Abstract
Objective
To investigate the feasibility of poststroke interventions using a motivational instructional design model with occupational therapy (OT) and swallowing therapy (ST) and the model's potential physical and mental health effects.
Design
An open-label, single-arm, feasibility study on the Attention, Relevance, Confidence, and Satisfaction model.
Setting
Two convalescent rehabilitation wards.
Participants
Twenty-five patients with stroke (N=25) (19 men; mean age, 62.4±11.9y; 61.9±36.8d from the first stroke) were recruited.
Interventions
Twelve participants received a motivational approach based on the Attention, Relevance, Confidence, and Satisfaction model during OT (OT group), and 13 received it during ST (ST group). The intervention lasted 40-60 minutes daily, 5 days weekly, for 4 weeks.
Main Outcome Measures
The primary outcomes included the dropout rate, an adverse event, and the participants’ acceptability of the intervention. Paretic arm function was assessed in the OT group; swallowing ability was assessed in the ST group; and activities of daily living, depressive symptoms, and apathy were assessed in both groups.
Results
No participants dropped out of the intervention or experienced an adverse event. Twenty-one participants (84%) were satisfied with the intervention, and 19 (76%) hoped to continue receiving it. The OT group showed statistically significant improvements in paretic arm function and activities of daily living (Cohen's r=0.68-0.77), whereas the ST group improved in swallowing ability, activities of daily living, and depressive symptoms (Cohen's r=0.62-0.85).
Conclusions
The interventions using the motivational instructional model with OT and ST were feasible and could improve poststroke paretic arm function, swallowing ability, and activities of daily living after stroke.
KEYWORDS: Cerebrovascular disease, Educational technology, Motivation, Rehabilitation
Stroke is a primary cause of disability and requires continuous care.1 Rehabilitation is recommended to promote poststroke functional recovery, enhance independence in daily activities, and improve quality of life.2 For example, task-specific training for upper-extremity function, such as constraint-induced movement therapy and mental practice, and functional task training to improve the activities of daily living (ADLs) and social participation are provided in occupational therapy (OT).2,3 In addition, swallowing therapy (ST) for patients with dysphagia includes compensatory strategies, such as modifying fluid and food consistencies or feeding posture, and rehabilitative approaches involving swallowing exercise or skill training.4 The independent efforts of the patient are essential to continue receiving these therapies. Therefore, motivation, a “mental function that produces the incentive to act; the conscious or unconscious driving force for action,”5 may be associated with improved poststroke functional recovery.6, 7, 8
Motivation for rehabilitation programs is a dynamic condition rather than a static quality.9 Social factors and patients’ personalities or clinical characteristics are possible determinants of motivation for rehabilitation.9, 10, 11, 12 For example, negative experiences and rehabilitation perceptions, such as boredom, low self-efficacy, and inadequate knowledge about the benefits of exercise, may decrease motivation.9, 10, 11 Notably, various motivational interventions, such as motivational interviewing and goal setting, are used in stroke rehabilitation13, 14, 15, 16, 17, 18, 19; however, there is insufficient evidence indicating that they improve rehabilitation outcomes.20,21 Therefore, developing additional strategies to improve patient motivation and outcomes is essential.
The Attention, Relevance, Confidence, and Satisfaction (ARCS) model is a motivational instructional design model that structurally presents policies and procedures on how educators should design learning environments to motivate students to learn based on motivational theories.22,23 It is currently applied to various fields, such as engineering, pharmacy, and nursing.24, 25, 26, 27, 28, 29 Regarding rehabilitation, only one study has used the ARCS model for patient education on fall prevention.24 The ARCS model helps educators identify the component of instruction that affects student motivation and determine strategies for solving motivational challenges in instructional materials and methods; therefore, it may also help therapists increase patient adherence to rehabilitation.16,19 However, to our knowledge, no study has used this model to motivate patients during rehabilitation programs. Therefore, we aimed to investigate the feasibility of an intervention using the motivational instructional design model with OT and ST and its potential effects on physical and mental health outcomes.
Methods
Study design
This was an open-label, single-arm feasibility study. The study protocol was approved by the appropriate ethics committees at the 2 hospitals (approval numbers: 216-2 and 18-62). All participants provided written informed consent before enrollment in the study. The study was conducted following the Declaration of Helsinki of 1964, as revised in 2013. The study protocol was preregistered in the University Hospital Medical Information Network.
Study setting
This study was conducted in convalescent rehabilitation wards. Intensive rehabilitation programs to increase the likelihood of home discharge are provided in the wards for patients who still need assistance in ADLs after acute treatment.30 Notably, all study participants underwent one-on-one conventional inpatient daily rehabilitation, including 40-60 minutes of physical therapy and OT. Additionally, participants with dysphagia received 40 minutes of ST, 5 days weekly. OT included task-specific training and functional task practice. ST included compensatory strategies and rehabilitative approaches.
Participants
Patients were consecutively recruited from 2 hospitals between August 2019 and March 2022. Patients in 1 of the 2 hospitals received the intervention using the ARCS model with OT (OT group), and those in the other hospital underwent the intervention using the ARCS model with ST (ST group). The inclusion criteria for both groups were age 40-90 years, being within 180 days of first-ever stroke, having received OT or ST for at least 1 week after admission, scheduled for hospitalization for at least 4 weeks in the future during screening, and a Mini-Mental State Examination score of ≥24 points.24,31 An additional inclusion criterion for participants in the OT group was having unilateral upper-extremity motor paralysis, defined using a score of <66 points in the upper-extremity motor subscale of the Fugl-Meyer assessment because a maximum score of 66 indicates no impairment.32 An additional inclusion criterion for participants in the ST group was having dysphagia, defined using a Food Intake Level Scale (FILS) score of <9 points.33 The FILS has been validated on the Functional Oral Intake Scale (ρ=0.96-0.99).33 In addition, the intrarater reliability for the FILS was excellent, ranging from 0.83 to 0.97, although the intrarater reliability for the Functional Oral Intake Scale has not been reported.33 Furthermore, the FILS may be theoretically more sensitive to changes in the oral intake of food and liquid over time, as it includes 10 items compared to the 7 items in the Functional Oral Intake Scale. Participants were excluded if they had mental impairment hindering their compliance or any comorbid neurologic disorders. Potentially eligible participants were identified through medical records reviewed by a researcher at each hospital (second and third authors). Demographic and clinical data, such as age and stroke type, were obtained from patient medical records.
Intervention
The intervention was to explicitly motivate participants using the ARCS model during inpatient daily OT and ST sessions. The ARCS model was used to assess the participants’ motivational challenges and design motivational strategies, which were implemented in both groups during the 5-day weekly therapy sessions.
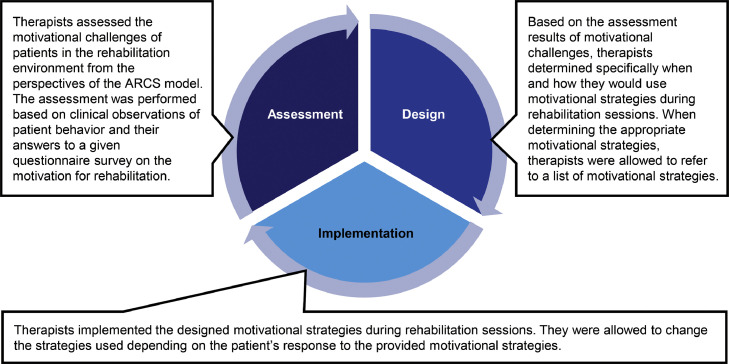
The intervention comprised an iterative process with a cycle of assessing motivational challenges, designing motivational strategies, and implementing them (fig 1), which lasted 4 weeks and consisted of 20 therapy sessions.
Fig 1.
Intervention involving the application of the ARCS model of motivational instructional design to rehabilitation.
Assessment of motivational challenges
Therapists assessed the motivational challenges of patients in the rehabilitation environment from 4 perspectives, shown as the 4 statements in box 1. The assessment was performed based on the clinical observations of patient behavior and their answers to a given questionnaire survey on the motivation for rehabilitation. The survey included 4 items corresponding to the 4 dimensions of the ARCS model. Each item was rated on a 5-point Likert scale that ranges from 1 to 5 (1=strongly disagree, 2=disagree, 3=uncertain, 4=agree, 5=strongly agree). In addition, the sum of the scores of the 4 items was calculated as the motivation level score. The questionnaire given to participants in the OT group is shown in box 1. The assessment was conducted at baseline and the end of the 5th, 10th, 15th, and 20th therapy sessions.
Box 1.
A survey presented to participants in the OT group.
| Below are statements regarding your experiences and perceptions of occupational therapy programs provided by me within the past 7 days. Please read each one and indicate to what extent you agree or disagree with each statement. |
|
Statement 1: I was interested in the provided occupational therapy programs. ○ strongly disagree ○ disagree ○ uncertain ○ agree ○ strongly agree |
|
Statement 2: I understood the relevance of the provided occupational therapy programs to my goals and needs. ○ strongly disagree ○ disagree ○ uncertain ○ agree ○ strongly agree |
|
Statement 3: I had the confidence to accomplish the provided occupational therapy programs. ○ strongly disagree ○ disagree ○ uncertain ○ agree ○ strongly agree |
|
Statement 4: I was satisfied with the provided occupational therapy programs. ○ strongly disagree ○ disagree ○ uncertain ○ agree ○ strongly agree |
NOTE. Participants in the ST group were given a survey in which “occupational therapy” was replaced by “swallowing therapy.”
Design of motivational strategies
Based on the assessment results of motivational challenges, therapists determined specifically when and how to use motivational strategies during therapy sessions. This procedure was performed at baseline and the end of the 5th, 10th, and 15th therapy sessions. In this study, motivational strategies were defined as concrete tactics, techniques, or approaches to orient patients on rehabilitation by solving motivational challenges.17 Therapists were allowed to refer to a list of motivational strategies (table 1) when determining appropriate ones. The first author initially developed the list based on data from the educational literature on the ARCS model,22,23,25,29,34 semistructured interviews with physical therapists,35 and our previous study on motivational strategies for stroke rehabilitation.18 Finally, the first and last authors who learned about the ARCS model completed the list after reviewing the contents for clarity and relevance. Examples of the design of motivational strategies based on the motivational challenges are provided in supplemental table S1 (available online only at http://www.archives-pmr.org/).
Table 1.
List of motivational strategies based on the ARCS model.
| Categories | Subcategories | Examples of Motivational Strategies |
|---|---|---|
| Attention | Perceptual arousal ie, capturing the patient's interest |
• Engaging in pleasant conversation with the patient to help him/her enjoy the rehabilitation process. • Providing a suitable rehabilitation environment so that the patient can comfortably engage in the practice. |
| Inquiry arousal ie, stimulating the patient's inquiry |
• Allowing the patient to consider how he/she could successfully perform the provided practice tasks. | |
| Variability ie, maintaining the patient's attention |
• Providing rehabilitation programs with variations. | |
| Relevance | Goal orientation ie, meeting the patient's needs/goals |
• Providing the patient with the practice tasks that are related to his/her rehabilitation goal. • Explaining the necessity of practice to the patient. |
| Motive matching ie, matching the patient's interests and learning styles |
• Offering a group rehabilitation program. • Providing the patient with rehabilitation programs that have game-like properties, such as virtual reality. |
|
| Familiarity ie, creating links to patient experiences |
• Applying patient preferences, such as hobbies, to practice tasks. • Providing practice tasks that the patient can complete using his/her previous experience. |
|
| Confidence | Learning requirements ie, developing a positive expectation for success |
• Setting rehabilitation goals that are perceived by both the therapist and the patient as relevant and achievable. • Providing verbal and/or visual feedback regarding the results of the practice to the patient. |
| Success opportunities ie, supporting or enhancing the patient's belief in his/her competence |
• Gradually increasing the difficulty of a task according to the ability of the patient. | |
| Personal responsibility ie, establishing the patient's effort and ability as his/her basis for success |
• Respecting the patient's self-determination. | |
| Satisfaction | Natural consequences ie, intrinsic reinforcement |
• Recommending the patient use tools such as a diary or graphs that enable him/her to track his/her progress. • Providing opportunities to use newly acquired skills through rehabilitation practices. |
| Positive consequences ie, extrinsic rewards |
• Providing the patient with positive evaluations and encouragement. • Promising that the patient can do his/her favorite practice tasks after completing his/her least favorite practice task. |
|
| Equity ie, demonstrating fair treatment among patients |
• Sharing the criteria for evaluation with the patient. |
Implementation of motivational strategies
Therapists implemented the designed motivational strategies during therapy sessions and could change them depending on the patient's response.
Therapist training in delivering the intervention
All therapists received 2 sessions of 60-minute training in delivering the intervention by the first and last authors before starting participant enrollment. On training day 1, they learned the concept of the ARCS model. On day 2, they practiced procedures for determining motivational strategies using the ARCS model. To assess the reliability of the therapists’ ability to use the model, we asked therapists to report to the researchers via email weekly on the design and implementation of motivational strategies in the intervention over the previous week. The therapists received corrective feedback if appropriate motivational strategies were not designed based on the participants’ motivational challenges.
Outcome measures
The primary outcome was feasibility, including the dropout rate, an adverse event, and the participants’ acceptability of the intervention.36,37 In addition, physical and mental health outcomes were evaluated within 3 days before and after the intervention. The same therapist performed the assessments and the intervention for each participant.
Primary outcome
Therapists recorded the occurrence of dropouts and an adverse event as these occurred during the intervention period. To assess the acceptability of the intervention, the participants were asked to rate the 2 items on satisfaction with the intervention and intention to continue receiving it using a 5-point Likert scale ranging from “strongly disagree” to “strongly agree” within 3 days after the intervention (box 2). To quantitatively assess acceptability, we set our threshold as at least 75% of the overall participants answering “agree” or “strongly agree” to the 2 items.38
Box 2.
Survey to assess the participants’ acceptability of the intervention.
| Below are statements regarding your acceptability of the intervention provided in this study. Please read each one and indicate to what extent you agree or disagree with each statement. |
|
Statement 1: I am satisfied with the intervention. ○ strongly disagree ○ disagree ○ neither agree nor disagree ○ agree ○ strongly agree |
|
Statement 2: I hope to continue receiving the intervention. ○ strongly disagree ○ disagree ○ neither agree nor disagree ○ agree ○ strongly agree |
Physical and mental health outcomes
Physical outcomes included motor function of the paretic upper extremity, swallowing ability, and ADLs. The motor function of the paretic upper extremity was assessed in the OT group using the Motor Activity Log amount of use and quality of movement scales,39 swallowing ability in the ST group was assessed using the Mann Assessment of Swallowing Ability and the FILS,33,40 and the degrees of independence in ADLs in both groups were evaluated using the motor subscale of the Functional Independence Measure (FIM).41 Mental health outcomes, including depressive symptoms and apathy, were assessed in both groups using the Self-rating Depression Scale (SDS)42 and the Apathy Scale,43 respectively. An SDS score of ≥50 points indicated depressive symptoms.44 An Apathy Scale score of ≥14 points indicated having an apathy.43
Statistical analyses
There is little consensus on the appropriate sample size for a feasibility study.45 According to a previous study,46 a sample of 24 participants (12 per group) was required to provide useful information about the feasibility aspects of the study.
We used descriptive statistics to characterize the study sample and summarize the feasibility outcomes. Participants’ characteristics were compared between the groups using the unpaired t test for continuous variables and Fisher exact test for dichotomous variables. The Friedman test was also used to examine changes in the motivation level score during the intervention. To compare physical and mental health outcomes before and after the intervention, we used the Wilcoxon signed-rank test and calculated Cohen's r as a measure of the effect size, where 0.1 is considered a small effect size, 0.3 is considered a medium effect size, and 0.5 is considered a large effect size.47 Statistical analyses were performed using the Statistical Package for the Social Sciences software, version 27.0.a Statistical significance was set at 2-sided p<.05.
Results
Participants
Twenty-five patients with stroke participated in this study, 12 of whom were in the OT group. The participants’ characteristics are presented in table 2. The 2 groups showed no significant differences in the participants’ characteristics.
Table 2.
Participants’ characteristics.
| Variable | Overall (N=25) | OT Group (n=12) | ST Group (n=13) | P Value |
|---|---|---|---|---|
| Age (y) | 62.4±11.9 | 61.2±13.3 | 63.6±11.1 | .62* |
| Sex, male/female | 19/6 | 9/3 | 10/3 | .99† |
| Type of stroke, ischemic/hemorrhage | 14/11 | 7/5 | 7/6 | .99† |
| Side of motor paresis, right/left | 12/13 | 6/6 | 6/7 | .99† |
| Time since stroke (d) | 61.9±36.8 | 65.2±29.7 | 58.8±43.4 | .68* |
NOTE. Values are presented as mean ± SD and number. P values indicate significant differences between the OT and ST groups.
Unpaired t test.
Fisher exact test.
Feasibility of the intervention
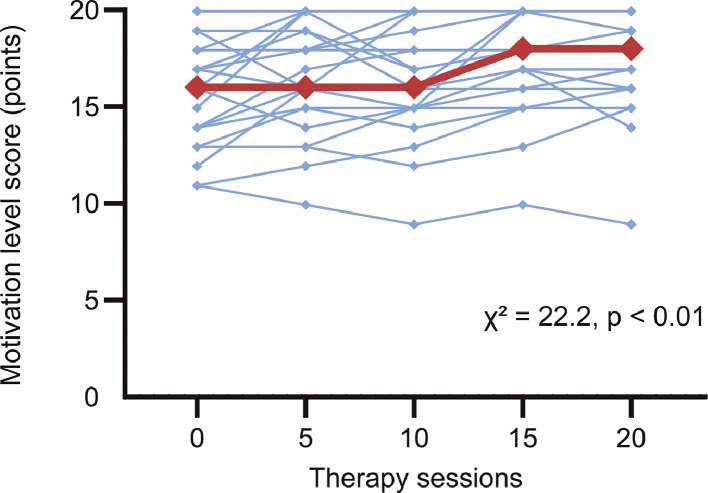
No participant dropped out or experienced an adverse event during the intervention period. The results of the survey regarding the acceptability of the intervention are shown in table 3. Twenty-one (84%) participants responded with “agree” or “strongly agree” to the statement regarding their satisfaction with the intervention, whereas 19 (76%) answered “agree” or “strongly agree” to the item regarding their intention to continue receiving it. The survey on the motivation for rehabilitation was administered to all participants weekly. The median motivation level score significantly increased during the intervention (fig 2).
Table 3.
Participants’ responses to a survey on the acceptability of the intervention.
| Responses | Strongly Agree | Agree | Uncertain | Disagree |
|---|---|---|---|---|
| Satisfaction with the intervention | 7 (28) | 14 (56) | 2 (8) | 2 (8) |
| Intention to continue receiving the intervention | 12 (48) | 7 (28) | 5 (20) | 1 (4) |
NOTE. Values are presented as numbers (%).
Fig 2.
Changes in the motivation level score during the intervention. The red line represents the median data; blue lines, the individual participant data.
Potential physical and mental health effects of the intervention
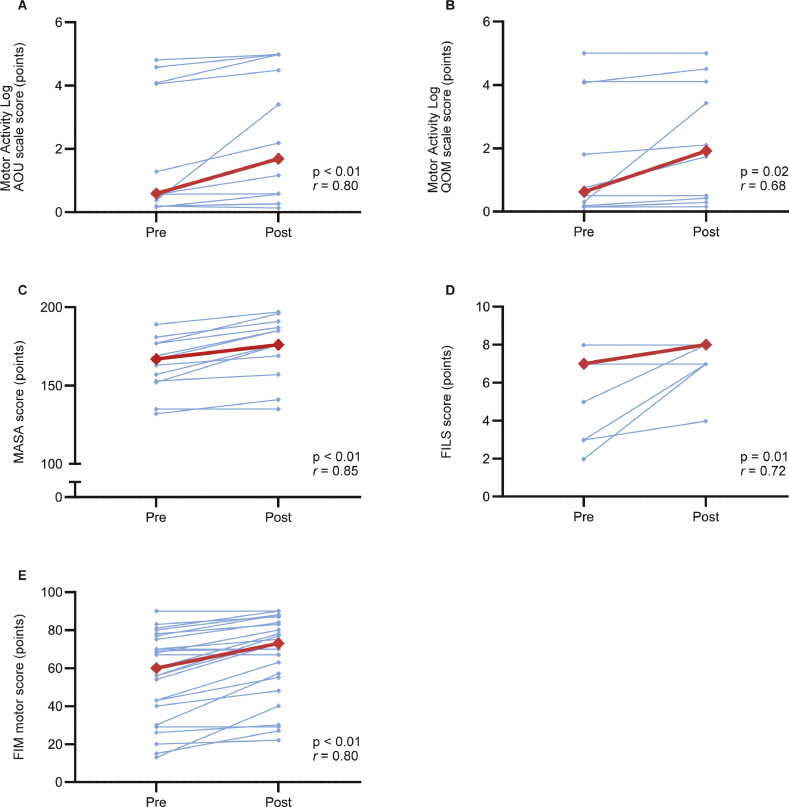
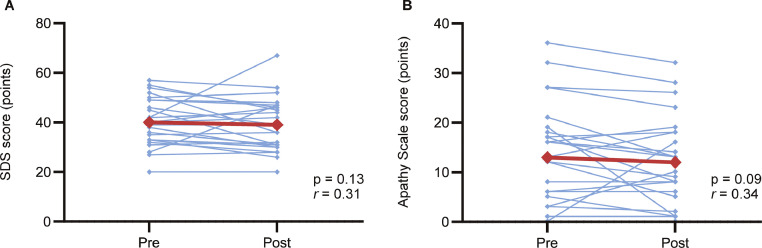
Changes in physical and mental health outcomes during the intervention are shown in figures 3 and 4, respectively. The numerical data underlying figures 3 and 4 are provided in supplemental table S2 (available online only at http://www.archives-pmr.org/). Furthermore, the individual data on these outcomes before and after the intervention are available in supplemental table S3 (available online only at http://www.archives-pmr.org/). In the OT group, statistically significant improvements were observed in the scores of the Motor Activity Log amount of use (Cohen's r=0.80; fig 3A) and quality of movement scales (Cohen's r=0.68; fig 3B) and FIM motor items (Cohen's r=0.77), but not in the SDS (Cohen's r=0.02) and Apathy Scale (Cohen's r=0.18) scores. In the ST group, the scores of the Mann Assessment of Swallowing Ability (Cohen's r=0.85; fig 3C), FILS (Cohen's r=0.72; fig 3D), FIM motor items (Cohen's r=0.85), and SDS (Cohen's r=0.62) significantly improved, whereas the changes in the Apathy Scale scores were statistically insignificant despite a large effect size (Cohen's r=0.52). Among all participants, the FIM motor score was statistically significantly improved during the intervention (Cohen's r=0.80; fig 3E), whereas the changes in the SDS (Cohen's r=0.31; fig 4A) and Apathy Scale (Cohen's r=0.34; fig 4B) scores were statistically insignificant despite a medium effect size.
Fig 3.
Changes in physical outcomes before and after the intervention. (A) The Motor Activity Log amount of use (AOU) scale score. (B) The Motor Activity Log quality of movement (QOM) scale score. (C) The Mann Assessment of Swallowing Ability (MASA) score. (D) The FILS score. (E) The FIM motor score. Red lines represent the median data; blue lines, the individual participant data. Abbreviation: r, Cohen's r for the Wilcoxon signed-rank test.
Fig 4.
Changes in mental health outcomes before and after the intervention. (A) The SDS score. (B) The Apathy Scale score. Red lines represent the median data; blue lines, the individual participant data. Abbreviation: r, Cohen's r for the Wilcoxon signed-rank test.
For mental health outcomes, before the intervention, 5 of the overall participants had scores of ≥50 points on the SDS, and 12 had scores of ≥14 points on the Apathy Scale. In the 5 participants with depressive symptoms, the median (interquartile range) SDS scores decreased from before (54 [52-55] points) to after the intervention (46 [45-52] points), with a large (but statistically insignificant) effect size (p=.13; Cohen's r=0.78). Additionally, in the 12 participants with apathy, the Apathy Scale scores statistically significantly decreased from before (19 [17-27] points) to after the intervention (16 [13-24] points), with a large effect size (p<.01; Cohen's r=0.75).
Discussion
The ARCS model is used to design the motivational aspects of learning environments to enhance and sustain students’ motivation to learn.22,23 To our knowledge, this is the first study to examine the feasibility and potential physical and mental health effects of the intervention using the ARCS model with OT and ST. Our results suggest that the intervention was feasible. We also found statistically significant improvements with a large effect size in the motor function of the paretic upper extremity and ADLs for the OT group and the swallowing ability, ADLs, and depressive symptoms for the ST group. These findings may provide therapists with helpful insight into effectively motivating patients to engage in stroke rehabilitation and offer researchers valuable information for designing future randomized controlled trials.48
A representative motivational intervention that has been used in rehabilitation is motivational interviewing, which is a collaborative communication style that helps patients resolve their ambivalence and strengthen intrinsic motivation for behavioral changes.13,14,20,49 However, previous studies with motivational interviewing after stroke reported that approximately 30% of participants discontinued the intervention.50,51 Conversely, no dropouts or adverse events were recorded during the intervention period in this study. Additionally, >75% of overall participants showed satisfaction with and intention to continue receiving the intervention, indicating good acceptability. Therefore, the motivational approach based on the ARCS model may be more feasible than motivational interviewing. The ARCS model would also present 2 advantages over motivational interviewing in rehabilitation. First, the motivational intervention based on the ARCS model is specifically designed to address motivational concerns in the rehabilitation environment through modifications in therapist behaviors (eg, explaining the necessity of practice) and the content of rehabilitation programs (eg, providing rehabilitation programs with variations). This allows therapists to effectively manipulate potential factors that influence patient motivation. Second, the ARCS model is highly accessible and can be readily adopted by therapists, including those with limited clinical experience. The therapists in this study received only 60-minute training sessions for 2 days. In contrast, successful implementation of motivational interviewing prompts relatively more intensive training in verbal and nonverbal communication skills.49 For example, a previous study reported that therapists underwent an extensive training program for 4 days, comprising up to 10 practice sessions until they were deemed competent and confident in the technique.50 Therefore, the ARCS model can be effectively used with relatively minimal training requirements.
The results suggest that the intervention is potentially effective in improving physical outcomes. However, we found no statistically significant improvements in depressive symptoms in the OT group and apathy in both groups. Before the intervention, only 5 participants had depressive symptoms, and 12 had apathy; therefore, the failure to detect statistically significant changes in mental health outcomes during the intervention could be attributed to ceiling effects.
Study limitations
First, we could not determine whether the improvements in physical outcomes observed in this study were attributed to using the ARCS model because of the lack of a control group. However, the positive results observed in this study support the need for a randomized controlled trial to investigate the effectiveness of using the ARCS model in rehabilitation. Second, the same therapist performed the assessment and intervention for each participant; therefore, there may be possible observer bias. The assessor should be blinded to the group allocation in future randomized controlled trials. Finally, all participants were recruited from convalescent rehabilitation wards. Patients who participated in this study may adhere more to their rehabilitation programs than acute stroke survivors and community-dwellers with long-term strokes.52 Furthermore, the maximal length of stay in the convalescent rehabilitation wards covered by the insurance is 180 days for patients with stroke and accompanying severe disabilities,30 which can be longer than the length of stay for inpatient rehabilitation after stroke in the United States (approximately 15 days).53 Therefore, further studies in acute and chronic rehabilitation settings and international research would improve the external validity of our findings.
Conclusions
This study demonstrated that applying the motivational instructional design model to OT and ST after stroke was feasible with the potential to improve the motor function of the paretic upper extremity, swallowing ability, and ADLs. These findings may provide valuable information to design a future randomized controlled trial.
Supplier
-
a.
Statistical Package for the Social Sciences software, version 27.0; IBM Corporation.
Acknowledgments
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this article.
Acknowledgments
The authors thank Ayana Hosobuchi, OT, BSc, Takahiro Nishiyama, OT, BSc, Haruna Kawahara, OT, BSc, Ayumi Nakamura, OT, BSc, Kosaku Katsumata, OT, MSc, Yuta Asada, OT, MSc, Shogo Nozaki, OT, BSc, and Miho Nanbu, OT, BSc at the Tokyo Bay Rehabilitation Hospital; Sakura Terasaka, ST, BSc, Kaede Yoshino, ST, BSc, Hiroki Ikeda, ST, BSc, Miyu Nakamura, ST, BSc, and Hiroka Takatsuji, ST, BSc at the Hamamatsu City Rehabilitation Hospital; and Kenjiro Kunieda, MD, PhD at the Gifu University for their help and support.
Data availability
The datasets used and/or analyzed during this study cannot be made publicly available owing to the need for participant confidentiality. However, they are available from the corresponding author upon reasonable request. The individual data on physical and mental health outcomes before and after the intervention are provided in supplemental table S3 (available online only at http://www.archives-pmr.org/).
Footnotes
Supported by a grant from JSPS KAKENHI (grant number JP20K21752). The funding source had no involvement in the study design; collection, analysis, and interpretation of data; writing of the report; and the decision to submit the article for publication.
Clinical Trial Registration No.: UMIN000037324 and UMIN000037506.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2024.100344.
Appendix. Supplementary materials
References
- 1.Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? J Stroke Cerebrovasc Dis. 2004;13:171–177. doi: 10.1016/j.jstrokecerebrovasdis.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:e98–169. doi: 10.1161/STR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 3.Pollock A, Farmer SE, Brady MC, et al. Interventions for improving upper limb function after stroke. Cochrane Database Syst Rev. 2014;2014 doi: 10.1002/14651858.CD010820.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10 doi: 10.1002/14651858.CD000323.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization, International classification of functioning, disability and health: ICF, 2001, World Health Organization. Available at: https://iris.who.int/handle/10665/42407. Accessed March 3, 2023.
- 6.Duncan PW, Horner RD, Reker DM, et al. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke. 2002;33:167–177. doi: 10.1161/hs0102.101014. [DOI] [PubMed] [Google Scholar]
- 7.Gunnes M, Indredavik B, Langhammer B, et al. Associations between adherence to the physical activity and exercise program applied in the LAST study and functional recovery after stroke. Arch Phys Med Rehabil. 2019;100:2251–2259. doi: 10.1016/j.apmr.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 8.Rapolienė J, Endzelytė E, Jasevičienė I, Savickas R. Stroke patients motivation influence on the effectiveness of occupational therapy. Rehabil Res Pract. 2018;2018 doi: 10.1155/2018/9367942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luker J, Lynch E, Bernhardsson S, Bennett L, Bernhardt J. Stroke survivors’ experiences of physical rehabilitation: a systematic review of qualitative studies. Arch Phys Med Rehabil. 2015;96 doi: 10.1016/j.apmr.2015.03.017. 1698-708.e10. [DOI] [PubMed] [Google Scholar]
- 10.Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2532–2553. doi: 10.1161/STR.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 11.Nicholson S, Sniehotta FF, van Wijck F, et al. A systematic review of perceived barriers and motivators to physical activity after stroke. Int J Stroke. 2013;8:357–364. doi: 10.1111/j.1747-4949.2012.00880.x. [DOI] [PubMed] [Google Scholar]
- 12.Maclean N, Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc Sci Med. 2000;50:495–506. doi: 10.1016/s0277-9536(99)00334-2. [DOI] [PubMed] [Google Scholar]
- 13.McGrane N, Galvin R, Cusack T, Stokes E. Addition of motivational interventions to exercise and traditional physiotherapy: a review and meta-analysis. Physiotherapy. 2015;101:1–12. doi: 10.1016/j.physio.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 14.McGrane N, Cusack T, O'Donoghue G, Stokes E. Motivational strategies for physiotherapists. Phys Ther Rev. 2014;19:136–142. [Google Scholar]
- 15.Maclean N, Pound P, Wolfe C, Rudd A. The concept of patient motivation: a qualitative analysis of stroke professionals’ attitudes. Stroke. 2002;33:444–448. doi: 10.1161/hs0202.102367. [DOI] [PubMed] [Google Scholar]
- 16.Oyake K, Sue K, Sumiya M, Tanaka S. Physical therapists use different motivational strategies for stroke rehabilitation tailored to an individual's condition: a qualitative study. Phys Ther. 2023;103:pzad034. doi: 10.1093/ptj/pzad034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oyake K, Suzuki M, Otaka Y, Momose K, Tanaka S. Motivational strategies for stroke rehabilitation: a Delphi study. Arch Phys Med Rehabil. 2020;101:1929–1936. doi: 10.1016/j.apmr.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Oyake K, Suzuki M, Otaka Y, Tanaka S. Motivational strategies for stroke rehabilitation: a descriptive cross-sectional study. Front Neurol. 2020;11:553. doi: 10.3389/fneur.2020.00553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oyake K, Yamauchi K, Inoue S, et al. A multicenter explanatory survey of patients’ and clinicians’ perceptions of motivational factors in rehabilitation. Commun Med (Lond) 2023;3:78. doi: 10.1038/s43856-023-00308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng D, Qu Z, Huang J, Xiao Y, Luo H, Wang J. Motivational interviewing for improving recovery after stroke. Cochrane Database Syst Rev. 2015;2015 doi: 10.1002/14651858.CD011398.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sugavanam T, Mead G, Bulley C, Donaghy M, van Wijck F. The effects and experiences of goal setting in stroke rehabilitation - a systematic review. Disabil Rehabil. 2013;35:177–190. doi: 10.3109/09638288.2012.690501. [DOI] [PubMed] [Google Scholar]
- 22.Keller JM. Development and use of the ARCS model of instructional design. J Instr Dev. 1987;10:2–10. [Google Scholar]
- 23.Keller JM. Springer; New York: 2010. Motivational design for learning and performance. [Google Scholar]
- 24.Schepens SL, Panzer V, Goldberg A. Randomized controlled trial comparing tailoring methods of multimedia-based fall prevention education for community-dwelling older adults. Am J Occup Ther. 2011;65:702–709. doi: 10.5014/ajot.2011.001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai X, Li Z, Zhang J, et al. Effects of ARCS model-based motivational teaching strategies in community nursing: a mixed-methods intervention study. Nurse Educ Today. 2022;119 doi: 10.1016/j.nedt.2022.105583. [DOI] [PubMed] [Google Scholar]
- 26.Jeon EY. What makes them the best English teachers? An analysis of the motivational strategy use based on ARCS model. Educ Res Policy Pract. 2021;20:263–278. [Google Scholar]
- 27.Luo X, Liu L, Li J. The effects of ARCS motivational instruction in physical education on learning cognition and the health-related physical fitness of students. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.786178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shellnut B, Knowltion A, Savage T. Applying the ARCS model to the design and development of computer-based modules for manufacturing engineering courses. Educ Technol Res Dev. 1999;47:100–110. [Google Scholar]
- 29.Wongwiwatthananukit S, Popovich NG. Applying the ARCS model of motivational design to pharmaceutical education. Am J Pharm Educ. 2000;64:188–196. [Google Scholar]
- 30.Miyai I, Sonoda S, Nagai S, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011;25:540–547. doi: 10.1177/1545968311402696. [DOI] [PubMed] [Google Scholar]
- 31.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 32.Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med. 1975;7:13–31. [PubMed] [Google Scholar]
- 33.Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manage. 2013;46:201–206. doi: 10.1016/j.jpainsymman.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 34.Visser J, Keller JM. The clinical use of motivational messages: an inquiry into the validity of the ARCS model of motivational design. Instr Sci. 1990;19:467–500. [Google Scholar]
- 35.Oyake K, Kondo K, Tanaka S. In: Proceedings of the 34th Annual Conference of Japan Society for Educational Technology. Horita T., editor. Miyagi; (Japan): 2018. Categorization of motivational strategies in rehabilitation based on ARCS model; pp. 667–668. [Google Scholar]
- 36.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.El-Kotob R, Giangregorio LM. Pilot and feasibility studies in exercise, physical activity, or rehabilitation research [editorial] Pilot Feasibility Stud. 2018;4:137. doi: 10.1186/s40814-018-0326-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blasi PR, Scrol A, Anderson ML, et al. Feasibility, acceptability, and limited efficacy of health system-led familial risk notification: protocol for a mixed-methods evaluation. Pilot Feasibility Stud. 2022;8:174. doi: 10.1186/s40814-022-01142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taub E, Miller NE, Novack TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993;74:347–354. [PubMed] [Google Scholar]
- 40.Mann G. Vol. 1. Cengage Learning; New York: 2002. (MASA: the Mann assessment of swallowing ability). [Google Scholar]
- 41.Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993;72:84–89. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 43.Starkstein SE, Fedoroff JP, Price TR, Leiguarda R, Robinson RG. Apathy following cerebrovascular lesions. Stroke. 1993;24:1625–1630. doi: 10.1161/01.str.24.11.1625. [DOI] [PubMed] [Google Scholar]
- 44.Dunstan DA, Scott N. Clarification of the cut-off score for Zung's self-rating depression scale. BMC Psychiatry. 2019;19:177. doi: 10.1186/s12888-019-2161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol. 2013;13:104. doi: 10.1186/1471-2288-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4:287–291. [Google Scholar]
- 47.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141:2–18. doi: 10.1037/a0024338. [DOI] [PubMed] [Google Scholar]
- 48.Collinson M, Anwar S, Graham L, et al. Designing and analysing feasibility studies of complex interventions: challenges related to assessing stop/go criteria. Trials. 2013;14:O20. [Google Scholar]
- 49.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 50.Watkins CL, Auton MF, Deans CF, et al. Motivational interviewing early after acute stroke: a randomized, controlled trial. Stroke. 2007;38:1004–1009. doi: 10.1161/01.STR.0000258114.28006.d7. [DOI] [PubMed] [Google Scholar]
- 51.Patel K, Watkins CL, Sutton CJ, et al. Motivational interviewing for low mood and adjustment early after stroke: a feasibility randomised trial. Pilot Feasibility Stud. 2018;4:152. doi: 10.1186/s40814-018-0343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yao M, Chen J, Jing J, Sheng H, Tan X, Jin J. Defining the rehabilitation adherence curve and adherence phases of stroke patients: an observational study. Patient Prefer Adherence. 2017;11:1435–1441. doi: 10.2147/PPA.S139854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cao Y, Nie J, Sisto SA, Niewczyk P, Noyes K. Assessment of differences in inpatient rehabilitation services for length of stay and health outcomes between US Medicare advantage and traditional Medicare beneficiaries. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during this study cannot be made publicly available owing to the need for participant confidentiality. However, they are available from the corresponding author upon reasonable request. The individual data on physical and mental health outcomes before and after the intervention are provided in supplemental table S3 (available online only at http://www.archives-pmr.org/).