Abstract
Background
The integration of Virtual Reality (VR) with Case-Based Learning (CBL) has the potential to revolutionise undergraduate medical education, particularly in complex subjects such as the anatomy and rehabilitation of the shoulder joint. This study aimed to explore the effectiveness of this innovative approach in enhancing learning outcomes and knowledge retention.
Methods
This study employed a parallel-group, assessor-blinded randomised controlled trial (RCT) design. A comprehensive five-week educational programme was developed, combining traditional lecture-based learning with VR-enhanced CBL. The study involved 82 undergraduate students from China Medical University, who were divided into groups receiving different combinations of VR and CBL. Student performance was evaluated through tests and questionnaires.
Results
In the anatomy-related courses, the integration of VR technology with CBL yielded significantly higher results (87.71 ± 5.60) compared to traditional methods (82.59 ± 6.64), with a statistically significant difference (P < 0.05). This provides compelling evidence of VR's potential to enhance student engagement and knowledge retention. In the context of physiotherapy-related courses, however, while the test scores of the VR-combined CBL group (81.85 ± 5.99) were marginally higher than those of the traditional CBL group (79.02 ± 7.57), this difference was not statistically significant (P > 0.05).
Conclusion
The present study provides preliminary evidence for the benefits of incorporating VR into medical education, particularly in anatomy. While the results are promising, further research is needed to explore the optimal integration of VR and CBL in rehabilitation studies and to assess their long-term impact on student learning and clinical performance.
Trial registration
The study was registered with Chinese Clinical Trials Registry (Registration Number: ChiCTR2400089295) on 05/09/2024.
Keywords: Virtual Reality, Case-Based Learning, Medical Education, Shoulder Joint Therapy, Learning Outcomes, Innovative Teaching Methodologies, Student Engagement, Knowledge Retention
Introduction
Virtual Reality (VR) has emerged as a rapidly advancing technology with particularly profound implications for medical applications. The integration of digital technology into the medical field promises to revolutionise how educational content is delivered and received. With its potential to offer immersive, interactive learning experiences, VR technology stands at the forefront of educational innovation [1]. As digital technologies progress at an unprecedented rate, they drive significant refinements in our educational paradigms. Traditional teaching methods are being redefined and enhanced, paving the way for more sophisticated and effective educational models [2]. VR, in particular, with its advanced motion tracking and superior imaging capabilities, creates a fully digitised environment where users can engage with content in a highly interactive and impactful manner. This technological innovation is not only reshaping entertainment and social interaction; it is also transforming the landscape of medical training and therapy, presenting new possibilities for both educators and learners [3].
Makransky and colleagues have been instrumental in synthesising existing studies into a coherent theoretical framework that explores how VR can enhance learning outcomes [4]. Their Cognitive Affective Model of Immersive Learning (CAMIL) identifies presence and agency as key factors facilitated by immersion and control. The model highlights six factors—interest, motivation, self-efficacy, embodiment, cognitive load, and self-regulation—that contribute to effective learning and knowledge transfer in immersive virtual reality environments. Their work identifies key psychological support mechanisms within VR environments and assesses their impact on educational effectiveness. This framework has significant implications for the design of pedagogical strategies and future studies, suggesting ways in which VR can be optimally utilised to support and enhance learning experiences [4].
The introduction of VR in medical education has initiated revolutionary changes, significantly enhancing student engagement, comprehension, and preparedness for clinical practice. By providing an immersive and detailed understanding of complex medical procedures, VR allows students to acquire essential skills in a controlled and interactive environment [5].
Advantages of virtual reality learning
VR technology exhibits exceptional capability in creating immersive and interactive learning environments, and it has been extensively implemented in the field of medical education and training [6]. This technology is recognized as an effective instructional method, due to its high levels of system usability and learner satisfaction [7]. VR technology provides a robust and standardized platform for clinical practice and procedural instruction across various disciplines, including internal medicine, surgery, rheumatology, ophthalmology, psychiatry, medical engineering integration, and biopharmaceuticals [8–13]. As an alternative to conventional anatomical training approaches, VR significantly reduces the risks associated with the complexities of human anatomy and the unpredictability of patient interactions [14]. Although VR does not notably decrease the time required to complete assessments, it has been shown to enhance test scores, satisfaction levels, and enjoyment within anatomical education [15, 16]. Furthermore, virtual reality learning environments create new opportunities for supporting learners and improving the learning process [17]. The study by Andreasen et al. demonstrates that students using VR technology to practice the ISBAR communication technique achieve superior educational outcomes compared to traditional paper-based methods [18]. In the context of cardiopulmonary resuscitation training, the application of VR technology significantly enhances students' performance and satisfaction [19].
Advantages of case-based learning
In clinical settings for medical students, Case-Based Learning (CBL) serves as an effective strategy for teaching basic science subjects [20]. Fink and his colleagues indicate that interactions with real patients during CBL are perceived as more authentic compared to virtual simulations, leading to higher diagnostic accuracy [21]. Furthermore, while VR increases the sense of presence, it also elevates cognitive load, which may diminish learning outcomes. Electroencephalogram (EEG) measurements have demonstrated that this increased cognitive demand can reduce the effectiveness of learning [22]. Additionally, VR's reliance on visual-spatial abilities can pose a limitation for students with weaker skills in this area. For these students, navigating and interacting within a 3D VR space can be challenging, potentially hindering their understanding of complex subjects like anatomy. In contrast, CBL provides a consistent learning experience across varying visual-spatial abilities, ensuring that all students, regardless of their inherent skills, can engage effectively with the educational content [23]. Therefore, while VR offers significant advantages in terms of engagement and interactivity, it is essential to balance its use with traditional methods like CBL, which provide high diagnostic accuracy and equitable learning opportunities.
Integration of virtual reality with case-based learning
In pursuit of nurturing highly skilled and refined medical professionals, educators utilize various pedagogical strategies to elevate student engagement, knowledge retention, and practical capabilities [24]. The outbreak of COVID-19 necessitated a pivot to online modalities, compelling the conversion of conventional face-to-face instruction and laboratory classes to remote formats [25]. Within the domain of medical education, there is an emerging exploration into the synergistic application of Virtual Reality and Case-Based Learning, aimed at providing students with tailored training scenarios that bridge theoretical knowledge with clinical practice experience [25, 26]. This amalgamation offers distinct advantages over traditional, singular teaching approaches, particularly in the cultivation of teamwork skills. The integration not only bolsters basic recall capabilities but, although it may augment the associated cognitive load, it leaves deeper cognitive processing unaffected [27]. Moreover, the fusion of VR and CBL creates a risk-free simulated environment, allowing students to repetitively practice complex medical procedures until proficiency is achieved, without diminishing educational quality [28]. For instance, Wainman et al. demonstrate that combining traditional teaching methods with pre-class online learning and practical training significantly enhances team performance. In conclusion, the educational methodology integrating VR and CBL merits further investigation [29].
Study and hypothesis
This investigation aims to elucidate the collaborative effects of Virtual Reality and Case-Based Learning in the domain of medical education, specifically regarding their potential to augment student engagement, enhance knowledge retention, and facilitate the development of practical skills. To achieve this, we have initiated a randomized controlled trial to assess the distinctions between a combined VR and CBL model and a traditional CBL approach within medical education. This evaluation focuses on students' acceptance of differing pedagogical strategies and their rates of knowledge retention under each method. This study examined various dimensions such as teaching methods, cognitive load, teacher-student interactions, skill enhancement, and overall satisfaction, all grounded in established educational theories [4, 7, 21, 22]. In summary, we posit the following hypothesis: the integration of VR with CBL will significantly elevate student engagement and knowledge retention when contrasted with the traditional CBL model [7].
Methods
Trial design
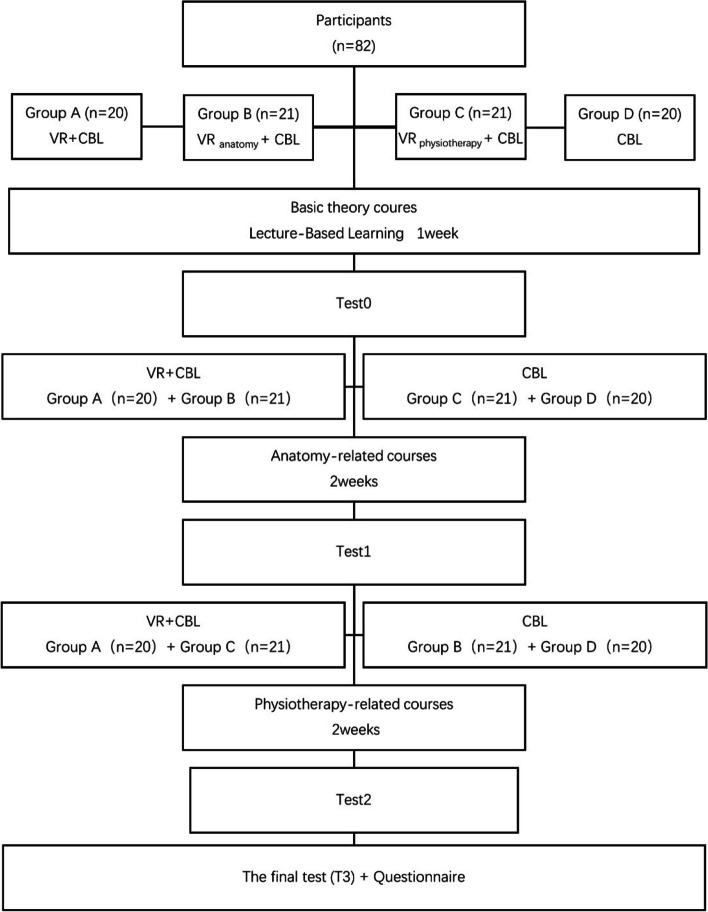
This study employed a parallel-group, assessor-blinded randomized controlled trial (RCT) design. The research meticulously arranged a comprehensive five-week educational plan, which included a course every two weeks, each lasting two hours, for a total of 20 teaching hours. The course setup was sequential and rigorously structured: the first week served as an introductory week to the basic theories of the shoulder joint; the following two weeks focused on detailed anatomical studies of the shoulder joint; and the last two weeks were dedicated to intensive rehabilitation physiotherapy of the shoulder joint (Fig. 1). The initial theoretical teaching was conducted through traditional Lecture-Based Learning (LBL). In contrast, the subsequent anatomy and rehabilitation physiotherapy modules employed CBL, based on eight carefully selected real cases of shoulder joint injuries. These cases were chosen to encompass a wide range of common pathological conditions and anatomical details. The course design emphasised four key areas: the anatomy of the shoulder joint, injury characteristics, radiological assessment and diagnostic techniques, and the formulation of personalised rehabilitation strategies. This study received ethical approval from the Ethics Committee of Shengjing Hospital of China Medical University, and all participants provided written informed consent.
Fig. 1.
Basic flowchart of course design and teaching methods
Participants
This study enlisted 82 third-year students from the Rehabilitation program at China Medical University, who had not yet undergone clinical internships or been exposed to complex shoulder joint rehabilitation courses. These students were considered ideal candidates for participation due to their lack of prior exposure to clinical settings and intricate rehabilitation protocols related to shoulder joints. Furthermore, they exhibited similar educational backgrounds and foundational knowledge, thereby minimising potential external influences on the study outcomes. The random allocation of these participants into different study groups ensured the reliability and validity of the research findings. Throughout the study, they underwent rigorous course scheduling and training to assess the impact of the educational program on their knowledge and skills pertaining to shoulder joint rehabilitation. Active participation from these individuals during the study period, combined with their valuable feedback post-course completion, provided deeper insights and understanding into the outcomes of this study.
Interventions
This study deployed a multifaceted teaching intervention among third-year undergraduates in the Rehabilitation Therapy programme at China Medical University, with the objective of enhancing student engagement, improving knowledge retention, and advancing the development of practical skills [4].
Theory
Case-based learning
To prepare for each Case-Based Learning course, teachers carefully selected a representative clinical case that met the course requirements and organised its medical history, test results, and imaging data. These materials were distributed to students two days before the course, allowing them to prepare in advance.
In this study, both the Virtual Reality combined with Case-Based Learning group (VR + CBL) and the Case-Based Learning group (CBL) dealt with eight complete and real cases of shoulder joint diseases, including frozen shoulder, rotator cuff tear, subacromial impingement syndrome, shoulder dislocation, calcific tendinitis of the supraspinatus tendon, long head of the biceps tendinitis, acromioclavicular joint dislocation, and suprascapular nerve entrapment.
Integration of virtual reality with case-based learning
The combined VR experiment group used VR equipment for teaching while conducting case-based learning. After the group report and teacher summary, students entered an interactive computer simulation environment. While the teacher explained relevant knowledge points, students directly observed real anatomical structures in the simulation environment and personally operated treatment methods, experiencing the entire process of diagnosing and treating shoulder joint injuries.
In the functional anatomy part of VR, students used the angle, axial, and temporal tools located in the lower right corner of the computer screen to learn the range of motion for shoulder flexion, extension, adduction, abduction, internal rotation, external rotation, and internal and external rotation in the abducted position. They also studied the biomechanical changes in the scapula, clavicle, sternum, and chest wall during these activities, the rhythm of the glenohumeral joint, and the anatomical starting and ending points of the muscles around the shoulder joint, including the rotator cuff, as well as the timing of their involvement in movement, guided by interactive step prompts.
In the rehabilitation treatment part, based on the aforementioned test results and the shoulder joint function scale provided by human–computer interaction, a rehabilitation treatment plan was formulated. This plan included setting rehabilitation goals, designing rehabilitation training movements, and learning various rehabilitation training methods, such as pendulum exercises, ball control, standing and prone push-ups, glenohumeral joint sliding, and shoulder mobilization techniques (Fig. 2).
Fig. 2.
Virtual Reality system. 1.Utilise the VR system to learn the Jobe Test: The upper limb is abducted to 90 degrees in the scapular plane, with the thumb pointing downwards, and then resists abduction. 2.Utilise the VR system to learn the Shoulder Drop Test: This test involves passively abducting the patient's shoulder to 90–120 degrees. If the affected shoulder cannot be maintained and falls after the examiner removes support, it indicates a supraspinatus tendon injury. 3.Utilise the VR system to learn glenohumeral traction: Learn how to apply traction to the glenohumeral joint using the VR system. 4.Students use head-mounted displays for VR learning
VR equipment information
VR software names: virtual reality training system for shoulder joint functional anatomy and movement principles V 1.0 (NO. 2023SR1418086) and virtual reality training system for the rehabilitation and treatment of rotator cuff injuries V1.0 (NO. 2023SR1418090). Computer hardware requirements: CPU: 3.5 GHz, RAM: 16 GB, GPU Memory: 8 GB, Storage Capacity: 500 GB. Operating system and version: Windows 10. Network bandwidth requirements: bandwidth ≥ 200 Mbps. Head-mounted display name: The HTC VIVE—Pro professional edition basic set. Head-mounted display information: The basic set includes two base stations (1.0) and two controllers (1.0). The head-mounted display uses SteamVR™ tracking (2.0) and features Hi-Res Audio certified built-in headphones. It also has a built-in microphone and an adjustable interpupillary distance (IPD) for optimal comfort.
Learning objectives
Following the completion of the educational interventions, this study anticipates improvements in students' knowledge retention rates, proficiency in acquired skills, and elevated levels of classroom participation and satisfaction.
Materials
The CBL group employed the nationally standardised textbook, ‘Musculoskeletal Rehabilitation’, along with eight authentic clinical cases of shoulder joint injuries for instructional purposes. In addition to the resources used by the CBL group, the VR + CBL group integrated a virtual reality simulation system and VR equipment into their teaching approach.
Educational strategies
Students were designated as Group A (n = 20), Group B (n = 21), Group C (n = 21), and Group D (n = 20). Group A received CBL teaching assisted by VR technology, Group D underwent traditional CBL teaching, Group B used VR technology assistance in anatomy courses only, and Group C applied VR technology assistance in physiotherapy courses only.
They first completed a one-week basic theoretical course on the shoulder joint, which included two courses held on Tuesday and Thursday, each lasting two academic hours. This was followed by a theoretical test (T0), the results of which were used for subsequent analysis. The test was a written test lasting 45 min, with a total score of 100 points.
The anatomy-related courses on the shoulder joint lasted for two weeks, with two courses each week (Tuesday and Thursday), totalling four courses, each lasting two academic hours. To prevent bias from different lecturers and time slots, each class analysed a case taught by the same teacher. In the first week, the morning session on the first day was allocated to Groups A and B, while the afternoon session was for Groups C and D. On the second day, the morning session was for Groups C and D, and the afternoon session for Groups A and B. The teaching sequence in the second week mirrored that of the first week. After the course, a theoretical test (T1) was conducted to evaluate the learning outcomes. This test was a written test lasting 45 min, with a total score of 100 points.
The rehabilitation physiotherapy-related courses on the shoulder joint also lasted for two weeks, with two courses per week (Tuesday and Thursday), totalling four courses, each lasting two academic hours. The scheduling order of the rehabilitation courses was identical to that of the anatomy courses. After the course, a test (T2) was conducted, which included a written test and a practical operation, with a total score of 100 points. The written test lasted 45 min and was worth 40 points, while the practical operation lasted three to five minutes per person and was worth 60 points.
The final test (T3) was conducted at the end of the semester, lasting 120 min, with a total written test score of 100 points. The scores for the shoulder joint-related questions, which accounted for 22%, were analysed. After T3, the statistical results of T0, T1, and T2 were announced to all students without compromising personal privacy. Each student's scores were shared individually, and a questionnaire survey was conducted.
In both the traditional CBL group and the VR + CBL group, students were divided into four teams, each comprising five to six members, to promote collaborative learning. Each team was tasked with reviewing relevant case materials, conducting research on the latest academic articles to solidify their knowledge foundation, and preparing a concise report. During the course sessions, each team was allotted five minutes to present their insights and pose questions. Following each team's presentation, the teacher provided comprehensive feedback, offered their own perspectives, and addressed students' queries, with approximately five minutes dedicated to question-and-answer sessions for each team. After all team presentations, the teacher delivered a case exposition, introducing key knowledge points and diagnostic and treatment methodologies. In the traditional CBL group, the teacher played relevant videos to enhance students' understanding of the case. Students emulated the actions depicted in the videos and demonstrated them within their groups while the teacher offered guidance. In the VR experimental group, students utilized VR equipment for more immersive learning to gain a deeper understanding of the case. The teacher initially demonstrated, after which students engaged in practical operations, with the teacher providing guidance. Each team was equipped with a set of VR devices, and team members used them in rotation, with each individual having five to ten minutes of operation time. Through the VR devices, they could directly observe anatomical structures, execute treatment procedures, and simulate the entire diagnostic and treatment process. Upon completing these processes, teachers in both the traditional CBL group and the VR + CBL group recapitulated the course content, further clarified students' queries, and assigned pertinent homework to reinforce learning outcomes.
Incentives
In this study, no incentives / reimbursements were provided to participants.
Instructors
The teaching was conducted by a team of experienced professional educators: the basic theory component was taught by a professor with 27 years of experience in medical education; the anatomy module was led by an anatomy expert with 16 years of teaching expertise; and the rehabilitation physiotherapy segment was conducted by a Master of Physical Therapy with 12 years of clinical practice experience.
Delivery
The CBL group employed a traditional face-to-face interactive teaching model, while the VR + CBL group utilised both face-to-face and virtual simulation modalities. The same course was delivered by the same instructor to both groups (which were subjected to identical interventions). The student-to-teacher ratio was either 40:1, 41:1, or 42:1.
Environment
Foundational theory classes were conducted in a lecture room with all students participating together. Both the anatomy-related courses and the rehabilitation therapy-related courses were held in the same classroom, regardless of whether VR was used. To minimise bias, groups undergoing different interventions attended classes at different times, with their schedules alternating accordingly.
Schedule
This study meticulously arranged a five-week comprehensive educational plan, consisting of a course every two weeks, each lasting two hours, totalling 20 teaching hours. The course structure was sequential and rigorously organised: the first week served as an introductory week to the basic theories of the shoulder joint; the following two weeks focused on detailed anatomical studies of the shoulder joint; and the last two weeks were dedicated to intensive rehabilitation physiotherapy for the shoulder joint.
In this study, the various educational methods employed did not require learners to possess specific adaptive capabilities, nor were there any alterations made to the educational methods specifically for the research. Attendance was managed by the teaching staff, who conducted roll calls at the beginning of each course. As these were compulsory courses within the programme, all students attended, resulting in a 100% attendance rate. The materials and educational strategies used in the interventions were delivered as originally planned, and all interventions were conducted on schedule.
Outcomes
Knowledge retention assessment
At the conclusion of each section of the course, a knowledge assessment was conducted to evaluate the students' understanding of the material. These assessments were independently created by the instructors and comprised 100 multiple-choice questions (each with five options), with a maximum score of 100 points. The duration of the test was 120 min. To minimise experimental bias and interference, the knowledge tests were proctored by a teacher who was not informed about the study. This teacher also reviewed and tabulated the results. In the final test, scores related to shoulder joint issues were specifically analysed, consisting of 22 multiple-choice questions (each with five options), with a maximum score of 22 points.
Anonymous questionnaire survey
An anonymous questionnaire survey was conducted to evaluate students' views on the course structure, content practicality, teaching methods, teacher-student interaction, assignments and feedback, learning resources, study load, skill improvement, course recommendation, and overall satisfaction [7, 20–22, 27]. The scoring range for each indicator in the questionnaire was from 1 to 5, with 1 being 'Strongly Disagree,' 2 being 'Disagree,' 3 being 'Neutral,' 4 being 'Agree,' and 5 being 'Strongly Agree. The student questionnaire exhibited high reliability, with a Cronbach's alpha exceeding 0.8.
Sample size
The sample size for this study was determined based on the research by Falahan et al., with a confidence level set at 95%, a test power of 80%, and an effect size of 0.65 [19]. Using G*Power (version 3.1.9.7), the total required sample size was calculated to be 78 participants. A total of 82 students were available and willing to participate, all of whom signed informed consent forms. Therefore, there were 82 participants in total, meeting the requirements outlined in the study design.
Randomization
Using a random number table method, the 82 students were divided into four groups, each comprising either 20 or 21 participants. To minimise experimental bias and interference, the random allocation was conducted by a teacher who was not informed about the specifics of this study. The groups were designated as Group A (n = 20), Group B (n = 21), Group C (n = 21), and Group D (n = 20). Group A received CBL teaching assisted by VR technology, Group D underwent traditional CBL teaching, Group B received VR technology assistance in anatomy courses only, and Group C applied VR technology assistance in physiotherapy courses only.
Blinding
Students were partially blinded in the study as they were assigned numbers without being informed of their significance. To ensure educational equity, the same instructor taught all groups, resulting in the instructors not being blinded. To reduce errors and bias, the teacher responsible for statistical analysis was blinded to the group assignments.
Statistical methods
Data analysis commenced with the Shapiro–Wilk test to ascertain the normality of continuous variables, setting the stage for appropriate statistical testing. For normally distributed data, comparisons were conducted using independent sample t-tests, one-way Analysis of Variance (ANOVA), and chi-square tests. Alternatively, non-normally distributed data were analyzed using Mann–Whitney and Kruskal–Wallis H tests, adhering to a statistical significance threshold of P < 0.05. The reliability of Likert scale responses was assessed via the Cronbach's alpha coefficient, ensuring the internal consistency of survey instruments. All statistical procedures were executed in SPSS software (Version 29.0).
Results
Baseline characteristics
Table 1 presents the demographic data of the undergraduates participating in this study. There were no significant differences between Groups A, B, C, and D in terms of age, gender, and theoretical test scores (P > 0.05). The mean age of all participants was 20.43 years, with a standard deviation of 0.65.
Table 1.
Baseline characteristics
| Characteristic | Group A (n = 20) |
Group B (n = 21) |
Group C (n = 21) |
Group D (n = 20) |
Statistics | P-value |
|---|---|---|---|---|---|---|
| Age | 20.15 (0.59) | 20.43 (0.51) | 20.48 (0.75) | 20.65 (0.67) | H = 5.419 | 0.144 |
| Gender | ||||||
| Men | 4 | 6 | 6 | 6 | Χ2 = 0.643 | 0.887 |
| Women | 16 | 15 | 15 | 14 | ||
| Test0 score | 82.70 (6.06) | 84.76 (5.35) | 82.95 (5.99) | 83.80 (6.65) | F = 0.497 | 0.685 |
Test0 score is the pretest
Outcomes and data analysis
Test scores evaluation
In the theoretical tests, there were no significant differences in the scores of students between groups (P > 0.05), indicating comparability in statistical terms.
Overall, compared to the pure CBL teaching method, VR + CBL demonstrated a significant advantage in the test scores for the anatomy course, although there was no statistical difference in the treatment course test scores (Table 2).
Table 2.
Comparison of the test scores between the VR + CBL and CBL
| VR + CBL (n = 41) |
CBL (n = 41) |
t value | P value | |
|---|---|---|---|---|
| Test1 score, mean (SD) | 87.71 (5.60) | 82.59 (6.64) | 3.778 | < 0.001 |
| Test2 score, mean (SD) | 81.85 (5.99) | 79.02 (7.57) | 1.878 | 0.064 |
Specific analysis: In the anatomy course, the groups using VR + CBL (Groups A and B) outperformed those using CBL (Groups C and D), demonstrating a significant effect of VR. In Test 1, Group A achieved superior results compared to Group B, which in turn surpassed Group D, while Group D marginally exceeded Group C in their overall scores. There was no statistically significant difference in scores between Group A and Group B (P > 0.05), nor between Group C and Group D (P > 0.05). However, the scores of Group A were significantly higher than those of Groups C and D (P < 0.05), and the scores of Group B were also significantly higher than those of Groups C and D (P < 0.05) (Table 3).
Table 3.
Comparison of the test scores between the group A, B, C, D
| Group A (VR + CBL) (n = 20) |
Group B (VR anatomy + CBL) (n = 21) |
Group C (VR physiotherapy + CBL) (n = 21) |
Group D (CBL) (n = 20) |
|
|---|---|---|---|---|
| Test0 score | 82.70 (6.06) | 84.76 (5.35) | 82.95 (5.99) | 83.80 (6.65) |
| Test1 score | 88.00 (5.62) | 87.43 (5.70) | 82.57 (5.90) a, b | 82.60 (7.49)a, b |
| Test2 score | 82.30 (5.92) | 81.43 (6.17) | 80.29 (8.75) | 77.70 (6.03)a |
| Test3 score1 | 17.50 (2.67) | 16.00 (2.00)a | 16.90 (2.05) | 15.65 (3.07)a |
Test score = Mean (SD). a = Compared with group A, P < 0.05. b = Compared with group B, P < 0.05. 1 Total score is 22
In the rehabilitation therapy course, Group A, which consistently used VR + CBL, achieved the highest scores, while Group D, which always used CBL, scored the lowest. Interestingly, the scores of Group C, which also employed VR + CBL, were lower than those of Group B, which used CBL. The analysis revealed a hierarchical score across the groups, with Group A leading, followed sequentially by Group B, Group C, and Group D, reflecting a gradation in achievement from highest to lowest. The scores of Group A were significantly higher than those of Group D (P < 0.05), but the differences in scores between the other groups were not statistically significant (P > 0.05) (Table 3).
In the final test, the results demonstrated a clear sequence in score rankings, with Group A leading, followed by Group C, Group B, and Group D in descending order. The difference in scores between Group A and Group D was statistically significant (P < 0.05), while the differences between Group B and Group D, as well as between Group C and Group D, were not statistically significant (P > 0.05) (Table 3).
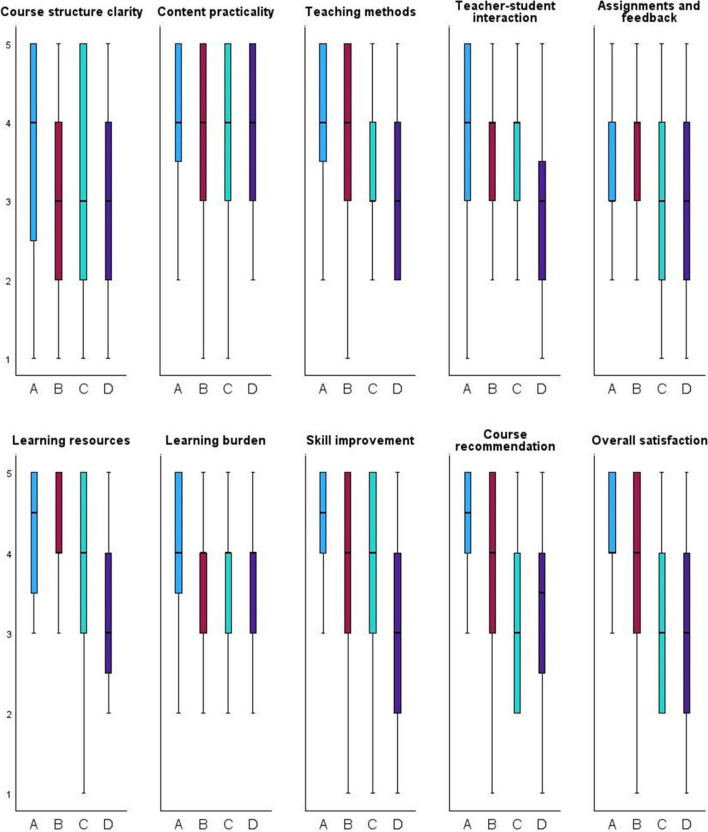
Student questionnaire evaluation
After the final test, student questionnaires were distributed and collected, resulting in 82 returned questionnaires and a 100% response rate. Analysis using the Kruskal–Wallis H test revealed significant differences (P < 0.05) among groups in six key areas: teaching methods, teacher-student interaction, learning resources, skill improvement, course recommendation, and overall satisfaction (Fig. 3). On the other hand, there were no significant differences (P > 0.05) regarding course structure clarity, content practicality, assignments and feedback, and learning burden (Table 4).
Fig. 3.
Student questionnaire evaluation
Table 4.
Student questionnaire evaluationa
| H value | P value | |
|---|---|---|
| Course structure clarity | 1.914 | 0.590 |
| Content practicality | 2.095 | 0.553 |
| Teaching methods | 8.987 | 0.030 |
| Teacher-student interaction | 11.679 | 0.009 |
| Assignments and feedback | 1.785 | 0.686 |
| Learning resources | 10.321 | 0.034 |
| Learning burden | 2.720 | 0.449 |
| Skill improvement | 11.107 | 0.015 |
| Course recommendation | 10.273 | 0.045 |
| Overall satisfaction | 13.366 | 0.007 |
Discussion
This study employed a variety of statistical methodologies to investigate the impact of VR + CBL on the learning outcomes of medical students. Statistical analyses revealed that in anatomy tests, Groups A and B, who utilized Virtual Reality technology, significantly outperformed Groups C and D, who did not use VR. This difference underscores the effectiveness of VR technology in enhancing students' mastery of the anatomy of the shoulder joint. It also validates the viability of substituting traditional CBL with VR + CBL in the field of anatomy [14]. However, in the rehabilitation therapy tests, although the VR group scored higher on average, the difference was not statistically significant, indicating that the impact of VR technology varies across different educational domains [30].
In order to deepen our understanding of these differences, we provide detailed descriptions of two VR learning environments. The VR environment for anatomy was specifically designed to simulate the three-dimensional structure of the shoulder joint, enabling students to gain a deeper understanding of various anatomical structures through interactive manipulation. The corresponding anatomy knowledge tests primarily assess students' ability to identify and understand these structures. Existing experiments have found that Virtual Reality is more effective in enhancing medical anatomy learning outcomes than traditional methods [15].
In the field of rehabilitation therapy, the VR environment simulates the rehabilitation process; however, these simulated scenarios may not align precisely enough with the post-test content on rehabilitation therapy knowledge, which affects the significance of the learning outcomes.
Another possible explanation is the high complexity of learning in rehabilitation therapy, which requires more practical operation and the accumulation of experience. Current VR technology may not yet fully replicate this complexity. Therefore, although VR technology provides a novel teaching method, its applicability and effectiveness may vary across different disciplines due to the specific requirements and complexities of the course content [31].
It is noteworthy to compare the performances of Group A (VR + CBL) and Group D (traditional CBL) across the anatomy and rehabilitation therapy tests: students in Group A consistently outperformed those in Group D. This suggests that Virtual Reality technology enables students to immerse themselves in an interactive artificial world, providing a more intuitive learning experience and deepening their understanding of complex shoulder joint structures and treatment methods [32]. These findings demonstrate that the educational model VR + CBL surpasses traditional simulation practices in educational outcomes, highlighting the potential to enhance learning effectiveness [33].
The comparison between Group B (using Virtual Reality only in the anatomy course) and Group C (using Virtual Reality only in the rehabilitation therapy course) revealed varying learning outcomes, reflecting the suitability and effectiveness of Virtual Reality technology across different educational contents [33]. Specifically, the application of Virtual Reality technology in anatomy learning may be more effective than in rehabilitation therapy learning [14, 31]. This difference not only underscores the necessity of flexibly applying and developing Virtual Reality technology in medical education but also highlights the importance of anatomical knowledge as a foundational basis for learning in rehabilitation therapy [34].
Further analysis indicates that the group integrating Virtual Reality technology comprehensively (Group A) consistently achieved higher scores across all tests than other groups. These findings confirm the significant positive impact of the comprehensive application of Virtual Reality technology on the overall learning outcomes of students [5, 30]. Statistical results show that VR + CBL significantly enhances students' acquisition of knowledge and skills in shoulder joint anatomy and rehabilitation therapy, emphasizing the potential value of Virtual Reality technology in providing immersive and interactive learning experiences in medical education [35, 36]. The study by Fink et al. has also demonstrated the efficacy of integrating teaching support into case-based learning, and that such support can significantly enhance learning success [37]. In addition, VR might also be useful to include support for anatomy curricula that lack resources like donor-based dissection.
The results of the questionnaire survey corroborated the findings of the statistical analysis. In terms of teaching methods, the groups using Virtual Reality technology (Groups A and B) received higher evaluations than the traditional Case-Based Learning group (Group D) and the partially VR-integrated group (Group C). This suggests that students perceive the integration of Virtual Reality technology as significantly enhancing the effectiveness of teaching methods, particularly in fostering intuitive understanding and practical operation [38, 39]. This finding is consistent with the improvements in learning outcomes and further validates the role of Virtual Reality technology in enhancing the quality of medical education [33]. Studies have shown that, compared to traditional methods, VR technology in education has increased test scores, satisfaction, and enjoyment, although it has not significantly reduced the time taken to complete tests [16].
In terms of teacher-student interaction and learning resources, students using VR technology reported higher satisfaction. This may be because the VR environment offers more opportunities for interaction between teachers and students, such as direct guidance and feedback in virtual scenarios, while also increasing student participation through virtual case discussions [5]. Additionally, VR technology enriches learning resources by simulating complex medical scenarios in the real world, reducing resource consumption and thereby improving teaching effectiveness [40].
Feedback on skill improvement indicated that the VR + CBL teaching method not only strengthened the learning of theoretical knowledge but, more importantly, enhanced students' practical operational abilities [10, 12]. This is particularly evident in physical therapy and clinical decision-making training, where students can repeatedly practice in a safe virtual environment, thereby deepening their understanding and application of course content [41]. Furthermore, the high course recommendation rate reflects students' recognition and satisfaction with the VR + CBL method, highlighting its potential impact and applicability in future medical education [42].
Students expressed high overall satisfaction with the VR + CBL method, further emphasising its popularity as a teaching approach. They universally believe that this innovative method enhances enjoyment, interactivity, and effectiveness in learning through its realistic virtual environments, marking it as a promising educational strategy [43]. Studies by Fink (2023) and others also confirm that VR education exhibits higher system usability and satisfaction [7]. This positive feedback supports the further development and application of Virtual Reality technology in medical education, particularly in skill-intensive and highly specialised medical fields [42, 44].
The survey results provide valuable insights, indicating that the introduction of VR technology not only improves students' learning outcomes and skills but also significantly enhances student satisfaction and participation [5, 30, 35]. Future research should further explore effective integration of VR technology with case-based learning methods, customising them according to different medical specialties and course content to enhance students' immersion and participation, thereby maximising teaching effectiveness and student satisfaction [45]. Additionally, research should consider the impact of introducing VR technology on the roles of teachers, teaching methods, and students' self-learning abilities [25].
Despite providing valuable insights into the application of Virtual Reality technology in medical education, this study faces several major limitations that might affect the universality and interpretation of the findings [46].
The sample size of the study was relatively small, which could limit the generalisability of our conclusions. Although an efficacy analysis was conducted to ensure that the sample size was sufficient to detect significant differences between teaching methods, a smaller sample may not fully represent the diverse population of medical students. Moreover, the diversity of the sample—such as educational background, grade level, and prior VR experience—was not thoroughly explored, which are factors that could influence the effectiveness of VR learning.
The scope of application for Virtual Reality technology was limited in this study. While we explored the use of VR in anatomy and rehabilitation therapy education, it did not extend to other medical fields, such as surgical procedures or clinical decision-making training, where the potential benefits of VR might differ. Expanding the scope of VR application could reveal a broader educational impact.
This study primarily focused on short-term learning outcomes, without assessing the long-term retention of knowledge and development of clinical skills by students. The impact of Virtual Reality technology on long-term memory retention and skill preservation is a crucial aspect of evaluating its true value in education.
In conclusion, to overcome these limitations and deepen our understanding of the innovative applications of Virtual Reality technology in medical education, future research should expand the sample size, increase sample diversity, explore the use of VR technology across a broader range of medical fields, and conduct longitudinal studies. These measures will facilitate a more accurate assessment of the educational benefits of Virtual Reality technology and its long-term impact on the development of students' clinical skills [39, 43, 47].
Conclusions
This study underscores the effectiveness of integrating VR with CBL in medical education, highlighting the achievements in student engagement, knowledge retention, and skill development, especially in the treatment of the shoulder joint. Despite the limited scope of the study and the small sample size, the results advocate for a broader application of VR technology in medical training subjects. The study suggests that by incorporating virtual reality into medical courses, it is possible to closely combine educational experience with the complexity of clinical practice, better preparing future medical professionals. This represents a significant advancement in the evolution of medical education methods.
Acknowledgements
The completion of this research was made possible by the collaborative efforts and selfless contributions of many parties. First and foremost, we would like to express our deepest gratitude to the 82 students who participated in this study. With informed consent, they not only actively cooperated with the research requirements and accepted the change of being rearranged into new learning groups from their original class structure, but also demonstrated a high level of enthusiasm and engagement in learning, which was crucial to the smooth progress of this research. We also extend our thanks to the participating professors and two professional teachers. Not only did they provide support for the experiment amidst their busy teaching schedules, but they also actively adopted the new teaching methods proposed in this study. Their professional knowledge and teaching experience provided a solid foundation for the implementation of this research and also added a guarantee for the learning outcomes of the students. To ensure the objectivity of the evaluation and the independence of data analysis, we specifically invited three teachers who were not involved in the course instruction to be responsible for the statistical work of test scores and questionnaires, and invited teachers from other teaching units to be responsible for the analysis work. They completed this task without any prior knowledge, ensuring the fairness and scientific nature of the data processing. We sincerely appreciate their diligent work and dedication.
Authors’ contributions
(I) Conception and design: All authors; (II) Administrative support: YH, XY L and GZ; (III) Provision of study materials: XY L, YH and GZ; (IV) Collection and assembly of data: ZL W, XM, ZH L and SL X; (V) Data analysis and interpretation: NY S, YN Z; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Funding
Education Program of Social Science Planning Funding of Liaoning China (L21CED010).
Medical Education Research Program of Liaoning China (No.2022-N004-06).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This research received approval from the Ethics Committee of Shengjing Hospital of China Medical University (2024PS112K). Conducted in adherence to the Declaration of Helsinki, this study ensures the anonymity of all participants, secures informed consent from all involved, and communicates the right to withdraw from the study at any time without facing any adverse effects for choosing not to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yu He, Ziliang Wang and Nianyi Sun contributed to the work equally and should be regarded as co-first authors.
References
- 1.Mahtab EAF, Egorova AD. Current and future applications of virtual reality technology for cardiac interventions. Nat Rev Cardiol. 2022;19(12):779–80. 10.1038/s41569-022-00789-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakshi SK, Lin SR, Ting DSW, Chiang MF, Chodosh J. The era of artificial intelligence and virtual reality: transforming surgical education in ophthalmology. Br J Ophthalmol. 2021;105(10):1325–8. 10.1136/bjophthalmol-2020-316845. [DOI] [PubMed] [Google Scholar]
- 3.Rudran B, Logishetty K. Virtual reality simulation: a paradigm shift for therapy and medical education. Br J Hosp Med (Lond). 2018;79(12):666–7. 10.12968/hmed.2018.79.12.666. [DOI] [PubMed]
- 4.Makransky G, Petersen G. The cognitive affective model of immersive learning (CAMIL): a theoretical research-based model of learning in immersive virtual reality. Educ Psychol Rev. 2024;33(3):937–58. 10.1007/s10648-020-09586-2. [Google Scholar]
- 5.Sidhu M, Dulai V. What do medical students think about incorporating VR into psychiatry education and training? BJPsych Open. 2022;8(S1):S35. 10.1192/bjo.2022.153. [Google Scholar]
- 6.Chen G, Zhao Y, Xie F, Shi W, Yang Y, Yang A, et al. Educating outpatients for bowel preparation before colonoscopy using conventional methods vs virtual reality videos plus conventional methods: a randomized clinical trial. JAMA Netw Open. 2021;4(11):e2135576. 10.1001/jamanetworkopen.2021.35576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fink MC, Eisenlauer V, Ertl B. What variables are connected with system usability and satisfaction? Results from an educational virtual reality field trip. Computers & Education: X Reality. 2023;100043. 10.1016/j.cexr.2023.100043.
- 8.Jin C, Dai L, Wang T. The application of virtual reality in the training of laparoscopic surgery: a systematic review and meta-analysis. Int J Surg. 2021;87:105859. 10.1016/j.ijsu.2020.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Pfeil A, Klemm P, Hueber AJ, Hoffmann T, Weise T, Oelzner P, et al. Enhancing student understanding of rheumatic disease pathologies through augmented reality: findings from a multicentre trial. Rheumatology (Oxford). 2023;kead508. 10.1093/rheumatology/kead508. [DOI] [PubMed]
- 10.Lin JC, Yu Z, Scott IU, Greenberg PB. Virtual reality training for cataract surgery operating performance in ophthalmology trainees. Cochrane Database Syst Rev. 2021;12(12):CD014953. 10.1002/14651858.CD014953.pub2. [DOI] [PMC free article] [PubMed]
- 11.Emmelkamp PMG, Meyerbröker K. Virtual reality therapy in mental health. Annu Rev Clin Psychol. 2021;17:495–519. 10.1146/annurev-clinpsy-081219-115923. [DOI] [PubMed] [Google Scholar]
- 12.Alvarez-Lopez F, Maina MF, Saigí-Rubió F. Use of a low-cost portable 3D virtual reality gesture-mediated simulator for training and learning basic psychomotor skills in minimally invasive surgery: development and content validity study. J Med Internet Res. 2020;22(7):e17491. 10.2196/17491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wismer P, Lopez Cordoba A, Baceviciute S, Clauson-Kaas F, Sommer MOA. Immersive virtual reality as a competitive training strategy for the biopharma industry. Nat Biotechnol. 2021;39(1):116–9. 10.1038/s41587-020-00784-5. [DOI] [PubMed] [Google Scholar]
- 14.Kurul R, Ögün MN, Neriman Narin A, Avci Ş, Yazgan B. An alternative method for anatomy training: immersive virtual reality. Anat Sci Educ. 2020;13(5):648–56. 10.1002/ase.1959. [DOI] [PubMed] [Google Scholar]
- 15.Zhao J, Xu X, Jiang H, Ding Y. The effectiveness of virtual reality-based technology on anatomy teaching: a meta-analysis of randomized controlled studies. BMC Med Educ. 2020;20(1):127. 10.1186/s12909-020-1994-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J, Li W, Dun A, Zhong N, Ye Z. 3D visualization technology for Learning human anatomy among medical students and residents: a meta- and regression analysis. BMC Med Educ. 2024;24(1):461. 10.1186/s12909-024-05403-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vogt A, Albus P, Seufert T. Learning in virtual reality: bridging the motivation gap by adding annotations. Front Psychol. 2021;12:645032. 10.3389/fpsyg.2021.645032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andreasen EM, Berg H, Steinsbekk A, Høigaard R, Haraldstad K. The effect of using desktop VR to practice preoperative handovers with the ISBAR approach: a randomized controlled trial. BMC Med Educ. 2023;23(1):983. 10.1186/s12909-023-04966-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falahan SN, Habibi E, Kamyari N, Yousofvand V. Impact of virtual problem-based learning of cardiopulmonary resuscitation on fourth-year nursing students’ satisfaction and performance: a quasi-experimental study. BMC Med Educ. 2024;24(1):425. 10.1186/s12909-024-05375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ha H, Lopez T. Developing health literacy knowledge and skills through case-based learning. AM J PHARM EDUC. 2014;78(1):17. 10.5688/ajpe78117.. [DOI] [PMC free article] [PubMed]
- 21.Fink MC, Reitmeier V, Stadler M, Siebeck M, Fischer F, Fischer MR. Assessment of diagnostic competences with standardized patients versus virtual patients: experimental study in the context of history taking. J Med Internet Res. 2021;23(3):e21196. 10.2196/21196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makransky G, Terkildsen T, Mayer R. Adding immersive virtual reality to a science lab simulation causes more presence but less learning. Learn Instr. 2019;60:225–36. 10.1016/j.learninstruc.2017.12.007. [Google Scholar]
- 23.Wainman B, Aggarwal A, Birk SK, Gill JS, Hass KS, Fenesi B. Virtual dissection: an interactive anatomy learning tool. Anat Sci Educ. 2021;14(6):788–98. 10.1002/ase.2035. [DOI] [PubMed] [Google Scholar]
- 24.Babini MH, Kulish VV, Namazi H. Physiological state and learning ability of students in normal and virtual reality conditions: complexity-based analysis. J Med Internet Res. 2020;22(6):e17945. 10.2196/17945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilkerson M, Maldonado V, Sivaraman S, Rao RR, Elsaadany M. Incorporating immersive learning into biomedical engineering laboratories using virtual reality. J Biol Eng. 2022;16(1):20. 10.1186/s13036-022-00300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eichel VM, Brandt C, Brandt J, Jabs JM, Mutters NT. Is virtual reality suitable for hand hygiene training in health care workers? Evaluating an application for acceptability and effectiveness. Antimicrob Resist Infect Control. 2022;11(1):91. 10.1186/s13756-022-01127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Albus P, Vogt A, Seufert T. Signaling in virtual reality influences learning outcome and cognitive load. Comput Educ. 2021;166:104154. 10.1016/j.compedu.2021.104154. [Google Scholar]
- 28.Malik TG, Mahboob U, Khan RA, Alam R. Virtual patients versus standardized patients for improving clinical reasoning skills in ophthalmology residents. A randomized controlled trial. BMC Med Educ. 2024;24(1):429. 10.1186/s12909-024-05241-4. [DOI] [PMC free article] [PubMed]
- 29.Wainman B, Pukas G, Wolak L, Mohanraj S, Lamb J, Norman GR. The critical role of stereopsis in virtual and mixed reality learning environments. Anat Sci Educ. 2020;13(3):401–12. 10.1002/ase.1928. [DOI] [PubMed] [Google Scholar]
- 30.Chen FQ, Leng YF, Ge JF, Wang DW, Li C, Chen B, et al. Effectiveness of virtual reality in nursing education: meta-analysis. J Med Internet Res. 2020;22(9):e18290. 10.2196/18290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birbara NS, Sammut C, Pather N. Virtual reality in anatomy: a pilot study evaluating different delivery modalities. Anat Sci Educ. 2020;13(4):445–57. 10.1002/ase.1921. [DOI] [PubMed] [Google Scholar]
- 32.Chuan A, Zhou JJ, Hou RM, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021;76(5):695–704. 10.1111/anae.15202. [DOI] [PubMed] [Google Scholar]
- 33.Rourke S. How does virtual reality simulation compare to simulated practice in the acquisition of clinical psychomotor skills for pre-registration student nurses? A systematic review. Int J Nurs Stud. 2020;102:103466. 10.1016/j.ijnurstu.2019.103466. [DOI] [PubMed] [Google Scholar]
- 34.Tortora C, Di Crosta A, La Malva P, Prete G, Ceccato I, Mammarella N, et al. Virtual reality and cognitive rehabilitation for older adults with mild cognitive impairment: A systematic review. Ageing Res Rev. 2024;93:102146. 10.1016/j.arr.2023.102146. [DOI] [PubMed] [Google Scholar]
- 35.Parmar D, Lin L, DSouza N, Jorg S, Leonard AE, Daily SB, et al. How immersion and self-avatars in VR affect learning programming and computational thinking in middle school education. IEEE Trans Vis Comput Graph. 2023;29(8):3698–713. 10.1109/TVCG.2022.3169426. [DOI] [PubMed]
- 36.Fazlollahi AM, Bakhaidar M, Alsayegh A, Yilmaz R, Winkler-Schwartz A, Mirchi N, et al. Effect of artificial intelligence tutoring vs expert instruction on learning simulated surgical skills among medical students: a randomized clinical trial. JAMA Netw Open. 2022;5(2):e2149008. 10.1001/jamanetworkopen.2021.49008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fink MC, Heitzmann N, Siebeck M, Fischer F, Fischer MR. Learning to diagnose accurately through virtual patients: do reflection phases have an added benefit? BMC Med Educ. 2021;21(1):523. 10.1186/s12909-021-02937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsukada K, Yasui Y, Miyata S, Fuyumuro J, Kikuchi T, Mizuno T, et al. Effectiveness of virtual reality training in teaching personal protective equipment skills: a randomized clinical trial. JAMA Netw Open. 2024;7(2):e2355358. 10.1001/jamanetworkopen.2023.55358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Latif H, Baez Sosa V, Segal Kersun L, Loren A, Groninger H, Shenoy A. Using virtual reality to promote mindfulness among medical trainees; a study of feasibility and acceptance. Blood. 2020;136(Supple 1):39. 10.1182/blood-2020-136701.
- 40.Harfouche AL, Nakhle F. Creating bioethics distance learning through virtual reality. Trends Biotechnol. 2020;38(11):1187–92. 10.1016/j.tibtech.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Canning CG, Allen NE, Nackaerts E, Paul SS, Nieuwboer A, Gilat M. Virtual reality in research and rehabilitation of gait and balance in Parkinson disease. Nat Rev Neurol. 2020;16(8):409–25. 10.1038/s41582-020-0370-2. [DOI] [PubMed] [Google Scholar]
- 42.Reymus M, Liebermann A, Diegritz C. Virtual reality: an effective tool for teaching root canal anatomy to undergraduate dental students - a preliminary study. Int Endod J. 2020;53(11):1581–7. 10.1111/iej.13380. [DOI] [PubMed] [Google Scholar]
- 43.Kim HJ, Lee HK, Jang JY, Lee KN, Suh DH, Kong HJ, et al. Immersive virtual reality simulation training for cesarean section: a randomized controlled trial. Int J Surg. 2024;110(1):194–201. 10.1097/JS9.0000000000000843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Orser BA, Spadafora SM. Competence-based training and immersion virtual reality: paradigm-shifting advances in medical education. Anesth Analg. 2022;135(2):220–2. 10.1213/ANE.0000000000006116. [DOI] [PubMed] [Google Scholar]
- 45.Sousa CV, Hwang J, Cabrera-Perez R, Fernandez A, Misawa A, Newhook K, et al. Active video games in fully immersive virtual reality elicit moderate-to-vigorous physical activity and improve cognitive performance in sedentary college students. J Sport Health Sci. 2022;11(2):164–71. 10.1016/j.jshs.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsai TY, Onuma Y, Złahoda-Huzior A, Kageyama S, Dudek D, Wang Q, et al. Merging virtual and physical experiences: extended realities in cardiovascular medicine. Eur Heart J. 2023;44(35):3311–22. 10.1093/eurheartj/ehad352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bond S, Laddu DR, Ozemek C, Lavie CJ, Arena R. Exergaming and virtual reality for health: implications for cardiac rehabilitation. Curr Probl Cardiol. 2021;46(3):100472. 10.1016/j.cpcardiol.2019.100472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.