Abstract
Introduction
Prior to the coronavirus disease-2019 (COVID-19) pandemic the U.S. Department of Veterans Affairs (VA) had the largest telehealth program in the United States. The pandemic motivated providers within the VA to expand telehealth in effort to reduce disrupted care while mitigating risks. The pandemic provides a rare opportunity to examine how to better engage veterans experiencing housing instability (HI) in telehealth diabetes care.
Methods
Mixed methods design to examine VA video connect (VVC) diabetes care utilization among veterans experiencing HI from March 1, 2019, to March 1, 2022, combining multivariable regression analyses of VA administrative data with semi-structured interviews. Study aims included: (a) examine changes in diabetes care delivery mode over the peri-pandemic timeframe; (b) identify sociodemographic and clinical characteristics associated with VVC care among veterans with HI; and (c) understand the facilitators and barriers of VVC utilization.
Results
Totally, 5904 veterans were eligible for study analysis. Veterans who are female (OR: 1.63; 95% CI: 1.3, 2.0; p < 0.0001), self-identify as Hispanic (OR: 1.44; 95% CI: 1.1, 1.9; p = 0.02), are married (OR: 1.39; 95% CI: 1.2, 1.6; p < 0.0001), and are in VA priority group 1 (OR: 1.21; 95% CI 1.1, 1.4; p = 0.004) were more likely to use VVC the pandemic. Veterans of older age (OR: 0.97; 95% CI: 0.97, 0.98; p < .0001) and rural dwelling (OR: 0.85; 95% CI: 0.7, 1.2; p = 0.04), were less likely to use VVC. Thirteen VA providers and 15 veterans were interviewed. Veterans reported that decisions about using VVC were driven by limitations in in-person care availability, safety, and convenience.
Discussion
Telehealth played an important role in providing veterans with HI access to diabetes care during the pandemic. Future interventions should seek to increase education and technology in effort to increase VVC uptake into routine diabetes care to ensure veterans’ optimal and equitable access.
Keywords: Video telehealth, diabetes, homelessness, veterans, COVID-19
Introduction
The U.S. Department of Veterans Affairs (VA) has the largest telehealth program in the United States, with over 900,000 veterans receiving 2 million remote care episodes. 1 Prior to 2019, telehealth was available in over 50 VA specialty care areas 2 (Appendix A), although the majority of remote utilization was for mental health and primary care.3,4 veterans experiencing housing instability (HI) may benefit from telehealth encounters, particularly during times of crisis. 5 Yet there is a paucity of research examining diabetes care telehealth utilization among veterans experiencing housing instability. The coronavirus disease-2019 (COVID-19) pandemic motivated VA providers (i.e. medical doctors, nurse practitioners, case managers, etc.) to expand telehealth rapidly to reduce disrupted care while mitigating COVID-19 risks.6,7 During March and April 2020, weekly VA Video Connect (VVC) encounters rose from 1102 to 13,068 in primary care; 1238 to 21,215 in specialty care. 8 The pandemic presented a natural experiment in how veterans experiencing HI and their providers responded to a change in diabetes care modality, providing a rare opportunity to examine how the VA can better engage a population with social/economic challenges.
Among veterans experiencing HI, the pandemic exacerbated disparities and potentiated examining barriers to diabetes care. 9 In the United States, the pandemic revealed wide disparities in infection and recovery rates by place of dwelling, race, ethnicity, socioeconomic status, and comorbidities. 10 For veterans with diabetes experiencing HI, the impact of COVID-19 was two-fold: first, veterans were at increased risk for severe coronavirus infection and its complications;11,12 and second, diabetes management was disrupted by reduced access to health care, food security, shelter, and transportation. 13 While confinement measures may reduce infection, isolation interferes with comprehensive diabetes care which requires regular patient–provider interactions. 12 To address this problem among veterans, clinicians turned to telehealth. Yet, technology barriers and internet unaffordability may have furthered a “digital divide”—disparate access to telehealth for veterans with HI. 8
We examined the extent to which VVC can be leveraged to mitigate diabetes care disruptions among veterans with HI during the pandemic. Our aims were to: (a) examine changes in diabetes care delivery mode over the peri-pandemic timeframe; (b) identify sociodemographic and clinical characteristics associated with VVC care among veterans with HI; and (c) understand the facilitators and barriers of VVC utilization. Identify the characteristics associated with VVC diabetes care utilization among veterans with HI and VA providers to inform interventions which seek to increase uptake.
Methods
We used a mixed-methods design to examine VVC diabetes care utilization among veterans experiencing HI between March 1, 2019, through March 1, 2022. Given the Quality Improvement nature of this National Center on Homelessness for Veterans (NCHAV) project, it was deemed exempt from research oversight by VA Central Western Massachusetts ethical review board. This determination included approval to verbally consent participants in the qualitative aim of this study.
Quantitative aim (aims 1 and 2)
To examine changes in diabetes care delivery mode over the peri-pandemic timeframe and to identify the veteran characteristics associated with VVC care. Veterans were identified by diagnostic and stop codes commonly used for housing instability in the VA's electronic medical record. 14 Stop codes, also referred to as decision support system (DSS) Identifiers, is a VHA term that characterizes VHA Outpatient Clinics by a six-character descriptor that is transmitted to the National Patient Care Database (NPCD) with each separate outpatient encounter. We examined access to telehealth (video and phone) and in-person care among veterans using the Corporate Data Warehouse (CDW), a national repository of clinical, administrative, and financial data from VA medical facilities including detailed information on each clinical visit. 15
Participant eligibility
Eligible Veterans Integrated Services Network (VISN) 1 Veterans included those (a) experiencing homelessness (Stop codes housing instability: 37, 504, 507, 508, 511, 522. 528–530, 555, 556, etc.); (b) with a diabetes diagnosis (ICD-10 codes E11.XX, Z59.XX); (c) who accessed care from a VA between March 1, 2019, and March 1, 2022, in at least one of the healthcare fields of interest (endocrinology, pharmacy, primary care, optometry, other diabetes care specialty, podiatry, MOVE!) utilizing any of the three modalities; and (d) have an electronic health record (EHR) record in the CDW. Veterans were excluded if they did not access VA care between March 1, 2019, and March 1, 2022, or had missing data on the outcome measures described below. Given the data was analyzed retrospectively in aggregate, inform consent was not obtained.
Quantitative analysis
The outcome of outpatient care encounters was classified into type and modality using VA stop codes. Encounters were classified into mutually exclusive categories based on primary, endocrinology, and specialty care services for three years: pre-pandemic year (3/1/2019–2/29/2020), pandemic year 1, PY1 (3/1/2020–2/28/2021), and pandemic year 2, PY2 (3/1/2021–2/28/2022). Visit modality was categorized as in-person, VVC, and phone utilization to form exclusive categories. Bivariate comparisons using Pearson's chi-square compared veterans’ characteristics by care modality. Of interest were veteran sociodemographics (e.g. age, sex, race/ethnicity, marital status, residential location) and clinical characteristics (e.g. previous outpatient encounters, condition severity, VA priority, and Elixhauser comorbidities). 16 VA priority is a rating from 1 to 6 based on service-connected disability, income, military service. 17 VA priority 1 represents the most economically disadvantaged Veterans versus those in priority groups 2–6. Multivariable logistic regressions were conducted to model associations between the veteran characteristics and the primary outcome, VVC utilization. Adjusted odds ratios or incident rate ratios and 95% confidence intervals (CIs) for each characteristic were reported. All analyses were conducted in SAS Enterprise Guide version 8.3 (SAS Institute, Cary, NC).
Qualitative aim (aim 3)
We conducted semi-structured interviews with both diabetes care providers and veterans to better understand their perceptions of VVC encounters.
Participant eligibility
Providers
For the purposes of this study, participants included VISN 1 VA providers in primary care, endocrinology, podiatry, optometry, pharmacy, and case management. Working with VA medical chiefs and the VA's Deputy Network Homeless Coordinator, we purposively selected providers and case managers throughout the VISN to ensure diverse care delivery settings. Providers and case managers were emailed an invitation to participate in a one-time phone interview, along with a study information sheet. Once individuals consented to participate, we scheduled the 30-minute interview in Microsoft Teams. At the beginning of each interview, a research coordinator reviewed the study with each participant and audio recorded the consent process before starting the interview. We conducted interviews with thirteen VA providers, the point which thematic saturation was reached. 18
Veterans
Participants were VISN 1 veterans experiencing diabetes and homelessness who were offered telehealth encounters within the study timeframe. We purposively selected a diverse group of 15–20 Veterans from our Aim 1 cohort representing different telehealth experiences (users and non-users) and sociodemographics (i.e. age, race, gender). Eligible participants were mailed a study invitation and information sheet. Once a veteran expressed an interest in participating, the individual was contacted by the study coordinator who reviewed the study information sheet, consented the participant, and scheduled the Microsoft Teams interview. Like the provider participants, a research coordinator reviewed the study with each veteran and audio recorded the consent process before starting the interview. After interviewing 15 veterans, we had reached saturation and ceased recruiting more participants.
Qualitative analysis
Interviews queried providers and veterans on their perceptions of the barriers and facilitators to VVC utilization during the pandemic. Using past methods employed by our team, both interview guides were piloted among our expert panel, and revised as needed prior to implementation. Digitally recorded interviews were 90 minutes in length, professionally transcribed, and then analyzed in Atlas.ti. 19 A priori codes were based on the interview guide questions and COVID-19 care disruption literature. Taking into consideration these themes, one PhD-level investigator (R.K.) employed open coding of the responses, creating code definitions and schemes as concepts emerged inductively from the data.20,21 This approach helped to identify relationships generated through the responses and from theories based on them. Codes with similar meanings were merged and organized into a broader category that covered the meanings. Applying content analysis, the investigator and lead research coordinator (R.K.; L.W.), through an iterative process, independently coded each of the responses and conferred to achieve consensus pertaining to the underlying themes. 22 Additional team members (D.K.M. (PhD researcher); A.A. (endocrinologist)) were consulted when discrepancies arose. 23 Collectively, the team systematically and rigorously analyzed the data to reflect the views of all participants and validate salient findings.
Results
Quantitative analysis
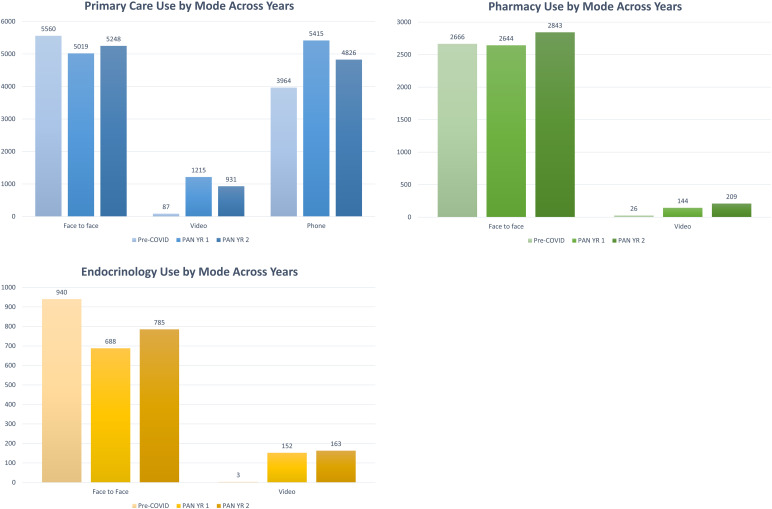
Eligible for this analysis were 5904 VISN 1 veterans who were experiencing diabetes and HI during the timeframe of interest and had any relevant visit data, which specified type of care as well as modality, for all three years of the study. Given that all these 5904 had complete data, no one was excluded from the analysis. Approximately, 62,673 clinical encounters were made by 5904 veterans during the study period. Of these encounters, 6267 (13%) visits were exclusively telehealth (VVC or phone); 23,897 (38%) visits were both telehealth and in-person modality; and 30,482 (49%) were only in-person visits. Figure 1 shows that across specialties, the telehealth-only demonstrated increase in the raw count for PY1, followed by a decrease in PY2 as care returned to in-person visits.
Figure 1.
Clinical care modality by specialty among veterans with diabetes and experiencing housing instability across both pandemic years.
There were 1503 (26%) veterans experiencing HI who had at least one VVC diabetes care encounter during PY1. Bivariate comparisons found veteran characteristics associated with VVC utilization included, younger age (60.5 years; SD: 11.2; p < 0.001), male (89% vs. 11%, female; p < 0.0001), self-identified non-Hispanic White (67% vs 6%, self-identified Hispanic, any race; p < 0.0001), and non-married (67% vs. 33%, married; p < 0.0001) Table 1). Residing in an urban area was also associated with VVC utilization (78% vs. 22%, rural; p = 0.005). Veterans assigned to VA priority groups 2–6 (51% vs. 49%, Priority 1; p < 0.0001) and who had higher comorbidities (88% ≥ 3 vs. 12% 2 or fewer; p = 0.0006) were more likely to utilize VVC.
Table 1.
Demographics for overall sample, any VVC and/or phone telehealth use among diabetic veterans experiencing housing instability across both pandemic years.
| Characteristic | Full sample N = 5904 |
VVC use, PY1 N = 1503 |
p-Value | Phone use, PY1 N = 5744 |
p-Value | VVC use, PY2 N = 1289 |
p-Value | Phone use, PY2 N = 5468 |
p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Age (Mean [SD], range) | 63.33 (11.18), 21.00–100.00 |
60.54 (11.18), 23.0–100.0 |
<0.0001 |
63.36 (11.11), 21.0–100.0 | 0.28 | 59.97 (11.38), 23.0–92.0 |
<0.0001 | 63.17 (11.04), 21.0–100.0 | 0.0007 |
| Sex | |||||||||
| Male | 5483 (92.9) | 1334 (88.8) | <0.0001 | 5332 (92.8) | 0.45 | 1136 (88.1) | <0.0001 | 5069 (92.7) | 0.08 |
| Female | 421 (7.1) | 169 (11.2) | 412 (7.2) | 153 (11.9) | 399 (7.3) | ||||
| Race/ethnicity a | |||||||||
| Missing | 194 (3.3) | 52 (3.5) | <0.0001 | 179 (3.1) | 0.29 | 31 (2.4) | 0.04 | 170 (3.1) | 0.03 |
| White, non-Hispanic | 4176 (70.7) | 1010 (67.2) | 4060 (70.7) | 886 (68.7) | 3849 (70.4) | ||||
| Black, non-Hispanic | 1171 (19.8) | 324 (21.6) | 1149 (20.0) | 285 (22.1) | 1108 (20.3) | ||||
| Hispanic, any race | 236 (4.0) | 87 (5.8) | 232 (4.0) | 62 (4.8) | 223 (4.1) | ||||
| Other, Non-Hispanic | 127 (2.2) | 30 (2.0) | 124 (2.2) | 25 (1.9) | 118 (2.2) | ||||
| Marital status | |||||||||
| Missing | 28 (0.5) | 9 (0.6) | <0.0001 | 28 (0.5) | 0.17 | 5 (0.4) | <0.0001 | 24 (0.4) | 0.27 |
| Married | 1699 (28.8) | 491 (32.7) | 1645 (28.6) | 428 (33.2) | 1564 (28.6) | ||||
| Single/divorced/widow(ed) | 4177 (70.8) | 1003 (66.7) | 4071 (70.9) | 856 (66.4) | 3880 (71.0) | ||||
| VA priority | |||||||||
| Group 1 | 2396 (40.6) | 735 (48.9) | <0.0001 | 2342 (40.8) | 0.07 | 659 (51.1) | <0.0001 | 2262 (41.4) | <0.0001 |
| Groups 2, 3, 4, 5, 6 | 3508 (59.4) | 768 (51.1) | 3402 (59.2) | 630 (48.9) | 3206 (58.6) | ||||
| Last residence | |||||||||
| Missing | 27 (0.5) | 5 (0.3) | 0.005 | 25 (0.4) | 0.91 | 4 (0.3) | 0.02 | 27 (0.5) | 0.0005 |
| Urban | 4448 (75.3) | 1174 (78.1) | 4329 (75.4) | 1005 (78.0) | 4148 (75.9) | ||||
| Rural | 1429 (24.2) | 324 (21.6) | 1390 (24.2) | 280 (21.7) | 1293 (23.7) | ||||
| Elixhauser group | |||||||||
| ≤2 | 880 (14.9) | 183 (12.2) | 0.0006 | 817 (14.2) | <0.0001 | 155 (12.0) | 0.001 | 776 (14.2) | <0.0001 |
| ≥3 | 5024 (85.1) | 1320 (87.8) | 4927 (85.8) | 1134 (88.0) | 4692 (85.8) | ||||
| Prior utilization, Pre-COVID | |||||||||
| Primary care | |||||||||
| Face to face | 5560 (94.2) | 1460 (97.1) | <0.0001 | 5436 (94.6) | <0.0001 | 1239 (96.1) | 0.0007 | 5176 (94.7) | <0.0001 |
| Video | 87 (1.5) | 49 (3.3) | <0.0001 | 86 (1.5) | 0.73 | 42 (3.3) | <0.0001 | 87 (1.6) | 0.008 |
| Phone | 3964 (67.1) | 1106 (73.6) | <0.0001 | 3911 (68.1) | <0.0001 | 944 (73.2) | <0.0001 | 3742 (68.4) | <0.0001 |
| Endocrinology | |||||||||
| Face to face | 940 (15.9) | 342 (22.8) | <0.0001 | 927 (16.1) | 0.006 | 283 (22.0) | <0.0001 | 906 (16.6) | <0.0001 |
| Video | 3 (0.1) | 3 (0.2) | — | 3 (0.1) | — | 1 (0.1) | — | 3 (0.1) | — |
| Phone | — | — | — | — | — | — | — | — | — |
| Pharmacy | |||||||||
| Face to face | 2666 (45.2) | 782 (52.0) | <0.0001 | 2634 (45.9) | <0.0001 | 687 (53.3) | <0.0001 | 2526 (46.2) | <0.0001 |
| Video | 26 (0.4) | 16 (1.1) | <0.0001 | 26 (0.5) | — | 15 (1.2) | <0.0001 | 26 (0.5) | — |
| Phone | — | — | — | — | — | — | — | — | — |
Self-identified veteran race/ethnicity.
Characteristics of VVC utilization remained constant in PY2, the only difference being veterans in priority group 1 (51%) utilized telehealth slightly more than those in priority groups 2–6 (49%: p < 0.0001).
Table 2 shows hierarchical multivariable analyses of the predisposing, enabling, and need characteristics associated with telehealth utilization in PY1. VVC utilization was more likely for those who were female (OR: 1.63; 95% CI: 1.3, 2.0; p < 0.0001), self-identified Hispanic (OR: 1.44; 95% CI: 1.1, 1.9; p = 0.02), or married (OR: 1.39; 95% CI: 1.2, 1.6; p < 0.0001). Veterans who were in VA priority group 1 (OR: 1.21; 95% CI 1.1, 1.4; p = 0.004) were more likely to use VVC, as were those seeing a provider in the year prior to the pandemic. Veterans who were older (OR: 0.97; 95% CI 0.97, 0.98; p < 0.0001), or residing in rural areas had reduced odds of VVC (OR: 0.85; 95% CI 0.7, 1.0; p = 0.04).
Table 2.
Demographics and clinic variables associated with VVC and phone telehealth utilization among diabetic veterans experiencing housing instability in pandemic year 1.
| Characteristic | VVC use, PY1 N = 1437 Odds ratio (95% CI) |
p-Value | Phone use, PY1 N = 5517 Odds ratio (95% CI) |
p-Value |
|---|---|---|---|---|
| Age | 0.97 (0.97–0.98) | <0.0001 | 1.01 (0.99–1.02) | 0.31 |
| Race/ethnicity a | ||||
| Non-Hispanic, White | Ref. | Ref. | ||
| Non-Hispanic Black | 1.01 (0.86–1.19) | 0.89 | 1.58 (0.97–2.59) | 0.07 |
| Non-Hispanic Other | 0.92 (0.59–1.42) | 0.69 | 1.59 (0.49–5.17) | 0.45 |
| Hispanic, any race | 1.44 (1.07–1.93) | 0.02 | 1.79 (0.64–5.05) | 0.27 |
| Sex | ||||
| Male | Ref. | Ref. | ||
| Female | 1.63 (1.31–2.04) | <0.0001 | 1.22 (0.58–2.57) | 0.60 |
| Marital status | ||||
| Single/Divorced/Widow(ed) | Ref. | Ref. | ||
| Married | 1.39 (1.21–1.59) | <0.0001 | 0.68 (0.47–0.97) | 0.03 |
| Last residence | ||||
| Urban | Ref. | Ref. | ||
| Rural | 0.85 (0.73–1.00) | 0.04 | 1.07 (0.72–1.60) | 0.74 |
| Elixhauser group (Pre-COVID) | ||||
| Less than or equal to 2 | Ref. | Ref. | ||
| 3 or more | 0.97 (0.79–1.19) | 0.78 | 1.67 (1.23–2.47) | 0.01 |
| VA priority | ||||
| Group 1 | 1.21 (1.06–1.38) | 0.004 | 1.10 (0.76–1.60) | 0.60 |
| Groups 2, 3, 4, 5, 6 | Ref. | Ref. | ||
| Prior utilization, pre-COVID | ||||
| Primary care | ||||
| Face to face | 2.10 (1.47–3.00) | <0.0001 | 2.03 (1.27–3.26) | 0.003 |
| Video | 1.98 (1.23–3.19) | 0.005 | — | |
| Phone | 1.21 (1.05–1.40) | 0.01 | 2.35 (1.61–3.44) | <.0001 |
| Endocrinology face to face | 1.56 (1.33–1.83) | <0.0001 | — | |
| Pharmacy | ||||
| Face to face | — | 1.89 (1.21–2.96) | 0.005 | |
| Video | 3.24 (1.39–7.55) | 0.006 | — | |
| Mental health visit | 1.21 (1.03–1.43) | 0.02 | — | |
| Pulmonary clinic visit | 1.27 (1.09–1.49) | 0.003 | — | |
| Cardiology clinic visit | 1.24 (1.07–1.43) | 0.004 | 3.12 (1.61–6.07) | 0.0008 |
| Pain clinic visit | 1.35 (1.16–1.58) | 0.0001 | 5.79 (1.82–18.43) | 0.003 |
| Telehealth visit | 1.41 (1.21–1.65) | <0.0001 | — |
Self-identified veteran race/ethnicity.
In PY2, the count indicates a slight decrease in telehealth utilization (Table 3). Predisposing characteristics of utilizing VVC included being female (OR: 1.59; 95% CI 1.2, 2.1; p = 0.0006) and married (OR: 1.28; 95% CI 1.1, 1.5; p = 0.003). Veterans who were more likely to use VVC had needs characteristics which included 3 or more Elixhauser comorbidities (OR: 1.64; 95% CI 1.3, 2.1; p = 0.07), VA priority group 1 (OR: 1.28; 95% CI 1.1, 1.5; p = 0.002), and having a VVC encounter in PY1 (OR: 1.86; 95% CI 1.5, 2.3; p < 0.0001), specifically, a Pharmacy VVC encounter (OR: 6.24; 95% CI 4.1, 9.5; p < 0.0001). Veterans residing in a rural location had reduced odds of video telehealth in PY2. There were no significant differences in VVC utilization across race and ethnicity in PY2.
Table 3.
Demographics and clinic variables associated with VVC and phone telehealth utilization among diabetic veterans experiencing housing instability in pandemic year 2.
| VVC use, PY2 N = 1075 |
Phone use, PY2 N = 5246 |
|||
|---|---|---|---|---|
| Characteristic | Odds ratio (95% CI) | p-Value | Odds ratio (95% CI) | p-Value |
| Age | 0.97 (0.96–0.98) | <0.0001 | 0.99 (0.98–0.99) | 0.02 |
| Race/ethnicity a | ||||
| Non-Hispanic White | Ref. | Ref. | ||
| Non-Hispanic Black | 1.01 (0.84–1.23) | 0.35 | 1.32 (0.97–1.78) | 0.07 |
| Non-Hispanic Other | 0.96 (0.58–1.60) | 0.84 | 1.23 (0.58–2.60) | 0.59 |
| Hispanic, any race | 0.75 (0.51–1.09) | 0.17 | 1.37 (0.72–2.61) | 0.33 |
| Sex | ||||
| Male | Ref. | Ref. | ||
| Female | 1.59 (1.22–2.08) | 0.0006 | 1.13 (0.71–1.79) | 0.62 |
| Marital status | ||||
| Single/divorced/widow(ed) | Ref. | Ref. | ||
| Married | 1.28 (1.09–1.52) | 0.003 | 0.96 (0.76–1.22) | 0.75 |
| Last residence | ||||
| Urban | Ref. | Ref. | ||
| Rural | 0.89 (0.74–1.08) | 0.23 | 0.76 (0.60–0.97) | 0.03 |
| Elixhauser group, Pre-COVID | ||||
| Less than or equal to 2 | Ref. | Ref. | ||
| 3 or more | 1.33 (0.98–1.80) | 0.07 | 0.89 (0.67–1.19) | 0.44 |
| Elixhauser group, PY1 | ||||
| Less than or equal to 2 | Ref. | Ref. | ||
| 3 or more | 1.64 (1.25–2.14) | 0.0004 | 1.25 (0.95–1.64) | 0.11 |
| VA priority | ||||
| Group 1 | 1.28 (1.09–1.49) | 0.002 | 1.28 (1.02–1.62) | 0.03 |
| Groups 2, 3, 4, 5, 6 | Ref. | Ref. | ||
| A1c levels pre-diabetic range, Pre-COVID | 0.84 (0.71–0.99) | 0.04 | - | |
| Prior utilization | ||||
| Primary care, pre-COVID phone | — | 1.41 (1.12–1.76) | 0.003 | |
| Primary care, PY1 | ||||
| Face to face | 1.33 (1.04–1.71) | 0.02 | — | |
| Video | 2.49 (2.08–2.98) | <0.0001 | — | |
| Phone | 0.67 (0.49–0.92) | 0.01 | 2.44 (1.81–3.28) | <0.0001 |
| Endocrinology, PY1 video | 3.04 (2.08–4.45) | <0.0001 | — | |
| Pharmacy, PY1 | ||||
| Face to face | — | 1.51 (1.18–1.94) | 0.001 | |
| Video | 6.24 (4.11–9.48) | <0.0001 | — | |
| Telehealth visit, pre-COVID | 1.26 (1.06–1.50) | 0.009 | — | |
| Telehealth visit, PY1 | 1.86 (1.53–2.25) | <0.0001 | 1.62 (1.28–2.05) | <0.0001 |
| Surgery visit, pre-COVID | 1.20 (1.00–1.42) | 0.05 | - | |
| Mental health visit, PY1 | 0.81 (0.67–0.98) | 0.03 | - | |
| Cardiology clinic visit, PY1 | 1.22 (1.03–1.44) | 0.02 | 1.65 (1.20–2.27) | 0.002 |
| Pulmonary clinic visit, PY1 | - | 1.49 (1.03–2.16) | 0.03 | |
| Primary care visit, PY1 | - | 1.88 (1.41–2.49) | <0.0001 | |
| Diabetes visit, PY1 | - | 2.27 (1.44–3.58) | 0.0004 | |
Self-identified veteran race/ethnicity.
Qualitative analysis
We interviewed 13 VA providers and 15 veterans with diabetes with HI during the study timeframe. VA providers included five physicians (two primary care, two endocrinologists, one podiatrist), one diabetes educator, two dieticians, a VISN 1 Network Homeless Coordinator, two pharmacists, an optometrist, and a physical therapist. Providers were chosen to represent major care needs of veterans with diabetes.
The fifteen veteran participants were more likely to be ≥55 years in age (87%); male (80%); self-identified non-Hispanic, White in race (53%); divorced, separated (53%); 60% had a current “place to stay” (40% unstable housing; 13% homelessness); and were living in an urban location (60%; rural, 20%; suburban, 20%).
Qualitative analysis revealed four common themes reported by both VA providers and veterans, including: (a) overall VCC experience; (b) internet service and technology barriers; (c) the need for VVC education; and (d) variation by specialty and care type. Each of these themes will be discussed in more detail in the subsequent paragraphs.
Veteran and provider VVC experience
The majority of veterans and providers reported satisfaction with using VVC for diabetes care. Across VA clinics, when providers utilized VVC, they claimed that they were able to learn more about their patient's environment.
“Many veterans are in their room or a small space …the whole place is in such disarray that I just don't know how they even get through on a daily basis.” (Endocrinologist)
Veterans voiced confidence that VVC is a convenient way to stay connected to care, particularly since transportation was also barrier to care during the pandemic. Most veterans reported residing in a location that was more than 30 minutes from a VA clinic. Therefore, veterans appreciated the opportunity to be seen by a provider without having to go into the clinic.
“One nice thing about doing VVC through your iPhone is you don't need to worry about getting a ride to the clinic.” (Veteran, male)
A few veterans reported being very satisfied with the VVC encounters and preferred to continue with = the visits post-pandemic.
“I’d prefer to keep that [VVC] going for anything that I don’t need to be physically present for… I’m just as good over the laptop.” (Veteran, male)
Respondents reported that VVC satisfaction was driven by care availability and convenience. Providers mentioned the importance of VVC in facilitating routine patient care during a time of isolation. Veterans reported using VVC because it was a safe care option. Providers reported that they appreciated that VVC provided an option to connect with patients when in-person visits were not an option.
“It doesn’t surprise me that patients, whether they’re homeless or not, were happy to connect…and were not so worried about the mode as they were lonely and needed care.” (Diabetes Nurse, female)
Internet service and technology barriers
Lack of technology and internet service were the predominant barriers to VVC for providers and veterans. Forty percent of the veterans interviewed did not have a smartphone or tablet to utilize for VVC care. Veterans also commented that internet services were often not available at the time of care resulting an access barrier.
“Video depends on where you are at the time…most of the time when I’m talking with Dr [name] it fades in and out, we lose each other… I have to go somewhere with good Wi-Fi.” (Veteran, female)
The majority of providers mentioned that having Information Technology (IT) support on site influenced staff willingness to use VVC with their patients. IT support was often needed in the first month of the pandemic to ensure providers and/or veterans were able to connect to the encounter.
“The days when VVC wasn't working, we could still do a phone call … but someone to assist [with VVC] is helpful.” (Pharmacist, female)
VVC education
VVC training would increase utilization among providers and veterans. Providers reported variability in VVC knowledge and training, resulting to varying levels of uptake. Onsite technicians and trainings to prepare e providers for VVC encounters were essential to utilization.
“Prior [to COVID] I really hadn’t pursued [VVC] very much…but after the training was done, going through the good and bad of learning… when technology works, it’s great.” (Primary Care Clinician, male)
Providers mentioned that test sessions prior to the veteran's visit aided in the implementation of VVC encounter(s). Providers discussed how important these trial sessions were to VVC efficiency.
[After the training] “I had an 80-year-old figure out how to get on the video call and it was a success.” (Diabetes Nurse, female)
Many veterans reported needing help to log onto a VVC appointment, and over a quarter of individuals reported “not knowing what to do” if the video dropped.
“I probably would need some help with telehealth; I’m not very tech savvy… when I was in college, the technology we had was an ink pen, a calculator, and a jacket.” (Veteran, male)
Veterans reported frustration with providers who were not familiar with VVC. One veteran underscored the bidirectional need for education to successfully implement VVC encounters.
“Not everybody at the other end knows how to use technology…especially with some of the older doctors, teach them to keep up with the technology.” (Veteran, male)
Utilization variation: care and specialty type
Providers reported using VVC for follow-up or screening appointments while urgent acute care remained in-person during the pandemic. One provider described how she was able to safely continue the majority of clinical services through VVC during the pandemic.
“I did things by VVC that I did not think could happen…sensor trainings, pump trainings, blood glucose testing…never, never in a million years would I have thought that those things could happen without having somebody right next to me.” (Diabetes Nurse Educator, female)
Other specialties, such as optometry, podiatry, and audiology, were very limited in the care they could provide through VVC. While VVC provided a convenient option for clinical encounters, the lack of diagnostic tools that could be used for virtual encounters limited some specialty care use.
“Other than doing basic follow-up it is hard to treat patients in optometry by telehealth…we just don’t have the right equipment, but it is possible [with the right equipment].” (Optometrist, female)
Discussion
Among veterans with diabetes experiencing HI during the pandemic, those who utilized VVC were more likely to be female, younger, self-identified Hispanic, married, and residing in an urban dwelling. Need characteristics included having prior VVC visits, more comorbidities, and VA priority group 1, compared to their counterparts. In the qualitative study, many participants reported that VVC is an effective and convenient mode to conduct clinical encounters, especially when in-person visits are not safe. Veterans using VVC were satisfied with their encounters but also underscored barriers to overcome, including access to stable internet service and devices such as smartphones, and VVC training.
The present study's findings may reflect healthcare-seeking traits of the broader veteran population, in which females are more likely to engage in virtual visits.24,25 Studies have identified several factors driving VVC utilization among female veterans including higher technology comfort level, experience with telehealth, and convenience.26,27 VVC utilization was also more common among married veterans with diabetes experiencing HI. Significant others may provide social support and encourage veterans’ engagement in VVC, although this relationship in the context of HI needs further research.24,28,29
We observed that VVC users experiencing HI were more likely to be self-identified Hispanic, while in-person visits were more common in their non-Hispanic, White counterparts. Racial and ethnic variations in VVC utilization shifted during the COVID pandemic; whether video utilization will persist among self-identified Hispanic veterans is unknown.23,30 In general, self-identified Hispanic patients tend to report lower rates of video care due to language barriers and lack of health insurance. 31 Our findings corroborate recent studies showing that veterans who self-identify from racial/ethnic minority backgrounds used VVC more than self-identified non-Hispanic White veterans during the pandemic.8,32 This difference in VVC utilization may be reflective of self-identified Hispanic veterans’ access to VA healthcare compared to the general population in which a higher proportion of self-identified Hispanics are uninsured.31,33 Additionally, English proficiency is needed for U.S. military service, so language may be less of a VVC barrier for veterans compared to civilians. 32 Future research should examine VVC uptake among all self-identified Hispanic veterans, not just those experiencing HI.
Age is inversely associated with VVC utilization among veterans with diabetes experiencing HI. Older patients are less likely to participate in VVC, and the reasons are multifactorial including inexperience and lack of technology.34,35 Still, VA providers and veterans with diabetes reported willingness to use VVC when equipped with adequate resources and training, despite age.
Aligned with previous literature, our veterans reported that VVC reduces the travel distance, time, and costs to access their local VA.36,37
The VA has made large efforts to mitigate the digital divide among racial/ethnic, geographical, and age diverse veteran populations,38,39 but we found some of our participants voiced not knowing how to access technology resources. Prior to the pandemic, the VA expanded its video-enabled tablet program to a cell phone option available to eligible veterans with clinical access barriers.36,40 Recent trends demonstrate that following the tablet or cellphone receipt, veterans’ engagement in VVC increased across VA clinical settings. 40 These trends coincide with previous work which reported that veterans experiencing HI welcome technology-based care to improve access to services.41,42 Our interviews report that many veterans with HI do not know how to access VA digital technology. While the VA is committed to increasing virtual care for all veterans, our data suggests that initiatives which aim to increase veterans’ technology access and digital education are still needed.
While this study contributes to the current literature and our understanding of VVC utilization among veterans experiencing HI, there are limitations. First, our analysis was limited to veterans with diabetes in New England, so our findings may not be generalizable outside of this geographical region. Second, analyses were limited to veterans who had a care encounter between March 1, 2019, and March 1, 2022; therefore, it is possible that we may not have captured changes in use, clinical modality, and experiences among all veterans with diabetes experiencing HI during the pandemic. Third, interviews have the potential for recall and social desirability bias, although most interviews took place within the same month as the VVC visit. Furthermore, our research team has a strong track-record in maintaining the confidentiality and anonymity of qualitative responses, and querying with neutral questions in which the interviewee has been instructed that there are no right or wrong answers. Notwithstanding, this study uncovered some new characteristics of veterans with diabetes with HI who are willing to engage in VVC encounters and provided some insights into how to effectively engage this population in future utilization.
Conclusion
This study examined health care utilization and its modality among veterans with diabetes with housing instability and found that VVC played an important role in care access during the pandemic. Employing both quantitative and qualitative methods, we identified some facilitators and barriers to VVC utilization among providers and veterans with diabetes. A comprehensive knowledge of VVC utilization patterns by veteran characteristics may inform tailored interventions that seek to close identified disparities gaps. While convenience and safety were facilitators of VVC care, enhanced technology and education are essential to future uptake and to mitigating the digital divide. Future work should assess how best to integrate VVC into routine diabetes care as in-person care is restored to ensure equitable access to care.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-pdf-3-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-pdf-4-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Acknowledgement
The authors would like to acknowledge the National Center on Homelessness Among Veterans (NCHAV) which made this project possible.
Appendix A: VA specialty care telehealth
Telehealth enables you to connect to the quality care you need in more than 50 specialty areas from your local VA clinic.
Clinical specialty
| TeleCardiology | TeleChaplain | TeleDentistry |
| TeleDermatology | TeleEyeCare | TeleGenomics |
| TeleGIHepatology | TeleHematology | TeleICU |
| TeleInfectious Disease | TeleMental Health | TeleMOVE! |
| TeleNephrology | TeleNeurology | TeleNutrition |
| TelePathology | TelePharmacy | TelePodiatry |
| TelePrimary Care | TelePulmonology | TeleRheumatology |
| TeleSCI/D | TeleSpirometry | TeleStroke |
| TeleSurgery | TeleTransplant | TeleWholeHealth |
| TeleWound Care | Virtual PACT | Womens Health |
TeleRehabilitation
| TeleAmputation | Telehealth Assistive Technology |
| TeleBlind Rehabilitation | TeleChiropractic Care |
| TeleKinesiotherapy | TeleOccupational TherapyTeleOrthotic Prosthetic Care |
| TelePhysical Medicine Physicia | TelePhysical Therapy |
| TeleProsthetic & Sensory Aids Service | TeleRecreational and Creative Arts Therapy |
| TeleSpeech Patholog |
Source: VA telehealth: In the Clinic | Telehealth VA, 2024.
Appendix B: List of acronyms
Acronym definition
- CDW
Corporate Data Warehouse
- COVID-19
Coronavirus Disease-2019
- DSS
Decision Support System
- HER
Electronic Health Record
- HI
Housing Instability
- IT
Information Technology
- NCHAV
National Center on Homelessness for Veterans
- NPCD
National Patient Care Database
- PY
Pandemic Year
- VA
Veterans Affairs
- VHA
Veterans Health Administration
- VISN
Veterans Integrated Services Network:
- VVC
VA Video Connect
Footnotes
Contributorship: RK, AA, LC, and DM researched literature and conceived the study. All authors were involved in protocol development, gaining ethical approval, patient recruitment and data analysis. RK wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
The data that support the findings of this study are available from the corresponding author, RLK, upon reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This National Center on Homelessness for Veterans (NCHAV) Quality Improvement project was deemed exempt from oversight by VA Central Western Massachusetts ethical review board.
Funding: This work was supported with an intramural grant from the National Center on Homelessness among Veterans.
Guarantor: RK will take full responsibility for the article, including for the accuracy and appropriateness of the reference list.
ORCID iDs: Rebecca L Kinney https://orcid.org/0000-0001-6752-5715
Laurel A Copeland https://orcid.org/0000-0002-9478-0209
Supplemental material: Supplemental material for this article is available online.
References
- 1.Veteran Healthcare Administration. VA’s telehealth program is already the largest in the nation. It’s about to get bigger. Accessed September 1, 2023, https://federalnewsnetwork.com/veterans-affairs/2018/12/vas-telehealth-program-is-already-the-largest-in-thenation-its-about-to-get-bigger/
- 2.Veterans Healthcare Administration. VA Telehealth Services. Accessed: September 15, 2023. https://telehealth.va.gov/
- 3.Stroupe KT, Martinez R, Hogan TP, et al. Health care utilization and costs of veterans evaluated for traumatic brain injury through telehealth. Telemed J E Health 2019; 25: 1144–1153. [DOI] [PubMed] [Google Scholar]
- 4.Adams SV, Mader MJ, Bollinger MJ, et al. Utilization of interactive clinical video telemedicine by rural and urban veterans in the veterans health administration health care system. J Rural Health 2019; 35: 308–318. [DOI] [PubMed] [Google Scholar]
- 5.Garvin LA, Hu J, Slightam C, et al. Use of video telehealth tablets to increase access for veterans experiencing homelessness. J Gen Intern Med 2021; 36: 2274–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hare N, Bansal P, Bajowala SS, et al. Work group report: COVID-19: unmasking telemedicine. J Allergy Clin Immunol Pract 2020; 8: 2461–2473.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaker MS, Oppenheimer J, Grayson M, et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract 2020; 8: 1477–1488.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heyworth L, Kirsh S, Zulman D, et al. Expanding access through virtual care: the VA's early experience with COVID-19. NEJM Catalyst in Care Delivery 2020. [Google Scholar]
- 9.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020; 8: 659–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry BL, Aronson B, Pescosolido BA. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proc Natl Acad Sci U S A 2021; 118: e2020685118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev 2015; 37: 177–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beran D, Perone SA, Castellsague Perolini M, et al. Beyond the virus: ensuring continuity of care for people with diabetes during COVID-19. Prim Care Diabetes 2021; 15: 16–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartmann-Boyce J, Morris E, Goyder C, et al. Diabetes care. Diabetes and COVID-19: risks, management, and learnings from other national disasters. Diabetes Care 2020; 43: 1695–1703. [DOI] [PubMed] [Google Scholar]
- 14.Tsai J, Szymkowiak D, Jutkowitz E. Developing an operational definition of housing instability and homelessness in veterans health administration's medical records. PLoS One 2022; 17: e0279973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Price LE, Shea K, Gephart S. The veterans affairs’s corporate data warehouse: uses and implications for nursing research and practice. Nurs Adm Q. 2015; 39: 311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meditz RW, Manberg CL, Rosner F. Improving access to a primary care medical clinic. J Natl Med Assoc 1992; 84: 361–364. [PMC free article] [PubMed] [Google Scholar]
- 17.Elixhauser A, Steiner C, Harris DRet al. et al. Comorbidity measures for use with administrative data. Med Care 1998; 36: 8–27. [DOI] [PubMed] [Google Scholar]
- 18.Weller SC, Vickers B, Bernard HR, et al. Open-ended interview questions and saturation. PLoS One 2018; 13: e0198606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scientific Software Development. Atlas.ti, Qualtative Data Analysis Software . 2020. https://atlasti.com/support/support-center/
- 20.Kinney RL, Haskell S, Relyea MR, et al. Coordinating women's preventive health care for rural veterans. J Rural Health 2022; 38: 630–638. [DOI] [PubMed] [Google Scholar]
- 21.Nowell B. Public Administration Research and Theory, 2019. [Google Scholar]
- 22.Wagner C, Dichter ME, Mattocks K. Women Veterans’ pathways to and perspectives on veterans affairs health care. Womens Health Issues 2015; 25: 658–665. [DOI] [PubMed] [Google Scholar]
- 23.Cordasco KM, Yuan AH, Rollman JE, et al. Veterans’ use of telehealth for veterans health administration community care urgent care during the early COVID-19 pandemic. Med Care 2022; 60: 860–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darrat I, Tam S, Boulis Met al. et al. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg 2021; 147: 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindsay JA, Caloudas A, Hogan J, et al. Getting connected: a retrospective cohort investigation of video-to-home telehealth for mental health care utilization among women veterans. J Gen Intern Med 2022; 37: 778–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moreau JL, Cordasco KM, Young AS, et al. The use of telemental health to meet the mental health needs of women using department of veterans affairs services. Womens Health Issues 2018; 28: 181–187. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein KM, Zullig LL, Dedert EA, et al. Telehealth interventions designed for women: an evidence map. J Gen Intern Med 2018; 33: 2191–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pandey KR, Yang F, Cagney KA, et al. The impact of marital status on health care utilization among medicare beneficiaries. Medicine (Baltimore) 2019;98:e14871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammadi I, Wu H, Turkcan A, et al. Data analytics and modeling for appointment no-show in community health centers. J Prim Care Community Health 2018; 9: 215013271881169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferguson JM, Wray CM, Jacobs J, et al. Variation in initial and continued use of primary, mental health, and specialty video care among veterans. Health Serv Res 2023; 58: 402–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ryskina KL, Shultz K, Zhou Y, et al. Older adults’ access to primary care: gender, racial, and ethnic disparities in telemedicine. J Am Geriatr Soc 2021; 69: 2732–2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guajardo E, Amspoker AB, Stanley MA, et al. Patterns of telehealth use for mental health treatment among hispanic veterans. Telemed J E Health 2023; 29: 788–792. [DOI] [PubMed] [Google Scholar]
- 33.Tai DBG, Sia IG, Doubeni CAet al. et al. Disproportionate impact of COVID-19 on racial and ethnic minority groups in the United States: a 2021 update. J Racial Ethn Health Disparities 2022; 9: 2334–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hise N, Buckner J, Ince Set al. et al. Telemedicine at the VA: examining smartphone connectivity rates to VA video connect and doximity dialer video. Ann Vasc Surg Brief Rep Innov 2022; 2: 100147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsai J, Rosenheck RA. Use of the internet and an online personal health record system by US veterans: comparison of veterans affairs mental health service users and other veterans nationally. J Am Med Inform Assoc 2012; 19: 1089–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Slightam C, Gregory AJ, Hu J, et al. Patient perceptions of video visits using veterans affairs telehealth tablets: survey study. J Med Internet Res 2020; 22: e15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gordon HS, Solanki P, Bokhour BGet al. et al. “I’m not feeling like I'm part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med 2020; 35: 1751–1758.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SY L. Smartphones prove a smart solution to combatting homelessness. October 10, 2023. https://news.va.gov/111139/smartphones-solution-combattinghomelessness/#:∼:text=Initially%2C%20the%20smartphones%20were%20provided,were%20considered%20%E2%80%9Cloaner%20devices.%E2%80%9D .
- 39.Zulman DM, Wong EP, Slightam C, et al. Making connections: nationwide implementation of video telehealth tablets to address access barriers in veterans. JAMIA Open 2019; 2: 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wray CM, Van Campen J, Hu J, et al. Crossing the digital divide: a veteran affairs program to distribute video-enabled devices to patients in a supportive housing program. JAMIA Open 2022; 5: ooac027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McInnes DK, Sawh L, Petrakis BA, et al. The potential for health-related uses of mobile phones and internet with homeless veterans: results from a multisite survey. Telemed J E Health 2014; 20: 801–809. [DOI] [PubMed] [Google Scholar]
- 42.McInnes DK, Solomon JL, Shimada SL, et al. Development and evaluation of an internet and personal health record training program for low-income patients with HIV or hepatitis C. Med Care 2013; 51: S62–S66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-pdf-3-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH
Supplemental material, sj-pdf-4-dhj-10.1177_20552076241282629 for A mixed-methods study of VA video connect utilization among veterans with diabetes experiencing housing instability during the pandemic by Rebecca L Kinney, Laurel A Copeland, Jack Tsai, Alice A Abbott, Kate Wallace, Lorrie A Walker, Jillian Weber, Shara Katsos and Donald K McInnes in DIGITAL HEALTH