Abstract
Purpose
This scoping review with expert insight aims to map outcome measures following supercharged end-to-side anterior interosseous nerve to ulnar nerve transfer procedures, integrating clinical, patient-reported, and electrodiagnostic measures. It also explores surgical rationale and recovery trajectories, aiming to standardize methodologies and enhance patient care in nerve transfer surgeries.
Methods
Our search encompassed multiple online databases, including MEDLINE, Embase, PubMed, and Google Scholar, ensuring rigor and comprehensiveness in identifying relevant literature.
Results
Through scrutiny of 17 studies involving 300 patients from 300 articles, along with expert consultations on supercharged end-to-side nerve transfer for ulnar nerve entrapment, promising outcomes emerge, particularly in cubital tunnel syndrome. Primary measures such as Medical Research Council scale assessments and Disabilities of the Arm, Shoulder, and Hand scores demonstrate notable postsurgery improvements, with minor complications noted. Factors influencing recovery include preoperative dysfunction duration and surgical technique. Surgery indications prioritize high ulnar nerve injuries and severe cubital tunnel syndrome.
Conclusions
The review highlights the importance of standardized outcome measures, early intervention, and comprehensive rehabilitation for optimizing supercharged end-to-side anterior interosseous nerve to ulnar nerve transfer outcomes.
Type of study/level of evidence
Therapeutic IIIa.
Key words: Anterior interosseous nerve, Cubital tunnel syndrome, Nerve transfer, Supercharged end-to-side, Ulnar neuropathy
The ulnar nerve is essential for hand function, controlling motor activities and providing sensation. Damage to the ulnar nerve can lead to muscle control imbalances, reduced lateral pinch strength, and digital dexterity, potentially resulting in claw hand deformity.1 In adults, proximal ulnar nerve damage often leads to irreversible degeneration of motor endplates before reinnervation, especially when a significant gap exists between the endplates and the injury site, hindering complete functional restoration.1
Nerve transfers to the distal ulnar nerve have become increasingly popular for treating severe cubital tunnel syndrome.2 The anterior interosseous nerve (AIN) to ulnar nerve transfer, first described in the 1990s, initially used end-to-end coaptations.3 Later research introduced reverse end-to-side, or supercharged end-to-side (SETS), neurorrhaphy, demonstrating that axonal augmentation through reverse end-to-side neurorrhaphy promotes functional recovery of denervated targets.4
In 2012, Barbour et al5 combined nerve transfer techniques with novel end-to-side methods to describe the first AIN to ulnar motor fascicle SETS transfers. This technique protects and maintains distal motor endplates in patients regenerating from proximal ulnar nerve injury. Supercharged end-to-side can preserve the injured nerve and potentially speed up reinnervation by adding more axons to the regenerated neuron. Specifically, SETS transfers the terminal AIN to the pronator quadratus muscle end-to-side to the motor fascicle of the ulnar nerve in the distal forearm. This method is particularly useful in second- and third-degree axonometric nerve damage, improving partial recovery and protecting motor endplates.5, 6, 7
Recent advancements in treating severe ulnar neuropathy, including SETS AIN to ulnar nerve transfers, highlight the need for standardized outcome measures. A recent publication introduced the abduction hand diagram as a novel outcome measure, reflecting ongoing innovation and underscoring the variability and lack of standardization in current methodologies.8 This variability complicates the comparison of surgical outcomes and hampers the generalization of successful techniques, making standardized measures essential.
The abduction hand diagram offers a straightforward recovery assessment, but the diversity of outcome measures demonstrates a fragmented approach to evaluating surgical efficacy. These measures range from subjective assessments like the Medical Research Council (MRC) scale to more objective methods such as nerve conduction studies and EMG.
This scoping review aims to systematically map existing evidence regarding the variety of outcome measures used following SETS AIN to ulnar nerve transfers for treating ulnar nerve entrapment. This includes clinical, patient-reported, and electrodiagnostic measures in both short-term and long-term follow-ups. Additionally, the review will integrate expert opinions and potentially unpublished data, assessing the consistency and relevance of these measures in capturing true clinical improvements.
The secondary aim is to explore the surgical rationale behind using SETS transfers, focusing on specific patient populations, diagnoses, and documented recovery trajectories. This will facilitate a deeper understanding of why these surgical interventions are chosen and their broader implications, providing insights to guide future clinical practice and research.
Together, these aims will offer a comprehensive overview of the outcome measures used in SETS transfers, identify gaps and inconsistencies in the literature, and pave the way for standardizing methodologies to enhance the quality and consistency of patient care in nerve transfer surgeries.
Materials and Methods
We followed the framework proposed by Arksey and O’Malley9 with additional suggestions by Levac et al10 to conduct a scoping review on the SETS AIN to ulnar nerve transfer. The review involved five stages: identifying the research question; identifying relevant studies; selecting studies for detailed analysis; charting the data; and collating, summarizing, and reporting the results. Additionally, we incorporated an expert panel to deepen our understanding of SETS nerve transfer beyond published literature, ensuring a comprehensive exploration of this complex subject.11
Data sources and searches
To identify relevant peer-reviewed articles, we searched online databases including MEDLINE, Embase, PubMed, and Google Scholar, with the last search completed in December 2023. A librarian-assisted search strategy targeted databases like PubMed, Embase, and MEDLINE, using keywords “(ulnar OR anterior interosseous) AND nerve AND transfer AND (cubital tunnel OR [ulnar neuropathy AND elbow])” to filter relevant studies on SETS nerve transfer impacts.
Study selection
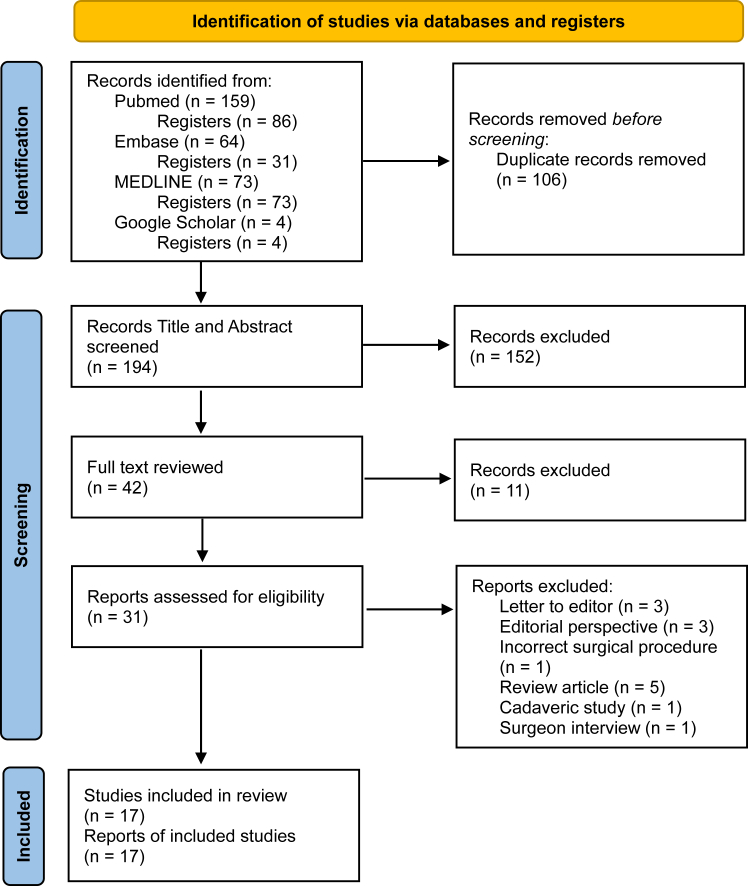
We included full-text, peer-reviewed English language studies discussing outcomes and influential factors following SETS AIN to ulnar nerve transfer in adults. Inclusion criteria covered various study designs, including qualitative, quantitative, mixed methods, and knowledge syntheses (narrative, systematic, and scoping reviews), as well as case reports and studies. Exclusions were made for conference abstracts, research letters, editorials, opinion pieces, and project evaluation reports. Studies not directly related to SETS nerve transfers, lacking focus on patient outcomes or procedural efficacy, or those not peer-reviewed were excluded. We prioritized English or translatable peer-reviewed articles. The selection process followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist and protocols for registration on the Open Science Framework as in Figure.12 Two independent reviewers conducted the search and screening, with discrepancies resolved by a senior author.
Figure.
Selection studies on outcomes and influential factors following supercharged end-to-side anterior interosseous nerve to ulnar nerve transfer.12
Extraction and charting the data
A data extraction form was developed to collect information on authors, publication year, country of origin, type of surgery, patient demographics, study design, and significant factors impacting recovery. Two reviewers (T.J. and M.F.) extracted data on publication year, surgery type, source, and methodological details to describe the population and surgical approach, alongside factors affecting recovery and patient satisfaction. An in-depth analysis of selected articles was conducted, with critical recovery-related factors organized through regular discussions to ensure a unified understanding. The team reviewed the data, resolving disagreements with senior author (J.M.) input. A systematic approach was adopted to identify and categorize information, directly employing and synthesizing extracted data.
Experts’ consultation
To ensure a comprehensive understanding of nonpublished data related to SETS AIN to ulnar nerve transfer outcomes, findings were presented to leading experts in the field, including hand and orthopedic surgeons with over 30 years of experience in nerve transfer techniques, from prominent institutions. Their insights on additional recovery factors and patient outcomes enriched our review with expert knowledge beyond published literature [available online on the Journal’s website at https://www.jhsgo.org].
Results
Our comprehensive search identified 296 articles, with four additional records, for a total of 300. After removing duplicates, 194 records were screened, and 38 full texts were reviewed, with 13 meeting the criteria. Four more articles were added from reference checking. Studies included cohorts (9, 53%), case reports (5, 29%), one case series, one randomized controlled trial, and one systematic review.8,13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 Supercharged end-to-side showed promise for ulnar nerve axon regeneration and improved recovery in revision surgeries for cubital tunnel syndrome.14,16,19, 20, 21, 22, 23, 24,27, 28, 29, 30, 31, 32, 33 Postoperative first dorsal interosseous (FDI) strength improved, with over 75% achieving MRC grade ≥ 3.16,18,19,21 Minor complications did not affect outcomes.15,16,27 Many surgeons prefer AIN-SETS transfers for high ulnar nerve injuries and severe cubital tunnel syndrome, reflecting growing clinical acceptance.34,35
Patient characteristics
A total of 300 patients with a mean age of 52 underwent SETS AIN to ulnar motor nerve transfers, with 70% being male (Table 1).8,13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28,36 Timing from injury to treatment is critical, with an 8-week cut-off for early or delayed intervention.14 Immediate surgical intervention is recommended for severe cases to prevent permanent disability.
Table 1.
Articles Reporting Outcomes from SETS Procedure
| Authors | Year of Publication | Study Design/Level of Evidence36 | Sample Size | Mean Age | Male (%) |
|---|---|---|---|---|---|
| Thorkildsen et al13 | 2024 | Prospective cohort study (level 2) | 9 | 40 | 6 (67) |
| Chen et al14 | 2021 | Retrospective cohort study (level 3) | 13 | 38 | 9 (69) |
| Dengler et al15 | 2020 | Retrospective cohort study (level 3) | 42 | 48 | 33 (79) |
| Doherty et al16 | 2020 | Retrospective cohort study (level 3) | 30 | 53 | 21 (70) |
| Dunn et al28 | 2019 | Systematic review (level 1) | 78∗ | 46 | 45 (58) |
| Evans et al17 | 2021 | Retrospective cohort study (level 3) | 30 | 57 | 22 (73) |
| Jarvie et al22 | 2018 | Case report (level 5) | 2 | 57 | 1 (50) |
| Kale et al23 | 2011 | Case report (level 5) | 1 | 65 | 1 (100) |
| Knight et al8 | 2023 | Case series (level 4) | 9 | 68 | 7 (78) |
| McLeod et al18 | 2020 | Retrospective cohort study (level 3) | 17 | 48 | - |
| Pathiyil et al24 | 2023 | Case report (level 5) | 1 | 36 | 0 (0) |
| Power et al25 | 2020 | Case report (level5) | 3 | 50 | 3 (100) |
| Tsang et al26 | 2021 | Case report (level 5) | 3 | 77 | 3 (100) |
| Xie et al27 | 2022 | Randomized control trial (level 1) | 45 | 56 | 34 (75) |
| Davidge et al19 | 2015 | Retrospective cohort study (level 3) | 55 | 50 | 38 (61) |
| Baltzer et al20 | 2016 | Retrospective cohort study (level 3) | 13 | 35 | - |
| Head et al21 | 2020 | Retrospective cohort study (level 3) | 17 | 57 | 11 (65) |
Our scoping review, encompassing 17 studies, explored diverse applications of SETS AIN to ulnar nerve transfers. Cubital tunnel syndrome was the focus of eight studies, comprising 47% of the review.15, 16, 17,21,23,25, 26, 27 Primary outcomes typically involved assessing muscle strength in the FDI and abductor digiti minimi using the MRC scale, alongside the Disabilities of the Arm, Shoulder, and Hand (DASH) score.17,26 Secondary outcomes encompassed electrodiagnosis, recovery time, clawing deformity restoration, pinch and grip strength measures, pain, hand abduction, and therapy adherence.15, 16, 17,21,23,25, 26, 27 Initial MRC FDI scores notably improved within 3 months postsurgery, with subsequent follow-ups indicating significant enhancement in muscle strength. Long-term observations revealed substantial improvements in DASH scores, pinch strength, and grip strength.15, 16, 17,21,23,25, 26, 27
Three additional studies examined mixed diagnoses involving proximal compression or traumatic injuries19,20,28 Primary outcomes focused on intrinsic muscle function return and FDI muscle MRC scores, with secondary outcomes including pinch and grip strength measures and claw deformity restoration. These studies observed that 69% of patients regained function within 3 to 12 months postoperation, with 23% experiencing rapid recovery within 3 months. Over time, patients showed improvement in FDI strength, with a higher proportion achieving grades equal to or greater than three. Comparative analysis revealed superior intrinsic function return in SETS patients (84%) compared to non-SETS patients (38%).19,20,28
A case report demonstrated successful SETS procedure use for traumatic nerve injury at the elbow, leading to restored ulnar intrinsic function.24 Three studies on severe ulnar neuropathy primarily assessed outcomes using MRC and QuickDASH (Quick Disabilities of the Arm, Shoulder, and Hand) scores, showing a 22% improvement in MRC scores postsurgery.8,18,22 Early SETS procedures within 12 months of diagnosis yielded significantly higher MRC scores at the last follow-up. QuickDASH scores improved by approximately 13 points after surgery. Two studies on high ulnar nerve injuries proximal to the elbow used Rosen scores and pinch strength as primary outcomes, indicating statistically significant improvements in pinch strength by 6 months post-SETS AIN transfers.13,14 Total Rosen scores showed significant improvements at 1 year, and QuickDASH scores improved at long-term follow-ups between 1 and 2 years posttreatment. Neurophysiological signs of improvement were detectable in only one of nine patients, suggesting uncertainty regarding the SETS procedure’s clinical role (Table 2).8,13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
Table 2.
Details of the Selected Articles
| Authors, Year (Type) | Diagnosis | Objective | Outcomes | Follow-Up Time (After Surgery) | Result |
|---|---|---|---|---|---|
| Thorkildsen et al,13 2024 (prospective cohort) | Complete ulnar nerve injuries at or proximal to the elbow | To use detailed clinical and neurophysiological examinations to strengthen outcome assessment after SETS for ulnar nerve injury |
|
|
|
| Chen et al,14 2021 (retrospective cohort) | Isolated and high ulnar nerve injuries | To compare motor recovery after early or delayed ETS AIN transfer versus conventional procedures |
|
|
|
| Dengler et al,15 2020 (retrospective cohort) | Severe cubital tunnel syndrome | To provide an update on their clinical experience in the setting of severe cubital tunnel syndrome |
|
|
|
| Doherty et al,16 2020 (retrospective cohort) | Severe cubital tunnel syndrome | To prove the hypothesis that the addition of SETS transfer to subcutaneous transposition will demonstrate early reinnervation of intrinsic musculature and improved functional recovery |
|
|
|
| Dunn et al,28 2019 (systematic review) | All types (transection, compression, lesion-in-continuity, motor neuropathy, and neuritis) | To review the demographics, outcomes, and complications following SETS for proximal ulnar nerve injuries |
|
|
|
| Evans et al,17 2021 (retrospective cohort) | Cubital tunnel syndrome | To evaluate the impact of adjunctive procedures including SETS and electrical stimulation on patient outcomes |
|
|
|
| Jarvie et al,22 2018 (case report) | Rapidly severe progressive ulnar neuropathy (no trauma) | To describe two cases with electromyographic findings where SETS was performed to successfully treat rapidly progressive ulnar neuropathy |
|
|
|
| Kale et al,23 2011 (case report) | Cubital tunnel syndrome | To report successful recovered ulnar intrinsic function after SETS procedure |
|
|
|
| Knight et al,8 2023 (case series) | Severe compressive ulnar neuropathy | To extensively explore hand therapy and rehabilitation outcomes after SETS nerve transfers |
|
|
|
| McLeod et al,18 2020 (retrospective cohort) | Severe chronic ulnar neuropathy (McGowan grade III ulnar neuropathy) | To evaluate intrinsic muscle recovery in patients who have undergone both a proximal ulnar nerve decompression at the elbow and an AIN-to-UMN transfer (both ETE and ETS) |
|
|
|
| Pathiyil et al,24 2023 (case report) | Severe traumatic ulnar neuropathy at elbow | To report the SETS procedural technique | NA | NA | NA |
| Power et al,25 2020 (case report) | Cubital tunnel syndrome | To present guidelines for patient selection after diagnosis of cubital tunnel syndrome | EMG | NA | NA |
| Tsang et al,26 2021 (case report) | Cubital tunnel syndrome | To evaluate the SETS AIN to ulnar nerve technique for cubital tunnel syndrome in comparison with a standard ulnar nerve transposition |
|
|
|
| Xie et al,27 2022 (randomized controlled trial) | Severe cubital tunnel syndrome based on the modified McGowan classification | To compare ulnar nerve decompression and anterior subfascial transposition with versus without SETS AIN to ulnar motor nerve transfer for advanced cubital tunnel syndrome |
|
|
|
| Davidge et al,19 2015 (retrospective cohort) | Both compression and high ulnar nerve injuries | To review clinical experience after SETS |
|
|
|
| Baltzer et al,20 2016 (retrospective cohort) | Proximal ulnar nerve injuries (either traumatic or compressive) | To prove that patients with a SETS AIN to ulnar motor nerve transfer would demonstrate superior return of intrinsic function compared with conventional treatment only |
|
|
|
| Head et al,21 2020 (retrospective cohort) | Severe cubital tunnel syndrome | To evaluate the clinical and electrodiagnostic pattern of reinnervation of intrinsic hand musculature following SETS AIN to ulnar motor nerve transfer |
|
|
|
ADM, abductor digiti minimi; AIN, anterior interosseous nerve; ETE, end-to-end; ETS, end-to-side; FDI, first dorsal interosseous; MRC, Medical Research Council; QuickDASH, Quick Disabilities of the Arm, Shoulder, and Hand; SETS, supercharged end-to-side; SF-12, 12-Item Short Form Survey; UMN, ulnar motor nerve; VAS, visual analog scale.
The outcomes from the scoping review of studies on SETS transfers for ulnar nerve entrapment can be categorized into primary and secondary measures, with certain variations observed across different diagnoses (Table 3).
Table 3.
Interventional Mapping Table of SETS Scoping Review with Expert Insights
| Category | Results | Expert Insights |
|---|---|---|
| Primary outcomes |
Subjectives:
|
|
| Secondary outcomes |
Subjectives:
|
|
| Timing of assessment |
|
|
| Donor site morbidity and complications |
|
|
| Factors associated with recovery |
|
|
| Indication for surgery |
|
|
ADM, abductor digiti minimi; FDI, first dorsal interosseous; MRC, Medical Research Council; PQ, pronator quadratus; QuickDASH, Disabilities of the Arm, Shoulder, and Hand; SETS, supercharged end-to-side.
Primary outcome measures
The primary outcome measures included the following:
-
1.
Medical Research Council scale for muscle strength: This scale assesses the strength of the FDI and abductor digiti minimi muscles.
-
2.
DASH and QuickDASH score.
-
3.
Rosen score: This score is applied mainly in studies dealing with high ulnar nerve injuries proximal to the elbow to assess overall nerve function and recovery.
-
4.
Return of intrinsic muscle function: The restoration of intrinsic muscle functionality is assessed, particularly in studies involving mixed diagnoses of proximal compression or traumatic injuries.
Experts agreed on primary outcomes and suggested three additional considerations for assessing recovery after SETS: intrinsic muscle strength in different forearm postures (with a preference for pronation), evaluation of dorsal web space intrinsic muscle atrophy (FDI muscle), and the use of Tinel sign for early motor nerve recovery assessment.
Secondary outcome measures
The primary outcome measures included the following:
-
1.
Electrodiagnosis: Nerve conduction studies and EMG were included to assess nerve and muscle response.
-
2.
Recovery time: The duration required for observable clinical improvement or recovery postsurgery, as noted in studies of cubital tunnel syndrome.
-
3.
Restoration of clawing deformity: Studies focused on the effectiveness of the surgery in correcting specific deformities associated with ulnar nerve damage, especially studies with mixed diagnoses.
-
4.
Pinch and grip strength measures: These measures are used to evaluate the functional recovery of hand strength, which is standard across all types of ulnar nerve injuries.
-
5.
Pain assessment: This outcome is used to evaluate changes in pain levels postsurgery, especially in studies of cubital tunnel syndrome and severe ulnar neuropathy.
-
6.
Hand abduction and therapy adherence: This outcome is used to evaluate patient compliance with therapeutic protocols, mostly noted in cubital tunnel syndrome studies.
-
7.
Sensation and physical examination: Egawa and Froment signs detect specific neurological impairments or improvements, particularly in studies of severe ulnar neuropathy.
Outcome measures vary across ulnar nerve injuries. Cubital tunnel syndrome studies prioritize DASH scores, MRC scale, and pain measures. Severe ulnar neuropathy research focuses on quality of life and QuickDASH scores. High ulnar injuries use the Rosen score for comprehensive nerve recovery assessment, reflecting tailored approaches to each condition.
Donor site morbidity and complications
Two studies found no deficits in pronation range of motion or strength; others also noted no donor site morbidity.14, 15, 16,18,19,26,27 Although three studies reported no postsurgery complications, two reported minor issues like infection and hematoma, manageable with standard care.14,16,26, 27, 28 Experts emphasize minimal donor site morbidity and manageable complications, highlighting surgical precision risks.
Factors associated with recovery
Preoperative dysfunction duration, patient-specific variables, nerve lesion severity, and surgical technique significantly influence recovery outcomes post supercharged nerve transfer.14, 15, 16,18, 19, 20,23,24,26,28,29,31,34,35,37 Older age and extended muscle atrophy are adverse predictors. Lesions closer to target areas show better recovery. Proper surgical placement and rehabilitation adherence are crucial determinants of success.19,25,26
Experts provided further insights enhancing recovery factor understanding, despite existing consensus on extracted evidence:
-
1.
Nerve transfer should occur 9 cms proximal to the wrist crease to avoid tension. Positioning distally may hinder regeneration.
-
2.
Decompression at ulnar Guyon canal is crucial to prevent recovery hindrance.
-
3.
Microscopic surgery aids precise dissection, reducing damage to tissues. Delicate sutures facilitate finer nerve suturing, enhancing regeneration.
-
4.
End-to-end nerve transfer is recommended for severe cases lacking ulnar motor nerve response, which is crucial for optimal recovery.
Indication for surgery
This review identified common indications for supercharged nerve transfer surgery. High ulnar nerve injuries proximal to the flexor carpi ulnaris muscle and severe cubital tunnel syndrome were prominent, cited in three (18%) and eight (47%) studies, respectively.13, 14, 15,17,21,23, 24, 25,27 Additionally, normal pronator quadratus (PQ) muscle function was highlighted as crucial in two (12%) studies.15,19
Experts stress evaluating the PQ muscle function before surgery, typically through EMG, to confirm its suitability as a nerve transfer donor. Additionally, they highlight the significance of an electrodiagnostic protocol in identifying appropriate candidates for ulnar nerve surgery.
Discussion
Our scoping review of 17 studies examined 300 patients, revealing a mean age of 52 years with 70% male representation. The research spans middle to older adult demographics, reflecting a male prevalence in the literature. Variability exists in outcome measures and timing of intervention for ulnar nerve pathology treated with SETS transfers, highlighting the need for standardized measures to improve comparisons and generalizability. Predominant diagnoses include cubital tunnel syndrome, with attention also given to traumatic and other ulnar neuropathies, indicating research focus on prevalent conditions impacting quality of life.
The review focuses on functional and neurological recovery postsurgery, with primary outcomes centered on MRC and DASH scores, crucial for evaluating nerve transfer surgery success.13,14 Assessing intrinsic muscle function provides insights into functional improvement and muscle strength recovery.19,20 Forearm posture, especially pronation, influences accurate assessment because of "donor dominance," enhancing intrinsic motor function compared to supination.15 Pronation optimizes muscle fiber alignment, improving force generation and neural signal transmission along the AIN pathway.38 Tinel sign now aids in assessing motor nerve recovery and monitoring progress from the anastomosis site to the wrist, thus reflecting the need for early detection of nerve regeneration and functional restoration.38 Observing FDI atrophy serves as a visual progress indicator postprocedure. Secondary outcomes, including electrodiagnosis and recovery time, provide insights into nerve transfer surgery efficacy.15,20 Physical examinations, such as range of motion assessment, strength measurement, ulnar nerve special tests, and pain assessment, are crucial for evaluating recovery.15,20 Recently, assessing total hand abduction distance and finger tracing aids in understanding hand functionality26
Post-SETS AIN to ulnar motor nerve transfer, initial improvement occurs within 2–3 months because of remyelination, with axonal regeneration starting at 4–5 months and supercharge transfers showing results at 6–7 months.25 Nascent units appear around 8.5 months, with ongoing recovery at 12 and 24 months because of reinnervation and neuroplasticity.16,32,39 Experts agree on the importance of conducting recovery evaluations at various time points because of the dynamic nature of nerve regeneration. Although there is consensus on medium-term evaluations, opinions vary on the timing within the 12- to 24-month range, reflecting differences in clinical practices and patient characteristics. Some prioritize earlier assessments for prompt rehabilitation adjustments, whereas others prefer later evaluations for observing substantial gains.
The AIN PQ branch serves as an excellent donor because of anatomical advantages, supported by minimal donor site morbidity in reviewed studies.29,40 Most studies report low serious complication rates with supercharge nerve transfer, affirming its safety.16,27 Scoping review and expert opinions concur, noting favorable outcomes, minimal donor site morbidity, and low complication rates for ulnar neuropathy treatment. The sole concern involves potential misidentification of nerves during sensory branch side-to-side anastomosis, risking transfer of the ulnar nerve's sensory branch instead of the motor branch.
Several factors significantly influence recovery outcomes. Longer preoperative dysfunction durations consistently correlate with poorer outcomes.34 Patient-specific factors such as age, anatomical considerations, medical comorbidities, and duration of muscle denervation impact recovery, with older age and prolonged atrophy serving as adverse predictors. The level and severity of the nerve lesion also affect recovery, with greater severity posing greater challenges.23 For severe cases, experts prefer the end-to-end method for optimal functional recovery. Surgical technique recommendations include performing the transfer approximately 9 cm above the wrist crease to prevent tension on the repair and avoiding distal placement, which may hinder nerve regeneration or compress the motor branch around the hamate.25 Comprehensive rehabilitation, supported by patient education and motivation, is vital for maximizing surgical intervention benefits and promoting functional recovery.26 These findings underscore the complex interplay of factors shaping the success of supercharge nerve transfer procedures for ulnar neuropathy.
Our scoping review highlights primary indications for supercharge nerve transfer, including high ulnar nerve injury, severe cubital tunnel syndrome resistant to previous interventions, and a normal PQ muscle.14,15 Understanding these indications aids clinician decision making and improves treatment outcomes for ulnar neuropathy. Experts recommend an electrodiagnostic protocol for cubital tunnel syndrome diagnosis, including nerve conduction velocity tests across the elbow, intrinsic muscle weakness assessments, and EMG to detect spontaneous activities in recipient muscles. Positive results, coupled with normal activity in the PQ muscle (donor), indicate readiness for a mixed surgical technique, combining ulnar nerve transposition, Guyon canal release, and SETS AIN to ulnar motor nerve transfer for comprehensive nerve injury management,25
Despite limitations such as publication bias and heterogeneous data, our review aims to provide a comprehensive analysis of SETS AIN to ulnar nerve transfer literature, emphasizing outcomes and potential research directions. The synthesis of expert feedback with scoping review findings has led to a robust set of primary and secondary outcomes for assessing functional and neurological recovery post-SETS surgery. This updated framework, grounded in solid evidence and clinical insights, prioritizes outcomes that resonate with patients' daily lives, aligning with the patient-centered care paradigm.
Conflicts of Interest
Dr Farzad reports support from Mitacs through the Mitacs Accelerate program. Dr MacDermid reports support from Canada Research Chair in Musculoskeletal Health Outcomes and Knowledge Translation, as well as the Dr James Roth Chair in Musculoskeletal Measurement and Knowledge Translation. Additionally, her work receives funding from a foundation grant from the Canadian Institutes of Health Research (#167284). No benefits in any form have been received or will be received related directly to this article.
Acknowledgments
We would like to extend our gratitude to the Hand Surgery Expert Group for their invaluable insights and expertise contributed to this study: Susan E. Mackinnon, MD, Professor of Plastic and Reconstructive Surgery, Washington University School of Medicine, Division of Plastic and Reconstructive Surgery; Amir R. Kachooei, MD, PhD, Rothman Orthopaedic Institute; Amir R. Farhoud, MD, Assistant Professor, Department of Orthopedic Surgery, Tehran University of Medical Sciences; and Reza S. Kamrani, MD, Department of Orthopedic Surgery, Tehran University of Medical Sciences.
Contributor Information
Tachit Jiravichitchai, Email: tjiravic@uwo.ca.
Hand Surgery Expert Group:
Susan E. Mackinnon, Amir R. Kachooei, Amir R. Farhoud, and Reza S. Kamrani
References
- 1.Lan C.Y., Tien H.Y., Lin Y.T., Hsu C.C., Lin C.H., Chen S.H. Prognosis of traumatic ulnar nerve injuries: a systematic review. Ann Plast Surg. 2019;82(1S suppl 1):S45–S52. doi: 10.1097/SAP.0000000000001727. [DOI] [PubMed] [Google Scholar]
- 2.Baron A., Strohl A. Severe Cubital Tunnel Syndrome: considerations for nerve transfer surgery. Curr Rev Musculoskelet Med. 2020;13(6):708–716. doi: 10.1007/s12178-020-09676-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y., Zhu S. Transfer of a branch of the anterior interosseus nerve to the motor branch of the median nerve and ulnar nerve. Chin Med J (Engl) 1997;110(3):216–219. [PubMed] [Google Scholar]
- 4.Fujiwara T., Matsuda K., Kubo T., et al. Axonal supercharging technique using reverse end-to-side neurorrhaphy in peripheral nerve repair: an experimental study in the rat model. J Neurosurg. 2007;107(4):821–829. doi: 10.3171/JNS-07/10/0821. [DOI] [PubMed] [Google Scholar]
- 5.Barbour J., Yee A., Kahn L.C., Mackinnon S.E. Supercharged end-to-side anterior interosseous to ulnar motor nerve transfer for intrinsic musculature reinnervation. J Hand Surg Am. 2012;37(10):2150–2159. doi: 10.1016/j.jhsa.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Davidge K.M., Mackinnon S.E. The supercharge end-to-side anterior interosseous to ulnar motor nerve transfer for restoring intrinsic function: clinical experience. J Hand Surg. 2013;38(10):e21–e22. doi: 10.1097/PRS.0000000000001514. [DOI] [PubMed] [Google Scholar]
- 7.von Guionneau N., Sarhane K.A., Brandacher G., Hettiaratchy S., Belzberg A.J., Tuffaha S. Mechanisms and outcomes of the supercharged end-to-side nerve transfer: a review of preclinical and clinical studies. J Neurosurg. 2020;134(5):1590–1598. doi: 10.3171/2020.3.JNS191429. [DOI] [PubMed] [Google Scholar]
- 8.Knight S., Miller T.A., McIntyre A., Larocerie-Salgado J., Ross D.C. The hand diagram: a novel outcome measure following supercharged end-to-side anterior interosseous nerve to ulnar nerve transfer in severe compressive ulnar neuropathy. J Hand Ther. Published online October 17, 2023 doi: 10.1016/j.jht.2023.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 10.Levac D., Colquhoun H., O’Brien K.K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westphaln K.K., Regoeczi W., Masotya M., et al. From Arksey and O’Malley and Beyond: customizations to enhance a team-based, mixed approach to scoping review methodology. MethodsX. 2021;8 doi: 10.1016/j.mex.2021.101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 13.Thorkildsen R.D., Kleggetveit I.P., Thu F., Madsen L.M., Bolstad B.J., Røkkum M. Supercharging of the ulnar nerve: clinical and neurophysiological assessment at 2 years for nine proximal injuries. J Hand Surg Eur Vol. 2024 doi: 10.1177/17531934231226174. [DOI] [PubMed] [Google Scholar]
- 14.Chen S.H., Mao S.H., Lan C.Y., et al. End-to-side anterior interosseous nerve transfer: a valuable alternative for traumatic high ulnar nerve palsy. Ann Plast Surg. 2021;86(2S suppl 1):S102–S107. doi: 10.1097/SAP.0000000000002657. [DOI] [PubMed] [Google Scholar]
- 15.Dengler J., Dolen U., Patterson J.M.M., et al. Supercharge end-to-side anterior interosseous-to-ulnar motor nerve transfer restores intrinsic function in cubital tunnel syndrome. Plast Reconstr Surg. 2020;146(4):808–818. doi: 10.1097/PRS.0000000000007167. [DOI] [PubMed] [Google Scholar]
- 16.Doherty C.D., Miller T.A., Larocerie-Salgado J., Byers B.A., Ross D.C. Reverse end-to-side anterior interosseous nerve-to-ulnar motor transfer for severe ulnar neuropathy. Plast Reconstr Surg. 2020;146(3):306e–313e. doi: 10.1097/PRS.0000000000007059. [DOI] [PubMed] [Google Scholar]
- 17.Evans A., Padovano W.M., Patterson J.M.M., et al. Beyond the cubital tunnel: use of adjunctive procedures in the management of cubital tunnel syndrome. Hand (N Y) 2023;18(2):203–213. doi: 10.1177/1558944721998022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLeod G.J., Peters B.R., Quaife T., Clark T.A., Giuffre J.L. Anterior interosseous-to-ulnar motor nerve transfers: a single center’s experience in restoring intrinsic hand function. Hand (N Y) 2022;17(4):609–614. doi: 10.1177/1558944720928482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidge K.M., Yee A., Moore A.M., Mackinnon S.E. The supercharge end-to-side anterior interosseous–to–ulnar motor nerve transfer for restoring intrinsic function: clinical experience. Plast Reconstr Surg. 2015;136(3):344e–352e. doi: 10.1097/PRS.0000000000001514. [DOI] [PubMed] [Google Scholar]
- 20.Baltzer H., Woo A., Oh C., Moran S.L. Comparison of ulnar intrinsic function following supercharge end-to-side anterior interosseous–to–ulnar motor nerve transfer: a matched cohort study of proximal ulnar nerve injury patients. Plast Reconstr Surg. 2016;138(6):1264–1272. doi: 10.1097/PRS.0000000000002747. [DOI] [PubMed] [Google Scholar]
- 21.Head L.K., Zhang Z.Z., Hicks K., Wolff G., Boyd K.U. Evaluation of intrinsic hand musculature reinnervation following supercharge end-to-side anterior interosseous–to–ulnar motor nerve transfer. Plast Reconstr Surg. 2020;146(1):128–132. doi: 10.1097/PRS.0000000000006903. [DOI] [PubMed] [Google Scholar]
- 22.Jarvie G., Hupin-Debeurme M., Glaris Z., Daneshvar P. Supercharge end-to-side anterior interosseous nerve to ulnar motor nerve transfer for severe ulnar neuropathy: two cases suggesting recovery secondary to nerve transfer. J Orthop Case Rep. 2018;8(5):25–28. doi: 10.13107/jocr.2250-0685.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kale S.S., Glaus S.W., Yee A., et al. Reverse end-to-side nerve transfer: from animal model to clinical use. J Hand Surg Am. 2011;36(10):1631–1639.e2. doi: 10.1016/j.jhsa.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 24.Pathiyil R.K., Elzinga K., Umansky D., Midha R. Distal anterior interosseous nerve to ulnar nerve motor branch reverse end-to-side transfer in a case of severe ulnar neuropathy. Neurosurg Focus Video. 2023;8(1) doi: 10.3171/2022.9.FOCVID2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Power H.A., Kahn L.C., Patterson M.M., Yee A., Moore A.M., Mackinnon S.E. Refining indications for the supercharge end-to-side anterior interosseous to ulnar motor nerve transfer in cubital tunnel syndrome. Plast Reconstr Surg. 2020;145(1):106e–116e. doi: 10.1097/PRS.0000000000006399. [DOI] [PubMed] [Google Scholar]
- 26.Tsang P., Larocerie-Salgado J., MacDermid J.C., Miller T.A., Doherty C., Ross D.C. Postoperative management and rehabilitation after the supercharged end-to-side anterior interosseous nerve to ulnar motor nerve transfer: a report of 3 cases. J Hand Ther. 2021;34(3):469–478. doi: 10.1016/j.jht.2020.03.021. [DOI] [PubMed] [Google Scholar]
- 27.Xie Q., Shao X., Song X., et al. Ulnar nerve decompression and transposition with versus without supercharged end-to-side motor nerve transfer for advanced cubital tunnel syndrome: a randomized comparison study. J Neurosurg. 2021;136(3):845–855. doi: 10.3171/2021.2.JNS203508. [DOI] [PubMed] [Google Scholar]
- 28.Dunn J.C., Gonzalez G.A., Fernandez I., Orr J.D., Polfer E.M., Nesti L.J. Supercharge end-to-side nerve transfer: systematic review. Hand (N Y) 2021;16(2):151–156. doi: 10.1177/1558944719836213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pathiyil R.K., Alzahrani S., Midha R. Reverse end-to-side transfer to ulnar motor nerve: evidence from preclinical and clinical studies. Neurosurgery. 2023;92(4):667–679. doi: 10.1227/neu.0000000000002325. [DOI] [PubMed] [Google Scholar]
- 30.Arami A., Bertelli J.A. Effectiveness of distal nerve transfers for claw correction with proximal ulnar nerve lesions. J Hand Surg Am. 2021;46(6):478–484. doi: 10.1016/j.jhsa.2020.10.015. [DOI] [PubMed] [Google Scholar]
- 31.Dy C.J., Mackinnon S.E. Ulnar neuropathy: evaluation and management. Curr Rev Musculoskelet Med. 2016;9(2):178–184. doi: 10.1007/s12178-016-9327-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Graf A., Ahmed A.S., Roundy R., Gottschalk M.B., Dempsey A. Modern treatment of cubital tunnel syndrome: evidence and controversy. J Hand Surg Glob Online. 2022;5(4):547–560. doi: 10.1016/j.jhsg.2022.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burahee A.S., Sanders A.D., Power D.M. The management of failed cubital tunnel decompression. EFORT Open Rev. 2021;6(9):735–742. doi: 10.1302/2058-5241.6.200135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chambers S.B., Wu K.Y., Ross D.C., Gillis J.A. Anterior interosseus to ulnar motor nerve transfers: a Canadian perspective. Hand (N Y) 2023 doi: 10.1177/15589447231174482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liao P.L., Wei C.Y., Letter to the editor: comment on. Chen S.H., et al. End-to-side anterior interosseous nerve transfer: a valuable alternative for traumatic high ulnar nerve palsy (Ann Plast Surg. 2021;86(suppl 1):S102–S107) Ann Plast Surg. 2022;89(3):337. doi: 10.1097/SAP.0000000000003013. [DOI] [PubMed] [Google Scholar]
- 36.Howick J., Phillips B., Ball C., Sackett D., Badenoch D. Oxford centre for evidence-based medicine: levels of evidence. University of Oxford, Centre for Evidence-Based Medicine. 2009;5 https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 [Google Scholar]
- 37.Mukit M., Uygur S., Konofaos P. Supercharge end-to-side anterior interosseous-to-ulnar motor nerve transfer restores intrinsic function in cubital tunnel syndrome. Plast Reconstr Surg. 2022;149(5):1041e–1042e. doi: 10.1097/PRS.0000000000009018. [DOI] [PubMed] [Google Scholar]
- 38.Kahn L.C., Moore A.M. Donor activation focused rehabilitation approach: maximizing outcomes after nerve transfers. Hand Clin. 2016;32(2):263–277. doi: 10.1016/j.hcl.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 39.Nyman E., Nyman T., Rubensson C., Thordstein M. Neuroplasticity following nerve transfer of the anterior interosseous nerve for proximal ulnar nerve injuries. Plast Reconstr Surg Glob Open. 2021;9(7) doi: 10.1097/GOX.0000000000003684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ustün M.E., Oğün T.C., Büyükmumcu M., Salbacak A. Selective restoration of motor function in the ulnar nerve by transfer of the anterior interosseous nerve. An anatomical feasibility study. J Bone Joint Surg Am. 2001;83(4):549–552. doi: 10.2106/00004623-200104000-00009. [DOI] [PubMed] [Google Scholar]