ABSTRACT
This paper reflects on the influences and outcomes of He Kāinga Oranga/Housing and Health Research Programme over 25 years, and their impact on housing and health policy in Aotearoa and internationally. Working in partnership particularly with Māori and Pasifika communities, we have conducted randomised control trials which have shown the health and broad co-benefits of retrofitted insulation, heating and remediation of home hazards, which have underpinned government policy in the Warm Up NZ-Heat Smart programme and the Healthy Homes Standards for rental housing. These trials have been included as evidence in the WHO Housing and Health Guidelines and led to our designation as a WHO Collaborating Centre on Housing and Wellbeing. We are increasingly explicitly weaving Māori frameworks, values and processes with traditional Western science.
KEYWORDS: Housing, health, wellbeing, policy interventions, mātauranga Māori, Pasifika
Introduction
Housing, land, infrastructure and people create a complex system. Housing is essential to social, cultural and environmental determinants of population health and wellbeing (Keall et al. 2010; Keall et al. 2012). In high-income countries such as Aotearoa New Zealand (Aotearoa), people spend most of their time indoors (Baker et al. 2007). Homes therefore potentially pose a health risk, but also provide opportunities to improve occupants’ health and increase equity (Howden-Chapman 2021).
He Kāinga Oranga/Housing and Health Research Programme was established in 2001 to investigate housing as a key determinant of health (Howden-Chapman and Carroll 2004). At that time, studies of the effects of housing on occupant health were unusual and required us to explore a wide variety of approaches. We were particularly concerned about growing inequalities in income, wealth and declining homeownership, particularly for Māori and Pasifika. We focused on housing, more than other structural determinants of health, because housing is a fundamental requirement for health and wellbeing. Everybody needs somewhere warm, dry, safe and affordable to live and call a home, yet Aotearoa has relatively low building and maintenance standards compared to other OECD countries (Douwes and Howden-Chapman 2011).
The aim of this article is to highlight why and how we established He Kāinga Oranga and broadly describe the research evolution over the last 25 years. It is not our intention here to summarise all our work but rather to highlight particular studies, their findings and their impact on housing policy. Our programme has been designed to provide an evidence base for improved housing and health policy that highlights the social and economic determinants of health and prioritises better outcomes for Māori and Pasifika. We begin by explaining the major influences for establishing He Kāinga Oranga before outlining our research goals. He Kāinga Oranga grew from the experiences of the Asthma Research Programme, which had already conducted several community studies to improve housing. Crane and colleagues intervened to improve heating and ventilation to control dust-mites (Crane et al. 1998). Public health, medical and Māori researchers collaborated with Wairarapa marae, concerned about high rates of asthma, to develop Asthma Prevention Plans, delivered at local marae (Beasley et al. 1993; D'Souza et al. 1994).
Te Rōpū Rangahau Hauora a Eru Pōmare research and other research had highlighted ethnic inequalities, which signalled the importance of designing sampling strategies that could addressed Te Tiriti o Waitangi and where possible incorporate equal explanatory power for Māori and Pākehā. These reports showed that the limited availability of quality, culturally appropriate housing, and discrimination in the rental housing (Harris et al. 2012) were associated with household crowding and higher rates of respiratory and infectious diseases (Pōmare et al. 1995; Blakely et al. 2005; Robson and Harris 2007; Te Rōpū Rangahau Hauora a Eru Pomare 2007).
Our parallel research in Pasifika communities followed in Dr Ian Prior’s footsteps and his long-standing relationship with the Tokelau community (Huntsman and Hooper 1997; Howden-Chapman and Woodward 2001) which indicated that many of these issues also affected the Pasifika community. Many multi-generational Pasifika families live in conventional three-bedroom houses designed for nuclear families, partly for cultural reasons and mutual support, but partly to lower each person’s rent burden (Pene et al, 2009a and 2009b). Stats NZ has highlighted that both Pasifika and Māori extended families continue to be more likely to be crowded.1 While most occupants are aware of the risks of household crowding and practise household behaviours to minimise these risks (Tiatia et al. 2016), crowding remains an important risk factor for close-contact infectious diseases, such as tuberculosis (Baker et al. 2011) meningococcal disease (Baker et al. 2000), rheumatic fever (Jaine et al. 2011; Bennett et al. 2022) and COVID-19 (Howden-Chapman et al, 2023). Furthermore, poor air and water quality and lack of access to adequate plumbing and sanitation, particularly in rental housing, are identified as household factors that contribute to the burden of infectious diseases (Amore et al. 2021), which are borne unequally by Maori and Pasifika households (Baker et al. 2012).
As a result of our partnership with the Tokelau community, which highlighted the fundamental problem of lack of affordable extended-family housing for migrants in Aotearoa compared to Tokelau (Howden-Chapman et al. 2000; Pene et al. 2009a), architect John Gray, Tokelau elders and researchers co-designed a multi-bedroom house for extended Pasifika families, which was built by Housing NZ in Porirua East, Wellington (Gray et al. 2008). Particular attention was paid to the multigenerational needs of the family and the need for good ventilation and heating (Pene et al. 2009a). This was the first occasion in which our research had a direct impact on the design and building of public housing.
Another significant international influence on our research programme was the momentum to link housing and health research through the UN Sustainable Development Goals (SDGs). The SDGs reinforced our systematic approach to addressing housing and the link to climate change (Howden-Chapman et al. 2017b; Grant et al. 2021). Urgent action is needed to mitigate climate change and make cities more sustainable, by increasing housing density and increasing active and public transport (Nilsson et al. 2018). Our sister research programme at the NZ Centre for Sustainable Cities, established in 2008, links our housing research to the pressing challenges of these wider urban systems, while supporting healthy, inclusive communities with diverse populations (Stuart and Thompson-Fawcett 2010; Ryks et al. 2014; Ürge-Vorsatz et al. 2014; Olin et al. 2022).
Research goals
He Kāinga Oranga’s overarching research goal is to contribute to the policy evidence needed to improve the quality and supply of sustainable housing, and hence health and wellbeing (Davis and Howden-Chapman 1996). Nationally, we work closely with iwi Māori and Māori Urban Authorities, community agencies, government departments and the Crown entity Kāinga Ora–Homes and Communities. Internationally, our national and international contribution was recognised by our designation in 2021 as a WHO Collaborating Centre on Housing and Wellbeing.2
He Kāinga Oranga began with the goal of analysing the evidence that poor quality housing affects health, and what practical interventions can make a difference, particularly for younger and older populations (Howden-Chapman et al. 1999), as well as Māori, Pasifika and other extended or multigenerational families, who live, or want to live together. Our multidisciplinary team works on the ‘borders of disciplinary imagination’ (Haigh et al. 2019), recognising that our view of the role of different types of evidence and their practical adequacy are not necessarily shared by others. We are building particularly on our decades long partnerships with the Tū Kōkiri Marae Keriana Olsen Trust and Tū Kotahi Māori Asthma Research Trust and Otago’s Memorandum of Understanding with Ngāti Toa Rangatira. Our ethos of ‘no survey without service’ is to ensure that the communities who share their knowledge with us also benefit from their engagement.
Increasingly, we are relying on Stats NZ’s Integrated Data Infrastructure (IDI) which, within strict and appropriate ethical and privacy constraints, and active consideration of Māori data sovereignty, allows us to analyse linked government administrative data on all citizens/residents and households to increase understanding of the antecedents of health and wellbeing, as well as the consequences. A key current goal is not only to utilise the Western-based model of science, but also to recognise and prioritise more explicitly Māori and Pasifika worldviews and research approaches in framing and answering important questions about the health and wellbeing impacts of housing. Our current efforts in relation to this goal are discussed toward the end of this paper, in the ‘Weaving together Western and Indigenous frameworks’ section.
Housing interventions for health and wellbeing
Temperature, respiratory and cardiovascular disease
Many homes in Aotearoa are cold in winter (Howden-Chapman et al. 2009; Howden-Chapman et al. 2012). Excess winter mortality occurs when housing does not adequately protect occupants from winter temperatures and infections (Davie et al. 2007; Telfar Barnard et al. 2008; Mann et al. 2009; O'Sullivan et al. 2011; Viggers et al. 2013; O'Sullivan et al. 2015), because of the combined effects of low-quality housing, inadequate insulation and fuel poverty linked to low incomes (Boardman 2010). Energy costs have risen about 40% faster than other household costs over the past 20 years3 and usually only limited areas of homes are heated; children’s bedrooms, which are often south-facing, are frequently unheated (Shorter et al. 2022). Inadequately heated houses are more likely to be damp and this can lead to the growth of mould (Oreszczyn et al. 2006) which, independently of temperature, can cause respiratory difficulties (Institute of Medicine of the National Academies 2004). A case control study of children living in cold, damp houses found that these children were more likely to be hospitalised for acute respiratory conditions (Ingham et al. 2019) and that once a child was admitted to hospital, they were more likely to be readmitted (Oliver et al. 2018).
These descriptive studies indicate that low indoor temperatures can cause illness and death, particularly among vulnerable young and older people, but focus less on preventive public health interventions and action to improve housing policy or building standards. After the 1970s oil shocks, the International Energy Agency focused on the demonstrable co-benefits of improving thermal efficiency in existing housing (Ryan and Campbell 2012) and referenced the underlying evidence produced by He Kāinga Oranga. The Housing, Insulation and Health Study was a household intervention, evaluated by a randomised control trial (RCT) of retrofitted insulation in 1,350 households, with 4,407 occupants, of whom two-thirds at baseline reported damp and three-quarters reported mould (Howden-Chapman et al. 2005). We deliberately enrolled 200 households in each of seven areas with significant Māori populations and organisations: South Auckland, Taranaki, Bay of Plenty, Nuhaka/Mahia, Porirua, Christchurch and Hokitika; half these households were Māori (49%) and a fifth were Pacific (22%) compared to 15% and 6% respectively in the total population (Howden-Chapman et al. 2005). The intervention resulted in a significant increase in indoor temperatures and decrease in humidity in the insulated houses, as well as savings in energy consumption relative to control houses. These indoor environment changes were sufficient to significantly improve the occupants’ self-reported health, wheezing, visits to doctors, days off work and children’s days off school (Howden-Chapman et al. 2007). Although a reduction in hospitalisations was not statistically significant, a cost-benefit analysis found benefits outweighed costs by a ratio of 1.8–1 (Chapman et al. 2009). In many quantitative studies, sample sizes are not sufficient to produce statistically significant conclusions for Māori subpopulations, but we followed the recommendations of Māori colleagues to ensure the sample would provide parity of explanatory power to enable identification of any differential Māori / non-Māori effect of the intervention (Reid et al. 2017).
As the average indoor temperature in the houses in the Housing, Insulation and Health Study did not reach the WHO recommended 18°C (64oF) we followed this trial with the Housing, Heating and Health Study, which involved replacing unsafe, portable unflued gas heaters (UFGHs) in the homes of 409 children with asthma (Gray et al. 2008). Because UFGHs release nitrogen dioxide (NO2) and other combustion by-products such as formaldehyde, they were replaced at no cost to the homeowner with their choice of a more efficient and effective heater: a flued gas heater; a heat pump; or a wood-pellet burner (Boulic et al. 2008; Howden-Chapman et al. 2008). Homes in the intervention group subsequently had significantly lower levels of NO2 in both living areas and children’s bedrooms (Gillespie-Bennett et al. 2008). Measurements of daily lung function and hourly indoor temperature showed that higher indoor temperatures had a small, but significant positive association with short-term variations in the lung function of children with asthma, who suffered greater upper and lower respiratory symptoms and used reliever medication more frequently (Gillespie-Bennett et al. 2011; Pierse et al. 2013). Independently-measured school absences were reduced by 21% (Free et al. 2010). Despite these 2008 findings being disseminated widely, UFGHs continue to be legal and widely available. They are more likely to be used by low-income tenants because they are portable and the fuel, though more expensive, can be pre-purchased.
In 2009, the Government rolled out the Warm-up NZ Programme nationally. The basis for investment in this combined insulation and heating scheme was the demonstrable health benefits (Howden-Chapman et al. 2007; Gray et al. 2008) and the estimates of cost-effectiveness in terms of morbidity and mortality prevented, compared with the costs of remediation (Chapman et al. 2017). This Programme has now been evaluated three times, first in a quasi-experimental cohort study using an administrative sample of about 900,000 people that looked at the risk of mortality for older members of the cohort, who had prior cardiovascular or respiratory hospitalisations, compared to a matched control group. The study found a significant protective effect from the retrofitted insulation for those with existing circulatory conditions, accompanied by a fall in energy use; but no significant changes were found for the addition of a heating intervention (Preval et al. 2017). A second quasi-experimental evaluation used a retrospective cohort design and compared changes in hospital admissions for intervention and control groups from 2009 to 2014 (Fyfe et al. 2020). Hospital admission rates were significantly lower in the intervention population. Post-intervention, lower hospital admission rates were found for asthma, cardiovascular disease, and ischaemic heart disease among Pasifika Peoples and for people over 65 years. There was also a four percent reduction in pharmaceuticals for treating respiratory exacerbations in the intervention group, but no change in medication to prevent asthma (Fyfe et al. 2022). The third most recent two-year study of the health and energy effects of the installation of heat-pumps found significant increases in indoor temperatures, well-being and reductions in electricity bills with a wellbeing Benefit Cost ratios of 7.49. 4
Another approach to warming the indoor environment follows studies in the UK (Osman et al. 2008; Osman et al. 2010) and Aotearoa (Viggers et al. 2013) which have explored using heating vouchers to reduce fuel poverty in vulnerable households. A recent UK House of Commons report has highlighted definitional issues of fuel poverty–as yet unresolved in Aotearoa–which make monitoring policy effectiveness problematic (Hinson and Bolton 2022). In 2019, the NZ Government introduced a Winter Energy Payment for people over 65 years and welfare beneficiaries (New Zealand Ministry of Social Development 2022). To evaluate the effectiveness of this policy, people over 55 years with doctor-diagnosed chronic obstructive pulmonary disease were recruited into the RCT Warm Homes for Elder New Zealanders Study, where their houses were insulated and they received an electricity voucher. The primary outcome was exacerbations requiring treatment with antibiotics, and/or corticosteroids (Viggers et al. 2013). The initial results showed no significant health gain among the intervention group, although secondary analyses suggested a lower mortality rate among participants assigned to the initial intervention group, suggesting that behavioural modification, through timing of messaging, may be important to the intervention group (Viggers et al, submitted).
Cold houses increase damp and mould, which was recently highlighted by the tragic death in the UK social housing of a two-year-old child from mould,5 and also accounts for a substantial proportion of the burden of respiratory disease in NZ (Riggs et al. 2021). Two of our intervention studies have focused on the vulnerability of children exposed to cold bedrooms. The MOULD study was an incident case-control study involving 150 children, aged between one and seven years, with new-onset wheeze, each of whom was matched to two control children with no history of wheezing. Children were skin prick tested with common allergens to establish atopy. The intervention was thermostatic heaters installed in the children’s bedrooms. Repeated measures of temperature and relative humidity were taken (Shorter et al. 2022); the presence and type of airborne microbes were collected on novel electrostatic dust cloths and analysed by qPCR. Neither temperature, relative humidity, nor microbes were associated with new-onset wheezing (Karvonen et al. 2019). Each child's home was assessed for moisture damage, condensation, and mould growth by researchers, independent building assessors and parents. There was a strong, positive, dose-dependent association between observations of visible mould and new-onset wheezing in children. This association between mould and new-onset wheeze was not modified by the children’s atopic status, suggesting a non-allergic association (Shorter et al. 2018). A linked study, NEST, being submitted, is a primary prevention study focused on babies, which aims to protect newborn infants being hospitalised for respiratory symptoms by heating the infants’ rooms and providing a variety of sleep-sacks made of different materials to explore the possible effects of these materials on the development of allergy and respiratory disease.
Indoor air quality, ventilation and infectious diseases
Children, people with chronic illnesses or disabilities and older people are more vulnerable to the indoor housing environment as they spend more time at home and make more demands on the home (Baker et al. 2007; Preval et al. 2017). WHO guidelines (World Health Organization 2009a and 2009b) considered natural ventilation as one of the most effective ways to reduce spread of infection and maintain health and wellbeing, although this relies on good quality outdoor air; some of our work has illustrated the association between indoor and outdoor NO2 levels in urban areas (Shaw et al. 2020). Indoors, infectious airborne viral particles can accumulate, putting everyone in the room at risk of infection, unless indoor air is continuously replaced with outdoor air (Escombe et al. 2007).
As Baker and colleagues have shown, lack of ventilation in homes contributes to the transmission of pulmonary tuberculosis (Baker et al. 2008), which is usually an airborne disease spread through infectious aerosols generated by infected people (Riley et al. 1995). Good ventilation is not only beneficial in preventing infectious disease transmission but can reduce indoor moisture and concentrations of toxic indoor air pollutants. According to the US Environmental Protection Agency, indoor air pollutant levels are typically two to five times higher than outdoor levels, and in some cases can exceed outdoor levels of the same pollutants a hundred-fold (United States Environmental Protection Agency 2022).
Mandatory lockdowns to prevent the spread of COVID-19 have highlighted the importance of appropriate building, heating and ventilation standards to prevent the spread of close-contact infectious disease, while accommodating viable day-to-day living and working arrangements. COVID-19 amplified existing inequalities linked to housing in low-, middle- and high-income countries (Shorter et al. 2022). The recognition of the importance of these factors was further amplified when it became evident that the COVID-19 virus was spread by airborne transmission (Morawska and Milton 2020), and socialising outside was safer than inside.
People who had been confined by lockdowns and were able to afford to move between houses, favoured suburbs with more space, both inside, which facilitated working from home, and outside. In many countries, the COVID-19 recovery stimuli created varying economic impacts. Along with a housing boom benefiting those with discretionary income, millions of people, particularly in the informal economy, lost income or jobs, and are behind in rents or mortgage payments, and are more at risk of eviction or foreclosure (Joint Center for Housing Studies of Harvard University 2021). Consequently, the NZ government along with many other countries introduced eviction moratoriums. He Kāinga Oranga researchers working with researchers from Waikato-Tainui College for Research and Development, and Tū Kotahi Māori Asthma Trust, secured a Marsden-funded research grant, Representation, Discourse and Reality: Eviction and its consequences in 2017. Through this we have conducted in-depth interviews on the profound effect of eviction on families before and during the COVID pandemic (Chisholm et al. 2021a) and noted an imbalance of power between landlords and tenants in the Tenancy Tribunal (Toy-Cronin and Bierre 2022).
Injuries and disabilities
In the WHO Housing and Health Guidelines Development Group (Howden-Chapman et al. 2017), household risks for injuries are highlighted as one of the key factors for protecting public health, particularly for people with disabilities (World Health Organization 2018). Keall and colleagues showed that high rates of home injury correspond to the high prevalence of housing hazards, indicating that addressing safety is a likely pathway to reducing injury rates (Keall et al. 2013). The Home Injury Prevention Intervention (HIPI) RCT, conducted with WISE Better Homes in Taranaki, studied rates of fall injuries for occupants in 840 homes (Keall et al. 2015). Half of these homes were randomised to receive modifications, such as handrails on outside steps and internal stairs and grab rails for bathrooms; control homes received the same modifications at the end of the trial. There was a 26% reduction in the rate of injuries caused by falls in the treatment group compared to the controls, and injuries specific to the home-modification intervention were cut by 39%. An economic analysis of this intervention found that the costs of home fall injuries fell by 33%, indicating that more expensive/severe injuries were likely to have been prevented to a greater extent than more minor injuries. The social benefits of injuries prevented were estimated to be at least six times the costs of the intervention. This benefit–cost ratio could be at least doubled for older people and increased by 60% for those with a prior history of fall injuries (irrespective of age).
As the HIPI study did not have adequate explanatory power to estimate the safety benefit for Māori, Cunningham and colleagues carried out a trial of 150 homes with Māori occupants, supplemented by a further 100 Māori homes funded by the He Kāinga Oranga research programme. Combining both studies there was a 31% reduction in the rate of fall injuries in the modified homes compared with households in the control group (Keall et al. 2021). Because Māori households are on average larger than non-Māori households, the intervention cost of each fall injury prevented was only around two-thirds of that for the previous HIPI intervention, indicating even greater cost-effectiveness and potential to reduce injury for Māori. This study demonstrated the benefits of conducting a separate study with Māori participants as opposed to a single larger study consisting of Māori and non-Māori: the focus could clearly be on the results for Māori, with potentially much greater policy traction, rather than for Māori as a comparison group. Even though a given study involving both Māori and non-Māori can achieve equal explanatory power for each group (Reid et al. 2017), a statistically significant estimate of the difference in benefits between the groups normally demands far larger sample sizes (assuming that such a difference does exist).
Housing standards and their enforcement
Housing standards vary from country to country, because of different climates, geography, housing stock and culture. They can be formal like a Building Code, which is part of the country’s legislative framework, or informal as with the regular home inspections by the women’s committees in Tokelau. Housing and health policies can also be centralised or collaborative. The overall effectiveness of formal guidelines to improve health and wellbeing, building codes and regulations, remains unclear and is an important research area (Werna et al. 2020). Regulations in Aotearoa are in some cases contentious (Howden-Chapman et al. 2011); state involvement to create and enforce housing standards can theoretically raise the cost of providing housing for lower income households, but also increase health and wellbeing, prevent hospitalisations and promote equity. The enforcement of legislation, particularly in rental housing, often lacks adequate scrutiny from planning and building control agencies, particularly for low-income households with significant socio-economic deprivation (Bierre et al. 2015; Sharpe et al. 2018; Chisholm et al. 2020a).
By contrast with Aotearoa, in England and Wales, the Health and Safety Rating System (HHSRS) became legally applicable to all dwellings and enforceable in 2006 (Housing Health and Safety Rating System (England) 2006, and Housing Health and Safety System (Wales) 2006, applying Part 1 Housing Act 2004. HMSO, UK). The HHSRS was later incorporated into the Decent Homes Standard, an administrative standard applied to all public sector dwellings and a target for all private rented dwellings (Homes (Fitness for Human Habitation) Act 2018 et al., Department for Communities and Local Government 2006; Howden-Chapman et al. 2017a). This Standard highlighted that unhealthy dwellings not only have a negative impact on physical, mental and social wellbeing, but also interfere with occupiers’ feeling of being ‘at home’. Progress in achieving these standards is regularly reported in the House of Commons and the media (Ministry of Housing 2018).
He Kāinga Oranga adapted the HHSRS framework to Aotearoa rental housing as a voluntary Rental Housing Warrant of Fitness (RWoF) proposal. This RWoF was based on the evidence of removing health hazards identified in the RCTs outlined above (Gillespie-Bennett et al. 2013; Bennett et al. 2016; Telfar-Barnard et al. 2017, 2019; Chisholm et al. 2019a; Pierse et al. 2020; Werna et al. 2020). While it generated considerable policy and public interest, it was eclipsed by the NZ Healthy Homes Guarantee Act (New Zealand Government 2017), which established the Healthy Homes Standards for rental housing. With a few exceptions (e.g. injury hazards), it had similar scope to the RWoF. The Ministry of Business, Innovation and Employment is responsible for initiating enforcement.
A collaborative partnership between local communities, academics, medical staff, the Ministry of Health and the private sector has developed a broad-based intervention informed by the WHO Healthy Housing Guidelines (World Health Organization 2018) called the Healthy Homes Initiative (HHI) (Chisholm et al. 2019b; International Science Council and British Broadcasting Documentary 2022). The HHI is a targeted programme to remediate the homes of low-income families who have had a child hospitalised for respiratory or infectious diseases, to prevent the readmission of children into hospital (Pierse et al. 2020). Over three-quarters of the participating children are from Māori and Pasifika homes. An independent, interim outcomes evaluation carried out by Pierse and colleagues utilising administrative IDI data found that the HHI programme had received 15,330 eligible referrals and delivered over 40,000 interventions to low-income households. This resulted in 1533 fewer hospitalisations, 9443 fewer general practice visits and 8784 fewer filled prescriptions in the first year after the programme’s intervention. The consequent savings to the health care system are estimated at approximately NZ$10.4 million annually, with the break-even investment period expected to be less than two years. This is a conservative estimate, as the initial analysis was based only on health outcomes from the first year after intervention and only for the referred child account (Pierse et al. 2019a). The latest report takes benefits for all household members into account over three years and shows a broad range of benefits: hospitalisations per person were reduced by 19.8% and school attendances and employment increased (Pierse et al. 2019b, 2022).
Inequalities and cumulative disadvantages
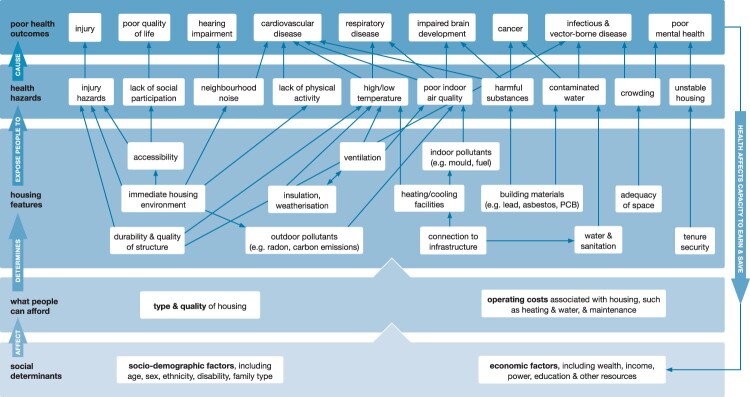
Housing has not only been a core activity area for public health but is a central component in tackling poverty (Shaw 2004). There is growing international evidence that disparities in housing are patterned along with other social, demographic, economic and environmental factors and contribute to the cumulative burden of persistent poor health outcomes in affected groups (Howden-Chapman et al, 2023). Figure 1 shows the socio-economic and demographic factors that shape housing, as well as the pathways and interventions that can be made to improve health and wellbeing.
Figure 1.
Pathways Housing and Health.
Owning a home is the largest asset for most households and tenure patterns graphically highlight which groups have an asset base to buffer them in hard times. Māori, Pasifika, disabled and low-income people, who have lower rates of homeownership, are more likely to be exposed to poorer rental housing conditions and consequently have higher levels of avoidable housing-related hospitalisations (Howden-Chapman et al. 2021). Housing costs are relatively high internationally and until recently have consumed an increasing proportion of disposable household income. The quality of the urban neighbourhood contributes to this pattern of advantage and disadvantage. Housing affordability is partly determined by the occupants’ costs of transport, which are in turn affected by housing location and the accessibility of public transport (Center for Transit-Oriented Development and Center for Neighborhood Technology 2006).
Stability and mobility
Insecure housing is historically patterned in many countries by ethnic and income inequality, which adds to cumulative disadvantage. The experience of land loss is an element common to many colonised Indigenous people. Ongoing alienation of Indigenous people’s communal land has severely restricted the location, quality and suitability of housing that is available to them, for example, socially-based tenure options or multi-generational housing typologies like papakāinga. Moreover, land alienation reduces the intergenerational asset base and cultural connections to the homeland (Kunitz 2007; Thom and Grimes 2022), inhibiting Māori access to multiple spaces of belonging. The notion of home for Māori ‘incorporates multiple scales and spaces’ (Olin et al. 2022, p. 7), which recognise the importance of maintaining connection with the ‘ancestral whenua’ (Berghan 2021, p. 6), In addition, new migrants, facing discrimination in the rental housing market, are often ‘trapped’ in inadequate housing leading to anxiety and reduced wellbeing (Teariki 2017).
There has been little research into the health effects of residential mobility and instability (Kearns and Parkes 2003), particularly for children and adolescents. It reduces the predictability of the environment and disrupts social networks, which can affect wellbeing. We know that moving house is a stressful experience and for tenants is less likely to be voluntary. In Aotearoa, a retrospective cohort study of children born in 2004, using data from the IDI, recorded children’s contact with government services to study both the socio-emotional behavioural (SEB) and health effects of moving residence. Of 313,164 children who had completed a before-school check showing SEB difficulties at four years of age, over two-thirds (69%) had moved house since they were born and 12% had moved more than four times. There was a linear association between residential mobility and increased SEB difficulties; and children exposed to greater residential mobility were eight percent more likely to obtain SEB difficulties scores, which are clinically problematic, than children exposed to fewer moves (Nathan et al. 2019). Using the same cohort, potentially avoidable hospitalisations were determined from hospital discharge data. Half the children had moved by two years of age; again there was a linear association between higher residential mobility and the increased likelihood of avoidable hospitalisation (Nathan et al. 2022).
Rental housing, housing providers and wellbeing
There has been comparatively little research into the important ways in which housing services, beyond those directly provided by the dwelling, can underpin positive health and wellbeing (Clapham et al. 2018). The housing maintenance behaviour of landlords in response to incentives, taxation and regulatory policies is a key factor (Chisholm et al. 2019). Research on HHIs has shown that improving housing quality gives people an increased sense of place, belonging and greater sense of wellbeing (McKay and Eggleton 2022).
Tenants have poorer health on most health and wellbeing measures. Two recent studies, both qualitative and quantitative, have focused on tenant wellbeing while exploring the additional impact of broader organisational processes and factors. A Scottish study, Housing Through Social Enterprise study, found that housing improvements and the quality of the housing services improved tenant wellbeing while providing them with a sense of home, and a recuperative space to retreat from daily life (Garnham et al. 2022). The study raises important questions about the limits to which either social or private housing providers can meet the needs of vulnerable tenants. It suggests that approaches to housing for low-income tenants need to go beyond providing a basic dwelling, to successfully intervene in the cycle of poverty, poor housing and poor health.
Tenant wellbeing is also the main focus of our current MBIE-funded programme, Public housing and urban regeneration: maximising wellbeing (PHUR), an ongoing, multi-centre, multi-disciplinary, five-year research programme that takes a community-based participatory systems approach (Israel et al. 1998) and focuses on the broader co-benefits of improving public housing in urban areas (Chapman et al. 2017). This programme evaluates the current major investments in public and affordable housing as part of urban regeneration, framed by a social, cultural, health and environmental wellbeing model aligned to the current government’s wellbeing budget model (Rangiwhetu et al. 2020). The research team is working in collaboration with seven public and community housing providers: Tāmaki Regeneration Company; Kāinga Ora–Homes and Communities, Porirua City Council and Ngāti Toa Rangatira; Wellington City Housing; the Wainuiomata Marae Trust; Ōtautahi Community Housing Trust, Dwell Housing Trust; and Salvation Army Social Housing. Some of the context for this project is provided by our previous University of Otago-funded research on how ideas about tenure mix are informing urban regeneration (Chisholm et al. 2021a, 2021b) and how contrary to conventional views, the concentration of public housing in a community supports tenant wellbeing (Chisholm et al. 2022).
A survey of the factors affecting the health and wellbeing of tenants is being analysed and these data will be supplemented by interviews with board and executive members and measures of tenant outcomes from the IDI. Overall, the research team is focused on: the landlords’ governance and financial arrangements; management reporting, particularly in relation to mātauranga Māori and the politically binding Te Tiriti o Waitangi; the design, quality, and scale of housing; the quality of the indoor environment; the community formation in relation to the surrounding neighbourhood and the influence of local urban design; energy and transport access; and the carbon emissions associated with the operational energy used in the housing and the tenants’ transport (Chapman and Howden-Chapman 2021). Other outcomes are the landlords’ approach to sustaining tenancy, the quality of urban regeneration efforts and outcomes, and the overall impacts on tenants’ and community wellbeing.
One of the overarching objectives of the programme is to make Te Ao Māori central to the research, given that Māori make up over a third of public housing tenants (Chisholm et al. 2022). All projects are reviewed and given feedback by Māori researchers within our team, particularly in terms of how they give effect to Vision Mātauranga and kaupapa Māori research methods. Three papers viewing wellbeing from different cultural perspectives are currently being finalised; including one which outlines a Whakawhanaungatanga Māori Wellbeing Model (Penny et al, in preparation) and one which outlines a Pasifika Wellbeing Framework (Teariki et al, in preparation). Another paper Māori Perspectives on Sustainability (Logan-Riley et al., in preparation) will contribute to the growing literature on this topic.
One of the critical measures of sustainability in relation to the built environment is reducing the amount of carbon embodied in new multi-level apartments, for example by substituting engineered timber for concrete slabs, as well as remediating existing public and other housing (Ürge-Vorsatz and Chapman 2021), and the ongoing emissions from household energy use (Grant et al. 2021) including from transport. Emissions can be reduced not only through higher energy efficiency standards, but also by locating housing closer to public transport interchanges and routes, which reduces emissions of local and global pollutants, particularly greenhouse gases, and provides multiple health co-benefits (World Health Organization 2011; Ürge-Vorsatz et al. 2014). The increasing rapidity of climate change makes it clear that tenants and other occupants need to be protected from extreme temperatures–more intense, prolonged heatwaves, as well as increasing periods of intense, cold weather. In our PHUR research programme, we are collecting household data in both summer and winter, along with electricity consumption, to better understand the relation between indoor temperatures and wellbeing.
Towards a more integrated approach
Improving the quality of housing and housing services so that people can have equitable access to affordable, warm, dry, safe houses, is at the forefront of public health research, policies and practice. Not only can improving housing lower the evident burden of disease (BoD), but there is growing evidence that it can increase the wellbeing of occupants and the communities in which they live (Rolfe et al. 2020; Rolfe and Garnham 2020; Davillas et al. 2022), as well as contributing to environmental sustainability (Chapman and Howden-Chapman 2021).
Following on from earlier work on the environmental BoD associated with inadequate housing in Europe (Braubach et al. 2011), we conducted an Aotearoa BoD study which analysed the considerable costs of poor housing arising from crowding, cold, damp or mould, and injury hazards linked to falls (Riggs et al. 2021). Hospitalisation data, no-fault accident insurance claims and mortality data were used to estimate the annual BoD from the most severe cases, as well as the resulting costs to the public sector. Using measures of the value of a statistical life, the estimated indirect cost of deaths and direct public sector costs attributable to these housing conditions was approximately NZ$141 million annually. A total of 229 deaths annually could also be attributable to adverse housing conditions. The costs to society from these deaths were around NZ$1 billion per year.
The BoD approach is an effort to evaluate many aspects of housing in terms of a consistent economic assessment of the health costs of the current housing system and implicitly the health benefits where better housing is provided, using the dollar value of costs and benefits to compare various policy investments (Keall et al. 2011). More recently, another way to view the impacts of housing is as an asset and researchers have considered returns on investments from various interventions (Davison et al. 2020). Being explicit about the assumptions that drive public health benefits entails considering the effect of assumptions on outcomes (Chapman et al. 2017). To date, this thinking tends to be underpinned by a narrow idea of trade-offs – dollars invested in one area are not available to be invested elsewhere – rather than thinking in terms of complementary positive outcomes in health and wellbeing. Improving people's living conditions, for example, by installing efficient heaters can not only reduce hospitalisation costs, but also improve comfort and higher quality life-years.
The government wellbeing policies and housing policies are prefaced on co-benefits, which align with outcomes elsewhere in the urban system and beyond. For example, in addition to directly saving health costs from better quality housing, better located housing in well, connected, walkable and activity-friendly neighbourhoods can also lead to more physical activity and thereby generate health benefits including less obesity (Sallis et al. 2016).
Weaving together western and indigenous approaches
In response to Māori preference for hapori to be able to build on communally-owned land, there is increasing state funding for papakāinga housing within the Māori housing framework MAIHI.6 MAIHI is a place-based approach and looks to develop partnerships with local Māori organisations who know their communities best, and can apply a kaupapa Maori lens to deliver solutions that are relevant to the various benefits of investing in marae-based housing and home-ownership and co-delivered by Maori. The MAIHI programme, though not without sectoral complications, recognises the growing desire for Māori to co-determine the rules of engagement with the government (Walker and Barcham 2010), underscored by Te Matapihi, the Māori peak housing organisation7 and Waitangi Tribunal reports.
Our approach to investigating health and wellbeing in relation to housing and neighbourhoods has primarily focused on research methods and guidelines that prioritise structural interventions that protect occupants from temperature extremes and injuries, as well as social and cultural practices around household crowding, a prime driver of infectious, close-contact diseases. For example, we know that people who feel secure in their identity, including their cultural identity and history of place, are more likely to report a more complete sense of wellbeing.
We prioritise collaborating with Māori and Pasifika communities and practise our values of ‘no survey without service’ to ensure that individuals, whānau (families) and communities who share their knowledge with us also benefit from their engagement. Depending on the questions we and our community partners are asking, we seek equal explanatory power between Māori and non-Māori participants, or when appropriate seek only Māori or Pasifika participants to enable group-to-group comparisons.
One of the positive challenges and opportunities in public health research in Aotearoa is identifying the limitations to Western approaches and continuing to learn from Indigenous approaches. We increasingly incorporate Te Ao Māori and Pasifika perspectives and concepts, which fundamentally look at health and wellbeing through a more holistic lens and include positive and negative impacts on mental, spiritual and cultural wellbeing and resilience (Macfarlane and Macfarlane 2019; Logan-Riley 2022). We are committed to undertaking research in partnership with Māori communities and Pasifika organisations, developing whanaungatanga (relationships) and prioritising kanohi ki te kanohi (face-to-face) and wānanga (learning) opportunities. Whenever we are invited, we strongly support Maori-led research and exchange knowledge and research findings with our partners and participants through inclusive hui (meetings) and other mediums (such as joint publications or short films accessible via YouTube).8
Our commitment to Te Tiriti o Waitangi and giving effect to Vision Mātauranga is evidenced by our focus on methodologies and interventions which support the kaupapa of our Māori partners, as well as the advancement of Māori iwi, hapū and whānau. In Wainuiomata, the urban Māori Trust is partnering with Kāinga Ora to build papakāinga housing with solar PV panels which, once linked to the marae, have the potential to form a smart grid providing opportunities for on-site energy sharing leading to reduced energy costs to residents as well as greater energy resilience to the community. He Kāinga Ora and potentially Te Puni Kokiri are government partners in He Tipu Manahau, innovative research which highlights to government agencies the strengths of Māori community processes, resources and structures, such as communally-owned land, the marae and the Wainuiomata Trust’s support of social and cultural practices, which non-Māori communities can also learn from (Stuart and Thompson-Fawcett 2010).
We are also engaged with the Waitangi Tribunal's Kaupapa Inquiry on Housing Policy and Services, through the facilitation of Te Matapihi. Our evidence provided to the Tribunal focused on homelessness and was heard at Te Puea Memorial Marae in August 2021. Our evidence drew on our work from the MBIE-funded research programme Ending Homelessness in New Zealand: Housing First (Ombler et al. 2017; Lawson-Te Aho et al. 2019; Pierse et al. 2019; Fraser et al. 2021; Fraser et al. 2022), and our work on severe housing deprivation (Amore et al. 2021) and housing lacking basic amenities (Viggers et al. 2021). Further contributions to this Inquiry is revolving around the Tribunal’s categories of whenua Māori, social/public housing, health and housing, and the housing market. Because our research is increasingly guided by mātauranga Māori, and because we have an explicit aim of reducing inequities and enabling Māori advancement, our contribution adds a supportive voice to the testimony of Māori whānau and Māori organisations and demonstrates how obligations under the Te Tiriti o Waitangi can be fulfilled to the benefit of all involved.
As our research develops, we will continue learning and interweaving Western and Indigenous approaches to maximise co-benefits. We recognise that from an Indigenous perspective, ‘home’ is ‘a place of belonging, safety, connection and acceptance [… .] to people and communities … [not simply to] a physical location or dwelling’, a place of connection with tipuna (ancestors) and ‘spiritual safety’ (Boulton et al. 2022, p. 4). We are more explicitly beginning to explore the wellbeing benefits associated with alternative housing approaches that shift away from the stand-alone house and colonial ideals to more inclusive, collectively-oriented housing models that may better support the creation of ‘home’ in this wider sense. Some of these alternatives include co-housing, papakāinga, and other shared, multi-generational or socially-based tenure options. Shifting to embrace urban development derived from diverse cultural values to meet a range of housing and tenure needs is complex and contested. For Māori and Pasifika this shift needs to happen in a self-determined way that leads to more inclusive and equitable environments through both statutes and practices related to urban planning and housing. Some culturally responsive frameworks, processes and urban intensification standards exist (such as the Te Aranga Māori Design Principles in Auckland/Tāmaki Makaurau9 or The Ministry for the Environment/Manatū mō te Taiao (MfE)’s recently-created medium density design guide that incorporates Te Ao Māori).10 Yet more Indigenous-led research and innovation is needed to realise culturally responsive built environments; and more equitable policies and processes are needed to support the creation of high-quality home spaces in accessible, supportive neighbourhood environments (Olin et al. 2022).This however, is dependent on establishing more effective pathways for Māori and Pasifika peoples to enter and progress through the often long and highly westernised research career labyrinth that currently predominates in Aotearoa.
Conclusion
Ways to improve the quality of housing and highlight housing equity in relation to Māori and Pasifika are increasingly moving to address the cultural suitability of housing and neighbourhoods, led by these communities and their understandings of wellbeing and ‘home’. The concentration of Western approaches is increasingly being challenged by Indigenous approaches, participation and sharing of decision making. In times of rapid climate change there is increased openness to embracing and learning from Indigenous knowledge.
Growing manifestations of climate change are increasing the numbers of people facing extreme temperatures, with related health and physical risks of flooding, fires and landslips. In many cases, housing is inadequate to protect occupants and maintain good health and wellbeing in the long term. Raising the building standards of new and existing houses, while heeding the adaptations of Indigenous approaches, is essential for public health and done well, can also be an important part of climate mitigation and adaptation. He Kāinga Oranga’s research has contributed to greater recognition of the broad cultural, health, social, environmental and economic co-benefits of improving housing design and placement.
The size of these challenges to the public’s physical and mental wellbeing requires action at many levels with recognition of the potential for significant co-benefits (Baker et al. 2020). At the global level, the SDGs and the 2018 WHO Housing and Health Guidelines (World Health Organization 2018) provide a robust evidence base for coordinated international action, to which we are contributing as a WHO Coordinating Centre on Housing and Wellbeing. National-level organisations, central and city governments, iwi, hapu, Māori urban authorities and local communities will need to enact and support policies that provide incentives for building of quality, affordable, culturally-appropriate homes in the right places, in a timely way for households of all ethnicities. Interweaving Western and Indigenous approaches not only better reflects the make-up of New Zealand society in the twenty-first Century and the intention of Te Tiriti o Waitangi, it can lead to co-benefits that draw on the strengths of each approach and provide a more complete picture of the relationship between housing and urban environments, health and wellbeing. He Kāinga Oranga has contributed to this important work, but clearly more research with complementary knowledge exchange remains to be done.
Acknowledgements
We would like to gratefully acknowledge all the thousands of families and whānau who have willingly and generously contributed to our studies and the community groups we have partnered with, who have supported them. In the Insulation Study we would like to acknowledge Olivia James at Ōtara Health Inc; Jo Hunt at Ōpōtiki Trade Training; Pounamu Skelton and the New Plymouth Office of Te Puni Kōkiri; Johnina Stymes and Alberta Hunga at Te Iwi o Rakaipaaka; Elyria Fau at Te Wāhine o Kahungungu.; Gail Chalmers and Ana Apatu at the Porirua Housing Action Group; Linda Wall, June Robinson, and the Rata Branch of the Māori Women’s Welfare League; Ann Currie at Crown Public Health; the interviewers and retrofit teams; and all the householders who took part in our study. We are grateful to our community coordinators the late Ruth Nepia, Pounamu Skelton, and Jo-Ani Robinson. In the Heating Study we would like to acknowledge our community partners in Porirua (Porirua Health Plus), in the Hutt Valley (Tū Kotahi Māori Asthma Trust, Community Planners, and Mid-Valley PHO, and Waiwhetu Marae), in Christchurch (Community and Public Health and Pacific Trust Canterbury), in Dunedin (Otago Asthma Society), and Sumaria Beaton in Bluff (Te Runaka o Awarua) and in 2005 Te Ropu Awhina (Te Amorangi Richmond). A full list is available on www.wnmeds.ac.nz/healthyhousing.html. In the Housing Injury Intervention Study, we would like to acknowledge Anaru Marshall and WISE Better Homes in Taranaki and builders Josh and Emily Shanley of New Plymouth. Wellington’s Sustainability Trust have supported us through all our projects.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Funding Statement
This work has been supported since 1991 by multiple grants: recent programme grants from Health Research Council of New Zealand are He Kāinga Oranga: Research to maximise the health and wellbeing from housing (HRC 20/683); the Ministry of Business, Innovation and Employment Endeavour Research Programmes: Public housing and urban gegeneration: Maximising wellbeing (UOOX2003); Housing children and youth: Ensuring Aotearoa’s future get the best start possible (UOOX1604) and the Marsden Fund Representation, Discourse and Reality: Eviction and its consequences (UOO1733).
Notes
Stats NZ Consumer price index: March 2022 quarter | Stats NZ HV calculations
Te Matapihi gives voice to the Māori housing sector, assisting individuals, whānau, hapū and iwi with housing policy, growth, resources and information.
The Housing Insulation and Health Study. https://www.youtube.com/watch?v =wbObl3tnleA&t = 45s. The Housing, Heating and Health Study, https://www.youtube.com/watch?v = U8EcY83W63U, https://www.healthyhousing.org.nz/news-events/science-healthier-home
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Amore K, Viggers H, Howden-Chapman P.. 2021. Severe housing deprivation in Aotearoa New Zealand, 2018 June 2021 update. Wellington: He Kāinga Oranga/Housing & Health Research Programme Department of Public Health University of Otago. [Google Scholar]
- Baker E, Pham NTA, Daniel L, Bentley R.. 2020. New evidence on mental health and housing affordability in cities: a quantile regression approach. Cities. 96(102455). doi: 10.1016/j.cities.2019.102455. [DOI] [Google Scholar]
- Baker M, Das D, Venugopal K, Howden-Chapman P.. 2008. Tuberculosis associated with household crowding in a developed country. Journal of Epidemiology Community Health. 62(8):715–721. [DOI] [PubMed] [Google Scholar]
- Baker M, Keall M, Lyn Au E, Howden-Chapman P.. 2007. Home is where the heart is – most of the time. New Zealand Medical Journal. 120:1264. [PubMed] [Google Scholar]
- Baker M, McNicholas A, Garrett MH, Jones N, Stewart J, Koberstein V, Lennon D.. 2000. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatric Infectious Disease Journal. 19(10):983–990. [DOI] [PubMed] [Google Scholar]
- Baker M, Telfar Barnard L, Kvalsvig A, Verrall A, Zhang J, Keall M, Wilson N, Wall T, Howden-Chapman P.. 2012. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. The Lancet. 379:1112–1119. [DOI] [PubMed] [Google Scholar]
- Baker M, Venugopal K, Howden-Chapman P.. 2011. Household crowding and tuberculosis. In: Braubach M, Jacobs DE, Ormandy D, editors. Environmental burden of disease associated with inadequate housing: a method guide to the quantification of health effects of selected housing risks in the WHO European region. Bonn: WHO Europe; p. 52–79. [Google Scholar]
- Beasley R, D'Souza W, Te Karu H, Fox C, Harper M, Robson B, Howden-Chapman P, Crane J, Burgess C, Woodman K, et al. 1993. Trial of an asthma action plan in the Maori community of the Wairarapa. New Zealand Medical Journal. 106(961):336–338. [PubMed] [Google Scholar]
- Bennett J, Howden-Chapman P, Chisholm E, Keall M, Baker MG.. 2016. Towards an agreed quality standard for rental housing: field testing of a New Zealand housing WOF tool. Australian and New Zealand Journal of Public Health. 40(5):405–411. [DOI] [PubMed] [Google Scholar]
- Bennett J, Moreland NJ, Zhang J, Crane J, Sika-Paotonu D, Carapetis J, Williamson DA, Baker MG.. 2022. Risk factors for group A streptococcal pharyngitis and skin infections: a case control study. The Lancet Regional Health - Western Pacific. 26(100507). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berghan J. 2021. Kaupapakāinga: the potential for Māori cohousing. Building Better Homes, Towns and Cities: Affordable Housing for Generations. Wellington: BBHTC. [Google Scholar]
- Bierre S, Bennett M, Howden-Chapman P.. 2015. Decent expectations? The interpretation of housing quality standards in tenancy tribunals in New Zealand. New Zealand Universities Law Review. 26(2):153–185. [Google Scholar]
- Blakely T, Tobias M, Robson B, Ajwani S, Bonne M, Woodward A.. 2005. Widening ethnic mortality disparities in New Zealand 1981-99. Social Science and Medicine. 61:2233–2251. [DOI] [PubMed] [Google Scholar]
- Boardman B. 2010. Fixing fuel poverty: challenges and solutions. London: Earthscan. [Google Scholar]
- Boulic M, Fjällström P, Phipps R, Cunningham M, Cleland D, Pierse N, Howden-Chapman P, Chapman R, Viggers H, Pollard A, the Housing and Health Team 2008. Cold homes in New Zealand – does increasing the heater capacity improve the indoor climate? Clean Air and Environmental Quality Journal. 42(3):23–29. [Google Scholar]
- Boulton A, Allport T, Kaiwai H, Harker R, Osborne GP.. 2022. Māori perceptions of ‘home’: Māori housing needs, wellbeing and policy. Kōtuitui Online. 1–12. doi: 10.1080/1177083X.2021.1920984. [DOI] [Google Scholar]
- Braubach M, Jacobs DE, Ormandy D, editors. 2011. Environmental burden of disease associated with inadequate housing: a method guide to the quantification of health effects of selected housing risks in the WHO European region. Geneva: World Health Organization Regional Office for Europe. [Google Scholar]
- Center for Transit-Oriented Development and Center for Neighborhood Technology . 2006. The affordability index: a new tool for measuring the true affordability of a housing choice. Washington: The Brookings Institution. [Google Scholar]
- Chapman R, Howden-Chapman P.. 2021. Does reframing urban policy around wellbeing support carbon mitigation? Special collection: urban systems for sustainability and health. Buildings and Cities. 2(1):688–99. [Google Scholar]
- Chapman R, Howden-Chapman P, Viggers H, O’Dea D, Kennedy M.. 2009. Retrofitting housing with insulation: a cost-benefit analysis of a randomised community trial. Journal of Epidemiology and Community Health. 63:271–277. [DOI] [PubMed] [Google Scholar]
- Chapman R, Preval N, Howden-Chapman P.. 2017. How economic analysis can contribute to understanding the links between housing and health. International Journal Environmental Research and Public Health. 14(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm E, Bierre S, Davies C, Howden-Chapman P.. 2021a. That house was a home’: qualitative evidence from New Zealand on the connections between rental housing eviction and poor health outcomes. Health Promotion Journal of Australia. doi: 10.1002/hpja.526. [DOI] [PubMed] [Google Scholar]
- Chisholm E, Howden-Chapman P, Fougere G.. 2020a. Tenants’ responses to substandard housing: hidden and invisible power and the failure of rental housing regulation. Housing, Theory and Society. 37(2):139–161. [Google Scholar]
- Chisholm E, Keall M, Bennett J, Marshall A, Telfar Barnard L, Thornley L, Howden-Chapman P.. 2019a. Why don’t owners improve their homes? Results from a survey following a housing warrant-of-fitness assessment for health and safety. Australian New Zealand Journal of Public Health. doi: 10.1111/1753-6405.12895. [DOI] [PubMed] [Google Scholar]
- Chisholm E, Pierse N, Davies C, Howden-Chapman P.. 2019b. Promoting health through housing improvements, education and advocacy: lessons from staff involved in Wellington’s healthy housing initiative. Health Promotion Journal of Australia. 31(1):7–15. [DOI] [PubMed] [Google Scholar]
- Chisholm E, Pierse N, Howden-Chapman P.. 2021a. Perceived benefits and risks of developing mixed communities in New Zealand: implementer perspectives. Urban Research & Practice. Advance Online Publication. doi: 10.1080/17535069.2020.1801831. [DOI] [Google Scholar]
- Chisholm E, Pierse N, Howden-Chapman P.. 2021b. What is a mixed-tenure community? views from New Zealand practitioners and implications for researchers. Urban Policy & Research. Advance Online Publication. doi: 10.1080/08111146.2020.1863780. [DOI] [Google Scholar]
- Chisholm E, Robertson O, Howden-Chapman P, Pierse N.. 2022. Does the proportion of public housing tenants in a community affect their wellbeing? Results from New Zealand – a retrospective cohort study using linked administrative data. Cities. 131:103916. doi: 10.1016/j.cities.2022.10916. [DOI] [Google Scholar]
- Clapham D, Foye C, Christian J.. 2018. The concept of subjective well-being in housing research. Housing, Theory and Society. 35(3):261–280. [Google Scholar]
- Crane J, Ellis I, Grimmet D, Lewis S, Fitzharris P.. 1998. A pilot study of the effect of mechanical ventilation and heat exchange on house-dust mites and Der p 1 in New Zealand homes. Allergy. 53:755–762. [DOI] [PubMed] [Google Scholar]
- Davie GS, Baker MG, Hales S, Carlin JB.. 2007. Trends and determinants of excess winter mortality in New Zealand: 1980 to 2000. BMC Public Health. 7:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davillas A, Burlinson A, Liu H-H.. 2022. Getting warmer: fuel poverty, objective and subjective health and well-being. Energy Economics. 106:105794. [Google Scholar]
- Davis P, Howden-Chapman P.. 1996. Translating research findings into health policy. Social Science and Medicine. 43(5):865–872. [DOI] [PubMed] [Google Scholar]
- Davison G, Ferris D, Pearson A, Shach R.. 2020. Investments with returns: a systematic literature review of health-focused housing interventions. Journal of Housing and the Built Environment. 35:829–845. [Google Scholar]
- Department for Communities and Local Government . 2006. A decent home: definition and guidance for implementation (update) In: Department of Communities and Local Government, editor. London. [Google Scholar]
- Douwes J, Howden-Chapman P.. 2011. Chapter 5, An overview of possible health effects from exposure to “leaky buildings”. The leaky building crisis: understanding the issues. Wellington: Thomson Reuters. p. 71–84. [Google Scholar]
- D'Souza W, Crane J, Burgess C, Te Karu H, Fox C, Harper M, Robson B, Howden-Chapman P, Crossland L, Woodman K, et al. 1994. Trial of a credit card asthma self-management plan. European Respiratory Journal. 7:1260–1265. [DOI] [PubMed] [Google Scholar]
- Escombe AR, Oeser CC, Gilman RH, Navincopa M, Ticona E, Pan W, Martínez C, Chacaltana J, Rodríguez R, Moore DA, et al. 2007. Natural ventilation for the prevention of airborne contagion. PLoS Med. 4(2):e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser B, Chun S, Ti P, Jiang T, Johnson E, Ombler JCM, Pierse N.. 2022. Post-housing first outcomes amongst a cohort of formerly homeless youth in Aotearoa New Zealand. Journal of the Royal Society of New Zealand. doi: 10.1080/03036758.03032022.02088572. [DOI] [Google Scholar]
- Fraser B, White M, Cook H, Chisholm E, Ombler J, Chun S, Tareha H, Pierse N.. 2021. Service usage of a cohort of formerly homeless women in Aotearoa New Zealand. SSM – Population Health. 15:100842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free S, Howden-Chapman P, Pierse N, Viggers H.. 2010. Housing heating and health study research team study team. 2010. More effective home heating reduce school absences for children with asthma? Journal of Epidemiology and Community Health. 64:379–386. [DOI] [PubMed] [Google Scholar]
- Fyfe C, Telfar Barnard L, Douwes J, Howden-Chapman P, Crane J.. 2022. Retrofitting home insulation reduces incidence and severity of chronic respiratory disease. Indoor Air. 32:e13101. doi: 10.1111/ina.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fyfe C, Telfar Barnard L, Howden-Chapman P, Douwes J.. 2020. Association between home insulation and hospital admission rates: retrospective cohort study using linked data from a national intervention programme. British Medical Journal. doi: 10.1136/bmj.m4571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnham R, Anderson S, Godwin D.. 2022. Intervening in the cycle of poverty, poor housing and poor health: the role of housing providers in enhancing tenants’ mental wellbeing. Journal of Housing and the Built Environment. 37(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie-Bennett J, Keall M, Baker MG, Howden-Chapman P.. 2013. Improving our nation’s health, safety and energy efficiency through measuring and applying basic housing standards: viewpoint article. New Zealand Medical Journal . 126(1379):74–85. [PubMed] [Google Scholar]
- Gillespie-Bennett J, Pierse N, Wickens K, Crane J, Howden-Chapman P.. 2011. The respiratory health effects of nitrogen dioxide in children with asthma. European Respiratory Journal. 38(2):303–309. [DOI] [PubMed] [Google Scholar]
- Gillespie-Bennett J, Pierse N, Wickens K, Crane J, Shields D, Nicholls S, Viggers H, Howden-Chapman P, Housing, Heating and Health Team . 2008. Sources of nitrogen dioxide (NO2) in New Zealand homes: findings from a community randomised controlled trial of heater substitution. Indoor Air. 18(6):521–528. [DOI] [PubMed] [Google Scholar]
- Grant L, Viggers H, Howden-Chapman P, editors. 2021. Improving buildings, cutting carbon. Wellington.: Steel Roberts Aotearoa. [Google Scholar]
- Gray JM, Howden-Chapman P, King B, Pene G.. 2008. Healthy housing for large households in New Zealand. Proceedings of 5th Warwick Healthy Housing Conference, March, Coventry, UK: University of Warwick.
- Haigh F, Kemp L, Bazeley P, et al. 2019. Developing a critical realist informed framework to explain how the human rights and social determinants of health relationship works. BMC Public Health. 19(1571). doi: 10.1186/s12889-12019-17760-12887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris R, Cormack D, Tobias M, Yeh L-C, Talamaivao N, Minster J, Timutimu R.. 2012. The pervasive effects of racism: experiences of racial discrimination in New Zealand over time and associations with multiple health domains. Social Science & Medicine. 74:408–415. [DOI] [PubMed] [Google Scholar]
- Hinson S, Bolton P.. 2022. Fuel poverty. London: House of Commons Library. https://researchbriefings.files.parliament.uk/documents/CBP-8730/CBP-8730.pdf. [Google Scholar]
- Homes (Fitness for Human Habitation) Act 2018 . Renting Homes (Wales) Act 2016, Renting Homes (Fitness for Human Habitation) (Wales) Regs 2022. HMSO, UK.
- Housing Health and Safety Rating System (England) 2006 . and Housing Health and Safety Rating System (Wales) 2006, applying Part 1 Housing Act 2004. HMSO, UK.
- Howden-Chapman P. 2021. Te Tapeke Fair Futures panel. 2021. Spotlight on Housing. https://www.royalsociety.org.nz/what-we-do/our-expert-advice/all-expert-advice-papers/spotlight-on-housing/.
- Howden-Chapman P, Bennett J, Edwards R, Jacobs D, Nathan K, Ormandy D.. 2023. Review of the impact of housing quality on inequalities in health and well-being. Annual Review of Public Health. 44:10.1-10.22. 10.1146/annurev-publhealth071521-111836. [DOI] [PubMed] [Google Scholar]
- Howden-Chapman P, Carroll P, editors. 2004. Housing and health: research, policy and innovation. Wellington: SteeleRoberts. [Google Scholar]
- Howden-Chapman P, Crane J, Matheson A, Viggers H, Cunningham M, Blakely T, O'Dea D, Cunningham C, Woodward A, Saville-Smith K, et al. 2005. Retrofitting houses with insulation to reduce health inequalities: aims and methods of a clustered, randomised trial in community settings. Social Science and Medicine. 61:2600–2610. [DOI] [PubMed] [Google Scholar]
- Howden-Chapman P, Fyfe C, Nathan K, Keall M, Riggs L, Pierse N.. 2021. The effects of housing on health and well-being in Aotearoa New Zealand. New Zealand Population Review. 47:16–32. [Google Scholar]
- Howden-Chapman P, Gatzweiller F, Luginaah I, Cooper R, editors. 2023. Cities under COVID-19: a systems approach. Beijing.: Springer Press. [Google Scholar]
- Howden-Chapman P, Matheson A, Viggers H, Crane J, Cunningham M, Blakely T, O'Dea D, Cunningham C, Woodward A, Saville-Smith K, et al. 2007. Retrofitting houses with insulation to reduce health inequalities: results of a clustered, randomised trial in a community setting. British Medical Journal. 334:460–464.17324975 [Google Scholar]
- Howden-Chapman P, Pene G, Crane J, Green R, Iupati L, Prior I, Teao I.. 2000. Open houses and closed rooms: Tokelau housing in New Zealand. Health Education and Behavior. 27(3):351–362. [DOI] [PubMed] [Google Scholar]
- Howden-Chapman P, Pierse N, Nicholls S, Gillespie-Bennett J, Viggers H, Cunningham M, Phipps R, Boulic M, Fjällström P, Free S, et al. 2008. Effects of improved home heating on asthma in community dwelling children: randomised community study. British Medical Journal. 337:852–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden-Chapman P, Roebbel N, Chisholm E.. 2017a. Setting housing standards to improve global health. International Journal of Environmental Research and Public Health. 14(12):1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden-Chapman P, Ruthe C, Crichton S.. 2011. Habitable houses: lessons learned? The leaky building crisis: understanding the issues. Wellington: Thomson Reuters. p. 303–315. [Google Scholar]
- Howden-Chapman P, Signal L, Crane J.. 1999. Housing and health in older people; ageing in place. Social Policy Journal of New Zealand. 13:14–30. [Google Scholar]
- Howden-Chapman P, Siri J, Chisholm E, Chapman R, Doll CNH, Capon A. . 2017b. SDG3: ensure healthy lives and promote well-being for all at all ages. In: Griggs DJ, Nilsson M, Stevance A, editors. A guide to SDG interactions: from science to implementation. Paris: International Council for Science; p. 84–126. [Google Scholar]
- Howden-Chapman P, Viggers H, Chapman R, O'Dea D, Free S, O'Sullivan K.. 2009. Warm homes: drivers of the demand for heating in the residential sector in New Zealand. Energy Policy. 37(9):3387–3399. [Google Scholar]
- Howden-Chapman P, Viggers H, Chapman R, O'Sullivan K, Telfar Barnard L, Lloyd B.. 2012. Tackling cold housing and fuel poverty in New Zealand: a review of policies, research, and health impacts. Energy Policy. 49:134–142. [Google Scholar]
- Howden-Chapman P, Woodward A, editors. 2001. Health of pacific societies; the life and works of Dr Ian Prior. Wellington: Steele Roberts. [Google Scholar]
- Huntsman J, Hooper A.. 1997. Tokelau: an historical ethnography. Auckland: Auckland University Press. [Google Scholar]
- Ingham TR, Keall M, Jones B, Aldridge DRT, Dowell A, Davies C, Crane J, Draper JB, Bailey LO, Viggers H, et al. 2019. Damp mouldy housing and early childhood hospital admissions for acute respiratory infection: a case control study. Thorax. 74:849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine of the National Academies . 2004. Damp indoor spaces and health. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- International Science Council and BBC Story Works February . 2022. The Science of a Healthier Home.
- Israel BA, Schulz A, Parker JA, Becker AB.. 1998. Review of community-based research: assessing partnership approaches to improve public health. Annual Review of Public Health. 19:173–202. [DOI] [PubMed] [Google Scholar]
- Jaine R, Baker M, Kamalesh V.. 2011. Acute rheumatic fever associated with household crowding in a developed country. The Pediatric Infectious Disease Journal. 30(4):1–5. [DOI] [PubMed] [Google Scholar]
- Joint Center for Housing Studies of Harvard University . 2021. The State of the Nation’s Housing.
- Karvonen A, Taubel M, Shorter C, Pierse N, Douwes J, Pekkanen J, Hyvarinen A, Howden-Chapman P, Stanley T, Barnes P, et al. 2019. Moisture damage related fungal microbiota and new-onset wheezing in children. Allergy. https://www.julkari.fi/handle/10024/1384.77. [Google Scholar]
- Keall MD, Baker M, Howden-Chapman P, Cunningham M, Ormandy D.. 2010. Assessing health-related aspects of housing quality. Journal of Epidemiology and Community Health. 64(9):765–771. [DOI] [PubMed] [Google Scholar]
- Keall MD, Crane J, Baker MG, Wickens K, Howden-Chapman P, Cunningham M.. 2012. A measure for quantifying the impact of housing quality on respiratory health: a cross-sectional study. Environmental Health. 11(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keall MD, Guria J, Howden-Chapman P, Baker MG.. 2011. Estimation of the social costs of home injury: a comparison with estimates for road injury. Accident Analysis and Prevention. 43(3):998–1002. [DOI] [PubMed] [Google Scholar]
- Keall MD, Howden-Chapman P, Baker MG, Kamalesh V, Cunningham M, Cunningham C, Guria J, Draper R, Skelton P.. 2013. Formulating a programme of repairs to structural home injury hazards in New Zealand. Accident Analysis & Prevention. 57(0):124–130. [DOI] [PubMed] [Google Scholar]
- Keall MD, Pierse N, Howden-Chapman P, Cunningham C, Cunningham M, Guria J, Baker MG.. 2015. Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: a cluster-randomised controlled trial. The Lancet. 385(9964):231–238. [DOI] [PubMed] [Google Scholar]
- Keall MD, Tupara H, Pierse N, Wilkie M, Baker MG, Howden-Chapman P, Cunningham C.. 2021. Home modifications to prevent home fall injuries in houses with Māori occupants (MHIPI): a randomised controlled trial. The Lancet Public Health. 6(9):e631–e640. [DOI] [PubMed] [Google Scholar]
- Kearns A, Parkes A.. 2003. Living in and leaving poor neighbourhood conditions in England. Housing Studies. 18(6):49–65. [Google Scholar]
- Kunitz SJ. 2007. The health of populations: general theories and particular realities. New York: Oxford University Press. [Google Scholar]
- Lawson-Te Aho K, Fariu-Ariki P, Ombler J, Aspinall C, Howden-Chapman P, Pierse N.. 2019. A principles framework for taking action on Māori/indigenous homelessness in Aotearoa/New Zealand. SSM-Population Health. 8(100450). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan-Riley A. 2022. Housing and wellbeing for Whānau Māori [PhD]. Wellington: University of Otago. [Google Scholar]
- Macfarlane A, Macfarlane S.. 2019. Listen to culture: Māori scholars’ plea to researchers. Journal of the Royal Society of New Zealand. 49:48–57. [Google Scholar]
- Mann S, Baker M, Hales S, Kamalesh V, Barnard LT, Zhang J, Howden-Chapman P.. 2009. Excess winter cardiovascular mortality nnd morbidity in New Zealand is seen in all disease subcategories. Heart, Lung and Circulation. 18(3):S256. [Google Scholar]
- McKay K, Eggleton K.. 2022. A place-based evaluation of a healthy homes initiative. Health Promotion Journal of Australia. 1–6. doi: 10.1002/hpja.609. [DOI] [PubMed] [Google Scholar]
- Ministry of Housing CLG . 2018. Greater protection for renters thanks to plans to tighten tenant safety. https://www.gov.uk/government/news/greater-protection-for-renters-thanks-to-plans-to-tighten-tenant-safety.
- Morawska L, Milton DK.. 2020. It Is time to address airborne transmission of Coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases. 71(9):2311–2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan K, Robertson O, Atatoa-Carr P, Howden-Chapman P, Pierse N.. 2022. Residential mobility and potentially avoidable hospitalisations in a population-based cohort of New Zealand children. Journal of Epidemiology and Community Health. 76:606–612. [DOI] [PubMed] [Google Scholar]
- Nathan K, Robertson O, Atatoa-Carr P, Howden-Chapman P, Pierse P.. 2019. Residential mobility and socioemotional and behavioural difficulties in a preschool population cohort of New Zealand children. Journal of Epidemiology and Community Health. 73:947–953. [DOI] [PubMed] [Google Scholar]
- New Zealand Government . 2017. Healthy Homes Guarantee Act.
- New Zealand Ministry of Social Development . 2022. Winter energy payment. In: ministry of social development, editor. Wellington: MSD. [Google Scholar]
- Nilsson M, Griggs D, McCollum D, Chisholm E, Howden-Chapman P, Messerli P, Neumann B, Visbeck Stafford-Smith M.. 2018. Mapping interactions between the sustainable development goals: lessons learned and ways forward. Sustainability Science. 6:1499–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olin CV, Howden-Chapman P, Berghan J, Thompson-Fawcett M, Ivory V, Witten K, Duncan S, Ka’ai T, Yates A, O’Sullivan K, et al. 2022. Inclusive and collective urban home spaces: the future of housing in Aotearoa New Zealand. Wellbeing, Space and Society. 3(100080). doi: 10.1016/j.wss.2022.100080. [DOI] [Google Scholar]
- Oliver J, Foster T, Kvalsvig A, Williamson DA, Baker MG, Pierse N.. 2018. Risk of rehospitalisation and death for vulnerable New Zealand children. Archives of Disease in Childhood. 103(4):327–334. [DOI] [PubMed] [Google Scholar]
- Ombler J, Ombler P, Nelson J, Howden-Chapman P, Lawson Te-Aho K, Fariu-Ariki P, Cook H.. 2017. Ending homelessness in New Zealand: housing first research programme. Parity. 30(10):5–7. [Google Scholar]
- Oreszczyn T, Ridley I, Hong SH, Wilkinson P, Warm Front Study Group . 2006. Mould and winter indoor relative humidity in low income households in England. Indoor and Built Environment. 15(2):125–135. [Google Scholar]
- Osman L, Ayres J, Garden C, Reglitz K, Lyon J.. 2010. A randomised trial of home energy efficiency improvement in the homes of elderly COPD patients. European Respiratory Journal. 35:303–309. [DOI] [PubMed] [Google Scholar]
- Osman L, Ayres J, Garden C, Reglitz K, Lyon J, Douglas J.. 2008. Home warmth and health status of COPD patients. European Journal of Public Health. 18(4):399–405. [DOI] [PubMed] [Google Scholar]
- O'Sullivan K, Howden-Chapman P, Fougere G.. 2011. Making the connection: the relationship between fuel poverty, electricity disconnection, and prepayment metering. Energy Policy. 39:733–741. [Google Scholar]
- O'Sullivan KC, Howden-Chapman P, Fougere G.. 2015. Fuel poverty, policy, and equity in New Zealand: the promise of prepayment metering. Energy Research & Social Science. 7:99–107. [Google Scholar]
- Pene G, Howden-Chapman PL, Peita M, Viggers H, Gray J.. 2009a. Living the Tokelauan Way in New Zealand: teenager’s perspectives on extended-family living and the evaluation of a purpose-built, extended family house. Wellington: Families Commission. [Google Scholar]
- Pene G, Peita M, Howden-Chapman P.. 2009b. Living the Tokelauan way in New Zealand. Social Policy Journal. 35:79–92. [Google Scholar]
- Penny G Whakawhanaungatanga Māori Wellbeing Model and Research Framework. Kotuitui, in preparation. Final list of co-authors not yet available
- Pierse N, Arnold R, Keall M, Howden-Chapman P, Crane J, Cunningham M, Heating Housing and Health Study Group . 2013. Modeling the effects of low indoor temperatures on the lung function of children with asthma. Journal of Epidemiology and Community Health. 67(11):918–925. doi: 10.1136/jech-2013-202632. [DOI] [PubMed] [Google Scholar]
- Pierse N, Johnson E, Riis L, Watson N.. 2022. Healthy homes initiative: three year outcomes evaluation Wellington, Motu. https://www.tewhatuora.govt.nz/about-us/publications/heathy-homes-initiative-three-year-outcomes-evaluation/.
- Pierse N, Ombler J, White M, Aspinall C, McMinn C, Atatoa-Carr P, Nelson J, Hawke K, Fraser B, Cook H, Howden-Chapman P.. 2019a. Service usage by a New Zealand housing first cohort prior to being housed. SSM - Population Health. 8(100432). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierse N, White M, Ombler J, Davies C, Chisholm C, Howden-Chapman P.. 2020. Well homes initiative: a home-based initiative to address housing-related ill health. Health Education and Behavior; p. 1–9. [DOI] [PubMed] [Google Scholar]
- Pierse N, White M, Riggs L.. 2019b. Healthy homes initiative outcomes evaluation service. In: Initial analysis of health outcomes (interim report). Wellington: Ministry of Health. [Google Scholar]
- Pōmare E, Keefe-Ormsby V, Ormsby C, et al. 1995. Hauora; Maori standards of health:III A study of the years 1970-1991. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare Māori Health Research Centre. [Google Scholar]
- Preval N, Keall M, Telfar-Barnard L, Grimes A, Howden-Chapman P.. 2017. Impact of improved insulation and heating on mortality risk of older cohort members with prior cardiovascular or respiratory hospitalisations. British Medical Journal Open. 7(11):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangiwhetu L, Pierse N, Howden-Chapman P.. 2020. Public housing and well-being: evaluation frameworks to influence policy. Health Education and Behavior. 47(6):825–835. [DOI] [PubMed] [Google Scholar]
- Reid P, Paine S-J, Curtis E, Jones R, Anderson A, Willing E, Harwood M.. 2017. Achieving health equity in Aotearoa: strengthening responsiveness to Māori in health research. New Zealand Medical Journal. 130:96–103. [PubMed] [Google Scholar]
- Riggs L, Keall M, Howden-Chapman P, Baker MG.. 2021. The environmental burden of disease from unsafe and substandard housing conditions in New Zealand: assessing the public sector costs. Bulletin of World Health Organization. 1(4):259–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley RL, Mills CC, Nyka W, Weinstock N, Storey PB, Sultan LU, Riley MC, Wells WF.. 1995. Aerial dissemination of pulmonary tuberculosis. a two-year study of contagion in a tuberculosis ward. American Journal of Epidemiology. 142(1):3–14. [DOI] [PubMed] [Google Scholar]
- Robson B, Harris R, editors. 2007. Hauora: Maori standards of health IV. A study of the years 2000-2005. Wellington: Te Ropu Rangahau Hauora a Eru Pōmare. [Google Scholar]
- Rolfe S, Garnham L.. 2020. Neighbourhood impacts on wellbeing: investigating the role of housing among low income tenants. Social Inclusion (Special Issue). 8(3):102–112. [Google Scholar]
- Rolfe S, Garnham L, Godwin J, Anderson I, Seaman P, Donaldson C.. 2020. Housing as a social determinant of health and wellbeing: developing an empirically-informed realist theoretical framework. BMC Public Health. 20(1138). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan L, Campbell N.. 2012. Spreading the Net: the multiple benefits of energy efficiency improvements. Paris: IEA. [Google Scholar]
- Ryks J, Howden-Chapman P, Robson B, Stuart K, Waa A.. 2014. Māori participation in urban development: challenges and opportunities for indigenous people in Aotearoa New Zealand. Lincoln Planning Review. 6(1-2):4–17. [Google Scholar]
- Sallis JF, Cerin E, Conway TL, Adams MA, Frank LD, Pratt M, Owen N, et al. 2016. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. The Lancet. 387(10034):2207–2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe RA, Taylor T, Fleming LE, Morrissey K, Morris G.. 2018. Making the case for “whole system” approaches: integrating public health and housing. International Journal of Environmental Research and Public Health. 15(11):2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw C, Boulic M, Longley I, Mitchell T, Pierse N.. 2020. The association between indoor and outdoor NO2 levels: a case study in 50 residences in an urban neighbourhood in New Zealand. Sustainable Cities and Society. 56:102093. [Google Scholar]
- Shaw M. 2004. Housing and public health. Annual Review of Public Health. 25:397–418. [DOI] [PubMed] [Google Scholar]
- Shorter C, Crane J, Barnes P, Kang J, Honeywell C, Robertson O, O’Sullivan K, Telfar-Barnard L, Pierse N, Howden-Chapman P.. 2022. The cost of achieving healthy temperatures in children’s bedrooms: evidence from New Zealand. Energy Policy. 164:112861. [Google Scholar]
- Shorter C, Crane J, Wickens K, Pierse N, Stanley T, Barnes P, Kang J, Howden-Chapman P, Wellington Region General Practitioner Research Network . 2018. Indoor visible mold and mold odor are associated with new onset wheezing in a dose-dependent manner. Indoor Air. 1(1):6–15. [DOI] [PubMed] [Google Scholar]
- Stuart K, Thompson-Fawcett M, editors. 2010. Tāone Tupu Ora: indigenous knowledge & sustainable urban design. Wellington: Steele Roberts. [Google Scholar]
- Teariki MA. 2017. Housing and health of Kiribati migrants living in New Zealand. International Journal of Environmental Research and Public Health. 14(10):1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfar-Barnard L, Bennett J, Howden-Chapman P, Jacobs DE, Ormandy D, Cutler-Welsh M, Baker MG, Keall M.. 2017. Measuring the effect of housing quality interventions: the case of the New Zealand “rental warrant of fitness”. International Journal of Environmental Research and Public Health. 4:1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfar-Barnard L, Bennett J, Robinson A, Hailes A, Ombler J, Howden-Chapman P.. 2019. Evidence base for a housing warrant of fitness. SAGE Open Medicine. 7:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfar Barnard LF, Baker MG, Hales S, Howden-Chapman PL.. 2008. Excess winter morbidity and mortality, housing, and socio-economic status. Reviews on Environmental Health. 23(3):1–22. [DOI] [PubMed] [Google Scholar]
- Te Rōpü Rangahau Hauora a Eru Pōmare . 2007. Hauora IV: Maori standards of health. Wellington: Ministry of Health. [Google Scholar]
- Thom R, Grimes A.. 2022. Land loss and the intergenerational transmission of wellbeing: the experience of iwi in aotearoa New Zealand. Social Science & Medicine. 296(114804). [DOI] [PubMed] [Google Scholar]
- Tiatia R, Howden-Chapman P, Robson B, Baker M, Brown D, Davies C, McLean M, Laing P, Sung Y, Sim D, et al. 2016. Household crowding and rheumatic fever study: technical report funded by the Health Research Council of New Zealand and the Ministry of Health. Wellington: He Kāinga Oranga/Housing and Health Research Programme, University of Otago, Wellington. [Google Scholar]
- Toy-Cronin B, Bierre S.. 2022. Sustaining tenancies or swift evictions: rent arrears in the tenancy tribunal. Victoria University of Wellington Law Review. 53:105–128. [Google Scholar]
- United States Environmental Protection Agency . 2022. Indoor air quality (IAQ). Washington, DC: USEPA. [Google Scholar]
- Ürge-Vorsatz D, Chapman R.. 2021. Chapter Two, 1.5°C of global warming: can we still get there? insights from the urban development sector. In: Grant L, Viggers H, Howden-Chapman P, editors. Improving buildings, cutting carbon. Wellington: Steele Roberts; p. 17–25. [Google Scholar]
- Ürge-Vorsatz D, Herrero ST, Dubash NK, Lecocq F.. 2014. Measuring the co-benefits of climate change mitigation. Annual Review of Environment and Resources. 39:549–582. [Google Scholar]
- Viggers H, Amore K, Howden-Chapman P.. 2021. Housing that lacks basic amenities in Aotearoa New Zealand: a supplement to the 2018 Census Estimate of Severe Housing Deprivation commissioned by Te Tūāpapa Kura Kāinga-Ministry of Housing and Urban Development. He Kāinga Oranga, Housing and Health Research Programme, University of Otago, Wellington, www.healthyhousing.org.nz.
- Viggers H, Howden-Chapman P, Ingham T, Chapman R, Pene G, Davies C, Currie A, Pierse N, Wilson H, Zhang J, et al. 2013. Warm homes for older people: aims and methods of a randomised community-based trial for people with COPD. BMC Public Health. 13(176):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viggers H, Ingham T, Chapman R, Crane J, Currie A, Davies C, Keall M, Pierse N, Howden-Chapman P. RCT: winter heating vouchers did not reduce COPD exacerbations, may have reduced mortality. Submitted.
- Walker R, Barcham M.. 2010. Indigenous-inclusive citizenship: the city and social housing in Canada, New Zealand, and Australia. Environment and Planning A. 42(2):314–331. doi: 10.1068/a41314. [DOI] [Google Scholar]
- Werna E, Tan D, Howden-Chapman P, Siri J.. 2020. As safe as houses? Why standards for urban development matter. Cities & Health. 6:2, 404–417. doi: 10.1080/23748834.2020.1747826. [DOI] [Google Scholar]
- World Health Organization . 2009a. Guidelines for indoor Air quality: dampness and mould. Copenhagen: WHO Europe. [PubMed] [Google Scholar]
- World Health Organization . 2009b. Natural ventilation for infection control in health-care settings. Geneva: WHO. [PubMed] [Google Scholar]
- World Health Organization . 2011. Health in the green economy: health co-benefits of climate change mitigation – housing sector. Geneva: World Health Organization. [Google Scholar]
- World Health Organization . 2018. Housing and health guidelines. Geneva: WHO. [Google Scholar]