Abstract
A rare congenital condition known as hydrometrocolpos (HMC) is characterized by the buildup of secretions in the vagina and uterus as a result of distal obstruction; this condition is frequently linked to imperforate hymen. This case report presents a prenatal diagnosis of isolated HMC in a 30-year-old primigravida, detected at 36 weeks gestation. Initial ultrasound revealed a large cystic mass, confirmed by fetal magnetic resonance imaging to be HMC. Postnatal examination of the new born confirmed imperforate hymen and HMC, which was effectively treated with hymenotomy, resulting in early resolution. This case underscores the importance of prenatal imaging in the early identification and management of HMC to prevent potential complications.
Keywords: Hydrometrocolpos, Prenatal, Sonographic diagnosis, Cystic mass, Magnetic resonance imaging
Introduction
A rare condition known as hydrometrocolpos (HMC) is characterized by the buildup of mucus or blood discharges in the vagina and uterus as a result of distal blockage. Fetal HMC, with a reported incidence of 1 in 16,000 female newborns, is unusual [1], in contrast to the comparatively common hematocolpos [2]. Usually diagnosed in adolescence or after menarche, HMC manifests as a painful primary amenorrhea with a pelvic mass [3].
Prenatal ultrasound diagnosis of fetal HMC is rare, with only a few cases reported in the literature. In 1962, Spencer and Levy [1] reported 62 cases of HMC, attributing its embryonic pathogenesis to the coexistence of estrogenic stimulation and vaginal obstruction. Failure to recognize and treat this condition in a timely manner can lead to serious complications [4], such as hydronephrosis, urinary retention, and intestinal obstruction [5].
We herein report a case of isolated HMC secondary to a congenital imperforate hymen diagnosed antenatally, identified by ultrasound and magnetic resonance imaging (MRI), which allowed for immediate surgical treatment postnatally and early resolution.
Case presentation
A 30-year-old primigravida was referred to our hospital for the evaluation of a fetal abdominal cystic mass detected incidentally at 36 weeks of amenorrhea. The parents were not consanguineous, and the medical and obstetric history was unremarkable. During the first trimester examination, the nuchal translucency was normal and the triple test results were low risk. A fetal morphological ultrasound performed at 22 weeks was reported as normal, and the patient's prenatal care had been uneventful until this finding.
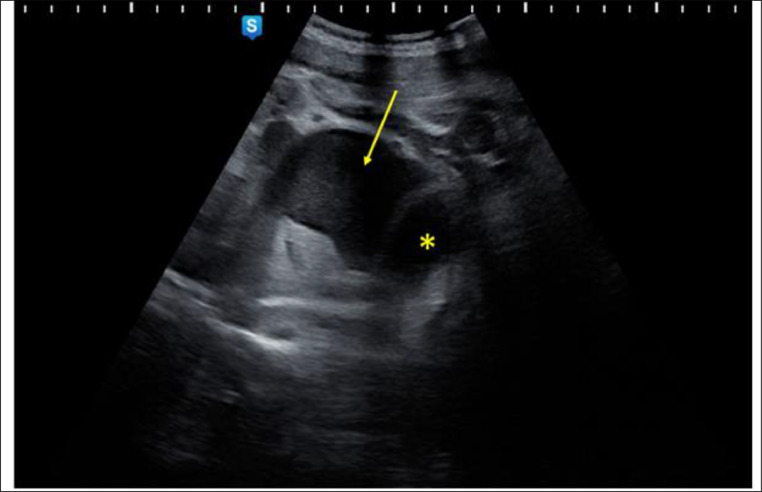
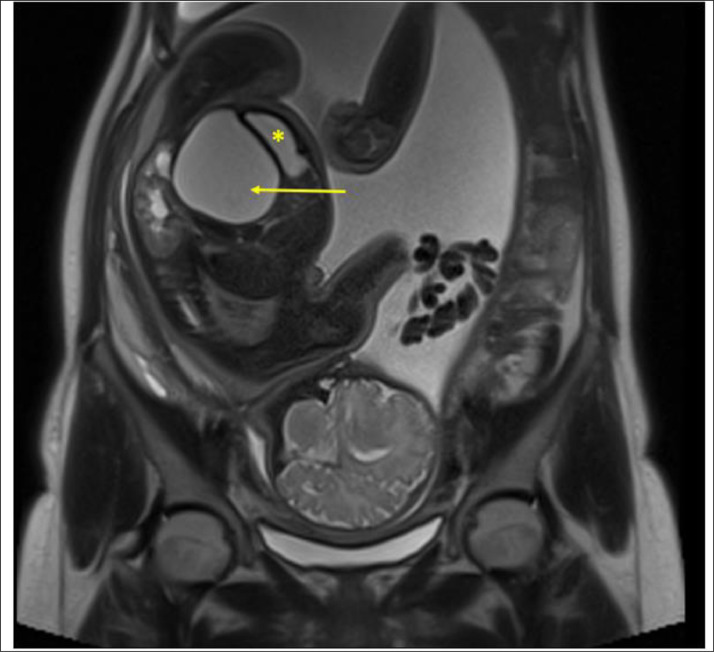
Upon admission, our initial ultrasound revealed a single female fetus, consistent with gestational age, with a large abdominal cystic mass. The suspicious image appeared as a large retrovesical cystic hypoechoic mass measuring 70 × 60 × 50 mm in maximum diameter (Fig. 1). Color Doppler imaging showed no neovascularization within the mass. The bladder appeared normal, and no other concomitant fetal anomalies were detected. Based on these prenatal ultrasound results, a fetal ovarian cyst was suspected. However, we completed our investigations with fetal MRI to confirm the diagnosis. The fetal MRI showed a pelvic mass behind the bladder and in front of the rectum with hypo- and hyperintense content on T2-weighted images, corresponding to a fluid debris level (Fig. 2). Thus, the diagnosis of congenital imperforate hymen with isolated HMC was established. At 39 weeks of gestation, a female newborn weighing 3700 g was delivered vaginally with good Apgar scores.
Fig. 1.
Fetal US showing a hypoechoic cystic retro vesical mass: Hydrometrocolpos (Arrow); Bladder (Asterisk)
Fig. 2.
MRI of the fetus in coronal section, T2-Weighted sequence showing a pelvic mass posterior to the bladder and anterior to the rectum with hypointense and hyperintense content corresponding to a fluid debris level: Hydrometrocolpos (Arrow); Bladder (Asterisk)
On the initial physical examination of the newborn, the abdomen was soft but distended above the umbilicus, and the mass measured 67 cm. The perineum was normal with a normally positioned perforated anus. However, an imperforate hymen was noted (Fig. 3). The remainder of the physical examination was unremarkable, excluding the presence of syndromic anomalies. An abdominal and pelvic ultrasound of the newborn showed a large pear-shaped retrovesical cystic mass, thickened and midline, with internal echoes measuring 70 × 60 mm, confirming the diagnosis of HMC. A cross-type hymenotomy with excision was performed by pediatric surgeons 4 days after birth, draining 60 mL of milky fluid. Follow-up 4 weeks after the hymenotomy showed complete regression of the HMC, as demonstrated by a control ultrasound. The newborn is currently 9 months old and asymptomatic.
Fig. 3.
Physical examination showing a bulging membrane covering the vaginal opening (arrow)
Discussion
HMC is a rare condition in fetal medicine (0.006%) that is typically detected incidentally during routine prenatal ultrasounds [6]. Various obstructive vaginal anomalies can be found, such as an imperforate hymen, a transverse vaginal septum, or partial vaginal atresia [6].
Congenital imperforate hymen is the most common congenital malformation of the female genital tract [7], with a reported incidence of 0.1%-0.014% [8]. When a hymen is still intact, excessive intrauterine stimulation of the fetal cervical mucous glands by maternal estrogen results in HMC, which accumulates secretions in the uterus and vagina [9]. The prenatal diagnosis of an imperforate hymen with HMC has been reported as early as 25 weeks of gestation [10]. This represents 15% of abdominal masses in female infants [11]. In neonates and young infants, HMC can be of 2 types depending on the type of accumulated fluid [12]: mucus secreted by the glands of the uterus and cervix or urine secondary to urogenital or cloacal malformations. The degree of surrounding structure compression affects how HMC presents. Compression of the urinary tract frequently results in varying degrees of hydronephrosis [13,14]. In more severe cases of compression, infants may present with acute urinary retention and intestinal obstruction [15,16].
HMC can be secondary to an isolated congenital imperforate hymen, as reported in our case, or may sometimes be part of multiple syndromic and nonsyndromic malformations [11,17,18]. Hence, in addition to congenital heart disease in Meckel-Kaufman syndrome/Bardet-Biedl syndrome [19,20], patients with congenital HMC should also be evaluated for other anomalies, such as postaxial polydactyly, renal, skeletal, auricular, and cardiac malformations in Mayer-Rokitansky-Küster-Hauser syndrome [21,22].
Prenatal diagnosis of an imperforate hymen and HMC has been reported in a few cases in the literature. It typically shows a hypoechoic retrovesical cystic mass in the fetal abdomen, similar to that reported in our case.
Prenatal differentiation of female urogenital anomalies can be challenging due to their rarity, variable presentation, and limitations in ultrasonographic imaging, particularly in late gestation. HMC may be misidentified as an abdominal cystic mass. Possible differential diagnoses include ovarian cyst, duplication cyst, mesenteric cyst, meconium cyst, urachal cyst, anterior meningocele, and a pelvic component of sacrococcygeal teratoma [23].
Prenatal ultrasound should also exclude any associated fetal anomalies that may be part of several syndromes.
Due to the low incidence of fetal HMC, clinicians have reported additional imaging, primarily fetal MRI, to establish the diagnosis and characterize the extent of the lesion [7]. MRI is reported to have complementary value due to its precise anatomical localization and contrast resolution [[24], [25], [26]]. In our case, HMC was strongly suspected on prenatal ultrasound due to a midline cystic pelvic mass located posterior to the bladder and connected to the dilated uterus. An antenatal MRI was performed to better characterize the mass, and the communication between the uterine and vaginal components was better visualized, establishing the etiology of the isolated imperforate hymen. No other fetal anomalies were found on ultrasound and MRI in our case.
HMC has been linked to several renal compromises, abdominal ascites [27], acute urine retention, and acute renal failure due to obstructive uropathy [28], all of which are complications of a congenital imperforate hymen.
The diagnosis of HMC complicating an imperforate hymen was confirmed after birth by postnatal ultrasound results and physical examination. The concordant results of antenatal ultrasound and MRI with postnatal imaging and physical examination led to the conclusion that prenatal diagnosis by ultrasound, sometimes supported by specific MRI imaging, allows for precise diagnosis of this rare condition, enabling appropriate management from early on. These findings also underscore the need to refine our prenatal ultrasound skills, particularly in low-resource countries where access to fetal MRI is not always available, but where precise prenatal and postnatal ultrasound imaging can be perfectly adequate.
Surgical interventions for HMC range from surgical drainage to correction of complex genital anomalies [29]. In most cases reported in the literature, isolated HMC due to a congenital imperforate hymen has been definitively treated, regardless of the patient's age, by hymenectomy [30], which remains the most common and effective approach for this condition, allowing for drainage and relief of the mass, as demonstrated in our case where hymenectomy was performed 4 days after birth and complete resolution of HMC occurred 4 weeks later.
HMC is not a life-threatening condition and, generally, outcomes associated with congenital imperforate hymen are good. However, delayed diagnosis and interventions can lead to serious complications due to compression of surrounding structures, infection, endometriosis due to blood accumulation, and infertility [29].
Therefore, extended follow-up into adulthood is crucial for cases of HMC, particularly when accompanied by other malformations, in order to identify and address any related issues.
Conclusion
The diagnosis of fetal HMC associated with a congenital imperforate hymen should always be considered when a large cystic pelvic mass is detected in a female fetus during obstetric ultrasound. Prenatal MRI may be necessary to better characterize the etiology and exclude other complex anomalies.
However, based on the findings from our case, an early antenatal ultrasound (US) followed by a postnatal US and a thorough physical examination may be sufficient for making the diagnosis, particularly in resource-limited medical facilities. This approach enables early and effective management, facilitating the resolution of underlying complications.
Patient consent
Complete written informed consent was obtained from the patient for the publication of this study and accompanying images.
Footnotes
Competing Interests: The authors declare that they have no known competing financia linterests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Spencer R, Levy DM. Hydrometrocolpos: report of three cases and review of the literature. Ann Surg. 1962;155(4):558–571. doi: 10.1097/00000658-196204000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dahnert W. 6th ed. Vol. 1007. Lippincott Williams and Wilkins; Philadelphia: 2007. pp. 1046–1047. (Radiologyreviewmanual). [Google Scholar]
- 3.Lui C.T., Chan T.W.T., Fung H.T., Tang S.Y.H. A retrospective study on imperforate hymen and haematometrocolpos in a regional hospital. Hong Kong J Emerg Med. 2010;17(5):435–440. [Google Scholar]
- 4.Bischoff A, Levitt MA, Breech L, Louden E, Peña A. Hydrocolpos in cloacal malformations. J Pediatr Surg. 2010;45(6):1241–1245. doi: 10.1016/j.jpedsurg.2010.02.097. [DOI] [PubMed] [Google Scholar]
- 5.Tanitame K, Tanitame N, Urayama S, Ohtsu K. Congenital anomalies causing hemato/hydrocolpos: imaging findings, treatments, and outcomes. Jpn J Radiol. 2021;39(8):733–740. doi: 10.1007/s11604-021-01115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaked O, Tepper R, Klein Z, Beyth Y. Hydrometrocolpos–diagnostic and therapeuticdilemmas. J PediatrAdolesc Gynecol. 2008;21(6):317–321. doi: 10.1016/j.jpag.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Garcia Rodriguez R, Pérez González J, Garcia Delgado R, Rodriguez Guedes A, de Luis Alvarado M, Medina Castellano M, et al. Fetalhydrometrocolpos and congenital imperforate hymen: prenatal and postnatal imaging features. J Clin Ultrasound. 2018;46(8):549–552. doi: 10.1002/jcu.22588. [DOI] [PubMed] [Google Scholar]
- 8.Kahn R, Duncan B, Bowes W. Spontaneous opening of congenital imperforate hymen. JPediatr. 1975;87(5):768–770. doi: 10.1016/s0022-3476(75)80306-4. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim G, Gungorduk K, Aslan H, Sudolmus S, Ark C, Saygin S. Prenatal diagnosis of imperforate hymen with hydrometrocolpos. Arch Gynecol Obstet. 2008;278(5):483–485. doi: 10.1007/s00404-008-0603-x. [DOI] [PubMed] [Google Scholar]
- 10.Winderl LM, Silverman RK. Prenatal diagnosis of congenital imperforate hymen. Obstet Gynecol. 1995;85(5 Pt 2):857–860. doi: 10.1016/0029-7844(94)00405-3. [DOI] [PubMed] [Google Scholar]
- 11.Reed MH, Griscom NT. Hydrometrocolpos in infancy. Am J Roentgenol Radium Ther NuclMed. 1973;118(1):1–13. doi: 10.2214/ajr.118.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Sharma D, Murki S, Pratap OT, Irfan G, Kolar G. A case of hydrometrocolpos and polydactyly. Clin Med Insights Pediatr. 2015;9:7–11. doi: 10.4137/CMPed.S20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aggarwal S, Kumar A. Fetalhydrocolpos leading to Pierre Robin sequence: an unreportedeffect of oligohydramnios sequence. J Perinatol. 2003;23(1):76–78. doi: 10.1038/sj.jp.7210846. [DOI] [PubMed] [Google Scholar]
- 14.- Silva ÍS, Martello R, Mendes A, Chaves A. Urinary retention due to hematocolpos. ActaMed Port. 2021;34(3):232–235. doi: 10.20344/amp.11912. [DOI] [PubMed] [Google Scholar]
- 15.Arriola-Montenegro L, Arriola-Montenegro J, Pia-Balmaceda M, Celis-Albujar C, Riva-Moscoso A, Cabanillas-Lozada P, et al. Hydrometrocolpos and post-axial polydactyly complicated with acute intestinal obstructihydroureteronephrosis. Cureus. 2021;13(8):e17612. doi: 10.7759/cureus.17612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okoro PE, Obiorah C, Enyindah CE. Experience with neonatal hydrometrocolpos in the Niger. Delta area of Nigeria: upsurge or increased recognition? Afr J Paediatr Surg. 2016;13(4):161–165. doi: 10.4103/0189-6725.194666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rohatgi M, Gupta DK, Luthra M. Neonatal hydrometrocolpos associated with McKusickKaufman syndrome. Indian J Pediatr. 1989;56(3):438–441. doi: 10.1007/BF02722322. [DOI] [PubMed] [Google Scholar]
- 18.Hu MX, Methratta S. An unusual case of neonatal peritoneal calcifications associated withhydrometrocolpos. PediatrRadiol. 2001;31(10):742–744. doi: 10.1007/s002470100524. [DOI] [PubMed] [Google Scholar]
- 19.Slavotinek AM, Biesecker LG. Phenotypic overlap of McKusick-Kaufman syndrome withbardet-biedl syndrome: a literature review. Am J Med Genet. 2000;95(3):208–215. [PubMed] [Google Scholar]
- 20.Forsythe E, Kenny J, Bacchelli C, Beales PL. Managing Bardet-Biedl syndrome-now and in the future. Front Pediatr. 2018;6:23. doi: 10.3389/fped.2018.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herlin MK, Petersen MB, Brännström M. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: a comprehensive update. Orphanet J Rare Dis. 2020;15(1):214. doi: 10.1186/s13023-020-01491-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morcel K, Camborieux L, Programme de Recherches sur les Aplasies Müllériennes. Guerrier D. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Orphanet J Rare Dis. 2007;14(2):13. doi: 10.1186/1750-1172-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anguenot JL, Ibecheole V, Salvat J, Campana A. Hematocolpos secondary to imperforatehymen, contribution of transrectal echography. Acta ObstetGynecolScand. 2000;79(7):614–615. [PubMed] [Google Scholar]
- 24.Hayashi S, Sago H, Kashima K, Kitano Y, Kuroda T, Honna T, et al. Prenatal diagnosis of fetalhydrometrocolpos secondary to a cloacal anomaly by magnetic resonance imaging. Ultrasound Obstet Gynecol. 2005;26(5):577–579. doi: 10.1002/uog.2584. [DOI] [PubMed] [Google Scholar]
- 25.Gupta P, Sharma R, Kumar S, Gadodia A, Roy KK, Malhotra N, et al. Role of MRI in fetalabdominal cystic masses detected on prenatal sonography. Arch Gynecol Obstet. 2010;281(3):519–526. doi: 10.1007/s00404-009-1190-1. [DOI] [PubMed] [Google Scholar]
- 26.Subramanian S, Sharma R, Gamanagatti S, Agarwala S, Gupta P, Kumar S. Antenatal MRdiagnosis of urinary hydrometrocolpos due to urogenital sinus. PediatrRadiol. 2006;36(10):1086–1089. doi: 10.1007/s00247-006-0249-4. [DOI] [PubMed] [Google Scholar]
- 27.El-Messidi A, Fleming NA. Congenital imperforate hymen and its life-threateningconsequences in the neonatal period. J PediatrAdolesc Gynecol. 2006;19(2):99–103. doi: 10.1016/j.jpag.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 28.Aygun C, Ozkaya O, Ayyýldýz S, Güngör O, Mutlu B, Küçüködük S. An unusual cause of acute renal failure in a newborn: hydrometrocolpos. Pediatr Nephrol. 2006;21(4):572–573. doi: 10.1007/s00467-006-0022-9. [DOI] [PubMed] [Google Scholar]
- 29.Khanna K., Sharma S., Gupta D.K. Hydrometrocolposetiology and management: past beckons the present. Pediatr Surg Int. 2018;34:249–261. doi: 10.1007/s00383-017-4218-9. [DOI] [PubMed] [Google Scholar]
- 30.Baek YJ, Kim JT, Jang SK, Choi OH. A case of imperforate hymen in newborn infant causinghydrometrocolpos and hydronephrosis. Korean J ObstGynecol. 2007;50:372–375. [Google Scholar]