Abstract
Background
Mental health literacy is a predictor of health outcomes in psychological distress. However, limited research has explored whether low mental health literacy is associated with recent depression and anxiety.
Methods
We used data from the Guangdong Mental Health Survey, a provincial representative and a population-based survey with a multistage stratified cluster random sampling method. We included adults aged 18 and above living in communities from September to December 2021 in Guangdong, China. Eligible participants were those who completed the mental health literacy questionnaire and assessments for depression and anxiety symptoms. We assessed the proportion of individuals with low mental health literacy by categories of psychological symptoms and whether low mental health literacy was associated with depressive and anxiety symptoms in the general population and subgroups.
Results
A total of 16,715 adults were included. We found that individuals with more severe symptoms had a greater proportion of low mental health literacy- it went from 89.4% in participants without depression or anxiety to 96.2% in people who co-occurred with depression and anxiety (x2 = 21.457, P < 0.001). After controlling confounders, low mental health literacy was associated with depression (adjusted Odds Ratio, aOR [95%CI]:2.74 [1.92–4.04]) and anxiety (2.27 [1.49–3.64]) in the total sample, when compared with adequate mental health literacy.
Conclusions
This study found a positive association between low mental health literacy and the presence of depression and anxiety. Tackling inadequate mental health literacy may be a key strategy to promote psychological well-being across the lifespan, especially for young adults.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20020-y.
Keywords: Health literacy, Depression, Anxiety, Psychological distress
Introduction
Depression and anxiety are the most common mental health problems that stand out for having a high prevalence and for their unpleasant outcomes. According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, depressive disorders accounted for the greatest share of mental illness DALYs (37.3%) followed by anxiety disorders (22.9%) [1]. Coexisting of these two mental health problems is common, which may lead to high burden and disorder severity [2]. The use of treatment for depression and anxiety disorders is low [3], despite there are evidence-based effective treatments including psychotherapy and pharmacotherapy. Therefore, preventing depression and anxiety from occurring is imperative, in addition to improving diagnosis and intervention for early psychological distress.
One potential modifiable target for mental health promotion and prevention is mental health literacy. Evidence suggests that mental health literacy plays a vital role in psychological well-being, and it might be associated with depression and anxiety because adequate mental health literacy may prevent people from unhealthy lifestyle that contributes to psychological distress [4–6]. However, previous studies indicated that mental health literacy is unsatisfactory, and low mental health literacy is common worldwide [7, 8]. In China, a recent systematic review revealed a low recognition rate among individuals for common mental disorders, with rates of 25.2% for depression and 18.2% for anxiety [8]. Low health literacy has been associated with non-communicable diseases [9, 10]. Similarly, low mental literacy may have an impact on depression and anxiety.
However, limited research has yet to examine whether low mental health literacy is associated with recent depression and anxiety. Research focused on this field is crucial because mental health literacy is modifiable and actionable in contrast to other predictors of poor psychological well-being. Moreover, little is known about the associations between mental health literacy and depression and anxiety during the adulthood. Previous studies have focused on specific groups, including adolescents [11], college students [12], and older adults [13].
This study aimed to deepen our understanding of the relationship between low mental health literacy and depression and anxiety, shedding light on the potential effects and implications of inadequate mental health literacy. First, we examined the distribution of low mental health literacy among individuals categorized by their psychological symptoms: those with both depression and anxiety, those with depression alone, those with anxiety alone, and those without either condition. Second, we evaluated the association between low mental health literacy and the prevalence of depression and anxiety in the overall population and across different age groups. It helps explore potential age-specific differences in the association between mental health literacy and psychological symptoms, providing insights that are crucial for tailored public health strategies.
Methods
Sample and procedures
The study sample was derived from the Guangdong Mental Health Survey, which was conducted from September to December 2021 in Guangzhou, China. The survey was a provincial representative and cross-sectional study that conducted to assess the prevalence of mental disorders and their social and psychological correlates that contributed to the psychological well-being of the general population. The study design and sample size have been described in previous studies [14]. In brief, a multistage stratified cluster random sampling method was used. All 21 cities in the province were included.
Eligible participants were individuals aged 18 and above who have lived in Guangdong Province for at least six months. A planned sample size of 20,680 was set before the survey was implemented. Some selected households did not meet the criteria or were unavailable for the survey. Finally, 16,715 participants provided valid data, giving a response rate of 80.8%.
The survey was carried out by a team of professionals comprising psychiatrists, public health physicians, community mental health doctors, nurses, and mental health social workers. Face-to-face assessments with the participants at community health service centers or participants’ houses were conducted. We used electronic questionnaires that required respondents to complete all fields before submission to ensure that all responses were complete. The study was carried out following the principles of the Declaration of Helsinki. The Research Ethics Committee of the Guangdong Provincial People’s Hospital, Guangzhou Academy of Medical Sciences approved the study. All participants gave informed consent prior to the survey.
Measurements
Mental health literacy
Mental health literacy was measured using China’s National Mental Health Literacy Questionnaire, which consists of three domains: mental health knowledge, mental health attitudes, and mental health skills. Specifically, mental health knowledge includes 20 items with a scoring range of 0-100; (b) mental health attitudes consist of 8 items with a scoring range of 8–32. (c) mental health skills consist of 16 items with a scoring range of 0–40. The overall mental health literacy score is calculated by summing the scores of the three domains, with higher scores indicating better mental health literacy. Mental health literacy was categorized into two groups (adequate/low). Adequate mental health literacy was defined using the following criteria, as suggested by the Institute of Psychology, Chinese Academy of Science who developed the questionnaire: (a) scoring 80 or higher in mental health knowledge, (b) scoring 24 or higher in mental health attitudes, and (c) score 28 or higher in mental health skills. Low mental health literacy was defined as not meeting these criteria for adequate mental health literacy.
Depression
Depression was assessed using the combination of the Chinese version of Patient Health Questionnaire-2 (PHQ-2) followed by PHQ-9. The two-step strategy was used to reduce the number of participants who had to complete the entire PHQ-9 [15]. The PHQ-2, which contains the first two questions from the PHQ-9 (depressed mood and anhedonia), has been suggested as a prescreening test before completing the full PHQ-9. Participants with a PHQ-2 score greater than 2 proceeded to complete the remaining items of the PHQ-9 questionnaire. The PHQ-9 consists of 9 items and each item assesses the severity of a particular depressive symptom that occurred over the preceding 14 days. Participants answered these items on a Likert scale ranging from 0 (Never) to 3 (Almost every day). The total score ranges from 0 to 27. A higher total score indicates more severe depression symptoms. Participants who had PHQ-2 scores of 2 and then PHQ-9 scores of 10 or greater were considered positive for current depression (yes/no). The cutoff point is in accordance with the study protocol and has been used in previous studies [16].
Anxiety
Anxiety was assessed using the Chinese version of Generalized Anxiety Disorder Scale-7 (GAD-7). It is a self-reported scale [17] that is used to assess anxiety symptoms and showed good psychometric estimates among Chinese population. The GAD-7 consists of 7 items and each item evaluates the severity of a particular anxiety symptom over the preceding 14 days. Participants answered these items on a Likert scale ranging from 0 (Never) to 3 (Almost every day). The total score ranges from 0 to 21. A higher total score indicates more severe anxiety symptoms. Participants who had a GAD-7 > = 10 were considered positive for current anxiety (yes/no). The cutoff point is in accordance with that used in previous studies [18].
Confounders
Socio-demographic and health information including age, sex, education level, marital status, residence, monthly household income, current smoking, current alcohol use, history of chronic diseases, previous help-seeking behavior, napping frequency, and sleep duration were assessed. Age (years) was grouped into three categories: young (18–44), middle-aged (45–64), and older ( > = 65) adults. The education level was divided into three categories: low, medium, and high. Monthly household income was measured with a six-item ordinal scale (from <¥3,500 to >¥20,000). The variable was categorized as low (<¥3,500), middle (¥3,500 to ¥6,000), and high (> ¥6,000). The presence of current smoking (yes/no) and current alcohol use were reported by the participants. The presence of current alcohol use was assessed using single items, adapted from previous surveys [19]. Previous help-seeking behavior (yes/no) was assessed using single-item measure, which has been used in large-scale surveys [20]. Measurements of current smoking, current alcohol use, history of chronic disease, previous help-seeking behavior, napping frequency, and sleep duration were described in the Supplementary Table 1.
Statistical analyses
We performed descriptive statists for the total sample using proportions (%), means, and standard deviations (SDs) where applicable. No missing data was detected. We used Pearson’s chi-squared tests, t tests, or Mann-Whitney tests to assess differences between the low- and adequate-mental-health-literacy groups. We assessed the proportions of participants with low and adequate mental health literacy among individuals categorized by their psychological symptoms: those with both depression and anxiety, those with depression alone, those with anxiety alone, and those without either condition. Specifically, participants with both anxiety and depression were classified as having coexisting depression and anxiety (yes/no). We compared the four groups using Pearson’s chi-squared linear-by-linear association in the total sample. To examine whether the association between low mental health literacy and depressive and anxiety symptoms remained significant among different age groups, we repeated the analyses for subgroups. We examined if low mental health was associated with current depression and current anxiety in the total sample and different age groups using logistic regression. We calculated unadjusted odds ratio (OR) and 95% confidential intervals (95%CIs) and adjusted OR (aOR) after adjustment for confounders including sociodemographic factors and other known risk factors for depression and anxiety. All statistical analyses were conducted using R version 4.2.2 and the significance level was set at 0.05 (two-tailed).
Results
Sample characteristics
A total of 16,715 participants (52.5% females, mean age of 49.0 ± 16.6 years) were included in the analysis. Among the total sample, 1,731 participants (10.4%) demonstrated adequate mental health literacy, while 14,984 participants had low mental health literacy. Participants with low mental health literacy were characterized by older age, lower proportions of females, urban residents, and previous help-seeking behavior, higher proportions of alcohol use, lower education level and income, and lower frequency of napping. Table 1 and Supplemental Table 2 show the comparison of characteristics in the total population and subgroups with different age.
Table 1.
Comparison of characteristics between participants with low and adequate mental health literacy in the total population
| Variables, % | Low MHL (N = 14984) | Adequate MHL (N = 1731) | Total sample (N = 16715) |
P |
|---|---|---|---|---|
| Age, yrs | < 0.001 | |||
| 18–44 | 6414 (42.8%) | 997 (57.6%) | 7411 (44.3%) | |
| 45–64 | 4932 (32.9%) | 415 (24.0%) | 5347 (32.0%) | |
| 65+ | 3638 (24.3%) | 319 (18.4%) | 3957 (23.7%) | |
| Education level | < 0.001 | |||
| Low | 3216 (21.5%) | 219 (12.7%) | 3435 (20.6%) | |
| Intermediate | 7311 (48.8%) | 601 (34.7%) | 7912 (47.3%) | |
| High | 4457 (29.7%) | 911 (52.6%) | 5368 (32.1%) | |
| Sex | < 0.001 | |||
| Female | 7790 (52.0%) | 989 (57.1%) | 8779 (52.5%) | |
| Male | 7194 (48.0%) | 742 (42.9%) | 7936 (47.5%) | |
| Marital status | 0.255 | |||
| Married | 11,947 (79.7%) | 1360 (78.6%) | 13,307 (79.6%) | |
| Single | 3037 (20.3%) | 371 (21.4%) | 3408 (20.4%) | |
| Residence | < 0.001 | |||
| Rural | 5849 (39.0%) | 571 (33.0%) | 6420 (38.4%) | |
| Urban | 9135 (61.0%) | 1160 (67.0%) | 10,295 (61.6%) | |
| Income | < 0.001 | |||
| <¥3,500 | 6725 (44.9%) | 557 (32.2%) | 7282 (43.6%) | |
| ¥3,500 to ¥6,000 | 4560 (30.4%) | 561 (32.4%) | 5121 (30.6%) | |
| >¥6,000 | 3699 (24.7%) | 613 (35.4%) | 4312 (25.8%) | |
| Smoking | < 0.001 | |||
| Yes | 3281 (21.9%) | 271 (15.7%) | 3552 (21.3%) | |
| No | 11,703 (78.1%) | 1460 (84.3%) | 13,163 (78.7%) | |
| Alcohol use | < 0.001 | |||
| Yes | 1489 (9.9%) | 98 (5.7%) | 1587 (9.5%) | |
| No | 13,495 (90.1%) | 1633 (94.3%) | 15,128 (90.5%) | |
| Chronic diseases | < 0.001 | |||
| Yes | 9242 (61.7%) | 1235 (71.3%) | 10,477 (62.7%) | |
| No | 5742 (38.3%) | 496 (28.7%) | 6238 (37.3%) | |
| Previous help-seeking behavior | < 0.001 | |||
| No | 12,418 (82.9%) | 1359 (78.5%) | 13,777 (82.4%) | |
| Yes | 2566 (17.1%) | 372 (21.5%) | 2938 (17.6%) | |
| Napping frequency, per week | < 0.001 | |||
| 0 | 2448 (16.3%) | 200 (11.6%) | 2648 (15.8%) | |
| 1–2 | 2692 (18.0%) | 248 (14.3%) | 2940 (17.6%) | |
| 3–4 | 2705 (18.1%) | 319 (18.4%) | 3024 (18.1%) | |
| 5+ | 7139 (47.6%) | 964 (55.7%) | 8103 (48.5%) | |
| Sleep duration, hours | 0.089 | |||
| < 7 | 4272 (28.5%) | 450 (26.0%) | 4722 (28.3%) | |
| 7–8 | 5326 (35.5%) | 638 (36.9%) | 5964 (35.7%) | |
| > 8 | 5386 (35.9%) | 643 (37.1%) | 6029 (36.1%) | |
| Depression | < 0.001 | |||
| No | 14,374 (95.9%) | 1699 (98.2%) | 16,073 (96.2%) | |
| Yes | 610 (4.1%) | 32 (1.8%) | 642 (3.8%) | |
| Anxiety | 0.004 | |||
| No | 14,634 (97.7%) | 1709 (98.7%) | 16,343 (97.8%) | |
| Yes | 350 (2.3%) | 22 (1.3%) | 372 (2.2%) |
Note MHL: mental health literacy
The proportions of participants with low mental health literacy
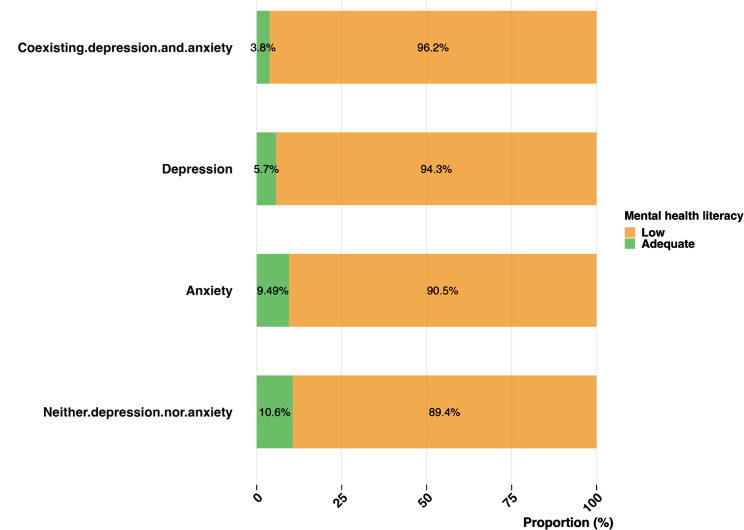
Within the total sample, the proportion of low mental health literacy was higher for individuals with more severe depressive and anxiety symptoms (Fig. 1), increasing from 89.4% in participants without either depression or anxiety to 96.2% in participants with coexisting depression and anxiety. The differences in the proportions across categories of psychological symptoms were statistically significant before (x2 = 21.457, P < 0.001) and after adjustment for confounders including education level, age, marital status, residence, income, alcohol use, previous help-seeking, napping frequency and sleep duration (P < 0.001). Supplemental Figs. 1–3 shows the proportions of low health literacy across different categories of psychological symptoms among young, middle-aged, and older adults.
Fig. 1.
Proportions of low mental health literacy across different categories of psychological symptoms
The association between low mental health literacy and depression and anxiety
Comparisons of characteristics of depression and anxiety in the total group were shown in Tables 2 and 3, respectively. Low mental health literacy was associated with recent depression and anxiety in the crude models (Table 4). After adjustments for confounders, low mental health literacy was associated with recent depression (OR: 2.25 [1.60–3.29], P < 0.001; aOR: 2.74 [1.92–4.04], P < 0.001) and anxiety (OR: 1.86 [1.23–2.95], P = 0.005), aOR: 2.27 [1.49–3.64], P < 0.001, respectively) in the total sample. There were no interactions between mental health literacy and different age groups (all P > 0.05).
Table 2.
Unadjusted odds ratio of depression in the total sample
| Variables, % | Without depression (N = 16073) |
Depression (N = 642) |
OR (95%CI, P) | |
|---|---|---|---|---|
| Age, yrs | 18–44 | 6998 (94.4) | 413 (5.6) | - |
| 45–64 | 5209 (97.4) | 138 (2.6) | 0.45 (0.37–0.54, p < 0.001) | |
| 65+ | 3866 (97.7) | 91 (2.3) | 0.40 (0.32–0.50, p < 0.001) | |
| Education level | Low | 3344 (97.4) | 91 (2.6) | - |
| Intermediate | 7670 (96.9) | 242 (3.1) | 1.16 (0.91–1.49, p = 0.236) | |
| High | 5059 (94.2) | 309 (5.8) | 2.24 (1.78–2.86, p < 0.001) | |
| Sex | Male | 7665 (96.6) | 271 (3.4) | - |
| Female | 8408 (95.8) | 371 (4.2) | 1.25 (1.06–1.47, p = 0.007) | |
| Marital status | Married | 12,918 (97.1) | 389 (2.9) | - |
| Single | 3155 (92.6) | 253 (7.4) | 2.66 (2.26–3.13, p < 0.001) | |
| Residence | Rural | 6224 (96.9) | 196 (3.1) | - |
| Urban | 9849 (95.7) | 446 (4.3) | 1.44 (1.21–1.71, p < 0.001) | |
| Income | >¥6,000 | 4130 (95.8) | 182 (4.2) | - |
| <¥3,500 | 7017 (96.4) | 265 (3.6) | 0.86 (0.71–1.04, p = 0.116) | |
| ¥3,500 to ¥6,000 | 4926 (96.2) | 195 (3.8) | 0.90 (0.73–1.10, p = 0.308) | |
| Smoking | No | 12,656 (96.1) | 507 (3.9) | - |
| Yes | 3417 (96.2) | 135 (3.8) | 0.99 (0.81–1.19, p = 0.888) | |
| Alcohol use | No | 14,555 (96.2) | 573 (3.8) | - |
| Yes | 1518 (95.7) | 69 (4.3) | 1.15 (0.89–1.48, p = 0.270) | |
| Chronic disease | No | 10,184 (97.2) | 293 (2.8) | - |
| Yes | 5889 (94.4) | 349 (5.6) | 2.06 (1.76–2.41, p < 0.001) | |
| Previous help-seeking behavior | No | 13,380 (97.1) | 397 (2.9) | - |
| Yes | 2693 (91.7) | 245 (8.3) | 3.07 (2.60–3.61, p < 0.001) | |
| Napping frequency, per week | 5+ | 7864 (97.1) | 239 (2.9) | - |
| 0 | 2535 (95.7) | 113 (4.3) | 1.47 (1.16–1.84, p = 0.001) | |
| 1–2 | 2803 (95.3) | 137 (4.7) | 1.61 (1.30–1.99, p < 0.001) | |
| 3–4 | 2871 (94.9) | 153 (5.1) | 1.75 (1.42–2.15, p < 0.001) | |
| Sleep duration, hours | > 8 | 5904 (97.9) | 125 (2.1) | - |
| < 7 | 4355 (92.2) | 367 (7.8) | 3.98 (3.25–4.91, p < 0.001) | |
| 7–8 | 5814 (97.5) | 150 (2.5) | 1.22 (0.96–1.55, p = 0.107) | |
| Mental health literacy | Adequate | 1699 (98.2) | 32 (1.8) | - |
| Low | 14,374 (95.9) | 610 (4.1) | 2.25 (1.60–3.29, p < 0.001) |
Table 3.
Unadjusted odds ratio of anxiety in the total sample
| Variables, % | Without anxiety (N = 16343) |
Anxiety (N = 372) |
OR (95%CI, P) | |
|---|---|---|---|---|
| Age, yrs | 18–44 | 7177 (96.8) | 234 (3.2) | - |
| 45–64 | 5262 (98.4) | 85 (1.6) | 0.50 (0.38–0.63, p < 0.001) | |
| 65+ | 3904 (98.7) | 53 (1.3) | 0.42 (0.31–0.56, p < 0.001) | |
| Education level | Low | 3384 (98.5) | 51 (1.5) | - |
| Intermediate | 7775 (98.3) | 137 (1.7) | 1.17 (0.85–1.63, p = 0.344) | |
| High | 5184 (96.6) | 184 (3.4) | 2.36 (1.74–3.25, p < 0.001) | |
| Sex | Male | 7789 (98.1) | 147 (1.9) | - |
| Female | 8554 (97.4) | 225 (2.6) | 1.39 (1.13–1.72, p = 0.002) | |
| Marital status | Married | 13,058 (98.1) | 249 (1.9) | - |
| Single | 3285 (96.4) | 123 (3.6) | 1.96 (1.57–2.44, p < 0.001) | |
| Residence | Rural | 6295 (98.1) | 125 (1.9) | - |
| Urban | 10,048 (97.6) | 247 (2.4) | 1.24 (1.00-1.54, p = 0.054) | |
| Income | >¥6,000 | 4188 (97.1) | 124 (2.9) | - |
| <¥3,500 | 7140 (98.0) | 142 (2.0) | 0.67 (0.53–0.86, p = 0.001) | |
| ¥3,500 to ¥6,000 | 5015 (97.9) | 106 (2.1) | 0.71 (0.55–0.93, p = 0.012) | |
| Smoking | No | 12,860 (97.7) | 303 (2.3) | - |
| Yes | 3483 (98.1) | 69 (1.9) | 0.99 (0.81–1.19, p = 0.888) | |
| Alcohol use | No | 14,806 (97.9) | 322 (2.1) | - |
| Yes | 1537 (96.8) | 50 (3.2) | 1.50 (1.09-2.00, p = 0.009) | |
| Chronic disease | No | 10,304 (98.3) | 173 (1.7) | - |
| Yes | 6039 (96.8) | 199 (3.2) | 1.96 (1.60–2.41, p < 0.001) | |
| Previous help-seeking behavior | No | 13,567 (98.5) | 210 (1.5) | - |
| Yes | 2776 (94.5) | 162 (5.5) | 3.77 (3.06–4.64, p < 0.001) | |
| Napping frequency, per week | 5+ | 7966 (98.3) | 137 (1.7) | - |
| 0 | 2584 (97.6) | 64 (2.4) | 1.44 (1.06–1.94, p = 0.017) | |
| 1–2 | 2846 (96.8) | 94 (3.2) | 1.92 (1.47–2.50, p < 0.001) | |
| 3–4 | 2947 (97.5) | 77 (2.5) | 1.52 (1.14–2.01, p = 0.004) | |
| Sleep duration, hours | > 8 | 5970 (99.0) | 59 (1.0) | - |
| < 7 | 4506 (95.4) | 216 (4.6) | 4.85 (3.65–6.54, p < 0.001) | |
| 7–8 | 5867 (98.4) | 97 (1.6) | 1.67 (1.21–2.33, p = 0.002) | |
| Mental health literacy | Adequate | 1709 (98.7) | 22 (1.3) | - |
| Low | 14,634 (97.7) | 350 (2.3) | 1.86 (1.23–2.95, p = 0.005) |
Table 4.
Association between low mental health literacy and recent depression and anxiety in the total sample
| Depression | Anxiety | |||
|---|---|---|---|---|
| Crude model | Adjusted model a | Crude model | Adjusted model a | |
| Adequate MHL | Reference | Reference | Reference | Reference |
| Low MHL | 2.25 (1.60–3.29) *** | 2.74 (1.92–4.04) *** | 1.86 (1.23–2.95,) ** | 2.27 (1.49–3.64) *** |
Note MHL: mental health literacy
a adjusted for age, education level, sex, marital status, residence, income, smoking, alcohol use, chronic diseases, previous help-seeking, napping frequency, and sleep duration
*** p < 0.001; ** p < 0.01; * p < 0.05
Among young adults, low mental health literacy was associated with recent depression (OR:2.21 [1.53–3.34], P < 0.001; aOR: 2.47 [1.68–3.78], P < 0.001, Supplemental Table 3) and anxiety (OR: 1.69 [1.09–2.76], P = 0.027; aOR:1.93 [1.22–3.21], P = 0.007; Supplemental Table 4). Among middle-aged adults, low mental health literacy was associated with recent depression (OR: 3.86 [1.46–15.72], P = 0.021; aOR: 3.68 [1.37–15.09], P = 0.028; Supplemental Table 5) but not anxiety (Supplemental Table 6). After adjustment for confounders, mental health literacy was not associated with recent depression in older adults (Supplemental Table 7).
Discussion
Primary findings
The main target of the study was to understand the relationship between low mental health literacy and depression and anxiety. We used a population-based survey with provincial presentative data (a) to assess the proportions of low mental health literacy among individuals experiencing different categories of psychological symptoms, and (b) to evaluate the associations between low mental health literacy and depression and anxiety across different stages of adulthood. We found that individuals with more severe depressive and anxiety symptoms had greater proportions of low mental health literacy compared to those with less severe symptoms. Second, low mental health literacy was associated with recent depression and anxiety in the crude analyses. After adjusting for confounders, this associations remained in the total sample and among young adults.
Comparison with previous studies
The study detected that the proportion of individuals with low mental health literacy was higher among the group with current depressive and anxiety than those without these symptoms. This is consistent with previous findings that people with depression and/or anxiety have low levels of mental health skills and awareness among adolescents [21] and older adults [13]. However, the current study features a significantly larger sample size and encompasses diverse age groups. Despite the fact that this study’s cross-sectional design limits making causal inferences, it implies that low mental health literacy may have a negative influence on depression and/or anxiety. The association is possible because individuals with inadequate mental health literacy may adopt poor lifestyle strategies, such as alcohol use and smoking, which hinder their mental well-being [4, 5]. Another explanation is that mental health literacy may mediate the relationship between resilience and psychological distress [22].
After adjusting for confounders, low mental health literacy was associated with recent depression in the total sample and among young and middle-aged adults. This result is aligned with previous cross-sectional studies among young adults, which showed college students with poor mental health knowledge had higher levels of depressive symptoms when compared to those with adequate knowledge [23, 24]. Intervention studies also supported the associations, which showed improving mental health literacy reduced depression symptoms [25]. Unlike other studies [13], we did not find low mental health literacy was associated with depression among older adults after controlling for known risk factors for depression. This may be explained that the associations between mental health literacy and psychological distress are typically different in younger and older people. Psychological distress in older adults may stem from other factors, such as chronic diseases [26, 27], other than mental health literacy. Another explanation is that most mental health literacy measurements are typically developed among young adults and limited to people with specific characteristics, such as college students [28, 29]. Therefore, further studies using sensitive measurements of mental health literacy for older adults are needed to explore the associations.
In our study, low mental health literacy was associated with recent anxiety in the total sample and among young adults after adjusting for confounders. The result is aligned with previous studies showing that young adults with poor mental health knowledge had higher levels of anxiety symptoms when compared to those with adequate knowledge [24]. Consistently, previous studies showed that interventions that targeted to improve mental health literacy reduced anxiety symptoms [25]. Our study did not find the associations between low mental health literacy and anxiety, which may be influenced by chronic diseases [30] and sleep problems [31]. We were not able to examine the associations between mental health literacy and anxiety among middle-aged and older adults due to the limited number of middle- aged and older adults who had adequate mental health literacy.
Implications
There are some important implications. First, the large proportion of low mental health literacy among adults with depressive and anxiety symptoms indicates that strategies to provide mental health services should cover difficulties inherent to low mental health literacy, such as cognitive change [32]. It is important to provide adequate psychoeducation for coexisting depression and anxiety. Previous studies showed that group psycho-educative cognitive-behavior therapy may be a promising strategy for coexisting depression and anxiety [33]. Second, our study suggested that strategies to improve mental health literacy should be tailed for adults. From a public health perspective, programs aimed at improving mental health literacy should be incorporated into mental health promotion and prevention of mental illness for adults across lifespan for people living in communities. Many studies have demonstrated that mental health literacy programs may be beneficial for young people in the school system. Similar programs should be adapted with a specific feasible and accessible focus in community settings and low resources areas. An example is the mhGAP-Intervention Guide carried out in Kenya with demonstrable results [34].
Limitations
Our study may have some limitations. First, the nature of the cross-sectional study design does not allow for a causal interpretation between low mental health literacy and depression and/or anxiety. Second, self-report measures were used for mental health literacy, depression, and anxiety, which may lead to some measurement error. However, the mental health literacy questionnaire was developed for the Chinese general population and has been recommended by China’s National Health Commission. In addition, PHQ-9 and GAD-7, which were used to measure depression and anxiety, are validated tools that have been applied to previous research. Third, the study was restricted to community-dwelling living in Guangdong, which may limit the generalizability of our findings. Future research may benefit from using a longitudinal study design and including individuals living in areas with limited health resources, together with structural assessments of depression and anxiety. Fourth, survey weights were not adjusted in our analyses due to a lack of detailed information on the sampling frame and weights. This might affect the generalizability of our findings. Finally, we used single items to measure smoking, alcohol use, and previous help-seeking behavior. Single-item measures are commonly used in large-scale studies to reduce respondent burden; however, they may not fully capture the complexity of these behaviors. Future studies should consider using more comprehensive scales and assessments.
Conclusion
This study aims to investigate the relationship between mental health literacy and depressive and anxiety in subgroups of adults. We identified that low mental health literacy was associated with severer depressive and anxiety distress in adults. We also found that low mental health literacy was linked to recent depressive symptoms in the total sample. Similarly, insufficient mental health literacy was associated with recent anxiety symptoms among adults. Enhancing awareness of mental health literacy should be prioritized as a crucial strategy for preventing depressive and anxiety and improving psychological well-being among adults. These measures could play a role in reducing important public health issues regarding the adverse impact of inadequate mental health literacy on psychological distress and promoting psychological well-being of the population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to acknowledge all participants and investigators in the study. The study received support from the Health Commission of Guangdong Province.
Abbreviations
- GBD
Global Burden of Diseases
- PHQ
Patient Health Questionnaire
- GAD-7
Generalized Anxiety Disorder Scale-7
- SDs
standard deviations
- OR
odds ratio
Author contributions
SZ: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. SW: Conceptualization, Data curation, Investigation, Methodology, Resources, Project administration, Writing – review & editing. KD: Data curation, Investigation, Resources, Project administration, Writing – review & editing. WT: Data curation, Investigation, Resources, Project administration, Writing - review & editing. LZ: Conceptualization, Methodology, Supervision, Writing – original draft, Writing -review & editing.
Funding
This project was supported by the Mental Health Prevention and Control of Guangdong Province, the National Social Science Foundation of China (Grant No. 19ZDA360), the National Natural Science Foundation of China (Grant No. 81803302), the Medical Scientific Research Foundation of Guangdong Province of China (Grant No.C2022010), Guangzhou Municipal Key Discipline in Medicine (2021–2023), Guangzhou High-level Clinical Key Specialty and the Guangzhou Research-oriented Hospital. The funding agencies had no role in the study design, data collection and management, data analysis, or interpretation of the data.
Data availability
The data of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was carried out following the principles of the Declaration of Helsinki. The Research Ethics Committee of the Guangdong Provincial People’s Hospital, Guangzhou Academy of Medical Sciences approved the study. All participants gave informed consent prior to the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shi-Bin Wang, Email: spiriorwang@126.com.
Liang Zhou, Email: liangzhou_csu@vip.163.com.
References
- 1.GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Penninx BWJH, Nolen WA, Lamers F, Zitman FG, Smit JH, Spinhoven P, et al. Two-year course of depressive and anxiety disorders: results from the Netherlands Study of Depression and anxiety (NESDA). J Affect Disord. 2011;133:76–85. [DOI] [PubMed] [Google Scholar]
- 3.Penninx BWJH, Pine DS, Holmes EA, Reif A. Anxiety disorders. Lancet. 2021;397:914–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacka FN, O’Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morales-Torres R, Carrasco-Gubernatis C, Grasso-Cladera A, Cosmelli D, Parada FJ, Palacios-García I. Psychobiotic effects on anxiety are modulated by Lifestyle behaviors: a randomized placebo-controlled trial on healthy adults. Nutrients. 2023;15:1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang Z, Yang X, Tan W, Ke Y, Kou C, Zhang M, et al. Patterns of unhealthy lifestyle and their associations with depressive and anxiety symptoms among Chinese young adults: a latent class analysis. J Affect Disord. 2024;352:267–77. [DOI] [PubMed] [Google Scholar]
- 7.Dang H-M, Lam TT, Dao A, Weiss B. Mental health literacy at the public health level in low and middle income countries: an exploratory mixed methods study in Vietnam. PLoS ONE. 2020;15:e0244573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li W, Reavley N. Recognition and beliefs about treatment for mental disorders in mainland China: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2020;55:129–49. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Health literacy development for the prevention and control of noncommunicable diseases: volume 1: overview. Geneva: World Health Organization: World Health Organization; 2022. [Google Scholar]
- 10.Gurgel do Amaral MS, Reijneveld SA, Geboers B, Navis GJ, de Winter AF. Low Health Literacy is Associated with the Onset of CKD during the Life Course. J Am Soc Nephrol JASN. 2021;32:1436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnco C, Rapee RM. Depression literacy and stigma influence how parents perceive and respond to adolescent depressive symptoms. J Affect Disord. 2018;241:599–607. [DOI] [PubMed] [Google Scholar]
- 12.Yao Z, Wang T, Yu Y, Li R, Sang X, Fu Y, et al. Mental health literacy and suicidal ideation among Chinese college students: the mediating role of depressive symptoms and anxiety symptoms. J Affect Disord. 2023. 10.1016/j.jad.2023.07.050. [DOI] [PubMed] [Google Scholar]
- 13.Ding K-R, Wang S-B, Xu W-Q, Lin L-H, Liao D-D, Chen H-B, et al. Low mental health literacy and its association with depression, anxiety and poor sleep quality in Chinese elderly. Asia-Pac Psychiatry off J Pac Rim Coll Psychiatr. 2022;14:e12520. [DOI] [PubMed] [Google Scholar]
- 14.Liao D-D, Dong M, Ding K-R, Hou C-L, Tan W-Y, Ke Y-F, et al. Prevalence and patterns of major depressive disorder and subthreshold depressive symptoms in south China. J Affect Disord. 2023;329:131–40. [DOI] [PubMed] [Google Scholar]
- 15.Levis B, Sun Y, He C, Wu Y, Krishnan A, Bhandari PM, et al. Accuracy of the PHQ-2 alone and in Combination with the PHQ-9 for screening to detect Major Depression: systematic review and Meta-analysis. JAMA. 2020;323:2290–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8:348–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- 18.Huang M, Liu Y, Wang J, Mo L, Wang Y, Chen L, et al. High rates of depression anxiety and suicidal ideation among inpatients in general hospital in China. Int J Psychiatry Clin Pract. 2019;23:99–105. [DOI] [PubMed] [Google Scholar]
- 19.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question Alcohol Screening Test. J Gen Intern Med. 2009;24:783–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osman N, Michel C, Schimmelmann BG, Schilbach L, Meisenzahl E, Schultze-Lutter F. Influence of mental health literacy on help-seeking behaviour for mental health problems in the Swiss young adult community: a cohort and longitudinal case–control study. Eur Arch Psychiatry Clin Neurosci. 2022. 10.1007/s00406-022-01483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lam LT. Mental health literacy and mental health status in adolescents: a population-based survey. Child Adolesc Psychiatry Ment Health. 2014;8:26. [Google Scholar]
- 22.Zhang J-Y, Ji X-Z, Zhou Y-Q. The Mediating Effect of Mental Health Literacy on psychological resilience and psychological distress of Medical College Students. Perspect Psychiatr Care. 2023;2023:e3461121. [Google Scholar]
- 23.Cheng S, An D, Yao Z, Liu JJ-W, Ning X, Wong JP-H, et al. Association between Mental Health Knowledge Level and depressive symptoms among Chinese College students. Int J Environ Res Public Health. 2021;18:1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang X, Wang X, Hu J, Xue Y, Wei Y, Wan Y, et al. Inadequate Mental Health Literacy and Insufficient Physical Activity potentially increase the risks of anxiety and depressive symptoms in Chinese College Students. Front Psychiatry. 2021;12:753695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pinho L, Correia T, Sampaio F, Sequeira C, Teixeira L, Lopes M, et al. The use of mental health promotion strategies by nurses to reduce anxiety, stress, and depression during the COVID-19 outbreak: a prospective cohort study. Environ Res. 2021;195:110828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birk JL, Kronish IM, Moise N, Falzon L, Yoon S, Davidson KW. Depression and multimorbidity: considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019;38:802–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei J, Hou R, Zhang X, Xu H, Xie L, Chandrasekar EK, et al. The association of late-life depression with all-cause and cardiovascular mortality among community-dwelling older adults: systematic review and meta-analysis. Br J Psychiatry. 2019;215:449–55. [DOI] [PubMed] [Google Scholar]
- 28.Kutcher S, Wei Y, Coniglio C. Mental Health literacy. Can J Psychiatry Rev Can Psychiatr. 2016;61:154–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Connor M, Casey L, Clough B. Measuring mental health literacy – a review of scale-based measures. J Ment Health. 2014;23:197–204. [DOI] [PubMed] [Google Scholar]
- 30.Liu X, Cao H, Zhu H, Zhang H, Niu K, Tang N, et al. Association of chronic diseases with depression, anxiety and stress in Chinese general population: the CHCN-BTH cohort study. J Affect Disord. 2021;282:1278–87. [DOI] [PubMed] [Google Scholar]
- 31.Zhou L, Zhang H, Luo Z, Liu X, Yang L, Hu H, et al. Abnormal night sleep duration and inappropriate sleep initiation time are associated with elevated anxiety symptoms in Chinese rural adults: the Henan Rural Cohort. Psychiatry Res. 2020;291:113232. [DOI] [PubMed] [Google Scholar]
- 32.Moreno-Peral P, Bellón JÁ, Huibers MJH, Mestre JM, García-López LJ, Taubner S, et al. Mediators in psychological and psychoeducational interventions for the prevention of depression and anxiety. A systematic review. Clin Psychol Rev. 2020;76:101813. [DOI] [PubMed] [Google Scholar]
- 33.Bains MK, Scott S, Kellett S, Saxon D. Group psychoeducative cognitive-behaviour therapy for mixed anxiety and depression with older adults. Aging Ment Health. 2014;18:1057–65. [DOI] [PubMed] [Google Scholar]
- 34.Mutiso VN, Pike KM, Musyimi CN, Rebello TJ, Tele A, Gitonga I, et al. Changing patterns of mental health knowledge in rural Kenya after intervention using the WHO mhGAP-Intervention guide. Psychol Med. 2019;49:2227–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of this study are available from the corresponding author upon reasonable request.