Supplemental Digital Content is Available in the Text.
Abstract
Background:
The World Health Organization is committed to strengthening access to pre-exposure prophylaxis (PrEP) for HIV prevention and its integration into primary care services. Unfortunately, the COVID-19 pandemic has disrupted the delivery of primary care, including HIV-related services. To determine the extent of this disruption, we conducted a systematic review and meta-analysis of the changes in access to PrEP services during the pandemic and the reasons for these changes.
Methods:
A search was conducted using PubMed, Scopus, Embase, PsycINFO, and Cinahl for studies published between January 2020 and January 2023. Selected articles described self-reported disruptions to PrEP service access associated with the COVID-19 pandemic or its responses. Pooled effect sizes were computed using a random-effects model.
Results:
Thirteen studies involving 12,652 PrEP users were included in our analysis. The proportion of participants reporting a disruption in access to PrEP services during the COVID-19 pandemic ranged from 3% to 56%, with a pooled proportion of 21% (95% confidence intervals: 8% to 38%). Social restrictions, financial constraints, and limited health insurance coverage were key factors affecting access to PrEP services during the pandemic.
Conclusions:
To our knowledge, this is the first meta-analysis to quantify the extent of disruptions to accessing PrEP services because of the COVID-19 pandemic. To increase the ability of primary care services to maintain PrEP services during public health crises, a mixture of strategies is worth considering. These include multi-month PrEP prescriptions, telehealth services, deployment of peer support groups to provide a community-based service or home delivery, and provision of financial support interventions.
INTRODUCTION
Pre-exposure prophylaxis (PrEP) use prevents HIV acquisition.1–4 Because of this benefit, the World Health Organization (WHO) includes PrEP in a recommended package of prevention services, targeting key population groups.5–8 This recommendation was also echoed by the Joint United Nations Programme on HIV/AIDS with its commitment to ensure access to PrEP for 3 million people at high risk of HIV infection by 2020.9 Furthermore, in 2022, the WHO reaffirmed its dedication to enhancing PrEP access and its integration into primary care services.10
The WHO declared the COVID-19 pandemic a public health emergency of international concern in January 2020.11 By 31 March 2024, more than 775 million confirmed COVID-19 cases and 7 million COVID-19-related deaths were reported to the WHO.12 The pandemic's impact on health care services, including primary care, has been profound, and collateral effects have also been observed. Although efforts have been made to continue HIV care delivery throughout the COVID-19 pandemic, disruptions to regular HIV services have been seen in many parts of the world,13–16 including access to condoms,17 HIV testing,17,18 HIV treatment,15,16 and PrEP.17,19–21
Throughout history, health care systems have faced similar disruptions during emergencies and crises. Examples include disruptions during wars or armed conflicts,22–24 natural disasters such as flooding and earthquakes,25–27 and previous disease outbreaks such as Ebola.28 These experiences have underscored the vulnerability of underprepared health care systems during crises, offering invaluable lessons. In 2021, in response to the COVID-19 pandemic, the WHO heightened its commitment to building health systems that are resilient against future public health threats.29
Although PrEP substantially reduces HIV transmission, its effectiveness heavily relies on the user's ability to access it in times of need. The experiences of both service providers and users throughout the COVID-19 pandemic can provide insights into the extent of the disruptions and the strategies necessary to develop resilient primary health care services that can ensure the continuous delivery of PrEP even in times of crisis. To the best of our knowledge, no meta-analysis has assessed the extent to which the COVID-19 pandemic impacted users' access to PrEP services.
To address this evidence gap and inform the design of policies and interventions to protect and strengthen PrEP services in the face of future public health threats, this systematic review was undertaken. The objectives of this review and meta-analysis were to identify the extent of disruptions to PrEP service access during the pandemic from a user perspective as well as the reasons for disrupted access and for the discontinuation of PrEP intake.
METHODS
Study Design
A systematic review and meta-analysis were undertaken, based on a comprehensive search of 5 databases: PubMed; Scopus; Embase; PsycINFO; and Cinahl. The search terms used were a combination of keywords and Medical Subject Heading terms on HIV, PrEP, and COVID-19 (see Supplemental Digital Content 1, http://links.lww.com/QAI/C327).
Study Selection
Studies were included if they were empirical research, based on a quantitative study design, and published between January 2020 and January 2023. Studies also needed to report on the impact of the pandemic by measuring self-reported disruptions to PrEP service access, referred to as self-reported difficulties or discontinuation of an appointment to receive a new or refill prescription, to obtain PrEP medicines, or more difficult access to PrEP services in general. No limitations were applied regarding language or country, whereas research letters, reviews, meta-analyses, and studies for which the full text was unavailable were excluded.
The protocol for this review was registered at PROSPERO CRD42022299312.
Records were managed in EndNote X9. All articles obtained from the databases were imported to Endnote X9 and Excel spreadsheet, with duplicates removed by L.P.L.W. L.P.L.W., D.B., S.N.S.N., Y.A.M., S.D.W., and I.W.C.S.D.P. then conducted title and abstract screening.
Data Extraction
Five authors (D.B., S.N.S.N., Y.A.M., S.D.W., and I.W.C.S.D.P.) then independently conducted full-text screening and data extraction using a standardized abstraction form, each handling approximately 7 different articles. Training sessions were provided by L.P.L.W. to ensure familiarity with the form and its usage. The data extracted included study details (authors, publication year), study characteristics (country, study design, study participants, recruitment sites, data collection period), and quantitative data reporting disruptions to PrEP service access. To prevent inconsistencies, L.P.L.W. reviewed all articles included in the data extraction process. Discrepancies were resolved by discussion between L.P.L.W. and D.B.
All data were imported and analyzed using Stata version 14 (StataCorp. 2019. College Station, TX).
Data Analysis
The pooled prevalence of PrEP users experiencing disruptions to PrEP service access was presented as the percentage of PrEP users self-reporting disruptions to PrEP service access among the total number of PrEP users in the study. The meta-analysis was conducted according to the DerSimonian and Laird method,30 with the pooled prevalence computed using a random-effects model to account for heterogeneity in the effect estimate.30–32 Statistical tests for heterogeneity do not perform well with pooled proportions and were therefore not conducted.33 However, the sources of heterogeneity were explored through visual inspection of forest plots and the investigation of outliers.33 Heterogeneity was also explored using subgroup analyses.
PRISMA guidelines were used to guide the review process and the development of the manuscript.34
Quality Assessment
The Joanna Briggs Institute Critical Appraisal Tool for Systematic Reviews was used to appraise the quality of the research evidence.35 D.B., S.N.S.N., Y.A.M., S.D.W., and I.W.C.S.D.P. independently assessed the quality of the included studies. Any discrepancies were addressed through discussions with L.P.L.W. Each study underwent evaluation against the criteria outlined in the tool, resulting in categorization into quality tiers. Studies meeting over 80% of the tool's criteria were deemed high quality, whereas those meeting 50%–80% were considered moderate, and those meeting less than 50% were categorized as low quality. Studies meeting 50% or more of the criteria were eligible for inclusion. This process mirrors the methodology used in previous meta-analyses.36
RESULTS
Study Characteristics
Our search found 793 articles. Among these, 373 duplicates were removed, and 386 were excluded after title and abstract screening. Of the 34 full reports reviewed, 19 were excluded because there was no full text, and 2 were research letters. These exclusions resulted in 13 studies eligible for analysis (Fig. 1). These 13 studies were conducted in 19 countries. Specifically, 12 studies were conducted within a single country—comprising 1 middle-income37 and 11 high-income countries, as classified by the World Bank's income classification.38 In addition, 1 study was conducted across 20 countries, encompassing 11 middle-income and 9 high-income countries17 (Table 1).
FIGURE 1.
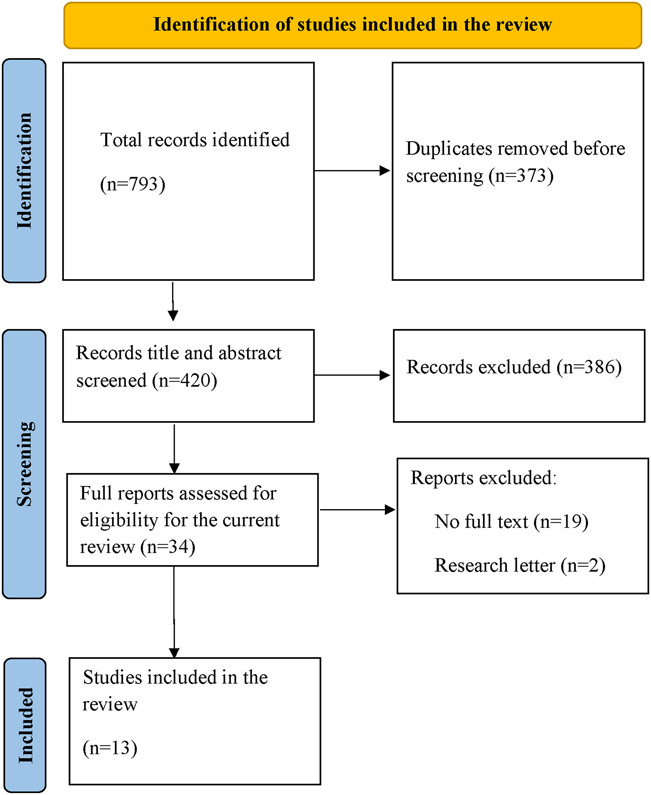
Study selection.
TABLE 1.
Characteristics of Studies Included in the Analysis
| Authors | Publication Year | Country | World Bank's Country Income Classification for the 2024 Fiscal Year | Study Design | Data Collection Methods | Data Collection Period | Data Collection Period in Relation to Government-Imposed Restriction Periods | Study Population(s) | Sampling Strategy | Recruitment Sites |
| Camp et al39 | 2021 | The United States | High-income country | Cross-sectional | Email survey | December 2019 and June 2020 | During restriction | MSM | Nonprobability | Clinic/s and social media or web-based |
| Chen et al20 | 2021 | The United States | High-income country | Cross-sectional | A Zoom platform interview | April–July 2020 | During restriction | MSM and transgender women | Probability | Community |
| Ciaccio et al40 | 2022 | France | High-income country | Cross-sectional | Online survey | June–July 2020 | During restriction | MSM | Nonprobability | Social media or web-based |
| Hammoud et al41 | 2021 | Australia | High-income country | Cross-sectional | Online survey | April 2020 | During restriction | Gay and bisexual men | Nonprobability | Social media or web-based |
| Hong et al18 | 2021 | The United States | High-income country | Cross-sectional | Online survey | April–September 2020 | Unreported | Young sexual minority men (YSMM) | Nonprobability | Social media or web-based |
| MacCarthy et al21 | 2020 | The United States | High-income country | Mixed-methods study | Telephone-based or app-based interview | April–May 2020 | Unreported | Latin sexual minority men (LSMM) and transgender women (LTGW) | Probability | Non-govermental organisations |
| Mistler et al42 | 2021 | The United States | High-income country | Cross-sectional | Telephone-based or app-based interview | May–October 2020 | Unreported | PWIDs with opioid use disorder | Nonprobability | Clinic/s |
| Morgan et al43 | 2022 | The United States | High-income country | Cohort | Online survey | March–August 2020 | Unreported | Black and/or Hispanic/Latino sexual minority men and gender diverse (SMMGD) | Nonprobability | Social media or web-based |
| Pampati et al44 | 2021 | The United States | High-income country | Cross-sectional | Online survey | October 2019–July 2020 | Unreported | MSM | Unreported | Social media or web-based |
| Rao et al17 | 2021 | Australia, Belarus, Belgium, Brazil, Canada, Egypt, France, German, Indonesia, Italy, Kazakhstan, Malaysia, Mexico, the Russian Federation, Taiwan, Thailand, Turkey, Ukraine, the United Kingdom, and the United States | Nine high-income countries and 11 middle-income countries | Cross-sectional | Online survey | April–May 2020 | During restriction | Users of gay social networking app Hornet | Nonprobability | Social media or web-based |
| Reyniers et al45 | 2021 | Belgium | High-income country | Cross-sectional | Online survey | April 2020 | During restriction | MSM | Nonprobability | Social media or web-based |
| Stephenson et al46 | 2021 | The United States | High-income country | Cross-sectional | Online survey | April–May 2020 | During restriction | Gay, bisexual, and other MSM (GBMSM) | Nonprobability | Social media or web-based |
| Torres et al37 | 2021 | Brazil | Middle-income country | Cross-sectional | Online survey | April–May 2020 | During restriction | MSM and transgender/non-binary (TGNB) | Nonprobability | Social media or web-based |
In total, 12,652 PrEP users were included in the studies. All studies were conducted as part of larger cross-sectional, cohort, or mixed-methods studies. Most studies (n = 11) used a cross-sectional study design,17,18,20,37,39–42,44–46 with only 1 using a cohort design43 and 1 a mixed-methods design.21 Most (n = 8) used an email or online survey, 2 used phone interviews,21,42 and 1 used a Zoom platform.20 Twelve studies recruited men who have sex with men (MSM) or lesbian, gay, bisexual, transgender and queer participants, with 6 studies specifically recruiting only MSM participants. One study was among people who inject drugs (PWIDs).42 Nine studies recruited participants from online networks or mobile apps and 4 studies recruited participants from clinics, nongovernmental organizations, or community settings. All studies collected their data around 2020, with 2 starting their data collection process in 2019.39,44 The period of data collection ranged from 1 to 9 months. Most studies (n = 10) were published in 2021, 1 in 2020, and 2 in 2022 (Table 1).
Disruption in Access to PrEP Services During the COVID-19 Pandemic
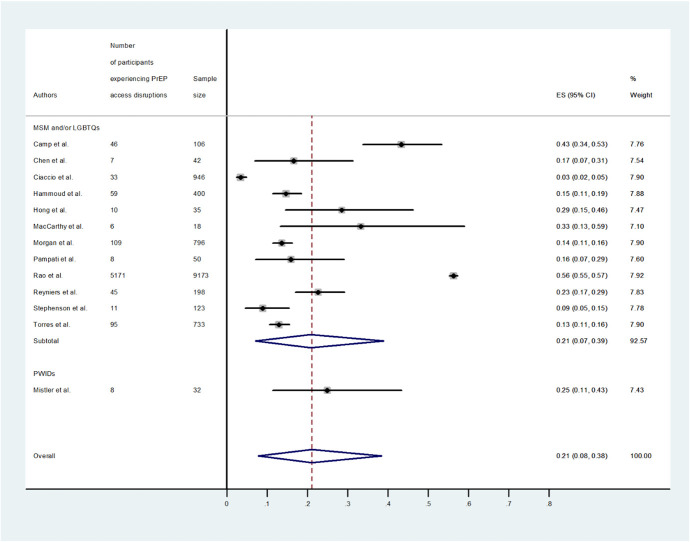
Among the 13 studies included in the meta-analysis, the proportion of participants self-reporting disruptions to PrEP service access ranged from 3% to 56%, indicating substantial heterogeneity, with an overall pooled proportion of PrEP users experiencing disruptions to PrEP service access of 21% [95% confidence intervals (CI): 8% to 38%] (Fig. 2).
FIGURE 2.
Forest plot of the proportion of PrEP users experiencing disruptions in access to PrEP services during the COVID-19 pandemic.
Stratified by population groups, a study conducted among PWIDs (n = 1) found that 25% (95% CI: 11% to 43%) of PrEP users experienced disruptions to PrEP service access. The pooled proportion of disruptions among those self-identified as MSM or lesbian, gay, bisexual, transgender and queer (n = 12) was lower, that is, 21% (95% CI: 7% to 39%) (Fig. 2). Two studies explored the reasons for such disruptions.20,21 Among the factors impacting the changes in access to PrEP services included social restrictions,21 financial constraints,20 and health insurance issues.21
PrEP Discontinuation and HIV Testing
In addition to disruptions to PrEP service access, some studies also reported user experiences of PrEP discontinuation, that is, interruptions in the use of PrEP (n = 5)18,21,37,40,41 and HIV testing disruptions (n = 8).17,18,21,41,42,44–46 Among the self-reported reasons for discontinuing PrEP use were reduced sexual activity or fewer sexual partners.18,21,37,40,41 One study explored the association between PrEP discontinuation and HIV testing and found that those who had discontinued PrEP had lower HIV testing rates compared with those who used PrEP during the COVID-19 pandemic.41
Risk of Bias and Quality of the Studies Included in the Analysis
The quality of the studies included in the analysis is depicted in Supplemental Digital Content 2, http://links.lww.com/QAI/C327. The appropriateness of the sampling frame and the adequacy of the sample size were unclear in most studies, although this issue is common when recruiting hidden or stigmatized populations.47 All studies described settings and subjects in detail.
DISCUSSION
Strengthening primary health care resilience to ensure access to PrEP and other HIV services is a priority for many countries. To our knowledge, this is the first meta-analysis to quantify the extent of disruptions to accessing PrEP services because of the COVID-19 pandemic, drawing attention to both high-income and low- and middle-income countries (LMICs), and inclusion of different key populations. We estimate the pooled proportion of PrEP users experiencing disruptions in access to be 21% (95% CI: 8% to 38%). This result is similar to the predicted reduction in PrEP prescriptions during the pandemic in the United States, modelled using a national pharmacy database, that is, 22% (95% CI: 19% to 25%).48 Disruptions to PrEP access increase vulnerability to HIV infection.43 Although some studies have reported a decrease in PrEP use because of a reduction in demand (ie, a decline in sexual contacts),18,40 some groups remained engaged in behaviors that could lead to HIV risk during the pandemic,18 including condomless sex40,49 and having multiple sexual partners.50,51
One of the key factors cited for disruptions to PrEP service access during the pandemic was financial barriers, including travel-related costs.20 Studies show that even before the COVID-19 pandemic, the cost of PrEP-associated consultations, medication, and laboratory tests was already a key barrier to accessing PrEP services, especially among socioeconomically disadvantaged or underinsured groups.20,52–56 In LMICs, it is common for patients to make substantial out-of-pocket payments toward their health care.57 These costs were exacerbated during the pandemic when many health services closed or reduced their patient intake, forcing patients to travel further to access PrEP.20 Given that many key populations, such as MSM or sex workers, lacked social support58 and experienced loss of income during the COVID-19 outbreak,58,59 financial support interventions, including cost-sharing, are expected to help maintain PrEP access during future public health crises.60 Further research is needed to investigate the effectiveness, cost-effectiveness and affordability of such interventions especially during public health crises.
PrEP clinical practice guidelines recommend that PrEP users undertake routine HIV testing.61 One study in Australia included in this review noted a strong correlation between the discontinuation of PrEP during COVID-19 restrictions and the lower likelihood of recently being tested for HIV.41 Similar findings were reported in the United States.46 A decrease in testing rates could be associated with a reduction in at-risk behaviors, which might consequently have a slight impact on the transmission of sexually transmitted infections. However, mathematical modeling has indicated that, despite a decrease in the number of sexual partners, the decline in HIV testing rates during the COVID-19 pandemic is linked to an increase in sexually transmitted infection transmission rates. This is especially notable for chlamydia trachomatis.62 Therefore, the disruption to PrEP service access, and thus access to HIV testing, underscores the need to consider alternative strategies to ensure the provision of testing services during public health crises.
In several countries, efforts were made to ensure sustainable access to PrEP during the COVID-19 pandemic. Initiatives included the provision of a multi-month PrEP supply,63–65 maintaining or extending clinic operating hours even during periods of social restriction,66 telehealth consultations,64–67 use of social media platforms to maintain demand and provide education about PrEP,64 additional community support for PrEP care (eg, peer support, lay health care providers,3 outreach workers64,68) and PrEP home delivery.69 Although the success of such telehealth interventions depends, for example, on good infrastructure and access to technology to enable telehealth,70 these interventions are shown to be feasible and effective across a range of settings and target groups.64
Our studies conducted in Indonesia highlighted several challenges encountered in mitigating the impact of the COVID-19 pandemic on health care systems while striving to sustain the delivery of HIV and tuberculosis (TB) services.71,72 These challenges encompassed interruptions in the supply of HIV and TB medicines, increased workload among health care workers tasked with managing both HIV and COVID-19-related strategies, and heightened risk of COVID-19 exposure among community health workers and peer groups of people living with HIV.71,72 It is imperative to consider these challenges when ensuring continued access to PrEP during public health crises.
A previous study showed that PrEP users strongly favored home delivery of PrEP and the use of HIV self-tests, supported by telemedicine services.73 Scaling up this delivery method is worth considering to ensure continued access and use of PrEP along with HIV testing during future crises.
Because of the enormous pressures on health systems during a pandemic and other public health emergencies, integration of PrEP into wider health services might also be worth considering to improve efficiency and ensure the continuation of PrEP. For example, as noted in some settings, a syringe services program could also be used to provide PrEP for PWIDs.74,75 Community-based antiretroviral delivery, involving outreach workers partnering with community-based organizations, was shown to have a positive impact on antiretroviral retention76 and might also be evaluated for use in other settings.
There are a few limitations to be considered when interpreting the results of this review. First, the current review included studies from only 19 countries, most of which were classified as high-income. Thus, the data presented are unlikely to be representative of LMICs more generally. Future studies would benefit from delving deeper into this issue within LMIC contexts. Second, study designs and methodologies used in each study varied widely. This could introduce variability, that is, clinical or methodological heterogeneities, which might then result in statistical heterogeneity.32 While conducting a statistical test to determine whether these variations are greater than what is expected by chance alone is important,32 the statistical tests for heterogeneity do not perform well with pooled proportions and were therefore not conducted.33 As a result, we were only able to explore heterogeneity using subgroup analyses and visual inspection. Thus, caution should be taken when interpreting the pooled estimate. Third, many studies lacked detailed information on timelines, making it difficult to determine whether data on disruptions to accessing PrEP services related to the lockdown period. Fourth, in our meta-analysis, the sample was drawn from various subsamples or was part of a larger study, which resulted in a lack of specificity regarding age, gender, and rural/urban location within the subsamples in the included studies. Fifth, reduced at-risk behavior may have led to a decline in PrEP need or a change from daily dosing to event-based dosing in MSM. This could have resulted in an overestimate of the level of disruption as some PrEP users who reported not being able to access PrEP services may not in fact have needed them. Finally, all studies used self-reported measures of disruptions to accessing PrEP services, and this may be prone to social desirability bias.77 Considering this limitation, future research on this topic could explore alternative methods, such as using health clinic visit data for PrEP appointment attendance, prescriptions, or refills. This approach may offer complementary evidence to generate a richer understanding of disruptions in PrEP service utilization.
CONCLUSIONS
This systematic review and meta-analysis quantified the level of disruptions in access to PrEP services during the COVID-19 pandemic. Policymakers and health providers need to ensure that PrEP users can continue to access PrEP services during public health crises and emergencies. Strategies worthy of consideration include the provision of financial support interventions including cost-sharing, digital or multi-month prescription or supply of medicines, telehealth consultations, and PrEP home delivery, including the provision of HIV self-testing.
Supplementary Material
Footnotes
The authors have no funding or conflicts of interest to disclose.
L. P. L. Wulandari, D. Boettiger, V. Wiseman: conceptualization of the study. L. P. L. Wulandari, D. Boettiger, S. N. S. Negara, Y. A. Mashuri, S. D. Wahyuningtias, I. W. C. S. D. Putra: identification of papers. L. P. L. Wulandari, D. Boettiger, S. N. S. Negara, Y. A. Mashuri, S. D. Wahyuningtias, I. W. C. S. D. Putra: data extraction. L. P. L. Wulandari: formal analysis, validation, visualization. L. P. L. Wulandari: writing—original draft. All authors: writing—review & editing. All authors took the decision to submit for publication.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
Data Availability Statement: All authors had access to the data. Datasets of this study are available upon reasonable request to this corresponding author.
D. Boettiger and V. Wiseman have contributed equally to the work.
REFERENCES
- 1.Estcourt C, Yeung A, Nandwani R, et al. Population-level effectiveness of a national HIV preexposure prophylaxis programme in MSM. AIDS (London, England). 2021;35:665–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grulich AE, Guy R, Amin J, et al. Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. Lancet HIV. 2018;5:e629–e637. [DOI] [PubMed] [Google Scholar]
- 3.Phanuphak N, Sungsing T, Jantarapakde J, et al. Princess PrEP program: the first key population-led model to deliver pre-exposure prophylaxis to key populations by key populations in Thailand. Sex Health. 2018;15:542–555. [DOI] [PubMed] [Google Scholar]
- 4.Smith DK, Sullivan PS, Cadwell B, et al. Evidence of an association of increases in pre-exposure prophylaxis coverage with decreases in human immunodeficiency Virus diagnosis rates in the United States, 2012-2016. Clin Infect Dis. 2020;71:3144–3151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UNAIDS . Global AIDS Strategy 2021-2026—End Inequalities. End AIDS. Geneva: UNAIDS; 2021. [Google Scholar]
- 6.UNAIDS . Political Declaration on HIV and AIDS: Ending Inequalities and Getting on Track to End AIDS by 2030. Geneva: UNAIDS; 2021. [Google Scholar]
- 7.World Health Organization . Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. 2nd ed. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 8.World Health Organization. Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations – 2016 Update. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 9.United Nations General Assembly . Political Declaration on HIV and AIDS: On the Fast Track to Accelerating the Fight against HIV and to Ending the AIDS Epidemic by 2030. New York: United Nations; 2016. [Google Scholar]
- 10.WHO . Global Health Sector Strategies on, Respectively, HIV, Viral Hepatitis and Sexually Transmitted Infections for the Period 2022-2030. Geneva: World Health Organization; 2022. [Google Scholar]
- 11.World Health Organization . COVID-19 Public Health Emergency of International Concern (PHEIC) Global Research and Innovation Forum. Geneva: World Health Organization; 2020. [Google Scholar]
- 12.World Health Organization . WHO COVID-19 Dashboard. Geneva: World Health Organization; 2024. [Google Scholar]
- 13.Global HIV Prevention Coalition . Preventing HIV Infections at the Time of a New Pandemic: A Synthesis Report on Programme Disruptions and Adaptations during the COVID-19 Pandemic in 2020. Geneva: UNAIDS; 2020. [Google Scholar]
- 14.Kiarie H, Temmerman M, Nyamai M, et al. The COVID-19 pandemic and disruptions to essential health services in Kenya: a retrospective time-series analysis. Lancet Glob Health. 2022;10:e1257–e1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SeyedAlinaghi S, Mirzapour P, Pashaei Z, et al. The impacts of COVID-19 pandemic on service delivery and treatment outcomes in people living with HIV: a systematic review. AIDS Res Ther. 2023;20:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer D, Slone SE, Ogungbe O, et al. Impact of the COVID-19 pandemic on HIV healthcare service engagement, treatment adherence, and viral suppression in the United States: a systematic literature review. AIDS Behav. 2023;27:344–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao A, Rucinski K, Jarrett BA, et al. Perceived interruptions to HIV prevention and treatment services associated with COVID-19 for gay, bisexual, and other men who have sex with men in 20 countries. J Acquir Immune Defic Syndr. 2021;87:644–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong C, Horvath KJ, Stephenson R, et al. PrEP use and persistence among young sexual minority men 17-24 Years old during the COVID-19 pandemic. AIDS Behav. 2022;26:631–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davey DLJ, Bekker L-G, Mashele N, et al. PrEP retention and prescriptions for pregnant women during COVID-19 lockdown in South Africa. Lancet HIV. 2020;7:e735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen YT, Duncan DT, Del Vecchio N, et al. COVID-19-Related stressors, sex behaviors, and HIV status neutral care among black men who have sex with men and transgender women in Chicago, USA. J Acquir Immune Defic Syndr. 2021;88:261–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacCarthy S, Izenberg M, Barreras JL, et al. Rapid mixed-methods assessment of COVID-19 impact on Latinx sexual minority men and Latinx transgender women. PLoS One. 2020;15:e0244421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Legesse AY, Hadush Z, Teka H, et al. Lived experience of healthcare providers amidst war and siege: a phenomenological study of Ayder Comprehensive Specialized Hospital of Tigray, Northern Ethiopia. BMC Health Serv Res. 2024;24:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elnakib S, Elaraby S, Othman F, et al. Providing care under extreme adversity: the impact of the Yemen conflict on the personal and professional lives of health workers. Soc Sci Med. 2021;272:113751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gesesew H, Berhane K, Siraj ES, et al. The impact of war on the health system of the Tigray region in Ethiopia: an assessment. BMJ Glob Health. 2021;6:e007328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Behrman JA, Weitzman A. Effects of the 2010 Haiti earthquake on women's reproductive health. Stud Fam Plann. 2016;47:3–17. [DOI] [PubMed] [Google Scholar]
- 26.Djafri D, Chongsuvivatwong V, Geater A. Effect of the September 2009 Sumatra earthquake on reproductive health services and MDG 5 in the city of Padang, Indonesia. Asia Pac J Public Health. 2015;27:Np1444–1456. [DOI] [PubMed] [Google Scholar]
- 27.Ray-Bennett NS, Corsel DMJ, Goswami N, et al. Understanding reproductive health challenges during a flood: insights from Belkuchi Upazila, Bangladesh. Gates Open Res. 2019;3:788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKay G, Black B, Mbambu Kahamba S, et al. Not All that Bleeds Is Ebola: How Has the DRC Ebola Outbreak Impacted Sexual and Reproductive Health in North-Kivu? New York, NY: The International Rescue Committee; 2019. [Google Scholar]
- 29.WHO. Building Health Systems Resilience for Universal Health Coverage and Health Security during the COVID-19 Pandemic and beyond: A Brief on the WHO Position; 2021. [Google Scholar]
- 30.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M, Hedges LV, Higgins JP, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. [DOI] [PubMed] [Google Scholar]
- 32.Ryan R, CCaCRG. Heterogeneity and Subgroup Analyses in Cochrane Consumers and Communication Group Reviews: Planning the Analysis at Protocol Stage. UK: Cochrane Consumers and Communication Review Group; 2016. [Google Scholar]
- 33.Ford N, Patten G, Rangaraj A, et al. Outcomes of people living with HIV after hospital discharge: a systematic review and meta-analysis. Lancet HIV. 2022;9:e150–e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ottawa Hospital Research Institute, University of Oxford, Monash University. PRISMA: transparent reporting of systematic reviews and meta-analyses; 2009. Available at: http://www.prisma-statement.org/. Accessed June 16, 2016.
- 35.The Joanna Briggs Institute . The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Prevalence Studies. Adelaide: The Joanna Briggs Institute; 2017. [Google Scholar]
- 36.Tola A, Assefa N, Dessie Y, et al. Epidemiology of hyperglycemia during pregnancy in Ethiopia: prevalence, associated factors, and feto-maternal outcomes: systematic review and meta-analysis. Syst Rev. 2024;13:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torres TS, Hoagland B, Bezerra DRB, et al. Impact of COVID-19 pandemic on sexual minority populations in Brazil: an analysis of social/racial disparities in maintaining social distancing and a description of sexual behavior. AIDS Behav. 2021;25:73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Bank . World Bank Country and Lending Groups. Washington, DC: World Bank; 2024. [Google Scholar]
- 39.Camp C, Saberi P. Facilitators and barriers of 2-1-1 HIV preexposure prophylaxis. PLoS ONE. 2021;16:e0251917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ciaccio MD, Villes V, Michels D, et al. Impact of the early 2020 COVID-19 crisis and lockdown on PrEP use among men who have sex with men (MSM) in France. Sex Transm Infections. 2022;98:510–517. [DOI] [PubMed] [Google Scholar]
- 41.Hammoud MA, Grulich A, Holt M, et al. Substantial decline in use of HIV preexposure prophylaxis following introduction of COVID-19 physical distancing restrictions in Australia: results from a prospective observational study of gay and bisexual men. J Acquir Immune Defic Syndr. 2021;86:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mistler CB, Curley CM, Rosen AO, et al. The impact of COVID-19 on access to HIV prevention services among opioid-dependent individuals. J Community Health. 2021;46:960–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morgan E, Caba AE, Eaton LA, et al. PrEP access affected by COVID-19 is associated with increased odds of HIV seroconversion. J Acquir Immune Defic Syndr. 2022;91:138–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pampati S, Emrick K, Siegler AJ, et al. Changes in sexual behavior, PrEP adherence, and access to sexual health services because of the COVID-19 pandemic among a cohort of PrEP-using MSM in the south. J Acquir Immune Defic Syndr. 2021;87:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reyniers T, Rotsaert A, Thunissen E, et al. Reduced sexual contacts with non-steady partners and less PrEP use among MSM in Belgium during the first weeks of the COVID-19 lockdown: results of an online survey. Sex Transm Infections. 2021;97:414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stephenson R, Chavanduka TMD, Rosso MT, et al. Sex in the time of COVID-19: results of an online survey of gay, bisexual and other men who have sex with men's experience of sex and HIV prevention during the US COVID-19 epidemic. AIDS Behav. 2021;25:40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crawford FW, Wu J, Heimer R. Hidden population size estimation from respondent-driven sampling: a network approach. J Am Stat Assoc. 2018;113:755–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang YLA, Zhu W, Wiener J, et al. Impact of coronavirus disease 2019 (COVID-19) on human immunodeficiency Virus (HIV) pre-exposure prophylaxis prescriptions in the United States-A time-series analysis. Clin Infect Dis. 2022;75:e1020–e1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hong C, Huh D, Schnall R, et al. Changes in high-risk sexual behavior, HIV and other STI testing, and PrEP use during the COVID-19 pandemic in a longitudinal cohort of adolescent men who have sex with men 13 to 18 years old in the United States. AIDS Behav. 2023;27:1133–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iain H, Diarmuid N, Gary George W, et al. COVID-19 restrictions and changing sexual behaviours in HIV-negative MSM at high risk of HIV infection in London, UK. Sex Transm Infections. 2021;97:521–524. [DOI] [PubMed] [Google Scholar]
- 51.Howarth AR, Saunders J, Reid D, et al. “Stay at home …”: exploring the impact of the COVID-19 public health response on sexual behaviour and health service use among men who have sex with men: findings from a large online survey in the UK. Sex Transm Infect. 2022;98:346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Srikanth K, Killelea A, Strumpf A, et al. Associated costs are a barrier to HIV preexposure prophylaxis access in the United States. Am J Public Health. 2022;112:834–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Unger ZD, Golub SA, Borges C, et al. Reasons for PrEP discontinuation after navigation at sexual health clinics: interactions among systemic barriers, behavioral relevance, and medication concerns. J Acquir Immune Defic Syndr. 2022;90:316–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chan C, Fraser D, Vaccher S, et al. Overcoming barriers to HIV pre-exposure prophylaxis (PrEP) coverage in Australia among Medicare-ineligible people at risk of HIV: results from the MI-EPIC clinical trial. Sex Health. 2022;18:453–459. [DOI] [PubMed] [Google Scholar]
- 55.Gaspar M, Grey C, Wells A, et al. Public health morality, sex, and COVID-19: sexual minority men's HIV pre-exposure prophylaxis (PrEP) decision-making during Ontario's first COVID-19 lockdown. Crit Public Health. 2022;32:116–126. [Google Scholar]
- 56.Qiao S, Li Z, Weissman S, et al. Disparity in HIV service interruption in the outbreak of COVID-19 in South Carolina. AIDS Behav. 2021;25:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bedado D, Kaso AW, Hailu A. Magnitude and determinants of out of pocket health expenditure among patients visiting outpatients in public hospitals in East Shoa Zone, Ethiopia. Clin Epidemiol Glob Health. 2022;15:101066. [Google Scholar]
- 58.Wirawan GB, Wardhani BDK, Pradnyani PE, et al. Behavioral changes, adaptation, and supports among Indonesian female sex workers facing dual risk of COVID-19 and HIV in a pandemic. Int J Environ Res Public Health. 2022;19:1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Iversen J, Sabin K, Chang J, et al. COVID-19, HIV and key populations: cross-cutting issues and the need for population-specific responses. J Int AIDS Soc. 2020;23:e25632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brooke GR, Sosnowy C, Zanowick-Marr A, et al. Facilitators for retaining men who have sex with men in pre-exposure prophylaxis care in real world clinic settings within the United States. BMC Infect Dis. 2022;22:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention: US Public Health Service . Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: A Clinical Practice Guideline. Atlanta: Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 62.Xiridou M, Heijne J, Adam P, et al. How the disruption in sexually transmitted infection care due to the COVID-19 pandemic could lead to increased sexually transmitted infection transmission among men who have sex with men in The Netherlands: a mathematical modeling study. Sex Transm Dis. 2022;49:145–153. [DOI] [PubMed] [Google Scholar]
- 63.Hoagland B, Torres TS, Bezerra DRB, et al. Telemedicine as a tool for PrEP delivery during the COVID-19 pandemic in a large HIV prevention service in Rio de Janeiro-Brazil. Braz J Infect Dis. 2020;24:360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kerzner M, De AK, Yee R, et al. Pre-exposure prophylaxis (PrEP) uptake and service delivery adaptations during the first wave of the COVID-19 pandemic in 21 PEPFAR-funded countries. PLoS One. 2022;17:e0266280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Quirke S, Quinn L, Hegarty D, et al. Virtual HIV pre-exposure prophylaxis outpatient service in the era of COVID-19. Int J STD AIDS. 2021;32:100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Phillips TR, Fairley CK, Donovan B, et al. Sexual health service adaptations to the coronavirus disease 2019 (COVID-19) pandemic in Australia: a nationwide online survey. Aust N Z J Public Health. 2021;45:622–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Henderson L, Gibbs J, Quinn J, et al. Maintaining access to HIV pre-exposure prophylaxis in a pandemic: a service evaluation of telephone-based pre-exposure prophylaxis provision. Int J STD AIDS. 2022;33:718–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matambanadzo P, Busza J, Mafaune H, et al. It went through the roof": an observation study exploring the rise in PrEP uptake among Zimbabwean female sex workers in response to adaptations during Covid-19. J Int AIDS Soc. 2021;24:e25813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Greenhalgh F Von Lingen A Cigan B, et al. How Has the COVID-19 Response Changed Medicine Deliveries for People Living with or at Risk of HIV? Glasgow, Scotland: HIV Glasgow Congress; 2020. [Google Scholar]
- 70.Rosen JG, Zhang L, Pelaez D, et al. Provider perspectives on HIV pre-exposure prophylaxis service disruptions and adaptations during the COVID-19 pandemic in Baltimore, Maryland: a qualitative study. AIDS Patient Care STDS. 2022;36:313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wulandari LPL, Negara SNS, Wahyuningtias SD, et al. Delivering HIV and TB services amidst the COVID-19 pandemic in Indonesia: a qualitative study of challenges and mitigation strategies. J Glob Health Rep. 2024;8. [Google Scholar]
- 72.Mashuri YA, Boettiger D, Wahyuningtias SD, et al. “I pity the TB patient”: a mixed methods study assessing the impact of the COVID-19 pandemic on TB services in two major Indonesian cities and distilling lessons for the future. BMJ Glob Health. 2024;9:e014943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hoagland B, Torres TS, Bezerra DRB, et al. High acceptability of PrEP teleconsultation and HIV self-testing among PrEP users during the COVID-19 pandemic in Brazil. Braz J Infect Dis. 2021;25:101037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roth AM, Tran NK, Felsher M, et al. Integrating HIV preexposure prophylaxis with community-based syringe services for women who inject drugs: results from the project SHE demonstration study. J Acquir Immune Defic Syndr. 2021;86:e61–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Furukawa NW, Weimer M, Willenburg KS, et al. Expansion of preexposure prophylaxis capacity in response to an HIV outbreak among people who inject drugs-cabell county, West Virginia, 2019. Public Health Rep. 2022;137:25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Boyd AT, Jahun I, Dirlikov E, et al. Expanding access to HIV services during the COVID-19 pandemic-Nigeria, 2020. AIDS Res Ther. 2021;18:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Latkin CA, Mai NVT, Ha TV, et al. Social desirability response bias and other factors that may influence self-reports of substance use and HIV risk behaviors: a qualitative study of drug users in Vietnam. AIDS Educ Prev. 2016;28:417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]