Abstract
Objective:
To investigate unmet needs for HIV ancillary care services by healthcare coverage type and Ryan White HIV/AIDS Program (RWHAP) assistance among adults with HIV.
Design:
We analyzed data using the 2017–2019 cycles of the CDC Medical Monitoring Project, an annual, cross-sectional study designed to produce nationally representative estimates of characteristics among adults with diagnosed HIV.
Methods:
Unmet need was defined as needing, but not receiving, one or more HIV ancillary care services. We estimated prevalence ratios (PRs) and 95% confidence intervals (CIs) using predicted marginal means to examine associations between healthcare coverage type and unmet needs for HIV ancillary care services, adjusting for age. Associations were stratified by receipt of RWHAP assistance.
Results:
Unmet needs for HIV ancillary care services were highest among uninsured persons (58.7%) and lowest among those with private insurance living with at least 400% of the federal poverty level (FPL; 21.7%). Uninsured persons who received RWHAP assistance were less likely than those who did not receive RWHAP assistance to have unmet needs for HIV clinical support services (aPR: 0.21; 95% CI: 0.16–0.28) and other medical services (aPR: 0.75;95% CI: 0.59–0.96), but not subsistence services (aPR: 0.97; 95% CI: 0.74–1.27). Unmet needs for other medical services and subsistence services did not differ by RWHAP assistance among those with Medicaid, Medicare, or other healthcare coverage.
Conclusions:
RWHAP helped reduce some needs for uninsured persons. However, with growing socioeconomic inequities following the coronavirus disease 2019 pandemic, expanding access to needed services for all people with HIV could improve key outcomes.
Keywords: ancillary care services, healthcare coverage, Ryan White HIV/AIDS Program, unmet needs
Graphical abstract
Introduction
Viral suppression is vital for the health and well being of people with HIV (PWH), as well as for preventing HIV transmission [1]. HIV care engagement and antiretroviral therapy (ART) adherence are strongly associated with maintaining viral suppression [2,3]. However, there are barriers to each that could prevent people from reaching viral suppression, including structural factors, such as access to HIV care services and payment of services [4]. In addition, support services that address social determinants of health play an essential role for the health and well being of PWH [5]. The U.S. HIV National HIV/AIDS Strategic Plan (NHAS) is a national roadmap for ending the HIV epidemic. A key area of focus in NHAS is increasing retention in care and ART adherence, and thus viral suppression, among PWH – with a particular emphasis on health equity and reducing disparities in treatment outcomes among those disproportionately affected by HIV [6].
A large percentage of PWH experience co-occurring social and medical conditions [7–12] that could complicate HIV care and management, which could further prevent PWH from engaging in care and maintaining viral suppression. HIV ancillary care services are those that support retention in HIV care and viral suppression among PWH, especially people who have complex medical needs [7,12,13]. These services are not robustly covered by traditional healthcare coverage plans [14] and include HIV clinical support services, such as case management; other medical services, such as dental care and mental health services; and subsistence services, such as transportation assistance and assistance with food and shelter [7,12]. The Ryan White HIV/AIDS Program (RWHAP) and its AIDS Drug Assistance Program (ADAP) funds jurisdictions and local community-based organizations to provide comprehensive HIV care, support services, medications, and healthcare coverage assistance to low-income PWH [15,16]. The RWHAP plays an important role in the national public health response to HIV; yet, unmet needs for HIV ancillary care services still persist and are associated with adverse HIV care continuum outcomes [4].
Healthcare coverage can also support access to care, but the healthcare coverage landscape among PWH in the United States is complex. PWH obtain coverage for healthcare services through a variety of sources, each having a different set of eligibility requirements and coverage of services. Differences in eligibility requirements and service coverage result in inherent differences in demographic characteristics and social determinants of health by healthcare coverage type [17]. A plurality of PWH rely on Medicaid, a large percentage of whom also rely on Medicare [17]. Although a large percentage of PWH have some source of healthcare coverage, many remain without coverage, particularly those living in states that have not elected to expand their Medicaid programs [17]. More than half of adults with diagnosed HIV rely on the RWHAP for access to outpatient medical and support services, coverage of medications, or healthcare coverage assistance [7,12]. Many of these services are not covered by traditional health insurance or coverage plans.
Across all coverage types, those who received support through the RWHAP were more likely to be virally suppressed, demonstrating the important role of the RWHAP in improving outcomes among PWH [17]. Given that access to HIV ancillary care services affects HIV clinical outcomes [4], understanding disparities in unmet needs for ancillary care services by healthcare coverage – and how RWHAP assistance might contribute to closing gaps in these disparities – could help in addressing national HIV care and treatment goals. However, national estimates of these unmet needs are lacking.
We used nationally representative data from the CDC Medical Monitoring Project (MMP) to investigate differences in unmet needs for ancillary care services by healthcare coverage type among adults with diagnosed HIV. To further explore the role of the RWHAP in addressing unmet needs, we also examined differences in unmet needs by receipt of RWHAP assistance within each healthcare coverage type.
Methods
Population
MMP is a complex sample survey conducted annually to produce nationally representative estimates of behavioral and clinical characteristics among adults with diagnosed HIV in the United States. During the 2017–2019 MMP cycles, MMP used a two-stage sampling design. First, 16 states and one territory were sampled from all states in the United States, the District of Columbia, and Puerto Rico. Next, a simple random sample of persons aged ≥18 years with diagnosed HIV was selected annually for each jurisdiction from the National HIV Surveillance System (NHSS), a census of persons with diagnosed HIV in the United States. Data on demographic, behavioral, and clinical characteristics were collected through face-to-face or phone interviews. Medical records were abstracted for interviewed participants who received HIV care during the previous 2 years. MMP is conducted as a part of routine surveillance and is considered non-research. Participating jurisdictions obtained institutional review board approval for data collection as needed and informed consent was obtained from all participants.
All sampled jurisdictions participated in MMP. Data were collected from June to May for each of the cycle years during 2017–2019; annual response rates for sampled persons ranged from 45% to 46%. Jurisdictions included in the analysis represented more than 70% of all persons living with diagnosed HIV in the United States by the end of 2019 [18].
Measures
Demographic characteristics and social determinants of health – including age and healthcare coverage type – as well as need for and receipt of ancillary care services were obtained through participant interviews.
Need for, and receipt of, ancillary care services was assessed through self-report and was based on the past 12 months. Ancillary care services were categorized into three domains: HIV clinical support services, other medical care services, and subsistence services. HIV clinical support services included HIV case management, adherence support services, HIV peer support, and patient navigation services. Other medical services included dental care, mental health services, and drug or alcohol counseling or treatment. Subsistence services included those through the Supplemental Nutrition Assistance Program (SNAP) or the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), transportation assistance, meal or food services, and shelter or housing services. Unmet need for a particular ancillary care service was defined as needing, but not receiving, that service.
Healthcare coverage was also assessed through self-report and was based on the past 12 months. Because participants could indicate having more than one coverage type (either simultaneously or multiple types over 12 months), healthcare coverage was categorized based on a hierarchy as follows: any private; Medicaid, including those also covered through Medicare; Medicare only; other public coverage, such as Tricare/CHAMPUS, Veteran’s Administration, or city/county coverage; and uninsured.
All coverage groups were relatively homogeneous with respect to poverty, with a vast majority falling below 400% of the federal poverty level (FPL), except for persons who received any private healthcare coverage (Appendix Figure, Supplemental Digital Content, http://links.lww.com/QAD/C462). Those with private coverage encompassed both relatively higher income people who received employer-based coverage and those with lower or moderate incomes who purchased individual private insurance including through the Affordable Care Act (ACA) Marketplace or for whom the RWHAP (including ADAP) purchased healthcare coverage [17]. Given the variability with respect to poverty level within this group, the private healthcare coverage group was further split into those living at less than 400% of the FPL and those living at 400% or more of the FPL. In addition to coverage, people were classified by whether they reported receiving assistance through the RWHAP or ADAP (’RWHAP assistance’).
Statistical analysis
Among all adults with diagnosed HIV with information on healthcare coverage (N = 12 273), we examined the percentage of persons who experienced 0, 1, 2, and 3 or more total unmet needs for ancillary care services, overall and by healthcare coverage type. We examined associations between healthcare coverage type and experiencing at least one unmet need for any ancillary care service, as well as unmet needs for HIV clinical support services, other medical services, and subsistence services. To investigate whether the RWHAP may have played a role in addressing unmet needs, we also assessed differences in unmet needs by receipt of RWHAP assistance within each healthcare coverage type.
We reported weighted percentages and 95% confidence intervals (CIs) for all characteristics. Differences between categorical variables were assessed using Rao-Scott chi-square tests. In addition, prevalence ratios with predicted marginal means were used to quantify differences between groups; associations were adjusted for age, which was presumed a priori to be a potential confounder (P<0.05). Data were weighted to adjust for person non-response and post-stratified to known population totals by age, race/ethnicity, and sex from NHSS. All analyses were conducted using SAS survey procedures and SAS-callable SUDAAN (SAS Institute Inc., Cary, North Carolina, USA).
Results
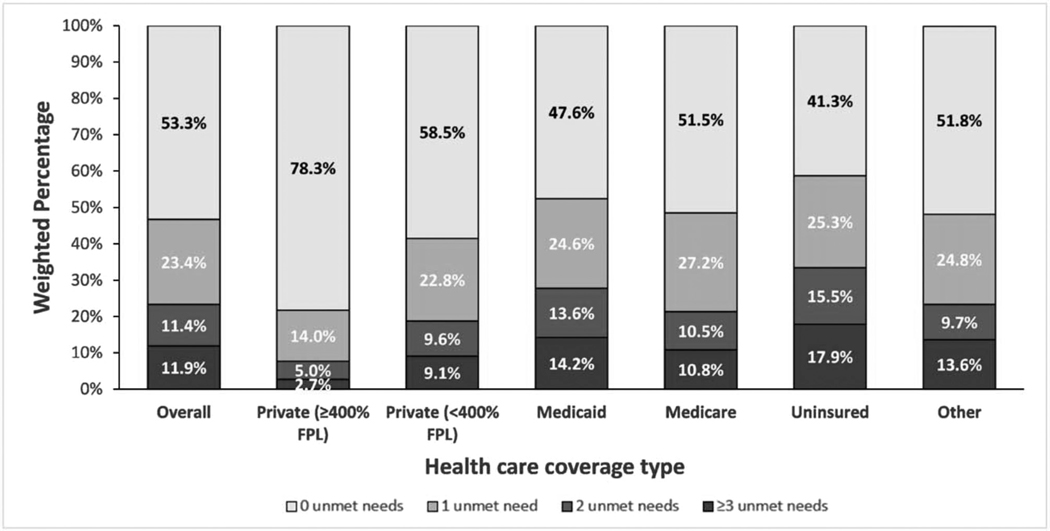
Nearly half (46.7%) of adults with diagnosed HIV had 1 or more unmet needs for ancillary care services; 23.4% reported 1 unmet need, 11.4% reported 2 unmet needs, and 11.9% reported 3 or more unmet needs (Fig. 1). Prevalence of unmet needs differed by healthcare coverage type, with any unmet need being lowest among those with private coverage living at 400% or more of the FPL (21.7%) and the highest among those who were uninsured (58.7%).
Fig. 1. Unmet needs for ancillary care services by healthcare coverage type* among adults with diagnosed HIV – United States, 2017–2020 (N = 12 273).
*Statistical differences assessed using a Rao-Scott chi-square test to adjust for complex survey design. P<0.001.
Compared with those who had private healthcare coverage living at 400% or more of the FPL, people with private coverage living at less than 400% of the FPL, Medicaid, Medicare, other types of coverage, or no coverage were more likely to have unmet needs for ancillary care services related to HIV clinical support services, other medical services, and subsistence services (Table 1). Associations with unmet needs for any ancillary care services were strongest among persons who had no healthcare coverage (aPR: 2.57; 95% CI: 2.23–2.96), compared with those who had private coverage who were living at 400% or more of the FPL. Although similar patterns emerged for all types of ancillary care services, the magnitude of associations between healthcare coverage and unmet needs was highest for subsistence services (range of aPRs: 5.87–10.45 for subsistence services vs. 1.49–2.25 for support and other medical services).
Table 1.
Associations between healthcare coverage type and unmet needs for HIV ancillary care services among adults with diagnosed HIV – United States, 2017–2020 (N = 12 273)a.
| Coverage type | ≥1 unmet need for any ancillary care servicesb | ≥1 unmet need for HIV clinical support servicesc | ≥1 unmet need for other medical serviced | ≥1 unmet need for subsistence servicee | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||||||
| n | wted row % (95% CI) | aPR (95% CI)* | P | n | wted row % (95% CI) | aPR (95% CI)* | P | n | wted row % (95% CI) | aPR (95% CI)* | P | n | wted row % (95% CI) | aPR (95% CI)* | P | |
|
| ||||||||||||||||
| Overall | 5608 | 46.7 (45.0–48.3) | 1755 | 15.4 (14.4–16.3) | 3412 | 28.8 (27.6–29.9) | 3114 | 25.9 (24.4–27.4) | ||||||||
| Private | ||||||||||||||||
| ≥400% FPL | 264 | 21.7 (18.9–24.5) | Reference | 106 | 8.8 (7.0–10.7) | Reference | 191 | 15.7 (13.0–18.3) | Reference | 45 | 3.2 (2.1–4.3) | Reference | ||||
| <400% FPL | 1117 | 41.5 (38.5–44.6) | 1.87 (1.60–2.18) | <0.001 | 362 | 13.5 (11.9–15.2) | 1.49 (1.16–1.91) | 0.002 | 697 | 26.2 (24.0–28.5) | 1.64 (1.36–1.99) | <0.001 | 525 | 19.6 (17.5–21.7) | 5.87 (4.12–8.36) | <0.001 |
| Medicaid | 2655 | 52.4 (49.9–54.9) | 2.40 (2.10–2.75) | <0.001 | 825 | 17.4 (16.0–18.7) | 1.96 (1.56–2.48) | <0.001 | 1585 | 32.0 (29.8–34.2) | 2.04 (1.71–2.44) | <0.001 | 1611 | 31.7 (29.3–34.1) | 9.83 (6.96–13.87) | <0.001 |
| Medicare | 451 | 48.5 (44.0–52.9) | 2.33 (1.99–2.73) | <0.001 | 136 | 15.4 (11.8–19.0) | 1.86 (1.34–2.58) | <0.001 | 260 | 27.2 (23.8–30.6) | 1.83 (1.49–2.25) | <0.001 | 253 | 27.4 (24.3–30.5) | 9.24 (6.50–13.13) | <0.001 |
| Uninsured | 651 | 58.7 (55.1–62.2) | 2.57 (2.23–2.96) | <0.001 | 169 | 17.6 (14.6–20.5) | 1.85 (1.43–2.39) | <0.001 | 413 | 37.0 (33.6–40.4) | 2.25 (1.86–2.72) | <0.001 | 407 | 36.6 (33.4–39.7) | 10.45 (7.33–14.88) | <0.001 |
| Other | 366 | 48.2 (44.1–52.3) | 2.17 (1.88–2.52) | <0.001 | 125 | 17.8 (14.7–20.8) | 1.96 (1.47–2.62) | <0.001 | 199 | 26.7 (22.5–30.9) | 1.67 (1.36–2.07) | <0.001 | 216 | 28.2 (24.7–31.8) | 8.51 (5.97–12.14) | <0.001 |
aPR, adjusted prevalence ratios; CI, confidence interval; FPL, federal poverty level.
Adjusted for age. All P-values are associated with aPRs.
Includes unmet needs for HIV clinical support services, other medical services, or subsistence services.
Includes unmet needs for HIV case management, adherence counseling, peer group, patient navigation services.
Includes unmet needs for dental, mental health, drug/alcohol counseling or treatment services.
Includes unmet needs for Supplemental Nutrition Assistance Program (SNAP) or Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) services, meal or food services, transportation assistance, or shelter or housing services.
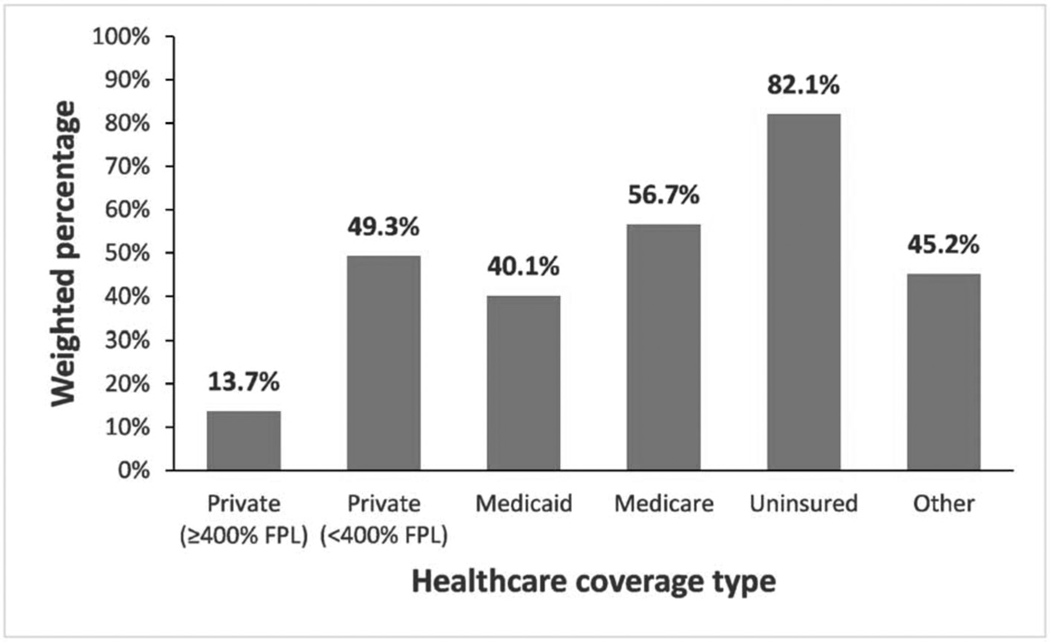
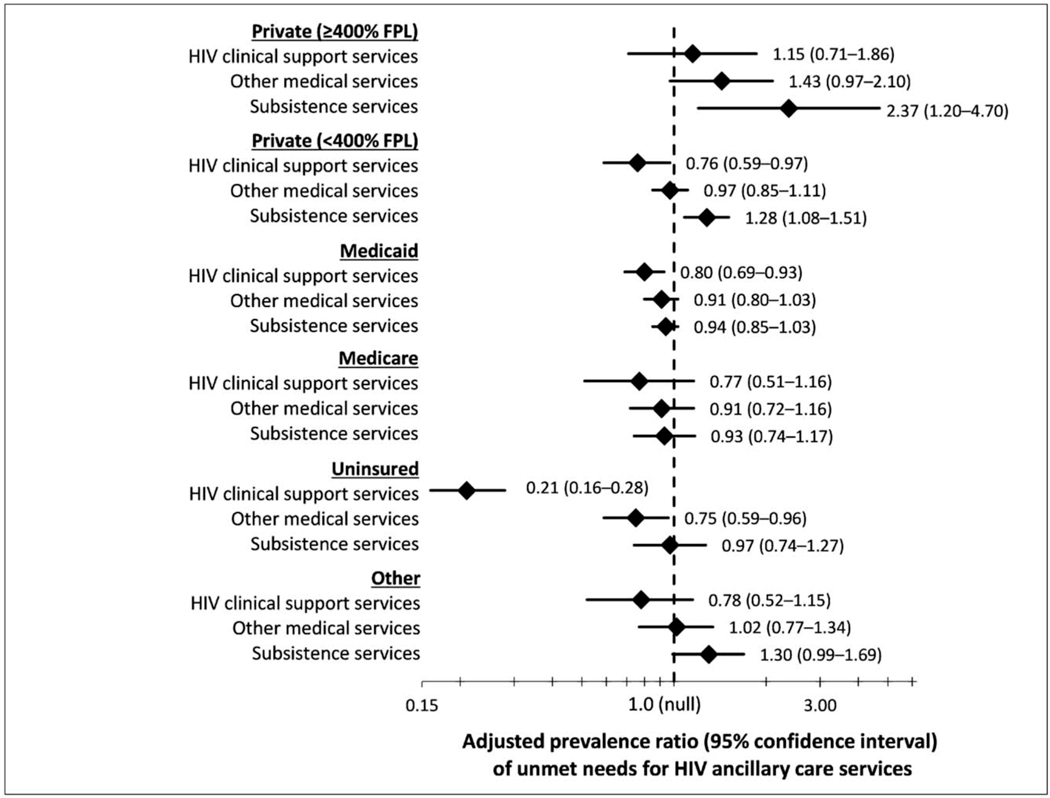
Receipt of RWHAP assistance was high for people with all healthcare coverage types (range: 40.1–82.1%), except for those with private coverage with 400% or more of the FPL (13.7%; Fig. 2). Receipt of RWHAP assistance was highest among people who were uninsured. Associations between receipt of RWHAP assistance and unmet needs for ancillary care services differed by healthcare coverage type (Fig. 3; Appendix Table, Supplemental Digital Content, http://links.lww.com/QAD/C463). Among persons who were uninsured, the prevalence of unmet needs for HIV clinical support services was 79% lower (aPR: 0.21; 95% CI: 0.16–0.28) and prevalence of unmet needs for other medical services was 25% lower (aPR: 0.75; 95% CI: 0.59–0.96) among those who received RWHAP assistance, compared with those who did not. There were no differences in unmet need for subsistence services by receipt of RWHAP assistance among the uninsured, although subsistence needs were quite high in this group (36.6%). Receipt of RWHAP assistance was also associated with lower prevalence of unmet needs for HIV clinical support services among those who had any private coverage living less than 400% of the FPL (aPR: 0.76; 95% CI: 0.59–0.97) and Medicaid (aPR: 0.80; 95% CI: 0.69–0.93). There were no differences in level of unmet need for other medical services or subsistence services among those with Medicaid or Medicare. Regardless of poverty level, people with any private coverage who received RWHAP assistance were more likely to have unmet needs for subsistence services than those who did not, although overall unmet need for subsistence services was lower for those living at 400% or more of the FPL than people living at less than 400% of the FPL (3.2 vs. 19.6%; Table 1).
Fig. 2. Receipt of Ryan White HIV/AIDS Program assistance by healthcare coverage type among adults with diagnosed HIV – United States, 2017–2020 (N = 12 273).
*Statistical differences assessed using a Rao-Scott chi-square test to adjust for complex survey design. P<0.001.
Fig. 3. Comparison of unmet needs for HIV ancillary care services among people who received assistance through the Ryan White HIV/AIDS Program versus those that did not (referent group) among adults with diagnosed HIV, by healthcare coverage type – United States, 2017–2020 (N = 12 273)*.
*Referent group for all associations was not receiving RWHAP assistance. All associations were adjusted for age. HIV clinical support services include: HIV case management, adherence counseling, peer group, patient navigation services. Other medical services include: dental, mental health, drug/alcohol counseling or treatment services. Subsistence services include: Supplemental Nutrition Assistance Program (SNAP) or Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) services, meal or food services, transportation assistance, or shelter or housing services. RWHAP, Ryan White HIV/AIDS Program.
Discussion
Unmet needs for HIV ancillary care services were high across all healthcare coverage types among all adults with diagnosed HIV but were highest among those who were uninsured–—particularly for subsistence services. Even among those with private coverage living ≥400% of the FPL, who had the lowest unmet need, over one in five had one or more unmet need for an ancillary care service. Despite having the highest prevalence of unmet needs for ancillary care services, uninsured persons who received RWHAP assistance had fewer unmet needs related to HIV clinical support services and other medical services, but not for subsistence services. Further, unmet needs for other medical services and subsistence services did not differ by receipt of RWHAP assistance among those with Medicaid, Medicare, or other healthcare coverage types, despite these people having a high level of unmet need for HIV ancillary care services.
Nearly all adults with diagnosed HIV with Medicaid, Medicare, or other types of coverage, and those who were uninsured were living at less than 400% of the FPL; these groups also had the highest level of unmet needs for ancillary care services. Although people who received any private healthcare coverage generally had lower unmet needs than people with other coverage types, those that were living at less than 400% of the FPL had levels of unmet needs – particularly for support services and other medical services – that were more similar to those among people with other coverage types. These results demonstrate that disparities in unmet needs for HIV ancillary care services by healthcare coverage type could at least partially be attributed to differences in socioeconomic status (SES) and other social determinants of health; this is supported by other literature [5,17,19]. PWH living in poverty may experience challenges – including unstable housing, food in security, or comorbidities such as depression, or anxiety – that are associated with adverse HIV clinical outcomes [9,10,12,20,21]. Specifically, PWH receiving Medicaid or Medicare often qualify for coverage due to income, disability, or older age, and thus, commonly have co-occurring conditions that may complicate their HIV care and cause challenges in engaging with the medical system [8]. These people may be more likely to have needs for HIV ancillary care services that, if not received, could prevent them from maintaining viral suppression. With growing socioeconomic inequities during and following the coronavirus disease 2019 (COVID-19) pandemic [22] and high need for subsistence services among PWH, allocating resources to address other medical and subsistence needs is even more important for removing barriers to engaging in HIV care and maintaining viral suppression. Health departments should continue to monitor the need for ancillary care services over time with respect to local HIV prevalence and characteristics and experiences of PWH in their local service area, including socioeconomic status and existence of co-occurring social and medical conditions.
Receipt of RWHAP assistance was common among adults with diagnosed HIV, but was much higher for all groups except for those with any private coverage living at 400% or more of the FPL. This likely reflects that many people with private coverage living at 400% or more of the FPL may be ineligible for RWHAP services based on their income. HIV outcomes tend to be better among those who receive RWHAP assistance, regardless of healthcare coverage status, but particularly among uninsured PWH [17]. Despite high unmet needs among uninsured persons, receipt of RWHAP assistance was high in this population, and may have provided particularly important assistance for meeting service needs. Without this safety-net program, it is likely the uninsured group would have very limited access to ancillary care services and to primary HIV care services more generally. RWHAP assistance may have also been beneficial for addressing unmet needs for HIV clinical support services among people with Medicaid, Medicare, and people with any private coverage living at less than 400% of the FPL. However, there was still substantial unmet need for services – particularly for subsistence – for a majority of adults with diagnosed HIV that were unaddressed and could lead to adverse HIV outcomes. Some of these services, including housing assistance and SNAP/WIC services, are not supported by the RWHAP. Nonetheless, the level of unmet needs for subsistence services may indicate need for expansion of resources for PWH through other federal safety net programs. Further, expanding Medicaid in remaining non-Medicaid expansion states could improve coverage of services for low income PWH, particularly in areas with limited access to RWHAP-funded facilities.
The persistence of unmet needs, even with RWHAP assistance, could be explained by multiple factors. First, the RWHAP serves the most vulnerable PWH [23], who may experience higher levels of unmet need [5]. Second, due to realities of funding availability, RWHAP grant recipients may not be able to serve all those in need, nor meet all needs of the clients served [14]. Third, RWHAP grant recipients allocate funds based on local community needs with input from local stakeholders and the scope of available and accessible services and income eligibility may vary by jurisdiction. Fourth, RWHAP requires that grant recipients allocate at least 75% of their funds to defined core medical services, which includes clinical medical visits, ADAP, healthcare coverage, medical case management, mental health services, oral healthcare, and outpatient care related to substance use disorder. RWHAP grant recipients can request a waiver to this requirement to provide more support services, including certain subsistence services [24,25]. The Health Resources and Services Administration (HRSA) is pursuing simplifications to the core medical services waiver process to reduce the burden on grant recipients [26]. Several of these factors may be addressed through the Ending the HIV Epidemic (EHE) in the U.S. initiative. HRSA HIV/AIDS Bureau EHE grant recipients in high HIV incidence areas and seven states with large rural epidemics have additional funding that is flexible and not limited to RWHAP service category definitions, policies, or income eligibility requirements to respond to the needs of PWH. However, EHE funding was not widely available during the years examined in this analysis.
Replicating components of the RWHAP comprehensive system of care using a ‘whole person’ approach in non-RWHAP HIV care settings could also be beneficial for those who have complex needs but limited resources for accessing ancillary care services. For instance, co-location of services could ensure that people have access to other needed services during HIV medical care appointments. Even in the absence of available services within the HIV care setting, maintaining partnerships with a diverse set of local non-medical and subsistence providers could facilitate linkage to life-saving resources. In addition, ensuring that needs are routinely assessed during HIV medical care appointments and other interactions with PWH could help identify services that would benefit patients and help continue to engage them in care. Strengthening administrative office support and leveraging Data To Care approaches could also help in following up with people who might be out of care or need additional assistance in addressing their needs [27]. Finally, the voices of PWH, their communities, and the communities that support PWH are a cornerstone of the RWHAP; the involvement of these communities in the planning, development and implementation of HIV and ancillary services helps ensure a person-centered approach to care.
This analysis is subject to limitations. First, all measures were self-reported and subject to measurement bias. Receipt of RWHAP assistance may have been underestimated and could have varied by health coverage type. For instance, people who were uninsured might not have reported receipt of RWHAP assistance through medication coverage or coverage of other services. In addition, people with private insurance may have also purchased insurance using RWHAP or ADAP funds and not have reported receiving RWHAP assistance, resulting in possible misclassification. Although it is difficult to assess directionality of this potential bias, future studies could consider using medical record abstraction to report or assess accuracy of reported healthcare coverage and receipt of RWHAP assistance to correct for this bias. Unmet needs could also reflect local limitations in service availability through the RWHAP in local service areas. For instance, level of available RWHAP funding at local facilities could vary, which could influence which services are available for clients. SNAP/WIC services, which were categorized as subsistence services in this analysis, are not directly funded through the RWHAP, although RWHAP grant recipients may make referrals to these services as needed. In a sensitivity analysis in which SNAP/WIC services were removed from the subsistence service category, findings did not meaningfully change. Data were cross-sectional, and thus, reported associations do not imply causality. Finally, response rates were suboptimal, but results were adjusted for non-response and post-stratified to known population totals by age, race/ethnicity, and sex from the NHSS using established, standard methodology [7,28]. Even with suboptimal response rates, there is still value in results obtained from unbiased sampling methods [29].
Unmet needs for HIV ancillary care services were high across all healthcare coverage types, with the highest unmet need experienced among people who were uninsured. Although the RWHAP provided substantial support for people who were uninsured, especially for HIV clinical support services and other medical services, additional resources may be needed to address gaps in their subsistence needs. There were also gaps in services for people with Medicaid, Medicare, and private insurance – particularly those related to subsistence. Broadening coverage opportunities for uninsured persons could help in addressing unmet need, especially in non-Medicaid expansion states, where lower levels of Medicaid coverage mirror higher levels of uninsured PWH [17]. With growing socioeconomic inequities among Americans following the COVID-19 pandemic, expanding availability of HIV ancillary care services for all PWH could play an important role in addressing barriers to achieving health equity, meeting national HIV prevention and treatment goals, and ending the HIV epidemic in the United States.
Supplementary Material
Acknowledgements
We acknowledge local MMP staff, health departments, and participants, without whom this research would not be possible. Funding for the Medical Monitoring Project is provided by the Centers for Disease Control and Prevention. Author contributions: S.D. designed the study and analysis, and wrote and critically reviewed the paper; S.M.C. led the analysis and critically reviewed the paper; L.D. contributed to design of the study and analysis, contributed to writing, and critically reviewed the paper; J.K. contributed to the design of the study, contributed to writing, and critically reviewed the paper; J.W. critically reviewed the paper; P.W.K. contributed to the design of the study and critically reviewed the paper; A.D. contributed to the design of the study and critically reviewed the paper; H.H. contributed to the design of the study and critically reviewed the paper; J.-F.L. contributed to analyzing the data and critically reviewed the paper; F.S. contributed to analyzing the data and critically reviewed the paper; L.B. contributed to the design of the study, contributed to writing, and critically reviewed the paper.
Funding:
CDC.
Disclaimers:
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
The views expressed in this publication are solely the opinions of the authors and do not necessarily reflect the official policies of the U.S. Department of Health and Human Services or the Health Resources and Services Administration, nor does mention of the department or agency name simply endorsement by the U.S. Government.
Footnotes
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson IB, Tie Y, Padilla M, Rogers WH, Beer L. Performance of a short, self-report adherence scale in a probability sample of persons using HIV antiretroviral therapy in the United States. AIDS 2020; 34:2239–2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yehia BR, French B, Fleishman JA, Metlay JP, Berry SA, Korthuis PT, et al. Retention in care is more strongly associated with viral suppression in HIV-infected patients with lower versus higher CD4 counts. J Acquir Immune Defic Syndr 2014; 65:333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dasgupta S, Tie Y, Beer L, Fagan J, Weiser J. Barriers to HIV care by viral suppression status among US adults with HIV: findings from the Centers for Disease Control and Prevention Medical Monitoring Project. J Assoc Nurses AIDS Care 2021; 32:561–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dasgupta S, Tie Y, Beer L, Weiser J. Unmet needs for ancillary care services are associated with HIV clinical outcomes among adults with diagnosed HIV. AIDS Care 2021:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The White House. National HIV/AIDS Strategy for the United States 2022–2025. 2021. Available at https://hivgov-prod-v3.s3.amazonaws.com/s3fs-public/NHAS-2022-2025.pdf
- 7.Centers for Disease Control and Prevention. Behavioral and Clinical Characteristics of Persons with Diagnosed HIV Infection–—Medical Monitoring Project, United States, 2019 Cycle (June 2019–May 2020). 2021. Available at https://www.cdc.gov/hiv/library/reports/hiv-surveillance-special-reports/no-28/index.html
- 8.Gallant J, Hsue PY, Shreay S, Meyer N. Comorbidities among US patients with prevalent HIV infection–—a trend analysis. J Infect Dis 2017; 216:1525–1533. [DOI] [PubMed] [Google Scholar]
- 9.Beer L, Tie Y, Padilla M, Shouse RL, Medical Monitoring P. Generalized anxiety disorder symptoms among persons with diagnosed HIV in the United States. AIDS 2019;33:1781–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gokhale RH, Weiser J, Sullivan PS, Luo Q, Shu F, Bradley H. Depression prevalence, antidepressant treatment status, and association with sustained HIV viral suppression among adults living with HIV in care in the United States, 2009–2014. AIDS Behav 2019; 23:3452–3459. [DOI] [PubMed] [Google Scholar]
- 11.Dasgupta S, Tie Y, Lemons-Lyn A, Broz D, Buchacz K, Shouse RL. HIV-positive persons who inject drugs experience poor health outcomes and unmet needs for care services. AIDS Care 2020; 33:1146–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons with diagnosed HIV infection–—Medical Monitoring Project, United States, 2019 cycle (June 2019-May 2020). 2020. [Google Scholar]
- 13.Conviser R, Pounds MB. The role of ancillary services in client-centred systems of care. AIDS Care 2002; 14 (Suppl 1):S119–S131. [DOI] [PubMed] [Google Scholar]
- 14.Kates J, Dawson L, Horn TH, Killelea A, McCann NC, Crowley JS, et al. Insurance coverage and financing landscape for HIV treatment and prevention in the USA. Lancet 2021; 397:1127–1138. [DOI] [PubMed] [Google Scholar]
- 15.Health Resources and Services Administration. Ryan White HIV/AIDS Program legislation. Available at https://hab.hrsa.gov/about-ryan-white-hivaids-program/ryan-white-hivaids-program-legislation
- 16.S.2240 – Ryan White Comprehensive AIDS Resources Emergency Act of 1990. Available at https://www.congress.gov/bill/101st-congress/senate-bill/2240 [PubMed]
- 17.Dawson L, Kates J. Insurance coverage and viral suppression amongpeoplewithHIV,2018.Availableat https://www.kff.org/hivaids/issue-brief/insurance-coverage-and-viral-suppression-among-people-with-hiv-2018/ [Google Scholar]
- 18.Centers for Disease Control and Prevention. HIV Surveillance Report, 2019; vol.32. Published May 2021. Available at http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- 19.Monroe AK, Lesko CR, Chander G, Lau B, Keruly J, Crane HM, et al. Ancillary service needs among persons new to HIV care and the relationship between needs and late presentation to care. AIDS Care 2019; 31:1131–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wainwright JJ, Beer L, Tie Y, Fagan JL, Dean HD, Medical Monitoring P. Socioeconomic, behavioral, and clinical characteristics of persons living with HIV who experience homelessness in the United States, 2015–2016. AIDS Behav 2020; 24:1701–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marcus RTY, Dasgupta S, Beer L, Padilla M, Fagan J, Prejean J. Characteristics of adults with diagnosed HIV who experienced housing instability –— Medical Monitoring Project, United States, 2018. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perry BL, Aronson B, Pescosolido BA. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proc Natl Acad Sci USA 2021; 118: e2020685118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health Resources and Services Administration. Ryan White HIV/AIDS Program annual client-level data report 2019. 2020. Available at https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/data/rwhap-annual-client-level-data-report-2019.pdf
- 24.Health Resources and Services Administration. Uniform standard for waiver of core medical services requirement for grantees under parts, A, B, and C. Available at https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/grants/13-07-waiver.pdf
- 25.Health Resources and Services Administration. Ryan White HIV/AIDS Program services: Eligible individuals and allowable uses of funds. Available at https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/grants/service-category-pcn-16-02-final.pdf
- 26.Health Resources and Services Administration. Updates to uniform standard for waiver of the Ryan White HIV/AIDS Program core medical services expenditure. Available at https://www.federalregister.gov/documents/2021/04/20/2021-08016/updates-to-uniform-standard-for-waiver-of-the-ryan-white-hi-vaids-program-core-medical-services
- 27.Centers for Disease Control and Prevention. Data to Care program guidance: Using HIV surveillance data to support the HIV care continuum. 2017. Available at https://www.cdc.gov/hiv/pdf/funding/announcements/ps18-1802/CDC-HIV-PS18-1802-AttachmentJ-Data-to-Care-Program-Guidance.pdf
- 28.Beer L, Johnson CH, Fagan JL, Frazier EL, Nyaku M, Craw JA, et al. A national behavioral and clinical surveillance system of adults with diagnosed HIV (the Medical Monitoring Project): protocol for an annual cross-sectional interview and medical record abstraction survey. JMIR Res Protoc 2019; 8: e15453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q 2006; 70:646–675. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.