Abstract
Objective
Rapid and effective reduction is difficult for minimally invasive plate osteosynthesis (MIPO) surgery. This study aims to introduce a bidirectional rapid reductor (BRR) designed to assist in the reduction during MIPO surgery for proximal humeral fractures (PHFs).
Methods
This retrospective study was conducted between June 2021 and February 2022 in the Third Hospital of Hebei Medical University, involving patients diagnosed with PHFs. A detailed technical approach of BRR in MIPO surgery was described, and the patients' outcomes based on postoperative radiographic results including x‐ray postoperative follow‐up, and clinical outcome parameters including visual analogue scale (VAS) and constant‐Murley score at last follow‐up were reported.
Results
A total of 12 patients were included in this study, comprising three males and nine females, with an average age of 67.58 years. The mean operative time was 70.92 min (range 63–80 min). The mean blood loss was 102.27 mL (range 50–300 mL). The mean VAS and constant‐Murley scores at final follow‐up were 0.33 and 88, respectively. All patients had their fractures healed without secondary displacement at last follow‐up. One patient experienced shoulder stiffness post‐operation. There were no adverse events or complications following the use of this technique, such as acromion fracture, nerve or blood vessel injury.
Conclusion
The BRR can assist MIPO for good reduction of PHFs. However, the efficacy should be validated with a large‐sample randomized controlled trial and longer follow‐up.
Keywords: Bidirectional rapid reductor, Minimally invasive surgical procedures, Shoulder fractures
This study suggests that the bidirectional rapid reductor is effective in the minimally invasive plate osteosynthesis (MIPO) treatment of proximal humeral fractures (PHFs). This device not only aids in achieving or maintaining reduction during MIPO surgery but also reduces operation and exposure times.

Introduction
Proximal humeral fractures (PHFs) rank as the second most common fracture of the upper extremity, constituting 5% of all fractures, and have surged to become the third most common fragility fracture among the elderly in the last two decades. 1 , 2 PHFs with significant displacement or instability following reduction are often treated surgically. 3 There are many surgical strategies that were proven to be clinically effective, including open reduction–internal fixation (ORIF), minimally invasive plate osteosynthesis (MIPO), intramedullary nails, and primary arthroplasty. 4 , 5 , 6 However, the optimal surgery technique for treatment for PHFs remains controversial. 7 The trend is leaning towards minimally MIPO surgery, because of its minimal trauma, reduced bleeding, expedited recovery, lower complication rates, and improved clinical outcomes. 8 , 9
Paradoxically, just as small incisions with MIPO, it is more difficult to achieve a satisfactory reduction of fracture sites. The primary procedure in reducing PHFs is to restore the alignment of the humeral head and shaft. This is typically achieved under X‐ray fluoroscopy guidance, where two doctors apply adverse traction to the upper limb and temporarily fix fracture sites with Kirschner wires. 8 , 9 In cases of varus fractures that are challenging to reduce, most scholars often use the joystick technique and elevators for assistance. 10 , 11 , 12 , 13 Borer et al. applied Kirschner wires or hooks to pry and pull the humeral head. 10 , 11 , 12 , 13 However, these manual reduction techniques have limitations in force and sustainability, which can sometimes be insufficient for acceptable reduction. Additionally, the instruments assisting in humeral head reduction may cause secondary fractures in elderly patients with osteoporosis. To achieve a satisfactory reduction of fracture sites, it is inevitably necessary to extend incision, longer operation and radiation time. 14 The higher rate of axillary nerve injury is another disadvantage of routine MIPO surgery. 4
The bidirectional rapid reductor (BRR) which was designed by our team, has previously found applications in MIPO surgeries for tibial plateau fractures and distal femoral fractures, 15 , 16 , 17 and it can achieve a better clinical outcome than ORIF surgery. Yet its utilization in MIPO for PHFs remains unexplored. Therefore, the purposes of this study were to: (i) introduce a novel surgical technique to assist in achieving accurate and convenient reduction for PHFs patients; and (ii) summarize tips and tricks which may be beneficial for orthopedists.
Methods
Study Population
This was a retrospective cohort study of consecutive patients who underwent MIPO surgery using BRR for proximal humeral fracture at our institution between June 2021 and February 2022. The inclusion criteria were: (i) unilateral, acute and closed fracture; (ii) consent for MIPO treatment assisted by BRR; (iii) older than 18 years old; (iv) diagnosed with PHFs by X ray or CT; and (v) no obvious surgical contraindications. The exclusion criteria were: (i) acromial deformity or pathological fractures; (ii) concurrent ipsilateral proximal ulna fractures and acromioclavicular dislocation; (iii) significant pre‐existing degenerative joint disease; (iv) systemic or local infection; and (v) patients requiring intensive care or those with severe systemic comorbidities, such as severe osteoporosis, hypertension, diabetes and heart disease.
Before surgery, all patients received treatment with a shoulder abduction brace to maintain primary alignment and alleviate pain. Definitive treatment was postponed until improvement in soft tissue conditions was observed. Full approval from the Ethics Committee of the third hospital of Hebei Medical University (S2020‐016‐1) was received for this study, and all enrolled subjects confirmed their informed consent for participation.
Surgical Protocol
Positioning
Patients were in supine position on a radiolucent operating table with the neck slightly turned to the opposite side of the affected limb. Disinfectant preparation covered the area from shoulder and neck to the distal end of the upper extremity on the injured side, including the iliac crest.
Closed Reduction and Internal Fixation with BRR
First, surgeons assemble the BRR (WEGO, Wei Hai city, PR China). The BRR (Figure 1) is composed of two carbon connecting rods, one folding scaffold and two traction bows. The olecranon and acromion of the ulna were selected for distal and proximal traction positions, respectively. To achieve the purpose of accurate location, a 5 mL syringe needle was inserted vertically into the acromion, and a 2.5 mm K‐wire was inserted in acromion horizontally in AP direction. Another 2.5 mm K‐wire was then drilled into the olecranon, with two K‐wires attached to the distal and proximal traction arches. And then, the two carbon connecting rods were connected to the traction bow and folding scaffold. By rotating the handle counterclockwise, a traction force in the opposite direction was generated along the vertical line of the upper limb at the fracture site. With the increasing traction force, the joint space widened, the tension of muscles, skin, and other soft tissues around the shoulder joint gradually increased, generating a continuous cuff‐like force to compress the fracture fragment. The surgeon control the traction force based on increased length of upper limb and tension of the skin. The traction force could not be too large, preventing acromion fracture. Then, plates were implanted using the MIPO technique. C‐arm fluoroscopy was performed in at least two directions to confirm the basic reduction of the fracture before plate implantation.
FIGURE 1.

The bidirectional rapid reductor device.
The procedure of plate implantation closely resembled those of conventional MIPO surgery. 13 However, a key distinction lay in the initial steps: the plate was first positioned externally using two needles, with its height guided by fluoroscopy. Subsequently, the plate was percutaneously inserted, and two screws were implanted at the distal and proximal ends. After achieving a satisfactory reduction of the fracture sites and position of the plate, the remaining screws were implanted. The surgical procedure was shown in an animation (Video S1). The radiation time during surgery was collected from the fluoroscopic device. All surgeries were performed with the same setting and the same device.
Post‐operative Management and Follow‐up
Post‐operative immediate radiography (AP and lateral views) and CT scans were obtained for all patients to evaluate the quality of reduction. Antibiotic prophylaxis was used to prevent infection within 24 h. All patients worn a shoulder abduction brace for 3 weeks. Continuous passive movement started on the fourth day after surgery. Weight‐holding activities were restricted for the first 8 weeks. At approximately 9–12 weeks, partial weight‐holding activities were allowed and gradually translated to full weight‐holding after confirmation of clinical and radiological union. All patients underwent routine radiography to evaluate the status of fracture site weekly, until fracture union.
The VAS (from 0 to 10, higher scores indicating more pain) was determined to assess the pain degree, 18 the constant‐Murley score (CMS, from 0 to 100, higher scores indicating better outcomes) was used to evaluate the shoulder junction, and if the CMS >80, the junction was defined as good. 19
Data Analysis
IBM SPSS Statistics 25 (SPSS Inc., Chicago, IL, USA) was employed for statistical analysis. Continuous variables were presented as mean ± standard deviation.
Results
Patient Demographics
A total of 23 patients with PHFs underwent MIPO assisted by BRR. However, 11 patients were excluded from the study: three due to concomitant ipsilateral proximal ulna fractures, six for non‐cooperation with follow‐up, one died from coronary heart disease within 1 year, and one due to recurrent fracture at the same site. Basic information, including sex, age, mechanism of injury, injured sides, and Neer types were gathered from all patients and summarized in Table 1. Among the 12 included patients, four were men and eight were women, with nine experiencing left shoulder injuries and three right shoulder injuries. The average age in this series was 67.58 years (range 44–84). Four patients suffered from Neer type IV, 2 from III, 5 from II, and 1 from I. Most of the patients (9/12, 75%) were injured by falling on the ground. 3 typical cases are shown in Figures 2, 3, 4.
TABLE 1.
Baseline characteristics and results of the patients
| No. | Age (year) | Side | Neer type | Mechanism injury | Operation time (min) | Blood loss (mL) | Fluoroscopy time (s) | Union time (weeks) | Follow‐up time (month) | Last follow‐up VAS | Last follow‐up CMS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 70 | Left | II | Fall | 76 | 50 | 14 | 12 | 12 | 0 | 95 |
| 2 | 76 | Right | II | Bruise | 80 | 50 | 14 | 8 | 10 | 0 | 92 |
| 3 | 84 | Left | III | Fall | 65 | 100 | 14 | 7 | 14 | 2 | 81 |
| 4 | 71 | Left | II | Fall | 75 | 150 | 11 | 9 | 8 | 0 | 90 |
| 5 | 74 | Left | II | Fall | 64 | 100 | 10 | 10 | 11 | 0 | 92 |
| 6 | 44 | Left | I | Fall | 78 | 50 | 14 | 9 | 6 | 0 | 96 |
| 7 | 70 | Right | II | Fall | 70 | 100 | 12 | 7 | 15 | 0 | 89 |
| 8 | 78 | Right | IV | Fall | 72 | 300 | 16 | 8 | 13 | 1 | 82 |
| 9 | 59 | Left | IV | Traffic accident | 63 | 100 | 9 | 11 | 7 | 0 | 85 |
| 10 | 62 | Left | III | Bruise | 68 | 65 | 21 | 16 | 9 | 2 | 80 |
| 11 | 58 | Left | IV | Fall | 71 | 60 | 14 | 9 | 11 | 0 | 86 |
| 12 | 65 | Left | IV | Fall | 69 | 60 | 12 | 10 | 13 | 0 | 88 |
Abbreviations: VAS, visual analogue scale; CMS, Constant‐Murley score.
FIGURE 2.
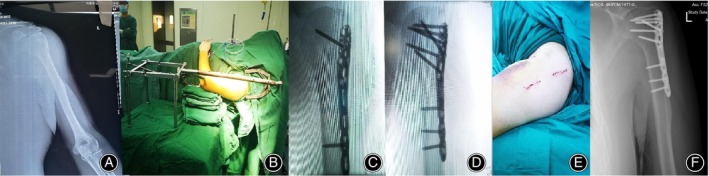
A 44‐year‐old man with a left proximal humeral fracture, Neer type I. (A) Preoperative radiograph showing a one‐part proximal humeral fracture. (B) Preoperative double reverse traction. (C) Intraoperative radiograph showing the fracture was nearly anatomically reduced. (D) Early postoperative radiograph tested the position of plate and screws. (E) Two surgical incisions were small. (F) 9 weeks postoperative radiograph showing fracture union.
FIGURE 3.

A 59‐year‐old woman with left proximal humeral fracture, Neer type IV. (A) Preoperative radiograph showing a four‐part proximal humeral fracture. (B) Preoperative double reverse traction. (C) Two surgical incisions were small. (D) Early postoperative radiograph showing the fracture was nearly anatomically reduced. (E) 11 weeks postoperative radiograph showing fracture union.
FIGURE 4.

A 70‐year‐old man with left proximal humeral fracture, Neer type III. (A) Preoperative radiograph showing a three‐part proximal humeral fracture. (B) Preoperative double reverse traction. (C) Intraoperative radiograph showing the fracture was nearly anatomically reduced. (D) Early postoperative radiograph tested the position of plate and screws. (E) 12 months postoperative radiograph showing fracture union and plate was removed.
Clinical Outcomes
The average operation time was 70.92 min (range 63–80 min). The average blood loss was 102.27 mL (range 50–300 mL). The average fluoroscopy time was 13.42 s (range 9–21 s). The mean VAS, CMS at final follow‐up were 0.33 and 88, respectively. The average follow‐up time was 10.75 month (range 6–15 month). Utilizing BRR, MIPO was successfully achieved in all patients, and none required conversion to open reduction. One patient contracted shoulder stiffness at the third month, and returned to normal activities with manipulation release treatment. Notably, there were no instances of wound dehiscence or axillary nerve injuries at the time of hospital discharge. No complications, such as deep infection, osteomyelitis, internal fixation loosening was observed in any of the patients, and routine follow‐up was performed until fracture healing.
Discussion
Main Findings
The rapid reductor could not only efficiently reduce the fracture but also maintained it in an anatomical position. Anatomic or nearly anatomic reduction of fracture site were achieved in all cases. This procedure offered advantages of less operation time and less exposure time. All fractures healed well and satisfactory functional recovery was identified in the majority of the patients.
Necessity of the Application of BRR
The ORIF technique is a popular surgical fixation for proximal humerus fractures, typically through the delto‐pectoral approach. 20 However, this approach may lead to several disadvantages, including injury to the deltoid muscle, increased blood loss, nonunion, avascular necrosis of the humeral head, and wound infection. 5 , 21 The MIPO technique using the deltoid splitting approach, as it preserves the blood circulation of periosteum around the fracture, resulting to reduce complications of the traditional ORIF technique. 21 However, for MIPO technique, anatomical reduction of fractures with more than two parts may be more difficult, as it mainly relies on indirection reduction of the fracture site, and exposure of medial aspects of the proximal humerus is limited. 22 Longer radiation exposure time is another disadvantage of MIPO, because it needs repeated use of fluoroscopy to attain an acceptable closed reduction in MIPO. 4 Based on the shortcomings of MIPO for PHFs, we tried to use BRR to improve outcomes of MIPO, made up for the shortcomings, and reduced the incidence of complications.
Technical Characteristics of the BRR
Its functionality is grounded in the principle that: (i) traction reduction aligns with the limb's vertical line; and (ii) sustained reverse traction aligns with the mechanical axis of the limb and the soft tissue slip trajectory. 16 Simultaneously, (iii) an extrusion force generated by the soft tissue around the fracture sites; and (iv) These dual forces collaborate effectively, which ensured better reduction of fracture sites and reduce disruption of blood circulation around the humeral head, especially for the varus fractures. If closed reduction of varus fractures were not successful, we also used the “Joy‐stick technique” or the elevator to disimpact the head and moved it into the correct position, with a special attention to medial hinge. 11 The head was preliminarily secured with K‐wires before applying the plate.
The BRR is designed to be suitable for placement on the intraoperative sterile operating table. Its user‐friendly nature is amplified by its easy installation procedure, with the entire installation process requiring approximately 5 min. The positioning of the traction rod anterior to the arm ensures that it did not obscure the incision. Extracutaneous needle location helped evaluate the plate's position, and might reduce the length of the surgical incisions.
Advantages and Pitfalls
The BRR is a pragmatic device designed to efficiently reduce fracture dislocation and the traction power is strong, sustainable, and adjustable. 16 , 17 , 23 This device effectively addresses the limitations of manual traction, such as inadequate traction strength, unsustainable force, and high labor costs. In previous studies, 13 , 24 , 25 , 26 the MIPO groups had a mean operation time of 80–133.6 min, blood loss of 87.5–155.2 mL, radiation exposure time of 19.2–38.5 s, and CMS score of 75.6–86.6. The above advantages of BRR could ensure our MIPO surgeries with less operation time, blood loss, radiation exposure time and higher CMS score than these studies. However, the differences in surgeons and sample sizes between this study and previous studies might influence the comparison results.
In our study, no patients suffered from axillary nerve injury and iatrogenic fracture. The sustained force generated by the BRR was instrumental in moving the anterior branch of the axillary nerve away from the humerus cortex, thereby reducing the risk of nerve injury. However, our speculation needs to be verified in cadavers in the future. Acromion fracture may occur during traction, likely due to factors such as osteoporosis, error position of K‐wire and excessive traction during surgery. To mitigate the risk of acromial fracture, it is imperative to explore the methods of applying precise traction force and identifying the optimal insertion point for K‐wire in the acromial region.
Limitations and Prospect
Our study has several limitations. First, we were unable to measure the traction force applied by the BRR, which could lead to iatrogenic fractures under excessive force. Second, we did not conduct cadaveric studies to assess the device, and we plan to improve the rationale for its use in future cadaver studies. Third, the mean follow‐up time was limited, and we should increase the follow‐up time to evaluate the treatment efficacy of fractures. Additionally, our sample size was small, and we did not conduct a comparative study. We intend to conduct a large‐sample randomized controlled trial in the future. In our study, patients with complex PHFs accounted for 50% (Neer type III + IV, 6/12), but the absolute quantity was small, and this result cloud not reflect an advantage in MIPO surgery for complex PHFs. And we recommend that junior surgeons initially apply BRR in simple proximal humeral fractures.
Conclusion
In conclusion, our findings suggested that the BRR could be effectively applied in the MIPO treatment of PHFs. The BRR not only helped achieve or maintain reduction in PHFs during MIPO treatment but also reduced operation and exposure times.
Conflict of Interest Statement
The authors have no relevant financial or non‐financial interests to disclose.
Ethics Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of The Third Hospital of Hebei Medical university (S2020‐016‐1). Informed consent was obtained from all individual participants included in the study. The authors affirm that human research participants provided informed consent for publication of the data.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, Y.Z.Z. and Z.L.Z.; methodology, P.H.W. and Y.Z.Z.; investigation, N.Y. and P.H.W.; formal analysis, Z.L.Z. and P.H.W.; resources, N.Y. and Z.L.Z.; writing—original draft, P.H.W. and Q.W.; writing—review and editing, P.H.W. and N.Y.; visualization, P.H.W. and Q.W.; supervision, Y.Z.Z.; funding acquisition, Y.Z.Z.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and that all authors are in agreement with the manuscript.
Supporting information
Video S1. “Detailed procedures of BRR combined with MIPO technique in the treatment of PHFs.”
Acknowledgments
This study was supported by the Integration Project of NSFC Joint Fund for Regional Innovation and Development (U23A6008), the Major Research plan of National Natural Science Foundation of China (91949203), the Key Projects of the National Natural Science Foundation of China (32130052), The Construction project of Shaoguan Social Development Science and technology Collaborative Innovation System (220603234531179, 230330168035974), The Natural Science Fundation of Hebei Province (H2024206050). We are grateful to the Sifan Yang of the Third Hospital of Hebei Medical University for their kind assistance.
Penghuan Wu, Na Yang, and Qiang Wu should be considered joint first author.
Yingze Zhang and Zhanle Zheng should be considered joint corresponding author.
Contributor Information
Zhanle Zheng, Email: 3803185097@qq.com.
Yingze Zhang, Email: dryzzhang@sina.com.
References
- 1. Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 2. Stirma GA, Secundino AR, Gonzalez G, et al. Inter/intra‐observer evaluation between radiographs and tomographies for proximal humerus fracture. Acta Ortop Bras. 2020;28(1):36–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burke NG, Kennedy J, Cousins G, Fitzpatrick D, Mullett H. Locking plate fixation with and without inferomedial screws for proximal humeral fractures: a biomechanical study. J Orthop Surg‐Hong K. 2014;22(2):190–194. [DOI] [PubMed] [Google Scholar]
- 4. Li F, Liu X, Wang F, Gu Z, Tao Q, Yao C, et al. Comparison between minimally invasive plate osteosynthesis and open reduction‐internal fixation for proximal humeral fractures: a meta‐analysis based on 1050 individuals. BMC Musculoskelet Disord. 2019;20(1):550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buchmann L, van Lieshout E, Zeelenberg M, et al. Proximal humerus fractures (PHFs): comparison of functional outcome 1 year after minimally invasive plate osteosynthesis (MIPO) versus open reduction internal fixation (ORIF). Eur J Trauma Emerg Surg. 2022;48(6):4553–4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maier D, Jaeger M, Izadpanah K, Strohm PC, Suedkamp NP. Proximal humeral fracture treatment in adults. J Bone Joint Surg Am. 2014;96(3):251–261. [DOI] [PubMed] [Google Scholar]
- 7. Abouelela A, Mubark I, Nagi A, Genena A. Short‐term clinical outcome of proximal humeral fracture fixation using minimally invasive trans‐deltoid approach. Ortop Traumatol Rehabil. 2020;22(4):221–226. [DOI] [PubMed] [Google Scholar]
- 8. Narayanan VL, Balasubramanian N. Complex proximal humeral fracture fixation with PHILOS plate using minimal invasive percutaneous plate osteosynthesis (MIPPO) technique: a series of 30 patients. Malays Orthop J. 2018;12(2):20–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brunner A, Thormann S, Babst R. Minimally invasive percutaneous plating of proximal humeral shaft fractures with the proximal humerus internal locking system (PHILOS). J Shoulder Elbow Surg. 2012;21(8):1056–1063. [DOI] [PubMed] [Google Scholar]
- 10. Oh HK, Cho DY, Choo SK, Park JW, Park KC, Lee JI. Lessons learned from treating patients with unstable multifragmentary fractures of the proximal humerus by minimal invasive plate osteosynthesis. Arch Orthop Traum Surg. 2015;135(2):235–242. [DOI] [PubMed] [Google Scholar]
- 11. Borer J, Schwarz J, Potthast S, Jakob M, Lenzlinger P, Zingg U, et al. Mid‐term results of minimally invasive deltoid‐split versus standard open deltopectoral approach for PHILOS (proximal humeral internal locking system) osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg S. 2020;46(4):825–834. [DOI] [PubMed] [Google Scholar]
- 12. Beeres F, Quaile OM, Link BC, Babst R. Reduction techniques for minimally invasive stabilization of proximal humeral fractures. Oper Orthop Traumato. 2019;31(1):63–80. [DOI] [PubMed] [Google Scholar]
- 13. Kim YG, Park KH, Kim JW, Oh JK, Yoon JP, Kim HJ, et al. Is minimally invasive plate osteosynthesis superior to open plating for fixation of two‐part fracture of the proximal humerus? J Orthop Surg‐Hong K. 2019;27(2):2309499019836156. [DOI] [PubMed] [Google Scholar]
- 14. Attala DD, Primavera MM, Di Marcantonio AA, et al. The role of minimally invasive plate osteosynthesis (MIPO) technique for treating 3‐ and 4‐part proximal humerus fractures in the elderly. A case study. Acta Biomed Ateneo Parmense. 2021;92(4):e2021251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chang H, Zheng Z, Yu Y, Shao J, Zhang Y. The use of bidirectional rapid reductor in minimally invasive treatment of bicondylar tibial plateau fractures: preliminary radiographic and clinical results. BMC Musculoskelet Disord. 2018;19(1):419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lian X, Zhao K, Chen W, Zhang J, Li J, Meng H, et al. Application of a double reverse traction repositor in the retrograde intramedullary nailing of distal femur fractures. J Orthop Surg Res. 2021;16(1):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang Z, Zheng Z, Wang Y, Zhu Y, Tan Z, Chen W, et al. Unilateral locking plate versus unilateral locking plate combined with compression bolt for Schatzker I‐IV tibial plateau fractures: a comparative study. Int Orthop. 2022;46(5):1133–1143. [DOI] [PubMed] [Google Scholar]
- 18. Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79(2):231–252. [DOI] [PubMed] [Google Scholar]
- 19. Constant CR. Assessment of shoulder function. Orthopade. 1991;20(5):289–294. [PubMed] [Google Scholar]
- 20. Liu Y, Wei X, Kuang Y, et al. Open vs. closed reduction combined with minimally invasive plate osteosynthesis in humeral fractures. Minim Invasive Ther Allied Technol. 2016;25(4):215–221. [DOI] [PubMed] [Google Scholar]
- 21. Sohn HS, Jeon YS, Lee J, Shin SJ. Clinical comparison between open plating and minimally invasive plate osteosynthesis for displaced proximal humeral fractures: a prospective randomized controlled trial. Injury. 2017;48(6):1175–1182. [DOI] [PubMed] [Google Scholar]
- 22. Gavaskar AS, Chowdary N, Abraham S. Complex proximal humerus fractures treated with locked plating utilizing an extended deltoid split approach with a shoulder strap incision. J Orthop Trauma. 2013;27(2):73–76. [DOI] [PubMed] [Google Scholar]
- 23. Li S, Yin Y, Zhang R, Chen W, Zhang Y. Minimally invasive treatment for fractures of lower extremity amputees using a rapid reductor. Int Orthop. 2019;43(6):1473–1478. [DOI] [PubMed] [Google Scholar]
- 24. Chiewchantanakit S, Tangsripong P. Locking plate fixation of proximal humeral fracture: minimally invasive vs. standard delto‐pectoral approach. J Med Assoc Thai. 2015;98(2):196–200. [PubMed] [Google Scholar]
- 25. Wang JF, Song HB, Gu HJ, Ling ZD, Ma HH. Case‐control study on minimally invasive plate osteosynthesis for the treatment of proximal humeurs fractures in elderly patients. Zhongguo Gu Shang. 2012;25(6):487–489. [PubMed] [Google Scholar]
- 26. Shen QF, Wen X, Yang SW, Chen X, Fan WX, Xu GZ, et al. MIPPO and ORIF for the treatment of elderly proximal humerus fractures of type Neer II:a case control study. Zhongguo Gu Shang. 2018;31(2):160–164. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. “Detailed procedures of BRR combined with MIPO technique in the treatment of PHFs.”


