Abstract
Background:
For almost 60 years, Indian psychiatry literature has called for all medical students to learn psychiatry so that millions of mentally unwell people across India might receive appropriate treatment. Yet for almost 60 years, medical students have disengaged from psychiatry education, resulting in limited learning. The literature has repeatedly cited the solution as one that involves longer exposure on posting and more exam questions, with little impact. This research sought to understand why medical students disengage from psychiatry education so that meaningful change might occur.
Methods:
The research utilized constructivist grounded theory, initially in one medical college in Mumbai, followed by a quantitative survey to test the findings with a wider group of interns across 10 states of India. An iterative process of data gathering and analysis was undertaken using the constant comparison method and theoretical integration.
Results:
Findings identified that 98% of interns believe all MBBS (doctors) should “know” psychiatry, with “know” meaning practical skills—how to assess and treat people with mental illness. The majority of students attend psychiatry to learn those skills, but on finding faculty too overworked to teach, they disengage, saying: “there’s nothing in it for me.” The findings indicate that more exam questions would not increase engagement.
Conclusion:
Medical students want to learn skills to help those in mental distress. Faculty do not have time and, arguably, the training to teach them. To address the nation’s mental health needs, the government needs to prioritize teaching of psychiatry skills by releasing and enabling psychiatry faculty, alongside the certification of psychiatry skills.
Keywords: Education, grounded theory, psychiatry, qualitative
Key Messages
Medical students want to learn psychiatry skills.
Students disengage because skills are not taught.
The government needs to prioritize the teaching of psychiatry skills.
The engagement of medical students in undergraduate psychiatry education has been identified as a major problem in Indian psychiatry literature for almost 60 years, first identified by Neki in 1965, 1 and cited as challenging even in 2023. 2 It is well recognized that the low status of psychiatry in the medical education curriculum is a contributory factor,3-5 with many considering recent changes in the curriculum not to be of sufficient significance to have any real impact.6,7 Meanwhile, the mental health needs of the nation continue to grow, 8 and because many students have not engaged in psychiatry9-13 and subsequently have not learned to address those needs, the lack of effective treatment outside of the psychiatry specialism continues. The literature offers many opinions as to why students do not engage and so do not learn psychiatry, 14 but until now, no one has researched this area and, specifically, has not elicited the student perception. The purpose of this research was to gain this understanding.
In this context of undergraduate psychiatry education, engagement is taken to mean behavioral, cognitive, and affective participation within learning activities.15,16 Behavioral engagement could be interpreted as physical attendance and include practical learning activities such as note-taking or asking questions. However, while attendance is positive, it does not necessarily mean full engagement in learning the subject. For this to occur, cognitive engagement is required, meaning active cognitive processing to enable the absorption and transfer of learning into practice. 17 To consider how students engage with psychiatry affectively or emotionally also seems pertinent, as the subject has the potential for stimulating disturbing emotions, such as fear or anger related to stigma, which could contribute to non-engagement, not the other way around.
Why It Matters: The Prevalence of Mental Illness in India
How medical students engage in or disengage from psychiatry education is highly relevant as it impacts the significant levels of mental disorders across India, disorders that essentially go untreated.18-20 In 2017, the Global Burden of Disease Study 1990–2017 21 estimated that 14.3% of people in India had a diagnosable mental health disorder. In March 2024, India had a population of over 1,438 million people, 22 which with a prevalence of 14.3% equates to over 205 million with such a disorder. Not all of these people receive the psychiatric help they need, thus forming the “treatment gap.” 23 The treatment gap for mental health disorders in India is estimated at 84.5%, 24 which equated in March 2024 to over 173 million people with a diagnosable mental disorder who are not receiving treatment. The impact of such high levels of untreated mental disorder is immense, including premature morbidity, disability, and subsequent socioeconomic losses, in addition to reduced quality of life. 24
Lack of Access to Psychiatry Treatment
For these 173 million people, it is recognized, in part, that the treatment gap relates to a common preference to seek spiritual help over psychiatric treatment,25-27 alongside a reported lack of awareness that mental disorders are “treatable.” 28 Even if treatment is sought, there is a significant lack of psychiatrists, with an estimate of fewer than 0.3 psychiatrists per 100,000 people, contrasting with the USA, which has an estimated 10.5. 29 Poor access to specialist psychiatric services is also a factor, as the majority of psychiatrists are situated in urban areas, while two-thirds of the population lives in rural settings.14,30 Such factors have led to a common acknowledgment that there are not enough psychiatrists in India to fulfill the overwhelming mental health needs of the nation.31-35
Treat Mental Illness in Primary Care
The lack of accessible psychiatric care has long been recognized as challenging, not only in India but also around the world. In 2001, the World Health Organization’s (WHO) World Health Report 36 made recommendations that mental health services are best delivered in primary healthcare by non-psychiatrists to enable faster, easier access to services. In 2012, the WHO addressed this lack of access to mental healthcare more specifically in their World Health Assembly report on the need for a comprehensive, coordinated, well-funded response from health and social sectors at the country level. 37 India was a signatory to this resolution, and the 2014 Indian National Mental Health Policy 38 was in part developed to address this need. However, in actuality the policy has struggled in implementation,39-41 with one reason being that medical officers who did not fully engage in undergraduate psychiatry education10,11,42,43 commonly do not know what to do. 44
Teach the Medical Students
To address the widespread lack of adequate psychiatric care, the leaders within the Indian psychiatry community continue to call for medical students to be trained in how to assess and treat common mental disorders within general healthcare.45-47 However, medical students continue to fail to engage in psychiatry education, with poor attendance rates being commonly reported in the literature,10,12,42,48 resulting in a deficit in learning, which means the treatment gap for mental disorders perpetuates.
Why Do They Not Engage?
The literature tells us the main reasons for the lack of engagement relate to the low significance afforded to psychiatry in the medical curriculum, including the lack of specialty status,38,48-50 the limited time allocation,35,45,51 and no full exam.10,12,44 These factors are repeatedly recorded across the years, 14 and this lack of meaningful change is cited as why the low levels of engagement remain static. However, some believe that the introduction of the Competency-based Medical Education curriculum (CBME) by the National Medical Council (NMC) 52 may have a positive impact on student engagement, bringing more focus on skill acquisition and less on rote learning.7,53 Alternatively, others feel the CBME changes are insufficient to have any real impact on student engagement in psychiatry education,6,7 with the main deficits being: (a) the continuance of subspecialty status;6,45 (b) minimal time allocation despite an increase from 20 hours under the former Medical Council of India (MCI) curriculum to 40 hours under the NMC CBME curriculum;12,35 (c) no change to the small allocation of psychiatry exam questions in the medical exam;7,34 and (d) most significantly, no certification of skills.46,50 With no certification or assessment of skills, the focus for students is expected to remain on rote learning facts, as fundamentally, that is all that is required.
Research Purpose
In light of the ongoing stasis of poor engagement in undergraduate psychiatry education, this research set out to understand the recent retrospective perspectives of medical interns as to why they did or did not engage in undergraduate psychiatry education and what they believe would have made a difference.
Methodology and Methods
Constructivist Grounded Theory
This research was undertaken using grounded theory, a well-established, rigorous, systematic research methodology that generates an explanatory theory as to how and why specific social processes occur—in this case, the disengagement of medical students from psychiatry education in India. The majority of previous research into Indian undergraduate psychiatry education has used quantitative approaches, generally using questionnaires with rating scales, and consequently has not been able to explore the “why” or “why not” questions. To gain the understanding needed, it was important to explore interns’ perspectives and so identify the patterns of behaviors, cognitions, and feelings that inform the engagement or disengagement process, relative to their sociocultural context.54,55 The type of grounded theory considered most appropriate was constructivist grounded theory within the interpretivist paradigm, with an ontological position of relativism, meaning what is known is subjective to individuals and relative to a social and cultural context,56,57 and an epistemology of social constructivism, where different subjective views are co-constructed, thus generating richer understanding without the need for consensus.58,59 A fundamental premise of constructivist grounded theory is the recognition that the researcher is intrinsic to this co-construction process, collaboratively making sense and exploring meaning with participants,54,55 in this case, the interns. Such co-construction of contextual understanding was particularly important in this research as the lead researcher was not from India. However, the researcher, Indian psychiatrist collaborators, and the interns saw this external or “outsider” positioning as advantageous, with the interns specifically naming her ‘non-faculty’ position as a distinct advantage. Thus, the senior psychiatrist’s commission to “get them to tell you—they won’t tell me, I’m faculty” was astute, with interns concurring: “that’s why we told you everything” (Focus Group (FG) 3, 2020). Nevertheless, it must also be acknowledged that the researcher has an intrinsic influence throughout the research process, including in all methodological choices and interpretations, and that being a Western researcher with Western perceptions and values could only be significant. Therefore, the need for reflexivity regarding researcher presuppositions and potential bias was paramount, and a robust reflexive process was upheld throughout. 60 Such reflexivity aligns with the practice of decolonization in intercultural research 61 and is highly congruent with constructivist grounded theory methodology.54,55
Methods
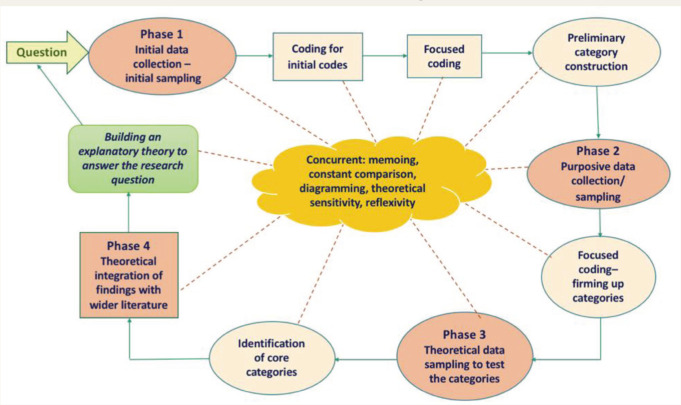
Constructivist grounded theory is an inductive methodology, which claims no hypothesis to be proved or disproved but commences with broad research questions about a little-known social process it seeks to understand. It uses an iterative pattern of data collection, with each set of findings informing what is explored next, as data analysis is consistently integrated between each data collection phase. The iterative pattern of methods used in data collection and analysis in this research can be seen in Figure 1.
Figure 1. The Methods of Data Collection and Analysis.
Phases 1 and 2: Data Collection and Analysis
Phases 1 and 2 data collection occurred over a two-year period (2020–2022) in a government medical college in Mumbai. It involved 10 focus groups with between two and nine interns in each and four interviews, equating to 40 intern participants. The necessary ethical approval was granted by the medical college in Mumbai and by Anglia Ruskin University in the UK. Participants were anonymized throughout.
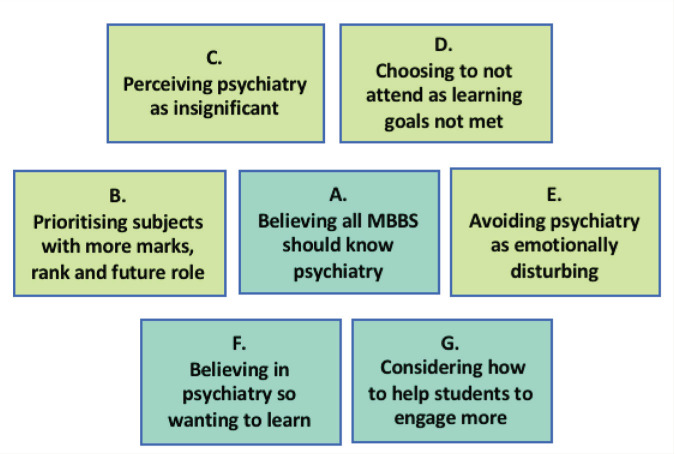
Phase 1 initial data gathering used a loosely structured questioning format, starting from six questions, with frequent clarification and exploration to aid the co-construction process. The interviews and focus groups were recorded and transcribed, with initial coding generating an initial 137 codes, which through the constant comparison method became 34 focused codes. In line with grounded theory methodology, codes were named using “gerunds,” meaning action words, to seat the codes in the behaviors of the students. Through increasing theoretical sensitivity, the focused codes were synthesized into seven categories or themes, aiming to identify the abstract concepts driving the students to engage in psychiatry education or not (Figure 2). The label of each category denotes a synthesis of the meaning of the codes in that category. Each category remains labeled as a gerund, which reflects the conscious or subconscious psychological and/or social processes the students were enacting in response to psychiatry education.
Figure 2. The Seven Categories Synthesized from 34 Focused Codes.
Phase 2 used these categories as a basis for purposive sampling, which means focused data gathering to attain greater depth in the areas of greatest pertinence, purposefully sampling to understand concepts, not for specific people types.
Phase 3: Data Collection and Analysis
Phase 3 used an online questionnaire, which was devised using an abductive approach to test the findings with a broader pool of interns. Such a strategy is in keeping with grounded theory methodology as part of theoretical sampling,54,57,62 which aims to attain a greater depth of understanding from a wider pool of participants, as related to the categories and concepts constructed from previous data collection. In this research, the questionnaire was used to test if the findings from Phase 1 and Phase 2 were resonant in more than one medical college. The questionnaire was, therefore, not previously validated, as all questions and options for answers arose from the categories as constructed from Phases 1 and 2 (Figure 2) and, as such, were specific to this research.
The questionnaire was circulated through the snowballing technique,63,64 where contacts and respondents were asked to forward the survey, including via Twitter. There were 51 respondents to the questionnaire, and it reached 10 states of India. In total, the research consulted with 91 interns.
Through a continuing process of constant comparison between the three phases of data and the interpretive process of memoing and diagramming, the 34 focused codes and seven categories synthesized into two clear core categories based on Categories A and C—(a) “Psychiatry is important” and (b) “yet simultaneously insignificant.” These two core categories hold a contradiction or a duality about the underlying perceptions of psychiatry as essential for all MBBS (qualified medical doctors) but at the same time, not. Through analysis of the findings, a clear pattern of how medical students engage, do not engage, or start to engage then disengage started to become clear, alongside a partial, subjective understanding as to why this might be, particularly in relation to the wider socio-cultural context, commonly not previously considered.
Phase 4: Theoretical Integration
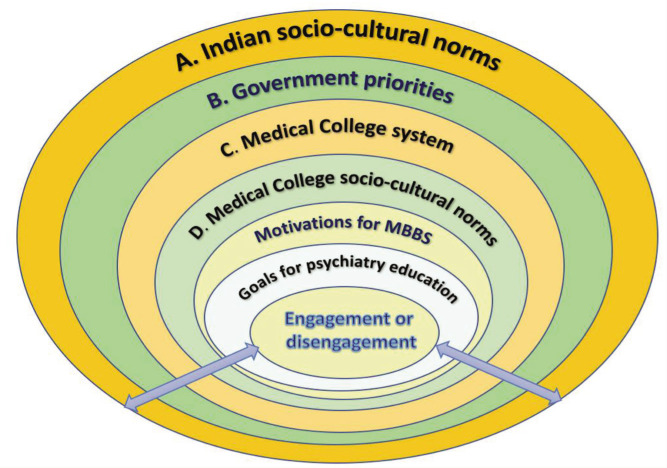
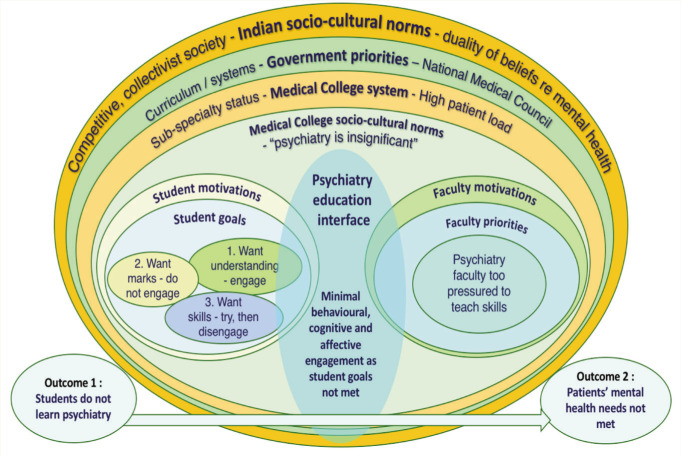
Theoretical integration aids the understanding as to why behaviors or processes occur and involves seating the research findings into the broader context of the literature and related existing theories. This is essential in order to be able to construct a substantive explanatory grounded theory to address the research purpose. To aid the analytic process, we used the conditional/consequential matrix (Figure 3), a grounded theory analytic tool created by Corbin and Strauss 65 that visually represents the micro- and macro conditions that influence or impact the core phenomenon.54,65 As part of the integrative analytic process, we used the matrix to map the wider socio-cultural conditions that influence medical students, analyzing how the micro- and macro-factors work in combination to seemingly maintain the common lack of engagement. This was how an understanding of the “why” or “why not” elements of the research question was developed.
Figure 3. Conditional/Consequential Matrix, Showing the Influences upon Engagement in Undergraduate Psychiatry Education.
Results
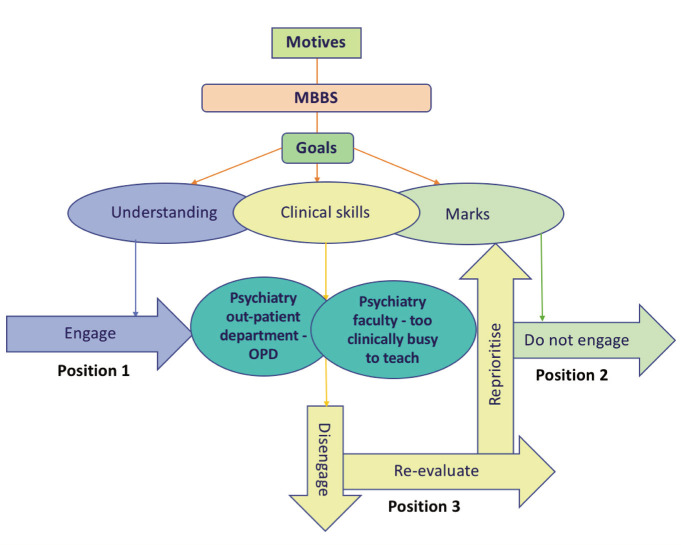
Through the iterative process of data gathering and analysis, the findings show that medical students adopt one of three positions regarding psychiatry education, positions that relate to their overall motivations to study for MBBS, which in turn inform their goals to engage in psychiatry (Figure 4).
Figure 4. The Three Positions Medical Students Adopt in Regard to Psychiatry Education.
Position 1—engage. Students in Position 1 are motivated to want to understand and help patients in mental distress and therefore want to engage in psychiatry education; many in this group want to be psychiatrists, but their numbers are few.
Position 2—do not engage. Students in Position 2 are primarily motivated toward achieving a good degree through gaining high marks in exams and so a high ranking in both undergraduate finals and postgraduate entrance exams. They want a good job with high pay, low stress, and a positive work–life balance. These students do not engage in psychiatry as it generates minimal marks in exams so is unable to meet their primary goal of securing a high rank.
Position 3—engage then disengage. Students in Position 3 want to learn skills to help people in mental distress, including assessment and communication skills, so that, at a minimum, they can identify mental disorders, communicate empathetically, and refer to psychiatry specialists as needed. These students know psychiatry is unable to offer them marks, yet they still initially attend, describing a goal of attaining applied knowledge/skills. They believe teaching “should be practical, to differentiate … theory is not enough” (FG 6, 2020), but their experience on posting is that “they don’t teach us because they don’t have enough time” (FG 4, 2020). They acknowledge the pressures on psychiatry faculty due to the high patient workload, resulting in a lack of priority for students and a leniency toward non-attendance, seen in the willingness to “sign us off anyway” (FG3, 2022). Such leniency has commonly become embodied in college culture, and a lack of engagement has become almost expected. This highlights the reciprocal nature of engagement, meaning when people try to engage, they need something or someone to engage with. If the “someone to engage with,” as in faculty, is not able to do so, engagement between the two sides is impossible. For some in Position 3, this meant they stopped attending altogether, prioritizing their time on more productive subjects; for others, they still attended in body, appearing to superficially behaviorally engage, but describe it as “you are physically present, but mentally, you are not” (FG 2, 2022), meaning they no longer process cognitively, disengage affectively, and memorize only as necessary “to pass MCQs” (interview 2, 2020).
Those in Position 3 form the majority of students. They feel that all MBBS should know practical psychiatry skills and they want to learn (Core Category 1—“psychiatry is important”), yet at the same time, they believe that learning such skills is unimportant within their medical training (Core Category 2—“yet simultaneously insignificant”), as indicated by both the curriculum and, inadvertently, through faculty, who have no time to teach due to their heavy clinical and administrative demands. Therefore, when faced with such a contradiction, the students almost all disengage.
The findings of the questionnaire in Phase 3 strongly exemplified this contradiction, with 98% of respondents believing that all MBBS should “know” psychiatry, with “knowing” being equated with practical clinical skills, to: (a) communicate with someone in mental distress; (b) assess mental illness; (c) assess suicide risk, plus (d) hold the basic knowledge of commonly occurring mental disorders. Yet respondents to the questionnaire indicated that 91% of their psychiatry education was not being taught clinical skills, with passive observation, private lectures, and reading books all scoring higher as a means of learning than faculty teaching skills or faculty lectures. Similarly, when asked what they felt would help medical students engage more, the top five responses involved clinical skill-based teaching or assessment, with “practical teaching of psychiatry assessment skills” being cited by 96% of respondents as a positive motivator to engage. More written exam questions was the least-motivating factor for increased engagement (15%), despite this being the most common recommendation for motivating learning in the psychiatry literature for 60 years.13,31,48,51,66 That interns describe being substantially more motivated by learning clinical psychiatry skills than by increasing psychiatry exam questions is very significant, as it impacts the recommendations of how the situation could potentially change.
Discussion
The contradiction in the findings between the two core categories—(a) “Psychiatry is important” and (b) “yet simultaneously insignificant”—demonstrates a duality of belief about mental ill-health and psychiatry that is apparent across the broader Indian socio-cultural context. This contradiction is seen to be highly influential upon student engagement, with the vast majority of students behaviorally acting on the “lack of significance” more than the belief that “psychiatry matters.” How this duality impacts on faculty is also key, being apparent both in the lack of time allocated to teach 45 and in the lack of pedagogically based training received. 67 The latter is a factor identified in research by Kishor et al., 67 where the majority (87%) of the psychiatry faculty believed they lacked in their ability to teach the clinical skills the students were seeking, which has become an element of increasing significance with the implementation of the CBME curriculum.
Within the data, this duality of belief about psychiatry can clearly be identified within individual medical students, among peers, within the culture of the medical college, and reportedly in the influence of families. However, as noted by Kahu, 17 such local layers of influence do not exist in isolation but commonly arise from a broader contextual sphere, such as a society or political system. In this context, the conditional/consequential matrix shown in Figure 3 represents these layers of influence and the socio-cultural contextual spheres in which they operate. At the heart of the matrix is the process of engagement/disengagement with undergraduate psychiatry education. Surrounding this are the individual’s goals about that process, which here means whether a student wants to learn psychiatry or not, and why that might be. The goals for psychiatry education are seated within the individual’s motivations, meaning their drivers toward achieving MBBS and postgraduate career aspirations. These motivations sit within the frame of the medical college and the socio-cultural influences arising from faculty and peers—expectations and patterns of behavior accepted as norms in the medical college environment. The medical college system underpins many of these expectations, with the weightage of the curriculum influencing where both students and faculty must align their priorities, including the need to address patient demands in a busy hospital environment. The curriculum itself is dictated nationally by the NMC, which sets the content and ascribes weightage to each subject in terms of time, exams, and marks and so the perceived significance and priority of each subject. The decisions of the NMC sit alongside governmental priorities for mental health and psychiatry services, including financial provision and service implementation. The government and its priorities are themselves influenced by the socio-cultural norms and values of a collectivist and competitive Indian society, which are underpinned by a longstanding duality of beliefs about the causes and nature of mental distress and what help is appropriate, thereby inadvertently challenging the applicability of psychiatry as a Western, bio-medical method of addressing potentially non-biological mental health needs. 68
The student engagement process cannot be fully understood without also considering how the individual is seated in this broader socio-cultural context, with such influences informing where their goals and motivations arise and the system that can or cannot meet them, why they occur as they do, and therefore, where change might be possible. When considering the process of student disengagement in Indian psychiatry education, it is important to understand these influences from the students’ perspective—why their learning goals are often not met and how that impacts their engagement, behaviorally, cognitively, and affectively.
Engagement Theory
As engagement in undergraduate psychiatry education has not been researched in India previously, no context-specific models of engagement or disengagement could add insight into this process. There were also no models found outside of a Western context, and expectations and practices in the West and non-West cannot be assumed to be the same. However, Kahu and Nelson’s 2018 69 framework of student engagement offers some parallels that merit consideration:
Recognizing the significance of socio-cultural context, including the political and social environment
Engagement being a two-way process that requires a student–faculty interface
Psychosocial elements being influential, particularly motivations and workload
Intended outcomes or goals being influencing factors in the short and longer terms
However, critical factors from the findings of this research that are not congruent with Kahu and Nelson’s 69 framework:
Disengagement—the primary process arising in our research is disengagement, with very limited faculty–student interface.
It cannot be assumed that students want to engage cognitively, behaviorally, and affectively, as other priorities often take precedence.
Faculty workload—the pressure of the patient workload on faculty means that they are not able to fully engage in delivering the extensive curriculum alongside managing the high patient load and administrative duties. Such pressures mean it cannot be assumed that faculty are able to engage.
Mechanisms of interaction—the processes that Kahu and Nelson 69 claim facilitate the two-way interaction of engagement—self-efficacy, emotion, belonging, and well-being—are largely not promoted in non-Western learning environments and could be seen to occur in reverse. For example, self- efficacy—having the capacity to take control of one’s behaviors toward one’s own goals—was not directed toward engagement in psychiatry but instead in the decision to not attend/engage, so the opposite. Similarly, emotions are seen as positive indicators of engagement for Kahu and Nelson, 69 particularly in relation to interest in the subject. In this research, interest was present for the very few who did engage, but the reverse was true for those who did not, with fear and anger being emotions that contributed to decisions not to engage. Belonging was also taken in reverse, with interns saying peer pressure induced non-engagement, as peers and seniors said there were more productive subjects than psychiatry, so there was no need to attend; in this context, therefore, “belonging” meant disengagement. With regard to well-being, for those who were worried about “catching” mental illness or who felt stressed with workload, disengagement was an effective method of promoting well-being, not the other way round.
Sociocultural influence—Kahu and Nelson 69 recognize the influence of socio-cultural context on the engagement process. However, the extent of the contextual influence arguably needs greater weightage, being seen in this research to impact all decisions regarding psychiatry education and whether that education is valid or tenable to engage with.
Thus, while Kahu and Nelson’s 69 model is useful and describes the engagement process in greater range and depth than other models, it also carries assumptions of engagement that are not fully applicable in this context.
The Theory of Disengagement
A theory of disengagement has therefore been generated that draws on Kahu and Nelson’s 69 model of engagement, but reflects the findings of this research as to how and why medical students commonly disengage from psychiatry education, as integrated within the wider sociocultural context of India. Figure 5 shows the Model of Disengagement, which is a diagrammatic illustration of that theory.
Figure 5. The Model of Disengagement: A Diagrammatic Representation of the Theory of Disengagement.
How medical students in India engage in or disengage from psychiatry education is dependent on their personal motivations for undertaking a medical degree, which generate their goals for psychiatry education—illustrated at the center left of the model (Figure 5). These goals lead to the three positions adopted by students in relation to psychiatry: Position 1, wanting to understand and so engaging; Position 2, wanting marks so not engaging; and Position 3, wanting clinical skills to assess and treat people in mental distress, so trying to engage, then disengaging as skills are commonly not taught. Position 3 is the stance adopted by the majority of medical students. Skills are usually not taught as psychiatry faculty are too pressured by a high patient load and an undoable curriculum in the time allocation (center right of the model). They are therefore not able to fully engage in teaching what students want, namely, clinical skills to assess and treat common mental illness. Thus, it can be seen that the “psychiatry education interface” at the heart of the model is empty, as the vast majority of students do not engage in the learning process as the faculty are unable to be present to teach them.
Why the faculty do not have the time to teach psychiatry skills to medical students relates to the wider socio- cultural context in India (the outer layers of the model—Figure 5), where there exists a duality of belief about the nature and potential validity of mental distress and the most appropriate help or treatment it necessitates.26,69 Such dual beliefs about mental illness and, consequently, psychiatry impact upon governmental priorities for mental health services 40 and psychiatry education,6,51 and so the NMC curriculum, the medical college structure and subject weightings, plus attitudes of non-psychiatry faculty, student peers, and family. In psychiatry education, this translates into no allocated time for faculty to teach aside from their responsibilities for patient care; minimal faculty training in the teaching of clinical skills; an unworkable and according to some a largely irrelevant specialist curriculum, 6 which is impossible to deliver in the short time allocation; and no certification for the learning of practical psychiatry skills.50,70 The combination of these factors results in the perpetuation of a message to students that despite what the NMC says, psychiatry is insignificant. Therefore, they put aside their desire to learn skills and disengagement inevitably occurs.
Recommendations
This research provides insights into how and why students engage in or disengage from undergraduate psychiatry education. The inability of faculty to meet students’ goals due to their high clinical and administrative workload and the accompanying message this gives is highly significant and needs to be addressed. This research therefore recommends:
The specific allocation of time for psychiatry faculty to teach clinical skills, aside from clinical responsibilities.
The acceleration of faculty training in pedagogical strategies to teach psychiatry skills, including how such skills can be practically assessed.
The certification of psychiatry skills on the NMC curriculum. (N.B.: While certification would be advantageous in ensuring the teaching of psychiatry skills receives a higher significance/priority in the view of students, peers, psychiatry faculty, and other faculty, it should be noted that the majority of students reportedly take up psychiatry looking to learn skills despite there being no marks, so the lack of certification should not be a reason to default on governmental allocating time for faculty to deliver skill-based teaching.)
Further research on the implementation of skill-based teaching to assess its impact on engagement in psychiatry education across India, including at undergraduate levels, and the subsequent impact on patient care.
Conclusion
This research has explored how and why medical students commonly disengage from undergraduate psychiatry. The findings demonstrate reasons for disengagement that differ from those reported in the literature for 60 years and therefore hold great significance. There is hope, in that the vast majority of undergraduates want to learn skills to help those in mental distress. Responsibility to enable such learning fundamentally rests with the government and its prioritization of the needs of over 123 million people in the treatment gap, both in providing appropriate, accessible services and in educating the next generation of MBBS with the practical psychiatry skills they need. To that end, within each medical college, faculty need to be enabled to deliver the practical, skill-based teaching the students want, not only pedagogically but with time, through the prioritization of workload to include teaching students how to help. When such changes occur, the research findings suggest that many more students will engage in psychiatry education in order to learn how to relieve the mental distress of the nation. And with that learning, the pattern of the last 60 years may begin to change.
Acknowledgments
The authors would like to acknowledge Lok Tilak Municipal Medical College, Mumbai, Professor Subodh Dave, Professor Thirunavukarasu, and Dr. Raja Natarajan for their ongoing support throughout this research.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval was granted by Lok Tilak Municipal Medical College, Mumbai, ref: IEC/88/19, and by Anglia Ruskin University, UK, ref: ESC-SREP-19-034. The subjects provided consent for participation in this study
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Neki JS. Indian psychiatric society honorary secretary‘s report for 1964–65. Indian J Psychiatry, 1966; 8: 70–75. [Google Scholar]
- 2.Patel AD, Pal A, Rahat F, et al. Attitude towards patients with psychiatric illness among undergraduate medical students at government medical college: a cross-sectional study. J Family Med Prim Care, 2023; 12: 756–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lingeswaran A. Psychiatric curriculum and its impact on the attitude of Indian undergraduate medical students and interns. Indian J Psychol Med, 2010; 32: 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poreddi V, Thimmaiah R, and Math SB. Attitudes toward people with mental illness among medical students. J Neurosci Rural Pract, 2015; 6: 349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kishor M and Vinay HR. Innovative ways and customizing psychiatry training for undergraduates. Indian J Psychiatry, 2015; 57: 431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob KS. Medical Council of India’s new competency-based curriculum for medical graduates: a critical appraisal. Indian J Psychol Med, 2019; 41: 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narwane S, Anikhindi A, and Mahavarkar V.. Study of perceptions of competency-based medical education reforms in India. Pravara Med Rev, 2021; 2: 4–13. [Google Scholar]
- 8.Charlson FJ, Baxter AJ, Cheng HG, et al. The burden of mental, neurological, and substance use disorders in China and India: a systematic analysis of community representative epidemiological studies. Lancet, 2016; 388: 376–389. [DOI] [PubMed] [Google Scholar]
- 9.Kulhara P and Avasthi A.. Teaching and training in psychiatry in India: potential benefits of links with the Royal College of Psychiatrists. Int J Psychiatry, 2007; 4: 31–33. [PMC free article] [PubMed] [Google Scholar]
- 10.Gulati P, Das S, and Chavan BS. Impact of psychiatry training on attitude of medical students toward mental illness and psychiatry. Indian J Psychiatry, 2014; 56: 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mutalik NR, Tejaswi TP, Kashinakunti M, et al. Attitude of medical undergraduate and postgraduate students towards psychiatry: a cross-sectional study. Open J Psychiatry Allied Sci, 2018; 9: 3–9. [Google Scholar]
- 12.Mishra KK, Rawekar AT, and Reshamvala AM. Absence of undergraduate medical students from psychiatric training: a study from central India. Ind Psychiatry J, 2021; 3:102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh OP. Closing treatment gap of mental disorders in India: opportunity in new competency-based medical council of India curriculum. Indian J Psychiatry, 2018; 60: 375–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayetti C, Jadhav S, and Deshpande SN. How do psychiatrists in India construct their professional identity? A critical literature review. Indian J Psychiatry, 2017; 59: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trowler V. Student engagement literature review. High Educ Acad, 2010; 11: 1–15. [Google Scholar]
- 16.Groccia JE. What is student engagement? New Dir Teach Learn, 2018; 154: 11–20. [Google Scholar]
- 17.Kahu ER. Framing student engagement in higher education. Stud High Educ, 2013; 38: 758–773. [Google Scholar]
- 18.Reddy IR. Undergraduate psychiatry education: present scenario in India. Indian J Psychiatry, 2007; 49: 157–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thirunavukarasu M. Psychiatry in UG curriculum of medicine: need of the hour. Indian J Psychiatry, 2007; 49: 159–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gulati P, Das S and Chavan BS. Impact of psychiatry training on attitude of medical students toward mental illness and psychiatry. Indian J Psychiatry, 2014; 56: 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sagar R, Dandona R, Gururaj G, et al. The burden of mental disorders across the states of India: the global burden of disease study 1990–2017. Lancet Psychiatry, 2020; 7: 148–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Worldometers. India population. www.worldometers.info/world-population/india-population/#:~:text=The%20current%20population%20of%20India,the%20latest%20United%20Nations%20data (accessed 23 March 2024. ).
- 23.Kohn R, Saxena S, Levav I, et al. The treatment gap in mental health care. Bull World Health Organ, 2004; 82: 858–866. [PMC free article] [PubMed] [Google Scholar]
- 24.Gautham MS, Gururaj G, Varghese M, et al. The national mental health survey of India (2016): prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry, 2020; 66: 361–372. [DOI] [PubMed] [Google Scholar]
- 25.Sax W. Ritual healing and mental health in India. Transcult Psychiatry, 2014; 51: 829–849. [DOI] [PubMed] [Google Scholar]
- 26.Rajan B, Cherupushpam SD, Saleem TK, et al. Role of cultural beliefs and use of faith healing in management of mental disorders: a descriptive survey. Kerala J Psychiatry, 2016; 29: 12–18. [Google Scholar]
- 27.Singh S. ‘I chained him to protect him from the spirits’. What are the challenges for psychiatrists in India? BJPsych Int, 2017; 14: 100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Regional consultation to develop regional strategic framework on social determinants of health actions in South-East Asia (2023–2030): report of a regional consultation, New Delhi, 2–4 August 2022. World Health Organization: regional office for South-East Asia. [Google Scholar]
- 29.World Health Organization. International data indicators: psychiatrists working in the mental health center, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/psychiatrists-working-in-mental-health-sector-(per-100-000) (accessed 15 June 2023. ).
- 30.Kallivayalil RA. The importance of psychiatry in undergraduate medical education in India. Indian J Psychiatry, 2012; 54: 208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thirunavukarasu M. Closing the treatment gap. Indian J Psychiatry 2011; 53: 199–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manohari SM, Pradeep RJ and Galgali RB. How to teach psychiatry to medical undergraduates in India? A model. Indian J Psychol Med, 2013; 35: 23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nayak A. Changing medical students’ attitudes to psychiatry through newer teaching techniques. Mens Sana Monogr, 2015; 13: 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kishor M, Gupta R, Ashok MV, et al. Competency-based medical curriculum: psychiatry, training of faculty, and Indian psychiatric society. Indian J Psychiatry, 2020; 62: 207–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bhasin PD, Gire N, Nautiyal H, et al. Developing an emerging psychiatric workforce in India: the need for robust psychiatric education. Int Soc Study Behav Dev Bulletin 2021; 2:, 2–6. [Google Scholar]
- 36.World Health Organization. World health report 2001. Geneva: World Health Organization, 2001. [Google Scholar]
- 37.World Health Organization. Sixty-fifth world health assembly: the global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level 2012, https://apps.who.int/gb/ebwha/pdf_files/WHA65/A65_R4-en.pdf Last accessed 24/March/24
- 38.Government of India Ministry of Health and Family Welfare. National mental health policy, 2014, https://nhm.gov.in/images/pdf/National_Health_Mental_Policy.pdf Last accessed 24/March/24
- 39.Gupta S, Misra M and Gill N.. Mental health review board under the mental health care act (2017), India: a critique and learning from review boards of other nations. Int J Law Psychiatry, 2022; 81: 101774. [DOI] [PubMed] [Google Scholar]
- 40.Gupta S and Sagar R.. National mental health policy, India (2014): where have we reached? Indian J Psychol Med, 2022; 44: 510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vanagundi R, Pokle S, Walwaikar R, et al. Exploring psychiatrists’ experiences during transition from mental health act, 1987 to mental healthcare act, 2017 in Goa, India. Indian J Psychol Med, 2023; 46: 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kodakandla K, Nasirabadi M and Pasha MS. Attitude of interns towards mental illness and psychiatry: a study from two medical colleges in South India. Asian J Psychiatry, 2016; 22: 167–173. [DOI] [PubMed] [Google Scholar]
- 43.Bhise MC, Marwale AV, Deshmukh AS, et al. Impact of differences in psychiatry curriculum of undergraduate medical and physiotherapy students on their attitude towards psychiatry. Indian J Psychiatry, 2016; 58: 208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta R and Khurana H.. Challenges in undergraduate psychiatric training in India. In: Malhotra S, Chakrabarti S (eds), Developments in psychiatry in India: clinical, research and policy perspectives. New Delhi, India: Springer, 2015, pp. 593–610. [Google Scholar]
- 45.Kallivayalil RA and Enara A.. Undergraduate education in psychiatry in India. Global Psychiatry, 2020; 3: 9–16. [Google Scholar]
- 46.Kishor M. A center for psychiatry education, faculty training, and research. Indian J Psychiatry, 2022; 64: 518–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salazar LJ, Chari U, Sharma P, et al. Facilitators and barriers to student learning and impact of an undergraduate clinical posting in psychiatry: a thematic analysis. Indian J Psychol Med, 2022; 44: 392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sagar R and Sarkar S.. Psychiatry as a separate subject in the undergraduate medical curriculum: the need re- emphasized. J Ment Health Hum Behav, 2016; 21: 88–90. [Google Scholar]
- 49.Kumar P, Jangid P and Sethi S.. Undergraduate psychiatry in India: a SWOT analysis. Asian J Psychiatry, 2018; 33: 46–51. [DOI] [PubMed] [Google Scholar]
- 50.Gupta S and Menon V.. Psychiatry training for medical students: a global perspective and implications for India’s competency-based medical education curriculum. Indian J Psychiatry, 2022; 64: 240–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thirunavukarasu M and Thirunavukarasu P.. Training and national deficit of psychiatrists in India: a critical analysis. Indian J Psychiatry, 2010; 52: S83–S88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.NMC (National Medical Commission). Competency-based medical curriculum. Psychiatry 2019; 2: 203. https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum/ (2019, accessed Jun 3 2023. ). [Google Scholar]
- 53.Sahadevan S, Kurian N, Mani AM, et al. Implementing competency-based medical education curriculum in undergraduate psychiatric training in India: opportunities and challenges. Asia Pac Psychiatry, 2021; 13: e12491. [DOI] [PubMed] [Google Scholar]
- 54.Charmaz K. Constructing grounded theory. London: Sage Publications, 2014. [Google Scholar]
- 55.Birks M and Mills J. Grounded theory: a practical guide. London: Sage Publications, 2015. [Google Scholar]
- 56.Guba EG and Lincoln YS. Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS (eds) Handbook of qualitative research. Thousand Oaks: Sage Publications, 1994, pp.105–117. [Google Scholar]
- 57.Hesse-Biber S. Qualitative approaches to mixed methods practice. Qual Inq, 2010; 16: 455-68. [Google Scholar]
- 58.Crotty MJ. The foundations of social research: meaning and perspective in the research process. Australia: Sage Publications, 1998. [Google Scholar]
- 59.Scotland J. Exploring the philosophical underpinnings of research: relating ontology and epistemology to the methodology and methods of the scientific, interpretive, and critical research paradigms. Engl Lang Teach, 2012; 5: 9–16. [Google Scholar]
- 60.van Veggel N, Allison J, Goldspink S, et al. The presuppositional interview is a means of transparent reflexive practice in grounded theory. Methodol Innov, 2023; 17: 31–40. [Google Scholar]
- 61.Thambinathan V and Kinsella EA. Decolonizing methodologies in qualitative research: creating spaces for transformative praxis. Int J Qual Methods, 2021; 20: 16094069211014766. [Google Scholar]
- 62.Guetterman TC, Babchuk WA, Howell Smith MC, et al. Contemporary approaches to mixed methods grounded theory research: a field-based analysis. J Mix Methods Res, 2019; 13: 179–195. [Google Scholar]
- 63.Streeton R, Cooke M and Campbell J.. Researching the researchers: using a snowballing technique. Nurse Res, 2004;12: 35–47. [DOI] [PubMed] [Google Scholar]
- 64.Hood JC. Orthodoxy vs. power: the defining traits of grounded theory. In: Bryant A and Charmaz K, (eds) The Sage handbook of grounded theory. Los Angeles: Sage Publications, 2007, pp.157–158. [Google Scholar]
- 65.Corbin J and Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. 4th ed. Thousand Oaks: Sage Publications, 2015. [Google Scholar]
- 66.Parikh NC, Sharma PS, Chaudhary PJ, et al. Study of attitude of interns toward psychiatry: a survey of a tertiary level hospital in Ahmedabad. Ind Psychiatry J, 2014; 23: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kishor M, Mysore AV, Mohan KI, et al. A survey among teachers of psychiatry to improve the quality of undergraduate training: outcomes from Karnataka. Indian J Psychol Med 2020; 42: 299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Avasthi A. Indianizing psychiatry—is there a case enough? Indian J Psychiatry, 2011; 53: 111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kahu ER and Nelson K.. Student engagement in the educational interface: Understanding the mechanisms of student success. High Educ Res Dev, 2018; 37: 58–71. [Google Scholar]
- 70.Ananthakrishnan N. Competency-based undergraduate curriculum for the Indian medical graduate, the new MCI curricular document: positives and areas of concern. SBV J Basic Clin Appl Health Sci, 2018; 1: 34–42. [Google Scholar]