Abstract
Introduction:
Unstable intertrochanteric fracture poses challenges in terms of obtaining stable fixation and good post-operative outcomes. There is a paucity of clinical data comparing the commonly used proximal femoral nail (PFN) and PFN anti-rotation (PFNA) implants, especially in relation to osteoporosis. The purpose of this study is to assess the comparative performance of PFN and PFNA fixation in the treatment of unstable femur intertrochanteric fractures.
Materials and Methods:
This prospective observational study was conducted to understand and analyze the advantages of PFNA over PFN in the management of unstable intertrochanteric fractures from May 2021 to October 2023 at the Department of Orthopaedics, Chettinad Hospital and Research Institute, Kelambakkam. Patients presenting with an unstable intertrochanteric fracture with Singh’s Index grades 1, 2, and 3 were included. Boyd and Griffin classification types 2, 3, and 4 were included in the study. The patients were randomized into two types of implant groups. All patients were operated with a standard protocol. Patients were followed up for a minimum of 6 months and any complications were noted. A comparison of functional outcomes was done using the Modified Harris Hip Score. Statistical analysis was done using the unpaired t-test/Mann–Whitney U test and Chi-square test/Fisher’s exact test. A P < 0.05 was considered significant.
Results:
Every follow-up period included a Harris Hip Score assessment. At 3 months, the average score of PFN was 71.9 (range 66–81) and at 6 months it was 77.86 (range 72–90). For PFNA, at 3 months, the average score was 74.87 (range 66–81), and at 6 months, it was 89.3 (range 76–94). The improvement was seen well in the PFNA group which is statistically significant (P = 0.023). The most prevalent fracture was a type 2 fracture.
Conclusion:
The results showed PFNA has better rotation stability with single screws and better functional outcomes in treating unstable intertrochanteric fractures when compared to PFN.
Keywords: Proximal femoral nail, unstable trochanteric fracture, lateral trochanteric wall, communicated fragments
Learning Point of the Article:
To understand the pattern and epidemiology of unstable intertrochanteric femur fractures.
To evaluate the outcome both clinical and radiological following unstable intertrochanteric femur fractures treated using PFN and PFNA in patients with osteoporosis.
To assess the outcome using the Harris hip scoring system.
Introduction
Proximal femoral fractures are a major cause of morbidity and mortality the world over in view of the huge population, high road traffic accident rate, and increasing age of population [1]. Intertrochanteric fractures accounted for 26% of all hip fractures in Asia in 1990, but this number is expected to climb to 37% in 2025 and 45% in 2050 [2, 3]. The chances of morbidity and mortality are high when conservative treatment options are opted [4]. These fractures are now treated surgically to establish a stable fixation that enables patients to be mobilized sooner, avoiding the difficulties that come with extended immobility. Extra medullary and intramedullary implants may also be utilized to repair these fractures; however, intramedullary implants provide better biological fixing and are load-sharing devices. Extra medullary devices are always under stress due to bending strain, which is bad for fractures, but intramedullary devices are under axial strain which causes compression. They are 3–4 times more prevalent in osteoporotic women with the most common mechanism of injury being a minor fall [5]. The objective of surgical therapy for intertrochanteric fracture is to return to a pre-injury state as soon as feasible. Internal fixation of these fractures was used to improve patient comfort, enable nursing care, shorten hospitalization, and lessen the problems associated with extended recumbency [6]. The goal of this research is to compare the functional and radiological outcomes of proximal femoral nail (PFN) and PFN Anti-rotation (PFNA) fixation in the treatment of femur intertrochanteric fractures.
Materials and Methods
This prospective observational study was undertaken on patients who were operated on between May 2021 and October 2023 at the Department of Orthopaedics, Chettinad Hospital and Research Institute, Kelambakkam.
Inclusion criteria
Patients above 18 years of age with unstable intertrochanteric fractures
Boyd and Griffin classification types 2, 3, and 4
Patients who are medically fit and willing for surgery.
Exclusion criteria
Boyd and Griffin classification type 1
Fractures extending into diaphysis compound fractures
Patients with pathological fractures.
Methods
This is a prospective observational study that includes 50 patients with unstable Intertrochanteric fracture with Singh’s index criteria used for osteoporosis grading. The patient was randomized into two implant groups where 25 cases were fixed with PFN whereas 25 cases were fixed with PFNA. All the surgeries were done in a single center by the same team of surgeons. All patients in this study was admitted from the emergency room, with complaints of pain in the affected hip and other affected body part after trauma, either due to a fall or due to RTA. All the patients were evaluated completely and a routine investigation was done. Diagnosis was made based on clinical findings and radiological examination. X-ray pelvis with both hip anteroposterior view and lateral view of the affected hip was sufficient for diagnosis. (Fig. 1,2). Patients with suspected intertrochanteric fractures satisfying inclusion and exclusion criteria were included in our study. All the patients underwent pre-anesthetic checkups, once they were fit, they were operated on as early as possible, with either PFN or PFNA. Assessment of the reduction quality was done by a comparison of the neck-shaft angle of the operated side and the normal side on AP view of immediate post-operative radiographs. A variation of <5° from the normal side was considered a “good” reduction The post-operative radiological outcome was assessed and compared using parameters such as tip-apex distance, Cleveland index, neck-shaft angle, and type of reduction. (Table 1,2). Fracture union rates were compared at 6 weeks and 6 months. (Fig. 3 4). At each follow-up, radiological and clinical assessment was done by modified Harris Hip Score. Evaluation for intraoperative blood loss and surgery time (skin to skin) was done. All the patient’s post-operative follow-ups were done at 6 weeks 3 and 6 months. Functional assessment was done on every follow-up at 6 weeks and 3 months, and the final assessment at 6 months was done using the Modified Harris Hip Score.
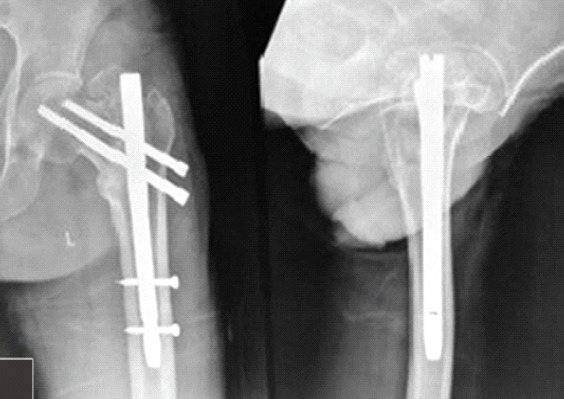
Figure 1.
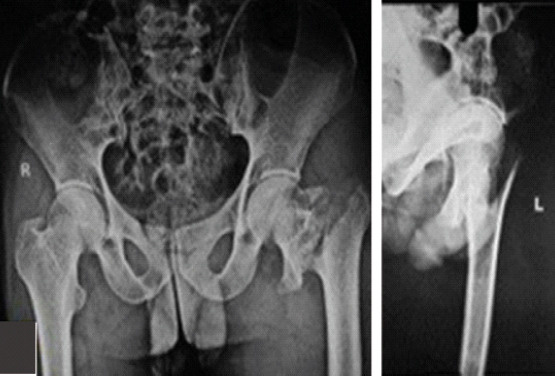
Initial pre-operative X-rays (proximal femoral nail).
Figure 2.
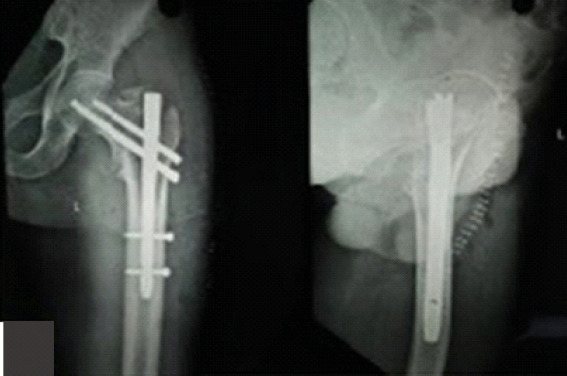
Immediate post-operative X-rays (proximal femoral nail).
Table 1.
Distribution of the study group according to modified Harris hip score.
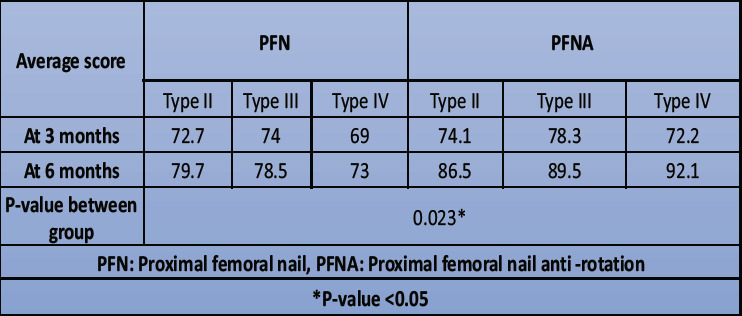
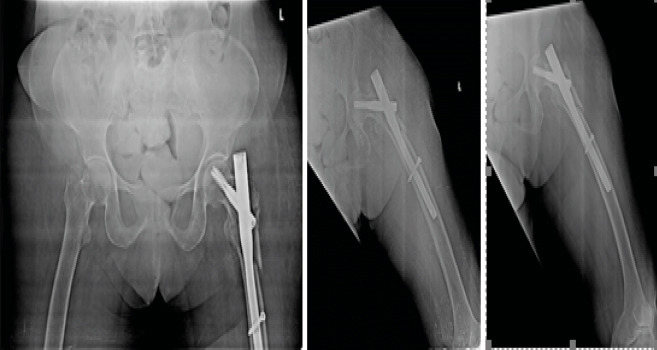
Figure 3.
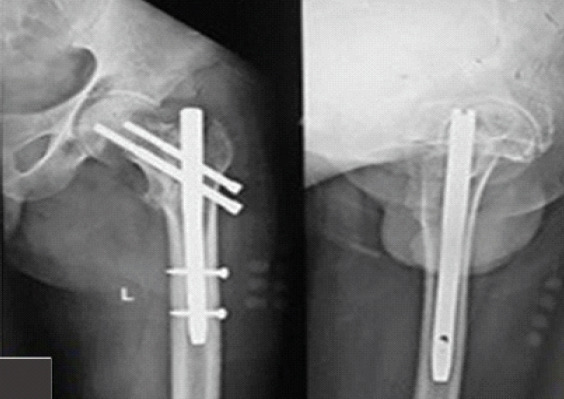
3 months follow-up X-rays (proximal femoral nail).
Figure 4.
6 months follow-up X-rays (proximal femoral nail).
Results
In this study of 50 patients with unstable intertrochanteric fractures, 25 patients were treated with PFNA and 25 patients with PFN. The following outcomes were observed from the result. According to our findings, most of them are in the age group of 40–49 years. Our PFN fixation patients had an average mean age distribution of 47.21, whereas our PFNA patients had a mean age distribution of 49.1, which was not statistically significant regarding gender distribution. In our study, the PFN group had 18 men and seven women whereas the PFNA group had 16 men and nine women. The right hip is involved predominantly in both groups. Most of the patients in both groups were injured due to trivial falls. In our study, we observed RTA at 48% and accident fall at 52% among the study group. We observed that nearly 60% of patients in the PFN group and 72% of patients in the PFNA group had Type II Boyd and Griffin fracture, whereas 32% of patients in the PFN group and 16% of patients in the PFNA group had type III fracture, and 8% of patients in the PFN group and 12% of patients in the PFNA group had type IV fracture. Among 50 cases, the maximum operating time falls between 61–75 min for both PFN and PFNA cases. Every follow-up period included a Harris Hip Score assessment. (Fig. 6). At 3 months the average score of PFN was 71.9 (range 66–81) and at 6 months it was 77.86 (range 72–90). For PFNA, at 3 months the average score was 74.87 (range 66–81), (Fig. 7)and at 6 months, it was 89.3 (range 76–94). (Fig. 8) The improvement was seen better in the PFNA group which is statistically significant (P = 0.023) (Table-1,2).
Figure 6.
Immediate post-operative X-rays (proximal femoral nail anti-rotation).
Figure 7.
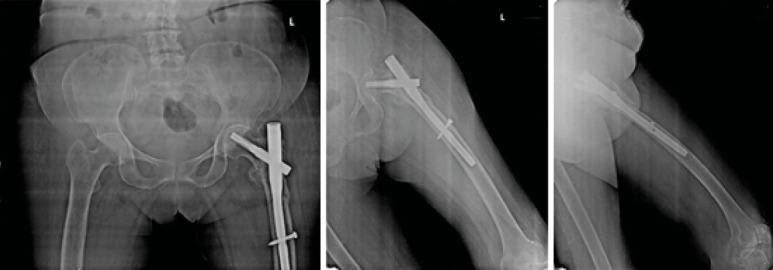
3 Months follow-up X-rays (proximal femoral nail anti-rotation).
Figure 8.
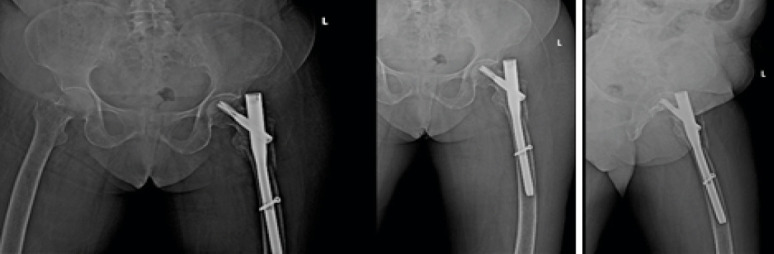
6 Months follow-up X-rays (proximal femoral nail anti-rotation).
Table 2.
Distribution of the study group according to comparison of the Cleveland index.
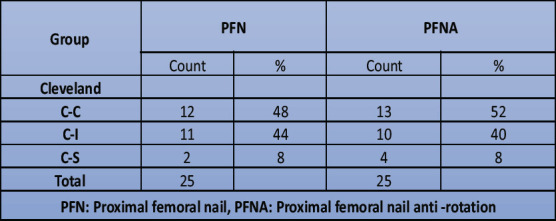
Figure 5.

Initial pre-operative X-rays (proximal femoral nail anti-rotation).
Discussion
The therapy of unstable intertrochanteric fractures is complicated by osteoporosis’ impact on the prognosis [7]. Osteoporosis predicts screw migration in the proximal femur, leading to implant failure [8]. Clinical studies have also revealed a link between osteoporosis and poor intertrochanteric fracture outcomes [9]. Today’s nail designs reflect the continued search for the best implant for these osteoporotic fractures. A helical blade device improved fixation in these fractures. The helical blade was created for its biomechanical effectiveness in osteoporosis [10]. The blade may be inserted without reaming, protecting the femoral head bone stock. With greater purchase and resistance to varus collapse and rotational stress [11]. It compacts the cancellous bone surrounding it compared to normal PFN, this caused reduced clinical difficulties in an osteoporotic patient group. Because of the anticipated benefit of enhanced purchase in osteoporotic bone, the use of PFNA in older patients was commonly advocated in the current study. Our data show PFNA has a statistically significant difference in functional outcomes as determined by the Harris Hip Score between the two implants. The average age of our 50 patients with unstable intertrochanteric fractures was 47 years. This contrasts with the older age groups suggested by Western literature. Our findings agree with those of Gupta et al. [9], Mohanty and Chacko [12]. Because Indians have a 10-year lower life expectancy than Westerners, and hunger and osteoporosis go hand in hand, the majority of instances occurred among the elderly. The reason why the intertrochanteric area is the most prevalent location of fracture is most likely related to tensile osteoporosis as we age. As a main joint in the weight-bearing system, the hip joint, which is already compromised, cannot sustain any unexpected aberrant force. The area between bone trabeculae enlarges and fills with fat, while dense tissue thins and calcar atrophies [13]. In the current study, the male-to-female ratio was 18:7 for PFN and 16:9 for PFNA. In our study, males were harmed more since their exposure to trauma throughout their daily lives was larger. Our study shows that 11 PFN and 13 PFNA patients were injured in a traffic incident, according to Horn and Warg. The mechanism of damage is not direct, but rather than the failure of stress-resistant forces during abrupt bending or twisting [14]. The average time between the injury and the operation was 9.6 days. The average operation time was calculated to be 67.7 min. The most prevalent kind of fracture was a type 2 fracture. Our findings are consistent with earlier studies that compared these implant types. Shah et al. compared the PFNA (helical blade) to the PFN and discovered that the PFNA had a lower cut-out rate [15]. Choo et al. reported that the PFNA had less post-operative sliding than the PFN, and discovered that helical blade nails significantly enhanced social function, mobility, and complication rates. In our study, discovered that the probability of a late complication and re-surgery is significantly higher with a PFN than with a helical blade device.
Conclusion
PFNA shows superiority over PFN as it has a lesser procedure time, less blood loss, and less complication rate and has a better outcome among intertrochanteric fracture patients with osteoporosis. PFNA2 seemed better, as it required less radiation exposure. PFNA2 System with the unique spiral blade has comparable rotational stability then PFN. This is achieved by compaction of the cancellous bone around the surface of the PFNA blade and results in an excellent fit between the blade and (generally osteoporotic) bone The age of the patient is an important factor in predicting functional outcome. The proper operative technique to maintain. the neck-shaft angle difference of fewer than 5° and to achieve fracture stability and avoid major complications In PFNA, an Innovative helical blade design provides better hold on both compact and cancellous bone and femoral head to improve stability and less incidence of screw cutout in case of unstable intertrochanteric fractures. PFNA-2 is a dependable implant for the fixation of unstable osteoporotic intertrochanteric fractures in the elderly. This also led to faster recovery and rehabilitation.
Clinical Message.
These intertrochanteric fractures are now treated surgically to provide a secure fixation, allowing patients to be mobilized sooner and avoiding the complications associated with prolonged immobility. This study is unusual in that it demonstrates the importance of adequate radiological characteristics in reducing the frequency of problems. It emphasizes the critical necessity of the neck-shaft angle, kind of reduction, and position of the compression screw/helical blade after surgery. It also shows a greater union rate among individuals with osteoporosis who have had PFNA surgery. This can aid surgeons in making decisions for osteoporotic patients. This study covered all forms of intertrochanteric fracture patients, which was not observed in earlier investigations. The number of patients involved is sufficient to offer a better insight into the merits and demerits of both types of implants.
Biography





Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Babhulkar S. Proximal femur fractures. Indian J Orthop. 2013;47:322. [Google Scholar]
- 2.Jonnes C, Sm S, Najimudeen S. Type II intertrochanteric fractures:Proximal femoral nailing (PFN) versus dynamic hip screw (DHS) Arch Bone Jt Surg. 2016;4:23–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Melton LJ 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20:687–94. doi: 10.1007/s00198-008-0742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jewett EL. One piece angle nail for trochanteric fractures. J Bone Joint Surg. 1941;23:803–10. [Google Scholar]
- 5.Kaufer H. Mechanics of the treatment of Hip injuries. Clin Orthop. 1980;146:53–61. [PubMed] [Google Scholar]
- 6.Broderick JM, Bruce-Brand R, Stanley E, Mulhall KJ. Prospective randomized comparative study. Osteoporotic hip fractures:The burden of fixation failure. Scientific World J. 2013;2013:515197. doi: 10.1155/2013/515197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheema G, Rastogi A, Singh V, Goel S. Comparison of cutout resistance of dynamic condylar screw and proximal femoral nail in reverse oblique trochanteric fractures:A biomechanical study. Indian J Orthop. 2012;46:259–6. doi: 10.4103/0019-5413.96369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akan K, Cift H, Ozkan K, Eceviz E, Tasyikan L, Eren A. Effect of osteoporosis on clinical outcomes in intertrochanteric hip fractures treated with a proximal femoral nail. J Int Med Res. 2011;39:857–65. doi: 10.1177/147323001103900319. [DOI] [PubMed] [Google Scholar]
- 9.Gupta RK, Gupta V, Gupta N. Outcomes of osteoporotic trochanteric fractures treated with cement-augmented dynamic hip screw. Indian J Orthop. 2012;46:640–5. doi: 10.4103/0019-5413.104193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gavaskar A, Subramanian M, Tummala N. Results of proximal femoral nail antirotation for low velocity trochanteric fractures in the elderly. Indian J Orthop. 2012;46:556. doi: 10.4103/0019-5413.101036. 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta RK, Sangwan K, Kamboj P, Punia SS, Walecha P. Unstable trochanteric fractures:The role of lateral wall reconstruction. Int Orthop. 2010;34:125–9. doi: 10.1007/s00264-009-0744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohanty SP, Chacko V. A comparative analysis of operative and non-operative management of trochanteric fractures. A study of 135 consecutive cases. Indian J Orthop. 1984;18:19–24. [Google Scholar]
- 13.Malhotra N, Mithal A. Osteoporosis in Indians. Indian J Med Res. 2008;127:263–8. [PubMed] [Google Scholar]
- 14.Horn JS, Wang YC. Mechanics of trochanteric anatomy of trochanteric fractures. Br Jr Surg. 1964;51:574. [Google Scholar]
- 15.Shah MR, Shah MM, Shah IM, Shah KR. Surgical and functional outcomes of the results of conventional two-screw proximal femoral nail (PFN) versus helical-blade anti-rotation proximal femoral nail (PFNA2) Cureus. 2023;15:e43698. doi: 10.7759/cureus.43698. [DOI] [PMC free article] [PubMed] [Google Scholar]


