Abstract
Background
Thoracic injuries are a very common entity throughout all age groups. With rising numbers of geriatric patients, characteristics of this patient group need to be better defined. The aim of this study was to investigate the impact of age on the outcome of thoracic trauma. In this project we provide a stratification of differentiated age groups regarding outcome parameter on rib fractures.
Methods
The study employed a retrospective design using data from patients who sustained thoracic trauma and received treatment at a level I trauma center over a 5-year period. Patients with the same pattern of injury and gender but different age (above and below 70 years) were matched.
Results
The mean age of the study population was 57 ± 19 years, 69% were male, 54% of patients had preexisting comorbidities. Hemothorax was present in 109 (16%), pneumothorax in 204 (31%) and lung contusions in 136 patients (21%). The overall complication rate was 36%, with a mortality rate of 10%. The matched pair analysis of 70 pairs revealed a higher prevalence of comorbidities in the older age group. They had significantly fewer pulmonary contusions and pneumothoraces than the younger patients and a shorter length of stay. However, the older age group had a significantly higher mortality rate.
Conclusions
Geriatric patients with rib fractures exhibit different patterns of intrathoracic injuries compared to their younger counterparts. Although numeric age may not be the most accurate predictor of adverse outcome, we found that higher age was associated with a clear trend towards an increased mortality rate. Our findings build a basis for further research to evaluate the outcome of age for instance with the tool of a rib fracture scoring system within stratified age groups in order to identify patients at major risk.
Keywords: age, rib fracture, outcome, case-control study
Introduction
Rib fractures are a common injury and can have significant impact on patient outcomes.1-3 Furthermore, age and comorbidities influence the outcome and likelihood of adverse events in chest trauma. 4 Rib fractures can cause a variety of problems for trauma patients, including pain, difficulty breathing, impaired lung function, pneumonia and ARDS.5,6 In some cases they are accompanied by hemo- or pneumothorax, pulmonary contusion or injury to other intrathoracic organs. 3 Management ranges from simple pain to surgical treatment like intrapleural drains and rib fixation in extensive injuries.7-9 Proper management and early identification of risk factors is important to ensure the best possible outcome for the patient.
The global population of older people is rapidly increasing. According to the United Nations, the number of people in the age group 65 years or older is expected to reach almost 1.5 billion by 2030. By 2050, this number is expected to nearly double. 10 They also conduct a different lifestyle and stay active up to a high age, increasing the probability for accidents and injuries. 11
Elderly patients who sustain rib fractures from blunt chest trauma have a higher risk of mortality and pulmonary morbidity compared to younger patients with similar injuries, and the risk increases with the number of fractured ribs.12,13 Approximately 10% of elderly patients with rib fractures suffer from severe pneumonia and about 10% die.13,14
Therefore, it is important to further characterize this patient group. In this study, we aimed to examine differences in younger vs older patients with rib fractures with special attention to adverse events and mortality.
Material and Methods
The study employed a retrospective design using data from patients who sustained thoracic trauma and received treatment at a level I trauma center over a 5-year period (from 2012 to 2016). The inclusion criteria were age over 17 years and at least 1 radiologically confirmed rib fracture or pulmonary contusion. A total of 663 patients were evaluated for this study. Data on their hospitalization, including sex, age, comorbidities, insurance (statutory or private), detailed description of the chest trauma, further concomitant injuries, length of stay, hours of ventilation, chest tube insertion, performed thoracotomy, and complications were obtained from electronic patient files, the Swiss classification of operations (CHOP), and the International Classification of Diseases (ICD) codes.15,16
We excluded all patients under the age of 17 to focus our analysis on an adult population. Additionally, any cases with missing relevant information were excluded to maintain the integrity and accuracy of our dataset. Specifically, we excluded all patients who did not have complete information regarding their thoracic trauma.
We defined as outcome criteria the duration of ventilation and of hospital stay, complications (categorized into pulmonary and general complications), and mortality rates.
The extent of injury was assessed by analyzing imaging as computerized tomography scans and x-rays and operative reports. Complications were defined as certain clinical events that occurred during hospitalization, such as pneumonia, respiratory insufficiency, myocardial infarction, urinary tract infection, anemia, and complications after surgical interventions. The abbreviated injury scale (AIS) and injury severity score (ISS) were assessed by experienced trauma surgeons and were included in the analysis.17,18 The study was conducted in compliance with ethical standards, having received approval from the institutional review board (IRB) with the number (PB_2016-01888).
Statistical Analysis
To investigate the influence of age on the outcome of chest trauma, we conducted a matched pair analysis that precisely matched patients based on the same broken ribs, as well as gender. For this purpose, a 24-digit code was created (12 ribs on the left and on the right side) and a binary classification system (0 and 1) was used to indicate the presence or absence of a fracture. Based on this code and gender, a 1:1 matching was performed. The 2 groups differed with respect to age (arbitrary above and below the age of 70 years). McNemar tests for dichotomous categorical variables, McNemar-Bowker tests for more than 2 categorical variables and paired t-tests for continuous variables were used in bivariate analysis comparing the 2 matched groups (Table 1).
Table 1.
Characteristics of Matched Groups.
| Parameter | Group Under 70 (n = 70) | Group Over 70 (n = 70) | P value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age (years) | Mean ± SD | 41 ± 14 | 80 ± 6.1 | <0.001 | ||
| Insurance | Statutory | 49 | 70 | 50 | 71 | 0.856 |
| Private | 21 | 30 | 19 | 27 | ||
| Comorbidity | Yes | 23 | 33 | 49 | 70 | <0.001 |
| Injury severity score | Median (IQR) | 13 (14) | 13 (24) | 0.637 | ||
| AIS body region | Head and neck median (IQR) | 3 (4) | 4 (4) | 0.396 | ||
| face median (IQR) | 0 (0) | 0 (0) | 0.835 | |||
| Chest median (IQR) | 3 (1) | 3 (1) | 0.014 | |||
| Abdomen median (IQR) | 1 (3) | 0 (0) | 0.018 | |||
| Extremities median (IQR) | 3 (1) | 2 (3) | 0.884 | |||
| Exterior median (IQR) | 0 (1) | 1 (1) | 0.423 | |||
| Pneumothorax | Yes | 26 | 37 | 16 | 23 | 0.031 |
| Hematothorax | Yes | 11 | 16 | 17 | 24 | 0.238 |
| Lung contusion | None | 49 | 70 | 64 | 91 | 0.006 |
| One side | 10 | 14 | 5 | 7.1 | ||
| Both sides | 11 | 16 | 1 | 1.4 | ||
| Chesttube | None | 52 | 74 | 54 | 77 | 0.335 |
| One side | 13 | 19 | 15 | 21 | ||
| Both sides | 5 | 7.1 | 1 | 1.4 | ||
| Length of stay (days) | Median (IQR) | 9 (8) | 5 (10) | 0.035 | ||
| Hours of ventilation | Median (IQR) | 0 (5) | 0 (16) | 0.747 | ||
| Lung associated complications | Pneumonia | 3 | 4.3 | 9 | 13 | 0.146 |
| Respiratory insufficiency | 2 | 2.9 | 5 | 7.1 | 0.375 | |
| General complications | Myocardial infarction | 1 | 1.4 | 0 | 0 | |
| Urinary tract infection | 4 | 5.7 | 4 | 5.7 | 1.0 | |
| Anemia | 11 | 16 | 9 | 13 | 0.815 | |
| Complications of surgical interventions | 9 | 13 | 6 | 8.6 | 0.581 | |
| Reanimation | Yes | 0 | 0 | 3 | 4.3 | |
| Death | Yes | 2 | 2.9 | 13 | 19 | 0.007 |
SD: Standard Deviation; IQR: Interquartile Range; AIS: Abbreviated Injury Scale.
The second aspect of the study involved a regression analysis to identify predictors of complications. The normality of the data was assessed with the Kolmogorov-Smirnov test. Bivariate analysis was performed using the Chi-square, Mann-Whitney U and Fisher tests, where appropriate. Risk factors for complications were evaluated in a stepwise backward likelihood logistic regression analysis. Significant (P < 0.05) or nearly significant factors (P < 0.1) in bivariate analysis were selected as potential confounders. For our regression analysis for complications the Hosmer and Lemeshow test (Chi-square = 15, P = 0.068) suggested an acceptable fit of the model. Omnibus tests of model coefficients indicated the overall significance of the model in this fitted model (P < 0.001). Our model had an R-square of 0.178.
Statistical analysis was conducted using IBM SPSS version 26 (IBM, Armonk, New York, USA).
Last, we stratified the patients from under 40 years to patients with an age of over 80 years into 6 subgroups of age and analyzed them regarding the outcome criteria number of broken ribs, length of stay (days), comorbidity, general complications, hemothorax, pneumothorax, lung contusion on both sides and rib series fracture or unstable thorax.
Results
The Study Population
The study population consisted of 663 patients with a mean age of 57 ± 19 years. Of the patients, 69% were male. A total of 54% of patients had at least 1 comorbidity. The mean number of broken ribs among patients was 5.1 ± 3.9. Lung contusion was present in 21% of patients, with 136 cases, of which 65 were bilateral. Pneumothorax was present in 31% of patients, with a total of 204 cases. Hemothorax was present in 16% of patients, with a total of 109 cases. A total of 24% of patients (n = 156) underwent chest tube insertion, with 7.4% receiving bilateral chest tubes. Seven patients (1.1%) required thoracotomy.
Complications were reported in 36% of all patients (n = 241). The most frequently reported lung-associated complications were pneumonia (6.9%) and respiratory insufficiency (4.8%). The most common general complications were anemia (14%), complications following surgical interventions (11%), and urinary tract infections (5.0%). The overall mortality was 10% (n = 66) (Table 2).
Table 2.
Characteristics of Patient Cohort.
| Parameter | (n = 663) | ||
|---|---|---|---|
| n | % | ||
| Age (years) | Mean ± SD | 57 ± 19 | |
| Insurance | Statutory | 478 | 72 |
| Private | 183 | 28 | |
| Comorbidity | Yes | 358 | 54 |
| Injury severity score | Median (IQR) | 14 (14) | |
| AIS body region | Head and neck median (IQR) | 3 (3) | |
| face median (IQR) | 0 (0) | ||
| Chest median (IQR) | 3 (1) | ||
| Abdomen median (IQR) | 0 (2) | ||
| Extremities median (IQR) | 2 (3) | ||
| Exterior median (IQR) | 0 (1) | ||
| Pneumothorax | Yes | 204 | 31 |
| Hematothorax | Yes | 109 | 16 |
| Lung contusion | None | 527 | 80 |
| One side | 71 | 11 | |
| Both sides | 65 | 9.8 | |
| Number of broken ribs | Median (IQR) | 4 (5) | |
| Chesttube | None | 507 | 77 |
| One side | 107 | 16 | |
| Both sides | 49 | 7.4 | |
| Thoracotomy | Yes | 7 | 1 |
| Length of stay (days) | Median (IQR) | 8 (11) | |
| Hours of ventilation | Median (IQR) | 0 (12) | |
| Lung associated complications | Pneumonia | 46 | 6.9 |
| Respiratory insufficiency | 32 | 4.8 | |
| General complications | Myocardial infarction | 4 | 0.60 |
| Urinary tract infection | 33 | 5.0 | |
| Anemia | 90 | 14 | |
| Complications of surgical interventions | 70 | 11 | |
| Reanimation | Yes | 12 | 1.8 |
| Death | Yes | 66 | 10 |
SD: Standard Deviation; AIS: Abbreviated Injury Scale; IQR: Interquartile Range.
Matched Pair Analysis
The study found 70 matched pairs for analysis. Results indicated no significant differences between the 2 groups in terms of Injury Severity Score (ISS), insurance type, hours of ventilation, the number of chest tubes, the occurrence of hemothorax, and lung-associated and general complications. However, the younger cohort had a higher incidence of pneumothoraces and a significantly higher rate of lung contusions. In contrast, the older cohort had a significantly higher prevalence of comorbidities. The length of stay was found to be significantly longer in the younger cohort, while the elderly group had a significantly higher mortality rate (Table 1).
Deceased Patients
In the younger patient cohort, there were 2 deaths. Both of these patients sustained severe head injuries, presented with an initial Glasgow Coma Scale (GCS) score of 3, and passed away within 24 hours of admission. In the older patient cohort, there were a total of 13 deaths recorded. Seven of these fatalities were due to head injuries, 3 were attributed to hemorrhagic shock, 2 were caused by multi-organ failure, and 1 death was attributed to other causes (Table 3).
Table 3.
Characteristics Deceased Patients.
| Parameter | Deceased Group under 70 (n = 2) | Deceased Group over 70 (n = 13) | |
|---|---|---|---|
| n | n | ||
| Glasgow coma scale on entry | Mean ± SD | 3.0 ± 0 | 6.5 ± 5.0 |
| Number of broken ribs | Mean ± SD | 8.0 ± 0 | 7.5 ± 5.1 |
| Injury severity score | Mean ± SD | 71 ± 6.4 | 48 ± 23 |
| Duration intensive care unit (hours) | Mean ± SD | 18 ± 9.2 | 84 ± 136 |
| Hours of ventilation | Mean ± SD | 18 ± 9.2 | 53 ± 99 |
| Reanimation | Yes | 0 | 3 |
| Comfort care | Yes | 1 | 4 |
| Cause of death | Head injury | 2 | 7 |
| Hemorrhagic shock | 0 | 3 | |
| Multiorgan failure | 0 | 2 | |
| Other reason | 0 | 1 | |
| Deceased within 24 hours after admission | Yes | 2 | 7 |
SD: Standard Deviation.
Number of Broken Ribs, Hospital Stay, Comorbidities and Complications
We found significant differences for comorbidities (P < 0.001), number of broken ribs (P = 0.014), and Injury Severity Score (P < 0.001). There were no significant differences for age over 70 vs under 70 years (P = 0.091), sex (P = 0.127), and insurance status (P = 0.695) (Table 5).
Table 5.
Predictors of complications
| Parameter | p-value | Odds ratio | 95% confidence interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Comorbidities yes vs. no | <0.001 |
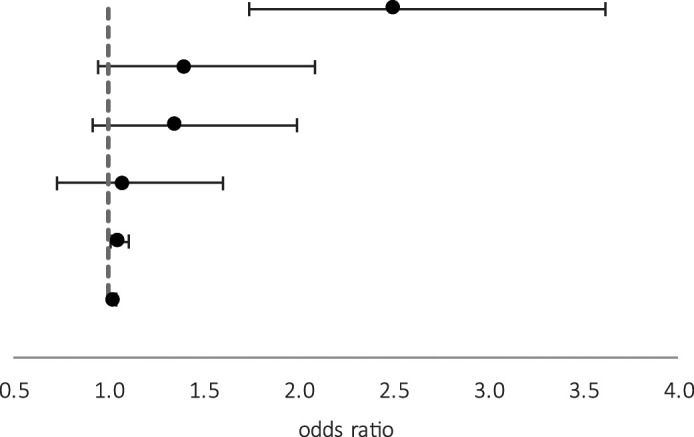
|
2.510 | 1.742 | 3.618 |
| Age over 70 years vs. age under 70 years | 0.091 | 1.406 | 0.947 | 2.089 | |
| Sex male vs. female | 0.127 | 1.353 | 0.918 | 1.994 | |
| Insurance status public vs. private | 0.695 | 1.082 | 0.730 | 1.604 | |
| Number of broken ribs | 0.014 | 1.059 | 1.011 | 1.108 | |
| Injury Severity Score | <0.001 | 1.031 | 1.019 | 1.042 | |
There was a general trend of an increase in the mean number of broken ribs with the age, peaking at 6.0 ± 6.9 for those 70-80 years old. The length of hospital stay was variable, with the longest duration observed in the 60-70 years category (15 ± 24 days). In contrast the >80 age group averaged the shortest stay of 7.8 ± 7.9 days (Table 4).
Table 4.
Influence of Age on Outcome.
| Parameter | Age (in years) | ||||||
|---|---|---|---|---|---|---|---|
| Under 40 | 40 - 50 | 50 - 60 | 60 - 70 | 70 - 80 | Over 80 | ||
| Number of broken ribs | Mean ± SD | 3.9 ± 3.2 | 4.8 ± 3.4 | 5.2 ± 4.0 | 5.8 ± 4.1 | 6.0 ± 6.9 | 5.3 ± 4.5 |
| Length of stay (days) | Mean ± SD | 12 ± 17 | 11 ± 10 | 11 ± 10 | 15 ± 24 | 9.7 ± 9.5 | 7.8 ± 7.6 |
| Comorbidity | % Yes | 30 | 40 | 51 | 65 | 67 | 83 |
| General complications | % Yes | 35 | 27 | 32 | 38 | 43 | 49 |
| Hematothorax | % Yes | 11 | 15 | 19 | 17 | 22 | 17 |
| Pneumothorax | % Yes | 41 | 33 | 31 | 30 | 28 | 17 |
| Lung contusion on both sides | % Yes | 18 | 12 | 10 | 7.2 | 5.7 | 3.4 |
| Rib series fracture or unstable throax | % Yes | 62 | 73 | 69 | 75 | 77 | 72 |
SD: Standard Deviation.
Comorbidities and Complications
The prevalence of comorbidities amplified with age, with the <80 years cohort indicating the highest at 83%. General complications showed a slight increase with age, peaking at 49% in the <80 years category (Table 4).
Specific Thoracic Injuries
Hemothorax presented most frequently in 70-80 age cohort (22%), whereas pneumothorax was most prevalent in the <40 age group (41%). The incidence of bilateral lung contusions decreased consistently with age, being most prominent in the <40 years group (18%) and least in the <80 years group (3.4%). Rib series fractures or unstable thorax were frequently observed across all age groups, with the 70-80 years cohort showcasing the highest incidence at 77%.
Regression Analysis
In a multivariate regression analysis, the presence of comorbidities, the absolute number of broken ribs, and the ISS were found to be significant predictors of general and postoperative complications (R square = 0.18) (Table 5).
We excluded reanimation in the regression analysis for mortality due to the high association with mortality. The analysis found complications, age, Injury Severity Score and length of stay as significant predictors for mortality (all with a P < 0.001) (Table 6).
Table 6.
Predictors of Mortality.
| Parameter | P-value | Odds Ratio | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Complications yes vs. no | <0.001 |
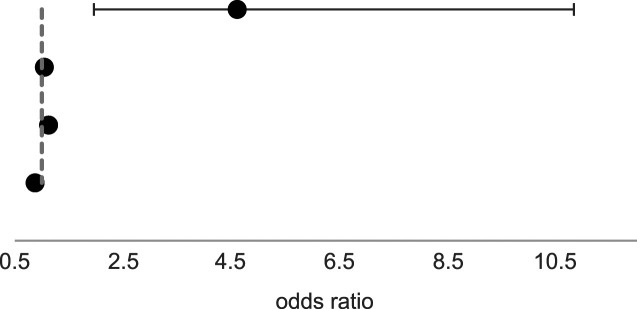
|
4.611 | 1.962 | 10.83 |
| Age | <0.001 | 1.047 | 1.023 | 1.070 | |
| Injury severity score | <0.001 | 1.125 | 1.095 | 1.155 | |
| Length of stay (days) | <0.001 | 0.875 | 0.827 | 0.925 | |
For our regression analysis for mortality the Hosmer and Lemeshow test showed a Chi-square of 5.4 and a P = 0.718. Omnibus tests of model coefficients indicated the overall significance of the model in this fitted model (P < 0.001). Our model had an R-square of 0.625.
Discussion
The aim of this study was to evaluate the impact of age on outcome in patients with chest trauma. Our results indicated that the elderly patient was overall sicker with a higher prevalence of preexisting conditions. Elderly patients had different injury patterns than their younger counterparts with fewer pneumothoraces and lung contusions. The mean ISS and complication rate did not show significant differences between the groups. Nevertheless, the geriatric group had a trend towards a higher mortality rate. We found comorbidities, ISS and number of broken ribs to be predictive for adverse outcome.
There are some limitations to this study that must be considered when interpreting its findings. We used retrospective data for this analysis, so data not included in the first place could not be obtained. Secondly, the study is limited to a single level I trauma center, which may limit the generalizability of the results. The findings may not be applicable to other populations or medical systems with different patient demographics, treatment practices, or resource availability. The retrospectively collected data may be partially incomplete, leading to potential missing information that could affect the results. Furthermore, the study may not have considered all relevant confounding variables, such as patient-specific factors, medical history, and social determinants of health that could have impacted the results.
In Addition we had no sufficient information on the mechanism of injury to perform further analysis.
We observed different injury patterns in the 2 cohorts. Younger patients displayed a higher incidence for pneumothoraces and lung contusions, but there was no significant difference in the ISS. Our findings are consistent with previous research indicating a higher prevalence of lung contusions in younger patients, 19 while rib fractures of elderly patients result more often from low energy trauma and result in a lower incidence of lung contusions20,21).
It is notable that the overall length of hospital stay was significantly longer for the younger patient population. A factor playing into that might be the 7 elderly patients that died within 24 hours of admission (Table 3). This unexpected result might also be influenced by different inclusion criteria in the other studies, for example only thoracic mono trauma. 22
Our data showed a higher mortality rate among elderly patients. However, 7 out of the 13 deceased patients in the elderly group and both deceased younger patients died due to severe head trauma. According to Marini et al, data indicates that among patients between the ages of 16 and 75 with rib fractures, severe traumatic brain injury is the primary cause of death. Conversely, for individuals over 80 years of age with rib fractures, respiratory complications are the most frequent cause of mortality.6,12,23-25
Our data did not show a significant difference in overall complications in the different age cohorts. This concurs with the results of another matched-pair analysis that focused on pneumonia as a complication of blunt thoracic trauma. 26
In a subanalysis we found a delirium rate in our older cohort of 10%. Among patients over 70 with rib fractures, those experiencing delirium had an average hospital stay of 20 days, compared to 7.5 days for those without delirium. Delirium patients also had higher rates of: haematothorax (33% vs 18%) and lung contusion (22% vs 7.6%). The frequency of pneumothorax was similar in both groups.
We found ISS, number of fractured ribs and comorbidities to be predictors for adverse outcome. The literature on prognostic factors for adverse outcomes is sparse.13,27
Previous studies have established that the number of fractured ribs is a reliable predictor of mortality and complications.28-30 This finding is reflected in various scoring systems designed to predict outcome after thoracic injury, which consider the presence and pattern of rib fractures.31-35
The finding of comorbidities being a predictor for complications rather than numeric age agrees with the term of frailty being increasingly discussed as a good indicator for outcome in geriatric patients.36-38 However, our study did not systematically assess frailty, so we cannot make a definitive statement on this issue.
The higher mortality among elderly patients and the predictive power of comorbidities suggests the importance of tailored treatment approaches, which have been shown to be beneficial.39,40 Nevertheless, accurately identifying frailty can be challenging. The available scoring systems to this point use numeric age rather than frailty for predicting outcome.41-43 Chen et al. described the Chest Trauma Score (CTS), which includes among other factors the numeric patient´s age. 31 A score ≥5 can predict a poorer outcome and is associated with increased mortality. 44 The CTS is also recommended especially for geriatric patients as it predicts pneumonia well 45 and may assist to evaluate early intensified focused care.
In this study we provided a stratification of small age groups with parameters describing the outcome of rib fractures, which shows interesting varieties in terms of complications or number of broken ribs within older age groups (Table 4). For example, did the amount of rib fractures increased the older the patients got up to 80 years, but decreased then at over 80 years, while general complications increased with increasing age.
This enhances the need for a further observation within stratified age groups, especially if the trend towards higher mortality rate in older age would alter after application of a score like CTS and its consequences like early intensified care.
As demographic trends shift, this may be a promising area for future research.
Conclusion
The management of thoracic trauma in elderly patients with multiple comorbidities poses unique challenges.
Our results show that numeric age may not be the most accurate predictor of adverse outcome in terms of length of stay, hours of ventilation and complications. But we found that higher age was associated with a clear trend towards an increased mortality rate.
Our findings build a basis for further research to evaluate the influence of age on outcome for instance with the tool of a rib fracture scoring system within stratified age groups.
The application of a score may help to evaluate patients with rib fractures objectively and provide a sensibilization for closer follow-ups and expedite therapeutical interventions in specified older age groups in clinical practice.
Footnotes
Author’s Note: Statement of location where the work was performed: Division of Trauma Surgery, University Hospital Zurich (USZ), University of Zurich (UZH), Raemistrasse 100, 8091 Zuerich, Switzerland.
Author Contributions: Franziska Ziegenhain, Dr med.: data acquisition, writing and analysis
Anne Sophie Mittlmeier: writing and analysis
Hans-Christoph Pape, Prof. Dr med.: concept and writing
Valentin Neuhaus, Prof. Dr med.: concept and writing
Claudio Canal, Dr med: writing, analysis and concept
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Statement
Ethical Approval
This retrospective cohort study was approved by the local ethics committee (Kantonale Ethikkommission Zürich, Switzerland, KEK ZH No. PB_2016-01888).
Informed Consent
The study was conducted in compliance with ethical standards, having received approval from the institutional review board (IRB) with the number (PB_2016-01888).
ORCID iDs
Anne S. Mittlmeier https://orcid.org/0009-0001-5026-5766
Valentin Neuhaus https://orcid.org/0000-0003-4012-5628
Claudio Canal https://orcid.org/0000-0002-6486-2481
References
- 1.Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43(1):8-17. doi: 10.1016/j.injury.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 2.Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. Am J Surg. 2013;205(5):511-515. doi: 10.1016/j.amjsurg.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 3.Lundin A, Akram SK, Berg L, Göransson KE, Enocson A. Thoracic injuries in trauma patients: epidemiology and its influence on mortality. Scand J Trauma Resuscitation Emerg Med. 2022;30(1):69. doi: 10.1186/s13049-022-01058-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haines KL, Zens T, Warner-Hillard C, DeSouza E, Jung HS, Agarwal S. Rib fracture location should Be evaluated when predicting morbidity and mortality in trauma patients. Am Surg. 2018;84(9):1462-1465. [PubMed] [Google Scholar]
- 5.Acker A, Brotfain E, Koyfman L, et al. Clinical outcomes of critically ill multiple trauma patients with rib fractures. A prospective study with retrospective control. Anaesthesiol Intensive Ther. 2021;53(1):25-29. doi: 10.5114/ait.2020.103510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marini CP, Petrone P, Soto-Sánchez A, García-Santos E, Stoller C, Verde J. Predictors of mortality in patients with rib fractures. Eur J Trauma Emerg Surg. 2021;47(5):1527-1534. doi: 10.1007/s00068-019-01183-5 [DOI] [PubMed] [Google Scholar]
- 7.Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110(6):1676-1680. doi: 10.1016/S0022-5223(95)70030-7 [DOI] [PubMed] [Google Scholar]
- 8.Klei DS, Oner FC, Leenen LPH, van Wessem KJP. Current treatment and outcomes of traumatic sternovertebral fractures: a systematic review. Eur J Trauma Emerg Surg. 2020. doi: 10.1007/s00068-020-01505-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Long R, Tian J, Wu S, Li Y, Yang X, Fei J. Clinical efficacy of surgical versus conservative treatment for multiple rib fractures: a meta-analysis of randomized controlled trials. Int J Surg. 2020;83:79-88. doi: 10.1016/j.ijsu.2020.09.010 [DOI] [PubMed] [Google Scholar]
- 10.Nations Department of Economic U., Social Affairs, Population Division. World Population Ageing 2019; 2020. (ST/ESA/SER.A/444).
- 11.Older People in Germany and the EU. 2016. [Google Scholar]
- 12.Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040-1046. doi: 10.1097/00005373-200006000-00007 [DOI] [PubMed] [Google Scholar]
- 13.Barry R, Thompson E. Outcomes after rib fractures in geriatric blunt trauma patients. Am J Surg. 2018;215(6):1020-1023. doi: 10.1016/j.amjsurg.2018.03.011 [DOI] [PubMed] [Google Scholar]
- 14.Van Vledder MG, Kwakernaak V, Hagenaars T, Van Lieshout EMM, Verhofstad MHJ, South West Netherlands Trauma Region Study Group . Patterns of injury and outcomes in the elderly patient with rib fractures: a multicenter observational study. Eur J Trauma Emerg Surg. 2019;45(4):575-583. doi: 10.1007/s00068-018-0969-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.(BFS) BfS . In: (BFS) BfS, ed. Schweizerische Operationsklassifikation (CHOP). Neuchatel: Bundesamt für Statistik (BFS); 2021. [Google Scholar]
- 16.World Health O. ICD-10: International Statistical Classification of Diseases and Related Health Problems : Tenth Revision. 2nd ed. Geneva: World Health Organization; 2004. [Google Scholar]
- 17.Baker SP, o'Neill B, Haddon JW, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma Acute Care Surg. 1974;14(3):187-196. [PubMed] [Google Scholar]
- 18.Abbreviated Injury Scale: 2015 Revision (6 ed.). Association for the Advancement of Automotive Medicine; 2016. Accessed August 30, 2024. https://www.aaam.org/abbreviated-injury-scale-ais/
- 19.Schulz-Drost S, Finkbeiner R, Lefering R, et al. Lung contusion in polytrauma: an analysis of the TraumaRegister DGU. Thorac Cardiovasc Surg. 2021;69(8):735-748. doi: 10.1055/s-0039-1700505 [DOI] [PubMed] [Google Scholar]
- 20.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50(1):116-119. [DOI] [PubMed] [Google Scholar]
- 21.Prins JTH, Van Lieshout EMM, Reijnders MRL, Verhofstad MHJ, Wijffels MME. Rib fractures after blunt thoracic trauma in patients with normal versus diminished bone mineral density: a retrospective cohort study. Osteoporos Int. 2019;31(2):225-231. doi: 10.1007/s00198-019-05219-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shi HH, Esquivel M, Staudenmayer KL, Spain DA. Effects of mechanism of injury and patient age on outcomes in geriatric rib fracture patients. Trauma Surg Acute Care Open. 2017;2(1):e000074. doi: 10.1136/tsaco-2016-000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed N, Kuo YH. Evaluating the outcomes of blunt thoracic trauma in elderly patients following a fall from a ground level: higher level care institution vs. lower level care institution. Eur J Trauma Emerg Surg. 2021;47(4):955-963. doi: 10.1007/s00068-019-01230-1 [DOI] [PubMed] [Google Scholar]
- 24.Elgar G, Smiley A, Latifi R. Major risk factors for mortality in elderly and non-elderly adult patients emergently admitted for blunt chest wall trauma: hospital length of stay as an independent predictor. Int J Environ Res Publ Health. 2022;19(14):8729. doi: 10.3390/ijerph19148729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardio Thorac Surg. 2003;23(3):374-378. doi: 10.1016/s1010-7940(02)00813-8 [DOI] [PubMed] [Google Scholar]
- 26.Marco CA, Sorensen D, Hardman C, Bowers B, Holmes J, McCarthy MC. Risk factors for pneumonia following rib fractures. Am J Emerg Med. 2020;38(3):610-612. doi: 10.1016/j.ajem.2019.10.021 [DOI] [PubMed] [Google Scholar]
- 27.Sawa J, Green RS, Thoma B, Erdogan M, Davis PJ. Risk factors for adverse outcomes in older adults with blunt chest trauma: a systematic review. Cjem. 2018;20(4):614-622. doi: 10.1017/cem.2017.377 [DOI] [PubMed] [Google Scholar]
- 28.Flagel BT, Luchette FA, Reed RL, et al. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138(4):717-723. doi: 10.1016/j.surg.2005.07.022 [DOI] [PubMed] [Google Scholar]
- 29.O'Donovan S, van den Heuvel C, Baldock M, Humphries MA, Byard RW. Fatal blunt chest trauma: an evaluation of rib fracture patterns and age. Int J Leg Med. 2022;136(5):1351-1357. doi: 10.1007/s00414-022-02866-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shulzhenko NO, Zens TJ, Beems MV, et al. Number of rib fractures thresholds independently predict worse outcomes in older patients with blunt trauma. Surgery. 2017;161(4):1083-1089. doi: 10.1016/j.surg.2016.10.018 [DOI] [PubMed] [Google Scholar]
- 31.Chen J, Jeremitsky E, Philp F, Fry W, Smith RS. A chest trauma scoring system to predict outcomes. Surgery. 2014;156(4):988-993. doi: 10.1016/j.surg.2014.06.045 [DOI] [PubMed] [Google Scholar]
- 32.Mommsen P, Zeckey C, Andruszkow H, et al. Comparison of different thoracic trauma scoring systems in regards to prediction of post-traumatic complications and outcome in blunt chest trauma. J Surg Res. 2012;176(1):239-247. doi: 10.1016/j.jss.2011.09.018 [DOI] [PubMed] [Google Scholar]
- 33.Chapman BC, Herbert B, Rodil M, et al. RibScore: a novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg. 2016;80(1):95-101. doi: 10.1097/TA.0000000000000867 [DOI] [PubMed] [Google Scholar]
- 34.Baker JE, Millar DA, Heh V, Goodman MD, Pritts TA, Janowak CF. Does chest wall Organ Injury Scale (OIS) or Abbreviated Injury Scale (AIS) predict outcomes? An analysis of 16,000 consecutive rib fractures. Surgery. 2020;168(1):198-204. doi: 10.1016/j.surg.2020.04.032 [DOI] [PubMed] [Google Scholar]
- 35.Choi J, Marafino BJ, Vendrow EB, et al. Rib Fracture Frailty Index: a risk stratification tool for geriatric patients with multiple rib fractures. J Trauma Acute Care Surg. 2021;91(6):932-939. doi: 10.1097/ta.0000000000003390 [DOI] [PubMed] [Google Scholar]
- 36.Maxwell CA, Patel MB, Suarez-Rodriguez LC, Miller RS. Frailty and prognostication in geriatric Surgery and trauma. Clin Geriatr Med. 2019;35(1):13-26. doi: 10.1016/j.cger.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 37.Panza F, Sardone R, Dibello V, Daniele A, Solfrizzi V, Lozupone M. Frailty and outcome after traumatic brain injury. Lancet Neurol. 2022;21(2):107-108. doi: 10.1016/S1474-4422(21)00418-X [DOI] [PubMed] [Google Scholar]
- 38.Pecheva M, Phillips M, Hull P, Carrothers A OR, Queally JM. The impact of frailty in major trauma in older patients. Injury. 2020;51(7):1536-1542. doi: 10.1016/j.injury.2020.04.045 [DOI] [PubMed] [Google Scholar]
- 39.Pyke OJ, Jr., Rubano JA, Vosswinkel JA, McCormack JE, Huang EC, Jawa RS. Admission of elderly blunt thoracic trauma patients directly to the intensive care unit improves outcomes. J Surg Res. 2017;219:334-340. doi: 10.1016/j.jss.2017.06.054 [DOI] [PubMed] [Google Scholar]
- 40.Sahr SM, Webb ML, Renner CH, Sokol RK, Swegle JR. Implementation of a rib fracture triage protocol in elderly trauma patients. J Trauma Nurs. 2013;20(4):172-175. doi: 10.1097/JTN.0000000000000008 [DOI] [PubMed] [Google Scholar]
- 41.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49(3):496-504. doi: 10.1097/00005373-200009000-00018 [DOI] [PubMed] [Google Scholar]
- 42.Moore EE, Cogbill TH, Jurkovich GJ, et al. Organ injury scaling III: chest wall, abdominal vascular, ureter, bladder, and urethra. J Trauma. 1992;33(3):337-339. [PubMed] [Google Scholar]
- 43.Maxwell CA, Mion LC, Dietrich MS. Hospitalized injured older adults: clinical utility of a rib fracture scoring system. J Trauma Nurs. 2012;19(3):168-174. doi: 10.1097/JTN.0b013e318261d201 [DOI] [PubMed] [Google Scholar]
- 44.Harde M, Aditya G, Dave S. Prediction of outcomes in chest trauma patients using chest trauma scoring system: a prospective observational study. Indian J Anaesth. 2019;63(3):194-199. doi: 10.4103/ija.IJA_750_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fokin A, Wycech J, Crawford M, Puente I. Quantification of rib fractures by different scoring systems. J Surg Res. 2018;229:1-8. doi: 10.1016/j.jss.2018.03.025 [DOI] [PubMed] [Google Scholar]


