Abstract
Introduction:
Colorectal cancer (CRC) is the second leading cause of cancer deaths in Latinos in the U.S., but it is unclear, from previous research, whether Latinos have differing rates of CRC screening methods compared with non-Hispanic Whites.
Methods:
This study used electronic health records from 686 community health centers across 21 states in the Accelerating Data Value Across a National Community Health Center of the National Patient-Centered Clinical Research Network. Records from English-preferring Latinos, Spanish-preferring Latinos, and non-Hispanic Whites aged 50–75 years were included. Five outcomes were compared between 2012 and 2017 to provide a comprehensive view of CRC screening: (1) any CRC screening, (2) stool-based screening, (3) annual rates of stool testing, (4) any referral for lower gastrointestinal endoscopy, and (5) endoscopy referral among patients with a positive stool-based screening.
Results:
In this study (N=204,243), Spanish-preferring Latinos had higher odds of any CRC screening (OR=1.44, 95% CI=1.23, 1.68), and stool-based testing (OR=1.82, 95% CI=1.55, 2.13) compared with non-Hispanic Whites. English- and Spanish-preferring Latinos had lower odds of having ever had a referral for endoscopy in the study period compared with non-Hispanic Whites (English: OR=0.23, 95% CI=0.15, 0.34; Spanish: OR=0.55, 95% CI=0.40, 0.74), even with a positive stool-based screening (English: OR=0.14, 95% CI=0.06, 0.33; Spanish: OR=0.33, 95% CI=0.19, 0.57).
Conclusions:
In a multi-state network of community health centers, Latino patients aged >50 years were more likely to receive stool-based screening tests for CRC than non-Hispanic Whites, but were less likely to receive endoscopy referrals than non-Hispanic Whites, even when experiencing a positive stool-based screening test. Initiatives to improve Latino CRC outcomes should encourage indicated referrals for lower gastrointestinal endoscopy.
INTRODUCTION
Cancer is the leading cause of death in Latinos.1 Colorectal cancer (CRC) is the second most prevalent cancer in Latinos, and the second leading cause of cancer death.2 In the last 20 years, screening for CRC in accordance with national guidelines3,4 has increased across numerous demographic groups, including Latinos. However, the increases in screening and improvements in outcomes have not been equivalent across all groups,3–5 and, according to survey data, Latinos in the U.S. are less likely to undergo CRC screening than non-Hispanic Blacks and non-Hispanic Whites.6,7
Studies have shown varying associations between receipt of screening endoscopy and various demographic features within Latino populations (geographic region of residence, income, other features in small numbers of clinics, narrowly defined geographic regions8–12), but not in large populations, over extended periods of time, or with significant consideration of crucial demographics in Latinos, such as preferred language, income, and insurance. Similarly, numerous local interventions have increased CRC screening among Latinos in a single clinic or small network of clinics,13–20 but assessment of completion of CRC screening in large populations of Latinos in a broad, real-world sample has been lacking.
Full understanding of screening disparities requires multi-year observations, as screening services and recommendations encompass multi-year time periods, in order to best inform population-wide improvement efforts in CRC screening. Also, Latino populations are disproportionately cared for in the nation’s community health centers (CHCs),21 facilities that routinely care for patients at risk of underscreening.22 Consideration of this setting is necessary to adequately evaluate screening in the specific Latino populations that may be at risk for underscreening, delayed diagnoses, and poor cancer outcomes. Specifically, as stool-based testing has been implemented widely, it is uncertain if the tests are used with recommended frequency (annually23), and if abnormal findings consistently result in follow-up endoscopy in the Latino population seeking care at CHCs.
In order to better understand long-term patterns of CRC screening among Latinos over time in real-world primary care settings, as well as provide better population-wide targets for improvement and equity, this large observational study evaluates CRC screening among Latino patients (English- and Spanish-preferring), compared with non-Hispanic White patients over a multi-year period using an electronic health record (EHR) data set spanning hundreds of CHCs across multiple states. It is hypothesized that Latino patients, when compared with non-Hispanic Whites, are less likely to receive all measurable screening modalities, less frequently screened when stool-based testing is employed, and less likely to be referred to endoscopy/follow-up when stool testing is abnormal.
METHODS
Patient-level EHR data from the Accelerating Data Value Across a National Community Health Center (ADVANCE) of the National Patient-Centered Clinical Research Network was utilized.24 These data were representative of 686 CHCs in 21 states (AK, CA, FL, GA, HI, IN, KS, MA, MD, MN, MO, MT, NC, NM, NV, OH, OR, RI, TX, WA, WI). Further details of the ADVANCE clinical data research network are described elsewhere.25 ADVANCE clinical data are routinely assessed for completeness and quality following the National Patient-Centered Clinical Research Network’s standard analytic queries and data quality check process, and have low missingness on relevant variables.
Study Population
The study population consisted of screening-eligible adults seen at ADVANCE CHCs, aged 50–75 years, with a face-to-face visit to a study clinic from January 1, 2012 to December 31, 2017.
Measures
Patients with a documented diagnosis of CRC or a surgical history of colectomy prior to the study start date or who received a diagnosis of CRC during the study period were excluded. Owing to scarcity of data for other languages, racial and ethnic groups were limited to: non-Hispanic Whites who prefer English, Latinos who prefer Spanish, and Latinos who prefer English.
Using Current Procedural Terminology and ICD-9 or ICD-10 codes, 5 outcomes to provide a comprehensive view of CRC screening in this setting were considered: (1) binary indicator denoting any CRC screening in the study period (i.e., results for any stool-based screening method or referral for colonoscopy or colonography or sigmoidoscopy26); (2) among patients without referral for endoscopy, a binary indicator denoting the presence of results of a stool-based screening method; (3) among patients with a stool-based method, annual rates of stool-based screening; (4) binary indicator denoting referral for lower gastrointestinal endoscopy (colonoscopy or flexible sigmoidoscopy); and (5) among patients with a positive stool-based screening, a binary indicator denoting endoscopy referral. For the stool-based screening rate outcome, each patient’s person time in the study/denominator was estimated using previously described approaches.27 Patient’s observation time/denominator was equal to the time between first and last visit plus 3 years after their last clinical encounter28; they had to be re-entered into observation if absent for >3 years.
The main independent variable distinguished 3 groups of adults using ethnicity and language data: (1) non-Hispanic Whites, (2) Spanish-preferring Latinos, and (3) English-preferring Latinos. Ethnicity and preferred language information is self-identified in the routine course of clinical care at CHCs. These data elements have a low proportion of missingness, as CHCs are federally mandated to collect these data.29 The term “Latino” is used because it is often preferred in the study population; the actual collected ethnicity variable is Hispanic and non-Hispanic.
Analyses included important patient-level EHR-derived confounders including age at first visit, sex, insurance status pattern measured across visits (never insured, some private insurance, some public insurance, and some public and private), average BMI across study visits, patient’s income across visits as a percentage of the U.S. federal poverty level (>138% or <138%), number of clinical encounters in the study period, diabetes diagnosis, atherosclerotic cardiovascular disease diagnosis, and U.S. region (Northeast, South, Midwest, West). Diabetes and heart disease were included as covariates as the presence of these features may: (1) affect utilization and care seeking and (2) especially with respect to heart disease, be associated with provider likelihood to order endoscopy (a procedure with potential cardiac risk).
Statistical Analysis
Patient characteristics are described in total and by the 3 ethnicity/language groups. For the binary outcomes of any CRC screening, endoscopy, and any stool-based testing among those without endoscopy referrals, logistic regression models were fitted to estimate ORs and their corresponding 95% CIs comparing ethnicity/language groups adjusted for covariates. For the outcome of yearly rate of stool-based testing, Poisson regression models were fitted to estimate adjusted rate ratios comparing ethnicity groups adjusted for covariates. All models accounted for the clustering of patients within clinics using a robust sandwich variance estimator. Analyses were conducted in Stata, version 15 and statistical significance was set at p-value<0.05. This study was reviewed by the IRB of Oregon Health & Science University.
RESULTS
Characteristics of the study population (N=204,243) are included in Table 1. Notably, more of the Spanish-preferring Latinos in the cohort (31% of the sample) were female, never insured, and more likely to have income <138% of the federal poverty level. English-preferring Latinos showed similar, but less stark differences compared with non-Hispanic Whites. Overall, 22.7% of non-Hispanic Whites, 30.0% of Spanish-preferring Latinos and 22.3% of English-preferring Latinos had any CRC screening in the study period. Non-Hispanic Whites demonstrated a higher prevalence of endoscopy (8.8%) compared with both Latino groups (Spanish=4.3%, English=2.4%). Whereas Latinos had a higher prevalence of fecal occult blood testing compared with non-Hispanic Whites, they had a lower prevalence of endoscopy after a positive fecal occult blood test (non-Hispanic Whites=19.8%, Spanish-preferring Latinos=4.5%, English-preferring Latinos=3.5%).
Table 1.
Characteristics of Older Adult Patients in the ADVANCE network January 1, 2012–December 31, 2017 (N=204,243), Overall and by Ethnicity and Language Group
| Ethnicity/Language group |
||||
|---|---|---|---|---|
| Characteristics | Overall | Non-Hispanic White | Latino preferring Spanish | Latino preferring English |
| N (row %) | 204,243 | 113,439 (55.5) | 63,062 (30.9) | 27,742 (13.6) |
| Age,a years | ||||
| 50–55 | 22,341 (10.9) | 13,656 (12.0) | 5,571 (8.8) | 3,114 (11.2) |
| 55–60 | 81,471 (39.9) | 45,620 (40.2) | 24,258 (38.5) | 11,593 (41.8) |
| 60–65 | 73,949 (36.2) | 39,983 (35.2) | 24,028 (38.1) | 9,938 (35.8) |
| 65–70 | 24,939 (12.2) | 13,421 (11.8) | 8,601 (13.6) | 2,917 (10.5) |
| 70–75 | 1,543 (0.8) | 759 (0.7) | 604 (1.0) | 180 (0.6) |
| Female | 115,082 (56.3) | 60,940 (53.7) | 38,432 (60.9) | 15,710 (56.6) |
| Insurance over study period | ||||
| Never insured | 43,222 (21.2) | 21,099 (18.6) | 16,053 (25.5) | 6,070 (21.9) |
| Some private | 32,247 (15.8) | 20,112 (17.7) | 8,021 (12.7) | 4,114 (14.8) |
| Some public | 111,260 (54.5) | 62,073 (54.7) | 34,358 (54.5) | 14,829 (53.5) |
| Some public and private | 17,514 (8.6) | 10,155 (9.0) | 4,630 (7.3) | 2,729 (9.8) |
| BMI, mean (SD) | 30 (6.7) | 30 (7.3) | 30 (5.6) | 30 (6.5) |
| Diabetes diagnosis | 54,271 (26.6) | 23,082 (20.3) | 22,694 (36.0) | 8,495 (30.6) |
| ASCVD diagnosis | 19,254 (9.4) | 12,458 (11.0) | 4,415 (7.0) | 2,381 (8.6) |
| Federal poverty level over study period | ||||
| <138% | 139,408 (68.3) | 69,002 (60.8) | 50,424 (80.0) | 19,982 (72.0) |
| ≥138% | 33,826 (16.6) | 23,044 (20.3) | 6,393 (10.1) | 4,389 (15.8) |
| Not documented | 31,009 (15.2) | 21,393 (18.9) | 6,245 (9.9) | 3,371 (12.2) |
| Number of encounters over study period, mean (SD) | 10.9 (13.1) | 10.8 (13.7) | 11.2 (12.0) | 10.8 (12.7) |
| Colorectal cancer screening uptake prevalence | ||||
| Any screenb | 50,869 (24.9) | 25,729 (22.7) | 18,940 (30) | 6,200 (22.3) |
| Endoscopy referralb | 13,315 (6.5) | 9,970 (8.8) | 2,692 (4.3) | 653 (2.4) |
| Stool based screenc | 40,071 (21) | 17,645 (16.6) | 16,777 (28.4) | 5,649 (21.8) |
| Stool based screen rate per 100 person yearsd | 46.7 | 46.6 | 49.5 | 39.1 |
| Endoscopy referral after positive stool-based screene | 529 (12.1) | 440 (19.8) | 65 (4.5) | 24 (3.5) |
| Person years in study | ||||
| [1,2) | 31,464 (15.4) | 17,510 (15.4) | 10,134 (16.1) | 3,820 (13.8) |
| [2,3) | 55,812 (27.3) | 30,938 (27.3) | 18,082 (28.7) | 6,792 (24.5) |
| [3,4) | 49,539 (24.3) | 28,414 (25.0) | 14,207 (22.5) | 6,918 (24.9) |
| [4,5) | 24,676 (12.1) | 14,535 (12.8) | 6,639 (10.5) | 3,502 (12.6) |
| [5,6] | 42,752 (20.9) | 22,042 (19.4) | 14,000 (22.2) | 6,710 (24.2) |
Notes: N (col %) reported unless otherwise noted.
At start of the study period.
Denominator is the full population n=(204,243 for overall; 113,439 for Non-Hispanic White; 63,062 for Latino preferring Spanish; 27,742 for Latino preferring English).
Out of population without endoscopy screening n=(190,928 for overall; 106,086 for Non-Hispanic White; 58,983 for Latino preferring Spanish; 25,948 for Latino preferring English).
Out of person years contributed by patients with at least 1 stool-based screen n=(158,298 for overall; 69,488 for Non-Hispanic White; 65,054 for Latino preferring Spanish; 23,756 for Latino preferring English).
Out of population with positive stool-based screen result n=(4,360 for overall; 2,223 for Non-Hispanic White; 1,452 for Latino preferring Spanish; 685 for Latino preferring English).
ASCVD, atherosclerotic cardiovascular disease.
Figure 1 demonstrates the covariate-adjusted ORs of any CRC screening, stool-based screening, and covariate-adjusted relative rates of stool-based screening comparing Spanish-preferring and English-preferring Latinos to the reference group of non-Hispanic Whites. Full model results are available in Appendix Table 1. Spanish-preferring Latinos had higher odds of any CRC screening compared with non-Hispanic Whites (OR=1.44, 95% CI=1.23, 1.68); English-preferring Latinos did not differ from non-Hispanic Whites (OR=0.93, 95% CI=0.81, 1.07). Among patients without any referral for endoscopy, Spanish-preferring (OR=1.82, 95% CI=1.55, 2.13) and English-preferring (OR=1.28, 95% CI=1.10, 1.49) Latinos had increased odds of having ever received stool-based screening for CRC. Among patients with a stool-based method, English-preferring Latinos had significantly lower annual rates of testing (rate ratio=0.88, 95% CI=0.79, 0.97) whereas Spanish-preferring Latinos had a slightly higher rate of stool testing (rate ratio=1.11, 95% CI=0.99, 1.25) than non-Hispanic Whites. However, these did not meet statistical significance for Spanish-preferring Latinos.
Figure 1.
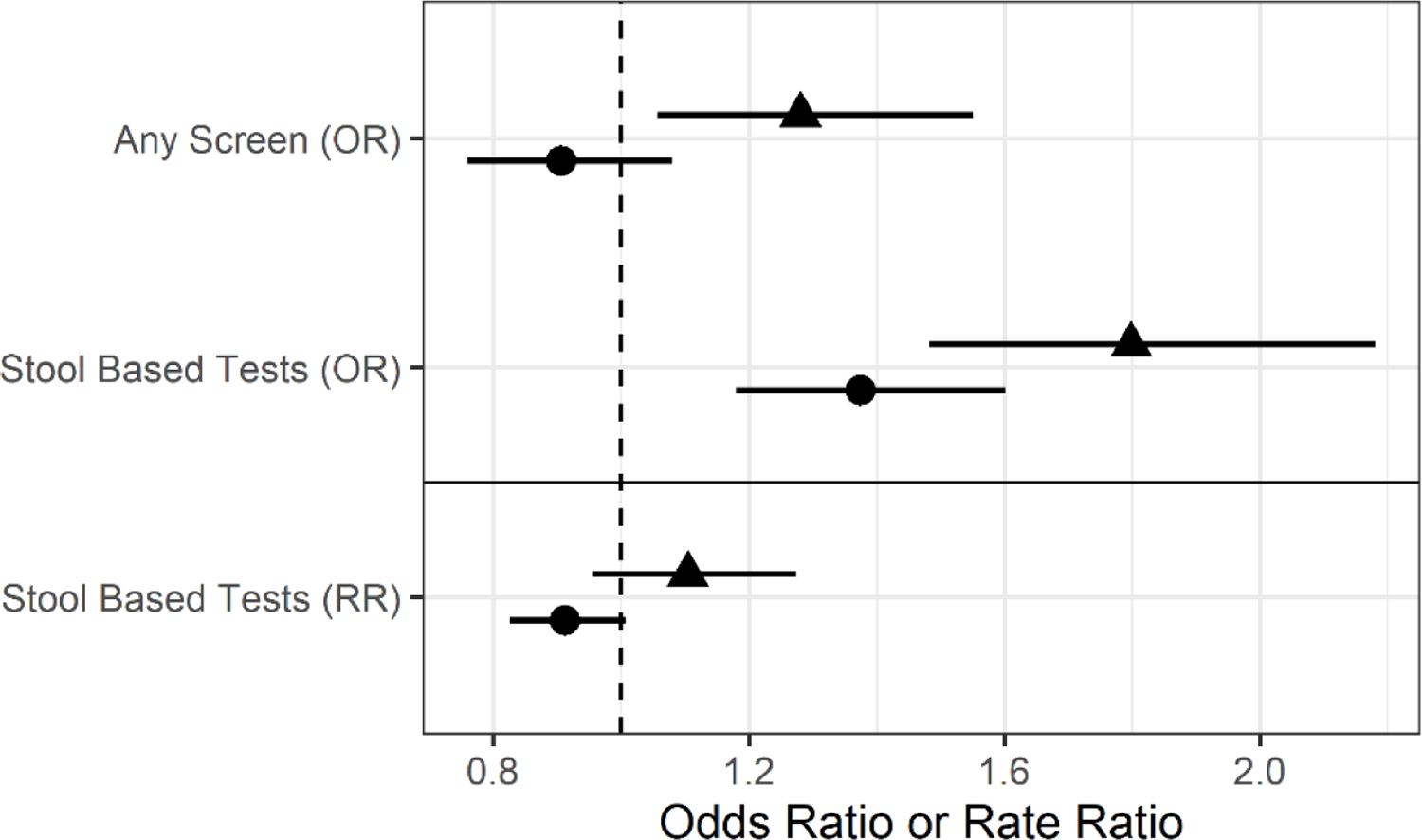
AORs of having received any colorectal cancer (CRC) screening, stool-based screening (among patients without a referral for endoscopy), and adjusted relative rates of stool-based screening (among patients with a stool-based method).
Notes: The reference group is non-Hispanic Whites. For the binary outcomes of any CRC screening, and any stool-based testing among those without endoscopy referrals, the authors fit logistic regression models to estimate ORs and their corresponding 95% CIs comparing ethnicity/language groups adjusted for age, sex, insurance, BMI, income, number of clinical encounters in the study period, diabetes diagnosis, atherosclerotic cardiovascular disease diagnosis, and U.S. region. For the outcome of yearly rate of stool-based testing the authors fit Poisson regression models to estimate adjusted rate ratios (RR) comparing ethnicity groups adjusted for covariates. All models accounted for the clustering of patients within clinics using a robust sandwich variance estimator.
language
 English
English
 Spanish
Spanish
RR, rate ratio.
Figure 2 displays the covariate-adjusted findings regarding lower gastrointestinal endoscopy. English- and Spanish-preferring Latinos had lower odds of having ever had a referral for endoscopy in the study period compared with non-Hispanic Whites (English: OR=0.23, 95% CI=0.15, 0.34; Spanish: OR=0.55, 95% CI=0.40, 0.74). Among patients with a positive stool-based screening, Spanish-preferring Latinos (OR=0.33, 95% CI=0.19, 0.57) and English-preferring Latinos (OR=0.14, 95% CI=0.06, 0.33) showed lower odds of receiving endoscopy referrals compared with non-Hispanic Whites.
Figure 2.
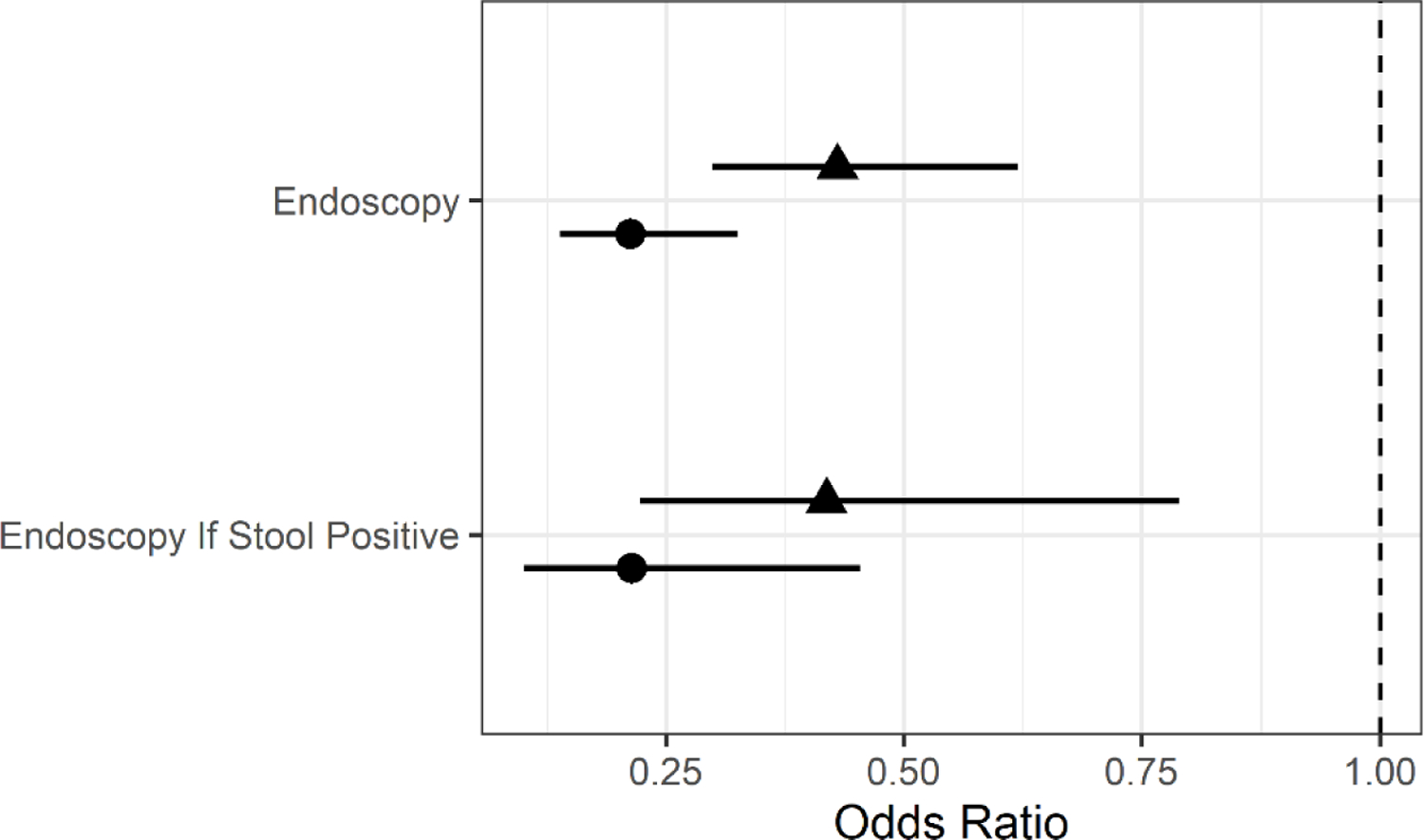
AORs of having received an endoscopy referral, and having received an endoscopy referral if stool positive.
Notes: The reference group is non-Hispanic Whites. The authors fit logistic regression models to estimate ORs and their corresponding 95% CIs comparing ethnicity/language groups adjusted for age, sex, insurance, BMI, income, number of clinical encounters in the study period, diabetes diagnosis, atherosclerotic cardiovascular disease diagnosis, and U.S. region. All models accounted for the clustering of patients within clinics using a robust sandwich variance estimator.
language
 English
English
 Spanish
Spanish
DISCUSSION
This analysis of CRC screening services in >200,000 Latino and non-Hispanic White patients in a multistate network of CHCs is one of the first to evaluate CRC screening equity in such a large, real-world sample over time using EHRs. Primarily, Latino patients were more likely than White patients to receive stool-based screening but less likely to receive endoscopy referrals, even when they had a positive stool-based screening test. Previous work has evaluated similar outcomes among Latino language groups in a smaller CHC sample9 and in national survey data,11 producing disparate findings: Liss and colleagues9 found higher colonoscopy rates in Spanish speakers after positive stool testing, whereas Diaz et al.30 found lower screening rates in Latino men with limited English proficiency. This study examined some of these same factors and outcomes in a larger geographically heterogeneous sample over time, potentially informing clinical and population health efforts to improve CRC screening more broadly.
Several results are notable. The prevalence of any screening in the sample was low overall. However, the analysis was not designed for or capable of determining which patients were “due” for screening (i.e., patients with completed screening tests in the years immediately prior to the study period), so this prevalence cannot be compared to national estimates of those up-to-date on screening. Still, these results underscore the critical need for CRC screening to be a high priority for underserved patients in primary care, especially among those seen in CHCs. In the adjusted analysis, Latino patients were more likely to receive stool-based testing than non-Hispanic White patients. Stool-based testing is generally inexpensive and can be easily implemented by CHCs,15,18,20 which often have community, cultural, and language engagement/resources31,32 that might facilitate the equitable implementation of this screening, or focus more so on Latino patients. Other work in this practice-based research network has demonstrated increased utilization of other preventive services as well.33–35 In the setting of disparities in cancer outcomes in recent years, equitable Latino utilization of this service in the community health setting is an encouraging direction.
However, stool-based testing is only part of a comprehensive approach to colon cancer prevention and early detection. In this study, Latinos were less likely to be referred for endoscopy, especially, and most concerningly, after a positive stool test (which should trigger a follow-up referral or order for a colonoscopy). Possible explanations for this trend may include communication difficulties from provider–patient language discordance, or providers may misunderstand patient barriers or intentions around getting endoscopy. This analysis adjusted for insurance (uninsured patients may have trouble paying for a colonoscopy, which can be costly) and some significant comorbidities (which may affect the likelihood of a referral for an invasive procedure). Although some endoscopies may be performed in CHCs, many require a referral to another facility or provider, which may introduce additional significant barriers less within reach of direct CHC services: economic/cost barriers, transportation barriers, or language barriers. It is also possible that the supply of endoscopists may differ in areas where Latino patients are served; however, in an analysis of Texas Medicare beneficiaries, increased colonoscopist density was associated with greater inequities in colonoscopy use among Latinos.36 It is unclear whether or how workforce factors may have affected these trends. In general, however, these results point to the equitable delivery of initial, “first contact” care but disparate care in the secondary evaluation and management of this common disease. Specifically, efforts aimed at reducing Latino CRC inequity may be best served by focusing on endoscopy availability, access, or utilization.
Limitations
This analysis was limited in the following ways. First, as mentioned previously, it was not possible to ascertain a denominator in which patients were definitively due for CRC screening; the denominator was informed by general age criteria over the study period. This primarily prevented the authors from assessing an overall screening prevalence, although this was not the primary goal of the study. The study period of 2012–2017 did not cover 10 years, which is the maximum interval for screening and may have misclassified patients as never screened. This misclassification could be unequal across these groups, resulting in bias, especially in the ever screened or stool testing screened outcomes. Second, although study patients come from one of the largest national networks of CHCs and included CHC data from 21 states, study findings may not generalize to the entire U.S. Latino population. However, OCHIN’s member CHCs share characteristics of the approximately 1,400 CHCs in the U.S., so study results have the potential to be generalizable to Latino’s seeking care at CHCs nationwide, and this is a crucial population in which to understand CRC screening. Patient–provider language concordance was not assessed (this data set does not have this information definitively), but CHCs are required to have interpreter/language resources for patients.31 Analyses specifically examining language concordance and specific ethnic subgroup (e.g., Mexican, Puerto Rican) would yield valuable insights. Screening tests were not differentiated from diagnostic tests (for lower gastrointestinal symptoms or anemia, for instance), although if patients received the latter this would suffice for being screened.
The screening of Black patients was not assessed; the focus here was on Latino patients because in national surveys, this group is most at risk for underutilizing CRC screening.6 Analyses focusing on Black patients’ receipt of the services described in this paper are needed as well. The study did not include patients aged >75 years because there are no universal screening recommendations in this age group. Also, the analysis did not evaluate if ordered/referred endoscopies were ever received, or whether or not there was sufficient local endoscopy capacity to handle a clinic’s potential volume. Future studies should evaluate the follow-up, communication, and documentation between CHCs and endoscopy centers. Lastly, though many important objective EHR-based confounders were incorporated into these analytic models, other important factors such as patient preference for CRC screening, family history of CRC or personal history of gastrointestinal conditions that elevate the risk of cancer, or full assessment of comorbidity were not accessible (though diabetes and heart disease were included).
CONCLUSIONS
In Latino populations, CRC is a common and deadly cancer. In a multi-state network of CHCs, Latino patients aged >50 years were more likely to receive stool-based screening tests for CRC than non-Hispanic Whites. However, Latinos were less likely to receive endoscopy referrals than non-Hispanic Whites, even when experiencing a positive stool-based screening test. Initiatives to improve Latino CRC outcomes should emphasize broad access to lower gastrointestinal endoscopy.
Supplementary Material
ACKNOWLEDGMENTS
Roopradha Datta, MPH made substantive contributions to the study.
Funders: National Institute on Aging, Grant number: R01AG056337. Oregon Health & Science University IRB number: STUDY00019022.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of these findings were presented as an Oral Presentation at the Annual Meeting of the North American Primary Care Research Group, November 2020. Virtual.
No financial disclosures and no conflict of interest were reported by the authors of this paper.
John Heintzman: Funding acquisition, Conceptualization, Writing Original Draft David Ezekiel-Herrera: Formal Analysis, Visualization, Writing - Review &Editing Ana R. Quiñones: Writing - Review &Editing Jennifer Lucas: Project Administration, Writing - Review & Editing Joseph Carroll: Writing - Review & Editing Sophia Gielbultowicz: Data Curation, Writing - Review & Editing Erika Cottrell, PhD: Writing - Review & Editing Miguel Marino: Funding Acquisition, Methodology, Formal Analysis, Writing - Review & Editing
REFERENCES
- 1.Centers for Disease Control and Prevention. Leading Causes of Death, Hispanic Females. https://www.cdc.gov/women/lcod/2017/hispanic/index.htm. Updated 2019. Accessed August 24, 2021.
- 2.American Cancer Society. Cancer Facts and Figures Hispanics/Latinos 2018–2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf. Published 2018. Accessed August 24, 2021.
- 3.Zhou J, Enewold L, Peoples GE, et al. Colorectal, prostate, and skin cancer screening among Hispanic and White non-Hispanic men, 2000–2005. J Natl Med Assoc. 2011;103(4):343–350. 10.1016/s0027-9684(15)30315-1. [DOI] [PubMed] [Google Scholar]
- 4.Zhou J, Enewold L, Peoples GE, et al. Trends in cancer screening among Hispanic and white non-Hispanic women, 2000–2005. J Womens Health (Larchmt). 2010;19(12):2167–2174. 10.1089/jwh.2009.1909. [DOI] [PubMed] [Google Scholar]
- 5.Martinsen RP, Morris CR, Pinheiro PS, Parikh-Patel A, Kizer KW. Colorectal cancer trends in California and the need for greater screening of Hispanic men. Am J Prev Med. 2016;51(6):e155–e163. 10.1016/j.amepre.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 6.Joseph DA, King JB, Dowling NF, Thomas CC, Richardson LC. Vital signs: colorectal cancer screening test use - United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69(10):253–259. 10.15585/mmwr.mm6910a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vargas Bustamante A, Chen J, Rodriguez HP, Rizzo JA, Ortega AN. Use of preventive care services among Latino subgroups. Am J Prev Med. 2010;38(6):610–619. 10.1016/j.amepre.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 8.Grzywacz V, Hussain N, Ragina N. Racial disparities and factors affecting Michigan colorectal cancer screening. J Racial Ethn Health Disparities. 2018;5(4):901–906. 10.1007/s40615-017-0438-x. [DOI] [PubMed] [Google Scholar]
- 9.Liss DT, Brown T, Lee JY, et al. Diagnostic colonoscopy following a positive fecal occult blood test in community health center patients. Cancer Causes Control. 2016;27(7):881–887. 10.1007/s10552-016-0763-0. [DOI] [PubMed] [Google Scholar]
- 10.Costas-Muñiz R, Jandorf L, Philip E, et al. Examining the impact of Latino nativity, migration, and acculturation factors on colonoscopy screening. J Community Health. 2016;41(5):903–909. 10.1007/s10900-016-0168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diaz JA, Roberts MB, Clarke JG, Simmons EM, Goldman RE, Rakowski W. Colorectal cancer screening: language is a greater barrier for Latino men than Latino women. J Immigr Minor Health. 2013;15(3):472–475. 10.1007/s10903-012-9667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez-Class M, Luta G, Noone AM, et al. Patient and provider factors associated with colorectal cancer screening in safety net clinics serving low-income, urban immigrant Latinos. J Health Care Poor Underserved. 2012;23(3):1011–1019. 10.1353/hpu.2012.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briant KJ, Sanchez JI, Ibarra G, et al. Using a culturally tailored intervention to increase colorectal cancer knowledge and screening among Hispanics in a rural community. Cancer Epidemiol Biomarkers Prev. 2018;27(11):1283–1288. 10.1158/1055-9965.epi-17-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mojica CM, Parra-Medina D, Vernon S. Interventions promoting colorectal cancer screening among Latino men: a systematic review. Prev Chronic Dis. 2018;15:E31. 10.5888/pcd15.170218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim B, Lairson DR, Chung TH, Kim J, Shokar NK. Budget impact analysis of against colorectal cancer in our neighborhoods (ACCION): a successful community-based colorectal cancer screening program for a medically underserved minority population. Value Health. 2017;20(6):809–818. 10.1016/j.jval.2016.11.025. [DOI] [PubMed] [Google Scholar]
- 16.Shokar NK, Byrd T, Salaiz R, et al. Against colorectal cancer in our neighborhoods (ACCION): a comprehensive community-wide colorectal cancer screening intervention for the uninsured in a predominantly Hispanic community. Prev Med. 2016;91:273–280. 10.1016/j.ypmed.2016.08.039. [DOI] [PubMed] [Google Scholar]
- 17.Sriphanlop P, Hennelly MO, Sperling D, Villagra C, Jandorf L. Increasing referral rate for screening colonoscopy through patient education and activation at a primary care clinic in New York City. Patient Educ Couns. 2016;99(8):1427–1431. 10.1016/j.pec.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 18.Greiner KA, Daley CM, Epp A, et al. Implementation intentions and colorectal screening: a randomized trial in safety-net clinics. Am J Prev Med. 2014;47(6):703–714. 10.1016/j.amepre.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inadomi JM, Vijan S, Janz NK, et al. Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch Intern Med. 2012;172(7):575–582. 10.1001/archinternmed.2012.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aragones A, Schwartz MD, Shah NR, Gany FM. A randomized controlled trial of a multilevel intervention to increase colorectal cancer screening among Latino immigrants in a primary care facility. J Gen Intern Med. 2010;25(6):564–567. 10.1007/s11606-010-1266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Association of Community Health Centers. Community Health Center Chartbook 2020. https://www.nachc.org/wp-content/uploads/2020/01/Chartbook-2020-Final.pdf. Published 2020. Accessed August 24, 2021.
- 22.The White House. The Obama Administration and Community Health Centers. https://obamawhitehouse.archives.gov/sites/default/files/05-01-12_community_health_center_report.pdf. Published 2012. Accessed February 10, 2021.
- 23.U.S. Preventive Services Task Force. Final recommendation: Colon Cancer Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening-june-2016. Published 2016. Accessed September 7, 2021.
- 24.The Advance Collaborative. A Short Guide to the ADVANCE Clinical Research Network (CRN). http://advancecollaborative.org/wp-content/uploads/2019/12/Short-Guide-to-the-ADVANCE-CRN-v2019-11-25.pdf. Published 2019. Accessed August 24, 2021.
- 25.DeVoe JE, Gold R, Cottrell E, et al. The ADVANCE network: accelerating data value across a national community health center network. J Am Med Inform Assoc. 2014;21(4):591–595. 10.1136/amiajnl-2014-002744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(23):2564–2575. 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 27.Rassen JA, Bartels DB, Schneeweiss S, Patrick AR, Murk W. Measuring prevalence and incidence of chronic conditions in claims and electronic health record databases. Clin Epidemiol. 2018;11:1–15. 10.2147/clep.s181242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hill E Understanding when to use the new patient E/M codes. Fam Pract Manag. 2003;10(8):33–36. [PubMed] [Google Scholar]
- 29.Bureau of Primary Health Care HRSA. Uniform Data System reporting Instructions for the 2018 Health Center Data. https://static1.squarespace.com/static/53023f77e4b0f0275ec6224a/t/5d005fa27167dd0001e13053/1560305575040/2018-uds-reporting-manual.pdf. Published 2018. Accessed March 1, 2021.
- 30.Diaz JA, Roberts MB, Goldman RE, Weitzen S, Eaton CB. Effect of language on colorectal cancer screening among Latinos and non-Latinos. Cancer Epidemiol Biomarkers Prev. 2008;17(8):2169–2173. 10.1158/1055-9965.epi-07-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Public health Services Act: 42 U.S. Code 254b - Health Centers. https://www.law.cornell.edu/uscode/text/42/254b. Accessed March 1, 2021.
- 32.López-Cevallos DF, Lee J, Donlan W. Fear of deportation is not associated with medical or dental care use among Mexican-origin farmworkers served by a federally-qualified health center--faith-based partnership: an exploratory study. J Immigr Minor Health. 2014;16(4):706–711. 10.1007/s10903-013-9845-1. [DOI] [PubMed] [Google Scholar]
- 33.Heintzman J, Bailey SR, Muench J, Killerby M, Cowburn S, Marino M. Lack of lipid screening disparities in obese Latino adults at health centers. Am J Prev Med. 2017;52(6):805–809. 10.1016/j.amepre.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heintzman J, Hatch B, Coronado G, et al. Role of race/ethnicity, language, and insurance in use of cervical cancer prevention services among low-income Hispanic women, 2009–2013. Prev Chronic Dis. 2018;15:E25. 10.5888/pcd15.170267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heintzman J, Bailey SR, Cowburn S, Dexter E, Carroll J, Marino M. Pneumococcal vaccination in low-income Latinos: an unexpected trend in Oregon community health centers. J Health Care Poor Underserved. 2016;27(4):1733–1744. 10.1353/hpu.2016.0159. [DOI] [PubMed] [Google Scholar]
- 36.Benarroch-Gampel J, Sheffield KM, Lin YL, Kuo YF, Goodwin JS, Riall TS. Colonoscopist and primary care physician supply and disparities in colorectal cancer screening. Health Serv Res. 2012;47(3 Pt 1):1137–1157. 10.1111/j.1475-6773.2011.01355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


