myringoplasty. Ear Surg 13(2):89–94 [DOI] [PubMed] [Google Scholar]
- 10.Özgür A et al (2016) Endoscopic butterfly cartilage myringoplasty. Otolaryngology 5(3):215–221 [Google Scholar]
- 11.Daneshi A et al (2020) Comparative analysis of endoscopic versus microscopic cartilage myringoplasty. *Int J Otolaryng
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


