Abstract
Background
Breast cancer remains a leading cause of cancer morbidity and mortality worldwide. In the United States, Black women face significant disparities in screening mammograms, experience higher rates of breast cancer at advanced stages, and are more likely to die from the disease.
Aims
This study aimed to develop and beta-test a virtual health navigation program to enhance breast cancer care within the Black community. We identified barriers to utilizing virtual patient navigators and factors impacting the adoption of virtual navigation for breast cancer information among Black women.
Methods
The vCONET (Virtual Community Oncology Navigation and Engagement) intervention was delivered through the Second Life virtual platform. The informational content was collaboratively developed with community members. Participants engaged in an informational session on risk factors, mammography information, and preventive behaviors. Surveys (n = 18) and focus groups (n = 9) assessed knowledge and insights into perceptions.
Results
Findings revealed a positive impact of the intervention, with participants expressing increased knowledge and willingness to seek further information about breast cancer prevention, and highlighted the engaging nature of the virtual environment, while acknowledging potential technological challenges.
Conclusion
Virtual health navigation shows promise in addressing breast cancer disparities by promoting awareness among Black women. Future efforts should optimize virtual navigation approaches through collaborative engagement for lasting impact, enhancing breast cancer care and equity in communities of color.
Keywords: breast cancer, virtual health navigation, digital health, black women, breast health disparities, community-based intervention
Introduction
Although there have been significant advances in cancer prevention and control, breast cancer remains a significant public health challenge, marked by persistent racial and socioeconomic disparities in cancer mortality. 1 Among the most impacted are Black women, who face substantial disparities across the cancer care continuum, from screening mammograms to treatment and survivorship, with mortality rates disproportionately higher than those of White women. 2 Furthermore, Black women carry a higher burden of triple-negative breast cancer and inflammatory breast cancer, both of which tend to occur at earlier ages and with increased severity than other ethnic groups. 1 Despite a 4% lower incidence rate of breast cancer than White women, Black women have a 40% higher breast cancer mortality rate, the highest of any U.S. racial or ethnic group.1-4
To address these disparities, the primary aim of this study was to develop and establish the usability of a Virtual Community Oncology Navigation and Engagement (vCONET) program. vCONET represents a novel approach that synthesizes proven strategies with innovative communication techniques aimed at enhancing breast health knowledge, awareness, and behavioral intent regarding breast cancer prevention education. Building on the Health Belief Model’s (HBM) emphasis on the importance of perceived benefits and barriers in shaping health behaviors, 5 the vCONET program targets perceptions of breast cancer severity, susceptibility to breast cancer, and the benefits of preventive measures. Additionally, vCONET incorporates patient navigation principles, which have been shown to enhance engagement and bridge healthcare disparities in underserved populations.6-8
The broader adoption of virtual care and telehealth, accelerated by the COVID-19 pandemic, has opened new avenues for health interventions 9 like vCONET. Therefore, we administered the intervention using a virtual platform to facilitate culturally sensitive health communication, education, and information dissemination. 10 Through this intervention, we sought to significantly contribute to the growing body of knowledge on community-centered, virtual health navigation and its potential in improving breast cancer outcomes for underserved populations.
Materials and Methods
Study Objectives
The study aimed to evaluate vCONET’s role in enhancing breast cancer awareness, screening behaviors, and health equity among Black women. The specific objectives were: (1) to identify perceived barriers in using virtual patient navigators, and (2) to understand factors influencing the adoption of a virtual navigator model for breast cancer screening among Black women. These objectives were framed within the Health Belief Model, emphasizing the perceived barriers and benefits to breast cancer screening and preventive health behaviors. 5
Program Description: Virtual Community Oncology Navigation and Engagement (vCONET)
Virtual Community Oncology Navigation and Engagement is an educational platform that was designed to address the distinct needs and experiences of Black women in the area of breast cancer awareness and prevention. At the core of its educational framework was the emphasis on the importance of regular mammography screenings, highlighting the benefits of early detection and the urgency of early interventions. The program also provided guidance on preventive strategies against breast cancer, including the adoption of a balanced diet and consistent exercise regimen. An essential component was the promotion of breast self-examinations, informing participants of the importance of regular self-checks to monitor any potential changes. Additionally, vCONET directly addressed the disparities faced by Black women in the context of breast cancer, aiming to increase awareness through targeted education and advocate for equitable access to essential screening resources. By leveraging a combination of collaborative content development, an engaging virtual platform, and a focus on community-specific needs, vCONET aims to positively influence participants’ awareness and intentions towards breast cancer screening and prevention. The collaborative process behind vCONET involved integrating community expertise and healthcare professionals’ insights to develop culturally relevant content addressing the specific needs of Black women in breast cancer awareness and prevention. This included input from oncologists, public health experts, and community advocates.
The Health Belief Model (HBM) was used as the primary analytical framework for our study. This model guided our interpretation by focusing on participants’ perceived susceptibility to breast cancer and their perceptions of the severity of the disease, the benefits they associated with preventive actions like mammography, and the barriers they faced in accessing cancer screening services. Each of these HBM components was used to categorize and understand the responses, facilitating a structured analysis of how beliefs influence behavior. For example, discussions about personal and community experiences with breast cancer were examined for cues that potentially encourage proactive health behaviors, such as seeking mammography screening or engaging with health education. This approach allowed us to systematically explore and document the effectiveness of the vCONET program in addressing these beliefs and modifying participant behavior towards breast cancer prevention and awareness.
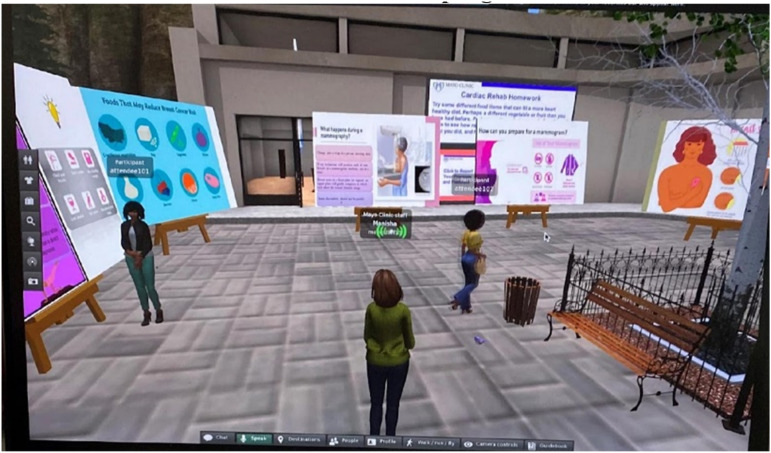
Virtual Community Oncology Navigation and Engagement was hosted on the Second Life computer program, offering participants an immersive virtual environment as depicted in Figure 1. Within this digital setting, participants were guided through the platform and its functionalities by the first author during an informational session. The implementation session was comprehensive, detailing breast cancer risk factors that are particularly relevant to Black women, providing insights into mammography, and suggesting practical measures to lower associated risks. The content presented was developed based on the principles of community engagement 11 and was reviewed by community members, medical experts, and leaders, whose feedback was incorporated into the final version for high potential impact. The program aimed to provide both knowledge and promote preventive behaviors related to breast cancer.
Figure 1.
Snapshot of vCONET (virtual community oncology navigation and engagement) intervention session within second life program.
Study Design and Framework
Our research utilized an explanatory sequential mixed-methods design. This involved a quantitative phase where pre- and post-program surveys were administered to measure changes in knowledge, attitudes, and behaviors towards breast cancer screening. The qualitative phase followed, with focus group discussions to delve deeper into the participants’ experiences. These discussions were facilitated by the first author, a female postdoctoral researcher at the time, and holds a Doctor of Public Health with extensive training in community engagement, public health and qualitative methodologies. All sessions were audio-recorded and transcribed verbatim for analysis. The HBM guided our approach across both phases, enriching our interpretation of how participants’ beliefs and attitudes might influence their health behaviors.
Quantitative Phase
We conducted pre- and post-program surveys to measure participants’ knowledge, attitudes towards breast cancer, and their behavioral intent regarding breast cancer screening. These surveys, conducted before and after participating in the vCONET program, served as foundational tools for gathering baseline data and collecting feedback on participants’ perceptions post-participation. The core measures for the surveys were adapted from existing literature and validated questionnaires.12-14
Qualitative Phase
Building on the insights from the quantitative findings, focus group discussions were conducted to explore participants’ experiences with the vCONET program. These discussions sought to understand participants’ perceptions of breast cancer risks and the program’s role in addressing health disparities. This study’s reporting adheres to the Consolidated criteria for reporting qualitative research (COREQ) guidelines. 15
Participant Recruitment, Demographics and Study Setting
Participants were Black or African American women aged 18 or older with sufficient English proficiency. The inclusion criteria also required participants to have basic reading skills to effectively interact with the intervention materials and surveys. For recruitment, we utilized snowball sampling methods, 16 capitalizing on existing networks and community event participation to reach potential participants. This strategy enabled us to connect with a diverse group, approaching individuals via phone, email, and in-person based on existing relationships and prior community engagement.
Initially, we conducted data collection in person at a community event that promoted breast cancer awareness, leveraging existing relationships with local community organizations. Prior to the event, we engaged in discussions with these organizations to explain the research objectives and express our commitment to building a foundation for future collaboration. The community event itself allowed for direct and meaningful interactions with participants. However, due to the onset of the COVID-19 pandemic variants, the study was adapted to a remote format after the initial implementation in October 2021. This required participants to access the vCONET program via their personal internet connections at home, ensuring the safety of all involved.
Ethical approval was granted by the Mayo Clinic Institutional Review Board (Approval No. 21-010111) on October 8, 2021. All participants provided verbal informed consent.
Data Collection Strategy and Analysis
To measure the impact of the vCONET program, our study employed a mixed-methods approach, integrating both quantitative surveys and qualitative focus groups to collect data. This strategy allowed for a nuanced understanding of the program’s effects on participants’ knowledge, attitudes, and behaviors towards breast cancer screening.
We used both pre- and post-intervention surveys to assess the vCONET program. The baseline survey collected initial data on participants’ knowledge and attitudes towards breast cancer and their prior engagement with screening activities. Immediately following their engagement with the vCONET program via the Second Life platform, participants were invited through the post-assessment survey to express their views on using the program, intention for future screening, as well as interest in joining focus group discussions. These discussions aimed to examine topics in more depth, such as breast cancer awareness, the effectiveness of the program, and community engagement in breast cancer prevention efforts. This approach not only measured the program’s immediate impact but also facilitated a richer understanding of participant experiences.
Quantitative Phase
The baseline and post-intervention surveys were designed to assess participants’ self-reported knowledge, attitudes, and behaviors regarding breast cancer and screening practices. The baseline survey included questions about participants’ demographics, health insurance status, regular medical care, history of mammography screening, awareness of clinical trials, and perceived breast cancer risk. Questions were a mix of Yes/No, multiple-choice, and Likert scale responses to gather comprehensive data on initial conditions.
The post-intervention survey focused on participants’ experiences with the vCONET program and its impact on their intentions towards breast cancer prevention. It included questions about satisfaction with the virtual Second Life platform, the perceived usefulness of the information received, comfort using the program, and intentions to undergo mammography screening within the next year. The post-survey also assessed difficulties encountered, preferences for reviewing information in different settings, and overall feedback on the program.
We used descriptive statistics to analyze the self-reported survey data, focusing on summarizing baseline responses and assessing post-intervention perceptions. This method allowed us to evaluate participants’ self-reported awareness and behavioral intentions related to breast cancer screening. These findings provide insights into the program’s perceived efficacy in meeting the study’s objectives.
Qualitative Phase
Following their participation in the vCONET program, interested participants were invited to voluntary focus group sessions, resulting in a total of 9 participants. Using a semi-structured guide, participants shared their experiences, specifically highlighting usability, effectiveness, and challenges of the virtual platform. Questions explored participants’ general experiences with health information sources, particularly how they receive and perceive breast cancer information. Discussions also probed community-specific needs, asking participants to suggest how breast cancer messages should be tailored and delivered to Black women in their community, focusing on the most relevant and engaging content and delivery methods. Audio recordings of these discussions, complemented by field notes, were utilized to capture the nuances of the conversations.
Thematic analysis process 17 was conducted by 2 researchers who independently reviewed the focus group data to identify key themes derived from the data. Discrepancies in coding were resolved through consensus to ensure thematic consistency. This approach allowed for the emergence of important themes from the data. NVivo software supported data organization, which contributed to an efficient analysis. We also included responses to open-ended survey questions in the qualitative analysis, adding depth to our findings. As an exploratory study, data saturation was reached across the 3 focus groups, demonstrating a thorough exploration of the topic and ensuring that the emergent themes comprehensively represented the participants’ experiences and the impact of the intervention. These findings were analyzed using the HBM dimensions of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. This analysis explores themes within these dimensions and demonstrates how these data reflect the target population’s experiences and the intervention’s impact.
Results
In this study, we recruited a diverse group of 18 participants, details of which can be seen in Table 1. Participants predominantly identified as African American (70%) from urban areas. The age distribution was broad, ranging from 18 to over 70 years, with a significant proportion (44%) aged between 50 and 69 years. Educational levels among participants varied, with a notable 56% holding advanced degrees. Employment statuses reflected a diverse workforce, with 33% employed full-time and 22% retired, highlighting varied economic backgrounds. In terms of socio-economic status, household incomes ranged from below $20,000 to over $60,000, demonstrating substantial diversity. Regarding healthcare access and practices, half of the participants had public health insurance, however, only a quarter reported having a mammography screening within the past year. Awareness of clinical trials related to breast cancer was relatively low at 38%, with 25% informed about their breast cancer risk by healthcare providers. Ethical approval for this study was
Table 1.
Participant Characteristics for the vCONET (Virtual Community Oncology Navigation and Engagement) Program.
| Characteristic | Percentage/Details |
|---|---|
| Total participants | 18 |
| Age distribution | 18-29 (15%) |
| 30-39 (10%) | |
| 40-49 (20%) | |
| 50-59 (25%) | |
| 60-69 (20%) | |
| 70-79 (8%) | |
| 80+ (2%) | |
| Ethnicity | African-American (70%) |
| African (10%) | |
| Caribbean (10%) | |
| Other (10%) | |
| Education level | Less than high school (5%) |
| High school (20%) | |
| Some college (25%) | |
| College degree (30%) | |
| Postgraduate (20%) | |
| Marital status | Single (30%) |
| Married (40%) | |
| Divorced (20%) | |
| Widowed (10%) | |
| Employment status | Full-time (33%) |
| Part-time (20%) | |
| Retired (22%) | |
| Unemployed (10%) | |
| Disability (15%) | |
| Residential area | Urban (100%) |
| Household income | Below $20,000 (22%) |
| $20,000-39,999 (25%) | |
| $40,000-59,999 (20%) | |
| $60,000-79,999 (15%) | |
| $80,000-99,999 (10%) | |
| $100,000+ (8%) | |
| Health insurance | Public (50%) |
| Private (40%) | |
| None (10%) | |
| Regular medical care | Has a regular doctor (80%) |
| Mammography screening | Had a screening in the last year (25%) |
| Awareness of clinical trials | Aware (38%) |
| Risk awareness | Previously informed about breast cancer risk (25%) |
The integration of pre- and post-intervention survey findings with insights from virtual focus group discussions provided a holistic understanding of the vCONET program’s impact. These combined results shed light on the program’s effectiveness, technological challenges, and the pivotal role of tailored information in advancing breast cancer care in marginalized communities.
Quantitative Findings
The vCONET program, delivered through the Second Life platform, significantly enhanced participants’ awareness and screening behaviors for breast cancer. Initial surveys distributed to eighteen participants showed that only 25% of participants had undergone mammography screening in the past year, despite most having health insurance. Post-intervention, 94% found the program beneficial, reflecting effective knowledge transfer. Notably, 77% of participants reported they intended to undergo mammography screening within the next year rose and 75% planned to seek further information on breast cancer prevention and early detection.
Participant satisfaction with the Second Life platform was high, with 88% expressing satisfaction, indicating the platform’s effectiveness in engaging users. Some participants provided feedback on improving the accessibility and user-friendliness of the technology. Despite these challenges, 94% of participants were willing to use the program again, underscoring its perceived value and acceptance.
These results demonstrate the vCONET program’s success in improving knowledge and proactive health behaviors among participants, highlighting the potential of virtual platforms for delivering impactful health education.
Focus Group Insights
After participating in the intervention, focus groups were conducted virtually to gain valuable insights into participants’ experiences and perceptions. The analysis revealed key themes directly derived from participant discussions, ensuring the representativeness and depth of our findings. Participant quotations are used throughout to illustrate these themes, enhancing the transparency and relatability of our results. Focus group discussions revealed several prominent themes that emphasized the program’s influence on breast cancer awareness and knowledge among Black women. These themes were grouped according to the Health Belief Model dimensions of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. Notably, the influence of the virtual environment, the balance between technological excitement and challenges, the significance of tailored knowledge and constant awareness, and the journey of trust-building and persistence in healthcare contexts within Black communities emerged at principal themes as demonstrated below and in Table 2. All names mentioned in the following section are pseudonyms.
(1) Perceived Susceptibility: Many participants reported an increased awareness of their personal risk of breast cancer. One participant stated, “I realized that my family history puts me at higher risk.” This increased awareness was further emphasized by the theme of Tailored Knowledge and Constant Awareness. Emily, a participant, noted the heightened impact of breast cancer within the Black community. Simultaneously, Jessica stressed the continuous need for health reminders, equating breast cancer prevention to routine health checks: “Just as important as checking your blood pressure or checking your blood sugar.” These insights illustrate how the program effectively heightened participants’ perceived susceptibility by providing personalized and relevant information.
(2) Perceived Severity: Participants acknowledged the serious consequences of breast cancer. For example, 1 participant commented, “I understand now how crucial early detection is because breast cancer can be very aggressive.” This understanding was enhanced by the theme of Virtual Interaction’s Impact. The immersive nature of the virtual platform significantly contributed to participants’ comprehension of the severity of breast cancer. Julie remarked, “I like the virtual world. It was way more engaging,” while Sarah acknowledged that her involvement with the program “…made me open to researching [breast cancer] way more.” These remarks suggest that the engaging nature of the virtual platform offered a distinct advantage in educating participants about the severity of the disease.
(3) Perceived Benefits: There was a notable increase in participants’ recognition of the benefits of regular mammograms and other preventive measures. One participant noted, “Regular screenings can really make a difference in catching cancer early.” This theme was also supported by the positive feedback under the theme of Virtual Interaction’s Impact , which reinforced the benefits of preventive actions. Participants’ increased recognition of these benefits highlights the program’s effectiveness in promoting proactive health behaviors.
(4) Perceived Barriers: Despite recognizing the benefits, participants also highlighted barriers such as fear and accessibility. One participant admitted, “I’m scared of what they might find,” while another mentioned, “Getting to the clinic is a challenge.” This was further explored under the theme of Tech-Curve Balance. Participants acknowledged the dual-edged nature of the virtual environment, which brought excitement and novelty but also posed a learning curve for those less accustomed to technological platforms. Laura noted, “Most people that are not technology-savvy might take them a little time to grasp it. But I think once they do it will be something exciting.” This duality hints at the need to ensure technological innovations remain accessible to all, regardless of prior tech exposure.
Table 2.
Qualitative Themes for vCONET.
| Health Belief Model Dimension | Theme | Description | Participant Quote(s) |
|---|---|---|---|
| Perceived susceptibility | Tailored knowledge and constant awareness | Participants emphasized the importance of tailored information specific to Black women and the need for repetitive dissemination. | “I think just a simple fact that it [breast cancer] affects us [black women] way more than it does other people. I don’t think that’s like commonly known because when I went into the [virtual program] I was like ‘wow are you serious? Wow how did I not know this? Okay this truly affects me.’” – Emily |
| “Repetition repetition; information information information. Say for instance during national breast cancer month Oct right everything is on TV everything is on commercials everything is on things… and then comes Nov, Dec, Jan, and it’s not. So again trying to figure out how to make it sound just as important to do preventive mammogram is just as important as checking your blood pressure or checking your blood sugar things like that.” – Jamie | |||
| Perceived severity | Virtual interaction’s impact | Participants recognized the profound influence of the virtual program on awareness and engagement, surpassing traditional methods. | “I like the just the virtual world. Like it was way more engaging and just actually going around and viewing the information was just way more intriguing than just going to a plain old PowerPoint.” – Julie |
| “Before I did this study I thought it was just going to the doctors you need a mammogram you need this you need that. After going through this [program] I was like ‘oh my god I didn’t know this. Oh my god are you serious? Is this this high for black women?’ So yeah normally just the doctors but this has definitely made me open to researching it way more.” – Sarah | |||
| Perceived benefits | Virtual interaction’s impact | There was a notable increase in participants’ recognition of the benefits of regular mammograms and other preventive measures. | “Regular screenings can really make a difference in catching cancer early.” – Janette |
| Perceived barriers | Tech-curve balance | Participants acknowledged both the potential and challenges of virtual navigation for individuals less technologically inclined. | “Most people that are not technology-savvy, it might take them a little time to grasp it. But I think once they do it will be something exciting.” – Laura |
Additionally, participants recognized the existing trust deficit between the Black community and healthcare establishments, leading to the theme of Trust-Building Journey and Persistence . Participants stressed the importance of continuous and sincere outreach by healthcare providers. Jessica and Emily highlighted that trust-building is a journey requiring persistence. Jessica remarked, “It’s important for health providers to keep reaching out and showing they care,” while Emily added, “Consistent information and support build trust over time.” These insights highlight the critical nature of health information dissemination and the relentless efforts needed to foster genuine trust within the community.
In summary, the focus group discussions provided nuanced insights into the potential and challenges of the program. The themes emphasized the importance of specifically tailored information for Black women, the imperative nature of constant health communication, and the enduring effort required to foster trust in Black community healthcare scenarios. The integration of these themes within the Health Belief Model dimensions of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers offers a comprehensive understanding of how the vCONET program influenced participants’ health behaviors and perceptions.
Discussion
This study aimed to explore the potential of virtual health navigation for breast cancer survivors in communities of color, specifically addressing disparities in cancer care. By emphasizing cultural sensitivity and inclusivity, the tailored virtual navigation sought to bridge the gap in breast cancer inequities through accessible information dissemination. The results demonstrated a positive impact on breast cancer awareness and knowledge among Black women, with participants showing increased awareness of breast cancer risk factors and screening practices. This led to a greater readiness to seek knowledge that aids in informed decision-making about prevention and early detection. The virtual environment proved both engaging and intriguing, providing an immersive experience that positively contributed to participants’ awareness and engagement.
Our analysis revealed several key findings: First, participants exhibited an increased understanding of breast cancer and its significance in screening practices. Second, there were notable positive shifts in attitudes towards breast cancer prevention, accompanied by intentions to engage in screening behaviors. Third, the provision of personalized, culturally sensitive information was found to effectively address the unique needs of the community. Our findings also highlighted the various dimensions of the Health Belief Model, including perceived susceptibility, severity, benefits, and barriers, and how these dimensions influenced participants’ attitudes and behaviors. While participants reported high satisfaction with the program, the feedback also highlighted opportunities for enhancing technology access and digital literacy, suggesting future improvements for broader accessibility.
The study also recognized potential challenges for individuals who may be less familiar with technology. While some participants expressed excitement about the possibilities of virtual navigation, others recognized the need for ongoing support to help individuals adapt to the virtual environment. Addressing these challenges is vital to ensure equitable access to breast cancer education and screening for all Black women, regardless of their comfort level with technology.
This study addresses a critical gap in the literature by examining the impact of virtual health navigation specifically tailored to the needs of Black women in relation to breast cancer. 18 While prior research acknowledges racial and ethnic disparities in breast cancer care, 19 there is limited information on the implementation and efficacy of virtual navigation models, particularly through more immersive virtual platforms. 20 This innovative approach aligns with the increasing interest in immersive technology-based patient advocacy and its multifaceted benefits for in the healthcare sector. 21
The community-engaged nature of vCONET is also a key strength. Throughout the study, we sought input and insights from community members, both during the program’s design phase and afterward to gather feedback. This collaborative approach ensured that vCONET was tailored to meet the specific needs and preferences of the community. Our findings highlight the importance of consistently disseminating information, especially through virtual tools, to reinforce the significance of preventive measures, such as mammograms, throughout the year. Past studies which have incorporated Second Life as a component of health communication have also shown promise of virtual delivery of health messages, 22 though further research is warranted to evaluate long-term effectiveness and address access barriers among marginalized populations.
Our study also adds to the growing body of literature by demonstrating the potential of virtual health navigation, observed in past studies and reviews highlighting virtual environments in different aspects of the cancer continuum.23,24 Thus, our findings offer valuable insights into the role of virtual health navigation in addressing breast cancer disparities among communities of color. This highlights the innovative use of virtual technology to promote health behavior change and emphasizes the need for further exploration and application in diverse healthcare settings.
In addition to these broader implications, our analysis also provided insights into the specific experiences of different age groups within the Black community. Interestingly, participants’ ages ranged from 18 to 79 years, with the majority falling within the 50-69 age group. This age distribution allowed for insights into how different age groups within the Black community responded to the virtual health navigation program. Younger participants showed familiarity and comfort with technology, leading to positive engagement with the virtual platform and increased breast cancer awareness. Initially hesitant, older participants quickly became proficient in navigating the virtual environment of Second Life, controlling their avatars effectively and thus challenging age-related stereotypes about adaptation to virtual capabilities. 25
As multiple age groups demonstrated increased intention for mammograms and seeking breast cancer information post-intervention, virtual navigation holds promise for engaging different age demographics in breast cancer care and prevention. We found that addressing technological barriers and literacy from the start, such as implementing a program orientation, is crucial for equitable access to virtual programs, which is consistent with another study’s findings on Second Life usage in healthcare settings. 26 Future interventions should consider community-specific preferences to improve breast cancer outcomes across all age groups in the Black community.
Limitations
This study had certain limitations. First, the literacy level criterion may have introduced a bias, as most participants had higher levels of education. Second, the study primarily focused on participants’ intentions to undergo breast screening rather than their actual behaviors, leaving room for further exploration of the factors influencing the transition from intention to action. Additionally, the virtual format of the program might have restricted participation to individuals with reliable internet access, potentially excluding those from different socioeconomic backgrounds or areas with limited internet connectivity. Although efforts were made to address these challenges by providing support, future research should consider these design limitations. To further test efficacy of a program like vCONET, future studies should also aim to expand and diversify the participant pool and develop strategies to bridge the gap between intention and action in healthcare decision-making processes.
Conclusion and Future Implications
Despite the limitations, this study highlights the contribution of vCONET as a tool for virtual health navigation for breast cancer care in communities of color. The community-based design and focus on addressing disparities through virtual technology highlight the potential of virtual navigation as an effective and accessible avenue for improving cancer care outcomes in underserved populations. As technology continues to advance, virtual health navigation can play a critical role in advancing health equity and promoting cancer prevention among vulnerable communities. By incorporating community input and leveraging immersive virtual platforms, we demonstrated the effectiveness of virtual navigation in enhancing breast cancer awareness, knowledge, and engagement among underserved populations.
Participants indicated that a more mobile-friendly application would significantly increase accessibility and reach. Addressing these technological challenges is critical to ensuring equitable access and participation in virtual navigation programs. Future research should consider developing and utilizing more adaptable and user-friendly technological platforms to overcome these barriers. This approach could enhance engagement and accessibility, making it easier for a broader range of participants to benefit from virtual health navigation. By leveraging advanced and versatile technology, we can better meet the diverse needs of underserved communities and further promote health equity.
In addition to the present findings, this study carries important future implications for advancing cancer care and health equity. The integration of virtual patient navigation as a tailored and culturally sensitive approach has the potential to be implemented on a broader scale, reaching marginalized communities and reducing disparities in breast cancer outcomes. Future studies should focus on expanding the reach of virtual navigation programs to include a more diverse and representative sample of communities of color, as well as exploring the long-term effects of such interventions on health behaviors and cancer-related outcomes. Additionally, ongoing efforts should be made to address technological accessibility concerns and provide support and training to ensure equitable access to virtual platforms. Making information available through multiple virtual modalities that are most preferable to the community would help with this. By continuously building on the success of virtual navigation, healthcare professionals can work towards creating a more inclusive and effective approach to breast cancer prevention and care, ultimately contributing to improved health outcomes and reduced disparities in communities of color.
Supplemental Material
Supplemental Material for Addressing Breast Cancer Equity Through Virtual Community Oncology Navigation and Engagement (vCONET) by Manisha Salinas and Folakemi T. Odedina in Journal of Cancer Control.
Supplemental Material for Addressing Breast Cancer Equity Through Virtual Community Oncology Navigation and Engagement (vCONET) by Manisha Salinas and Folakemi T. Odedina in Journal of Cancer Control.
Acknowledgments
We would like to acknowledge the staff, community members, and coordinators who contributed to this study. Special thanks to Brian Kaihoi for his assistance in integrating vCONET into Second Life and to the American Legion Post 194 for hosting the community space for part of our data collection and recruitment. Finally, we are grateful to all the study participants for their valuable contributions.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
Ethical Statement
Ethical Approval
Ethical approval was granted by the Mayo Clinic Institutional Review Board (Approval No. 21-010111) on October 8, 2021.
Informed Consent
Informed consent was obtained from all subjects involved in the study.
ORCID iD
Manisha Salinas https://orcid.org/0000-0002-6345-6385
References
- 1.Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat. 2019;177(3):537-548. doi: 10.1007/s10549-019-05340-7. [DOI] [PubMed] [Google Scholar]
- 2.Yedjou CG, Sims JN, Miele L, et al. Health and racial disparity in breast cancer. In: Breast Cancer Metastasis and Drug Resistance: Challenges and Progress. Berlin, Germany: Springer; 2019:31-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breast Cancer Prevention Partners . African American Women and Breast Cancer. San Francisco, CA: Breast Cancer Prevention Partners. https://www.bcpp.org/resource/african-american-women-and-breast-cancer/ (2020). [Google Scholar]
- 4.American Cancer Society . Cancer Facts & Figures for African American/Black People|More Black Women Die From Breast Cancer Than Any Other Cancer. Atlanta, GA: American Cancer Society; 2022. https://www.cancer.org/research/acs-research-news/facts-and-figures-african-american-black-people-2022-2024.html [Google Scholar]
- 5.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175-183. [DOI] [PubMed] [Google Scholar]
- 6.Fouad MN, Acemgil A, Bae S, et al. Patient navigation as a model to increase participation of African Americans in cancer clinical trials. J Oncol Pract. 2016;12(6):556-563. doi: 10.1200/JOP.2015.008946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghebre RG, Jones LA, Wenzel JA, Martin MY, Durant RW, Ford JG. State-of-the-science of patient navigation as a strategy for enhancing minority clinical trial accrual. Cancer. 2014;120(S7):1122-1130. doi: 10.1002/cncr.28570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reuland DS, Brenner AT, Hoffman R, et al. Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: a randomized clinical trial. JAMA Intern Med. 2017;177(7):967-974. doi: 10.1001/jamainternmed.2017.1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679-1681. [DOI] [PubMed] [Google Scholar]
- 10.Dixit N, Rugo H, Burke NJ. Navigating a path to equity in cancer care: the role of patient navigation. Am Soc Clin Oncol Educ Book. 2021;41:1-8. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention . Principles of Community Engagement. 2nd ed. Washington, DC: Department of Health and Human Services, National Institutes of Health, Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry, Clinical and Translational Science Awards; 2011. NIH publication 11-7782. [Google Scholar]
- 12.Merz EL, Riley NE, Malcarne VL, Sadler GR. Clinical trials-related knowledge, attitudes, and behaviors among Black and latina women: a randomized controlled trial of the women united: clinical trials and the fight against breast cancer program. J Cancer Educ. 2022;37(3):874-881. [DOI] [PubMed] [Google Scholar]
- 13.National health interview survey. https://www.cdc.gov/nchs/nhis/2024nhis.htm
- 14.Health information national trends survey. https://hints.cancer.gov/
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed] [Google Scholar]
- 16.Biernacki P, Waldorf D. Snowball sampling—problems and techniques of chain referral sampling. Socio Methods Res. 1981;10:141-163. [Google Scholar]
- 17.Saldaña J, Omasta M. Qualitative Research: Analyzing Life. Thousand Oaks, CA: Sage Publications; 2016. [Google Scholar]
- 18.Bayard S, Fasano G, Gillot T, et al. Breast cancer disparities and the digital divide. Curr Breast Cancer Rep. 2022;14(4):205-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gehlert S, Hudson D, Sacks T. A critical theoretical approach to cancer disparities: breast cancer and the social determinants of health. Front Public Health. 2021;9:674736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Offodile AC, Seitz AJ, Peterson SK. Digital health navigation: an enabling infrastructure for optimizing and integrating virtual care into oncology practice. JCO Clin Cancer Inform. 2021;5:1151-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ullah H, Manickam S, Obaidat M, et al. Exploring the potential of metaverse technology in healthcare: applications, challenges, and future directions. IEEE Access. 2023;XX:1-10. [Google Scholar]
- 22.Cowdery J, Kindred J, Michalakis A, Suggs LS. Promoting health in a virtual world: impressions of health communication messages delivered in second life. First Monday. 2011;16(9):2857. [Google Scholar]
- 23.Scates D, Dickinson JI, Sullivan K, Cline H, Balaraman R. Using nature-inspired virtual reality as a distraction to reduce stress and pain among cancer patients. Environ Behav. 2020;52(8):895-918. [Google Scholar]
- 24.Yazdipour AB, Saeedi S, Bostan H, Masoorian H, Sajjadi H, Ghazisaeedi M. Opportunities and challenges of virtual reality-based interventions for patients with breast cancer: a systematic review. BMC Med Inf Decis Making. 2023;23:17. doi: 10.1186/s12911-023-02108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mariano J, Marques S, Ramos MR, et al. Too old for technology? Stereotype threat and technology use by older adults. Behav Inf Technol. 2022;41(7):1503-1514. [Google Scholar]
- 26.Weiner E, Trangenstein P, McNew R, Gordon J. Using the virtual reality world of Second Life to promote patient engagement. Stud Health Technol Inf. 2016;225:198-202. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Addressing Breast Cancer Equity Through Virtual Community Oncology Navigation and Engagement (vCONET) by Manisha Salinas and Folakemi T. Odedina in Journal of Cancer Control.
Supplemental Material for Addressing Breast Cancer Equity Through Virtual Community Oncology Navigation and Engagement (vCONET) by Manisha Salinas and Folakemi T. Odedina in Journal of Cancer Control.