Abstract
Background
This study examined psychiatric hospitalisation patterns in San Salvatore Hospital in L’ Aquila (Italy), during two major crises: the 2009 earthquake and the COVID-19 pandemic lockdown. The investigation spans two four-year periods, from 2008 to 2011 and from 2019 to 2022, with a focus on the trimester around the earthquake and the first wave/lockdown of the pandemic.
Methods
We analysed weekly psychiatric unit admissions of adults diagnosed with schizophrenia spectrum disorder, major depression, bipolar disorder, and alcohol/substance use disorder. Four-year periods around the Earthquake and COVID-19 Lockdown were divided into sixteen trimesters, and Generalised linear models were used to analyse the relationship between weekly hospitalisation frequency and trimesters by diagnosis using a Poisson distribution.
Results
A total of 1195 and 1085 patients were admitted to the psychiatric ward in the 2008–2011 and 2019–2022 periods, respectively. Weekly hospitalisations in the earthquake trimester were lower than during the previous one for all diagnoses (schizophrenia spectrum: −41.9%, p = 0.040; major depression: −56.7%, p = 0.046; bipolar disorder: −69.1%, p = 0.011; alcohol/substance use disorder: −92.3%, p = 0.013). This reduction persisted for 21, 18, and 33 months after the earthquake for schizophrenia spectrum, bipolar, and alcohol/substance use disorders, respectively. Contrarily, patterns of weekly admissions around the COVID-19 lockdown remained substantially stable in the short term. However, a consistent long-term hospitalisation increase for all diagnoses characterised the first half of 2022 (the cessation of anti-COVID-19 measures; schizophrenia spectrum: +68.6%, p = 0.014; major depression: +133.3%, p = 0.033; bipolar disorder: +180.0%, p = 0.034; alcohol/substance use disorder: +475.0%, p = 0.001).
Conclusions
The present study indicated that exposure to major health crises can have both short- and long-term effects on psychiatric ward admission, holding significant implications for current and future major health emergency management strategies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06078-3.
Keywords: Trauma and stressor related disorders; Earthquakes; Natural disasters; Patient admission; SARS-CoV-2; COVID-19; Pandemics; Mental health; Resilience, psychological
Background
As humans worldwide face catastrophic events and their consequences daily, disaster management represents an urgent challenge for global health [1]. Catastrophic events can be natural, such as hurricanes, earthquakes, floods, pandemics [2], or man-made disasters, like war, terrorist attacks or radiation emergencies [3]. Following a crisis or a calamity, changes in health services utilisation patterns are commonly observed [4, 5], also due to access restrictions to healthcare facilities [6]. Moreover, an event may directly affect the population’s health, and its consequences may also be reflected by short- and long-term effects on the mental health of individuals, with potential repercussions on admission patterns to psychiatric wards [7–9]. An example of such a phenomenon was reported by Beaglehole and colleagues, who described a decrease in admission rates in the acute psychiatric wards over the 18 months following the Christchurch earthquakes in New Zealand [10]. Comparable observations were made several decades ago following the bombing that destroyed the city of London in 1940 [11]. However, the reduction in admission rates following a natural disaster may last only for the first period after the traumatic event, and the utilisation of health services may significantly increase again after a few months or years [12]. Conversely, Sakuma et al. (2018), who analysed the admission rates in two different psychiatric hospitals following the 2011 Great East Japan earthquake, highlighted an initial increase in admissions in the four weeks following the event [13]. Such results were also observed by Aoki and colleagues (2012), who reported an increase in compulsory treatment hospitalisations after the Great East Japan earthquake, particularly of patients diagnosed with schizophrenia [14].
At 3:32 am, on the 6th of April 2009, a 6.3 Mw earthquake devastated the city of L’ Aquila (Italy), and its surroundings, killing 309 people and injuring more than 1600. Several studies have been conducted on the earthquake’s acute, medium, and long-term mental health effects [15–19]. However, only a few studies observed admissions to the L’ Aquila psychiatric unit, and they mainly focused on the first months post-earthquake [20, 21]. Specifically, Pollice et al. (2010) observed that among admitted patients diagnosed with schizophrenia, nine patients (15%) met the criteria for Post-traumatic stress disorder and showed more severe positive symptoms and impairment in working memory [21]. However, this study does not provide data regarding specific admissions patterns over time.
Recently, the COVID-19 pandemic represented another catastrophic event that significantly impacted the population’s mental health, primarily because of the adopted restrictive measures to limit the virus spread [22–24]. In Italy, such measures included a national lockdown, the first and longest occurring from March 11th 2020, to May 4th, 2020 [25], followed by other and shorter lockdowns, preventive measures and curfews that lasted until the end of 2021.
Several studies investigated how this event influenced psychiatric hospital admissions and service utilisation [26–31]. Bonello et al. (2021), in a study carried out at the Malta Psychiatric Hospital, observed a decrease in inward admissions, specifically for depressive or anxiety disorders, a marked decrease in substance abuse admissions, but an increase in compulsory treatments [27]. In Italy, a study that analysed data on admissions in psychiatric wards in 12 different Italian regions compared data from the pre-lockdown period (i.e. 2018 and 2019), the lockdown (i.e. March 1st -April 30th, 2020) and post-lockdown (i.e. May 1st -June 30th, 2020), and reported a drastic decline in psychiatric admissions during the lockdown [28]. However, the study showed that the reduction was temporary, as in the two months following the lockdown, the hospitalization rate returned to pre-lockdown levels, with the exception of the elderly population (aged > 65 years) [28].
Another study by Dionisie et al. (2022) focused on the effect of the COVID-19 pandemic on hospital admissions in psychiatric departments according to diagnosis [32]. The study describes decreasing trends of hospitalisation for schizophrenia, acute psychotic disorder, depressive, and bipolar disorders during the imposition of lockdown measures, followed by an increase in admissions for psychotic and mood disorders occurring after the dissolution of the lockdown measures, although never exceeding pre-lockdown levels [32].
Despite the significant number of studies conducted on the effects of the L’ Aquila earthquake on mental health, no study has analysed how it influenced patterns of admissions in the psychiatric unit over a prolonged period. To the best of our knowledge, no Italian research has compared the impact of different catastrophic events on psychiatric unit admissions. Noteworthy, only the study by Vukojević and colleagues (2021) compared two catastrophic events regarding admissions to psychiatric wards in Zagreb: the Spanish flu pandemic and the COVID-19 pandemic [33]. Authors found a slight dip in acute psychiatric admissions when compared to a three-year period average before for both pandemics. The currently available literature provides conflicting results, and the potential impact of different traumatic events on hospitalisation rates, specifically in a psychiatric unit, has not been completely elucidated.
In such context, this study aims to analyse the trend of hospitalisations in the psychiatric ward (SPUDC – Servizio Psichiatrico Universitario di Diagnosi e Cura) of the “San Salvatore” Hospital of L’ Aquila (Italy) during the four-year period 2008–2011 and 2019–2022, with a focus on the second quarter of 2009 (L’ Aquila earthquake) and 2020 (COVID-19 lockdown/first wave). Temporal patterns of discharge diagnosis, compulsory admission, hospitalisation length, sociodemographic data, and the total number of patients admitted have been analysed to understand whether and how the two traumatic events influenced the trend of hospitalisations.
Methods
Participants and data extraction
We retrieved all discharge summaries (Scheda di Dimissione Ospedaliera, SDO) regarding the psychiatric ward from the archives of the “San Salvatore” Hospital in L’ Aquila (Italy) from 2006 to 2022.
Data from hospital discharge records included sociodemographic data, admission and discharge dates, and primary diagnosis at discharge, according to the International Classification of Diseases Version 9 (ICD-9). We used ICD-9 because our regional health information system is updated to ICD-9. Therefore, informatics systems, archives, and discharge records employ this classification system. To preserve privacy, patient identification codes were anonymised. After checking for records’ integrity and missing data, only adult patient admissions (≥ 18 years) were clustered into four diagnostic groups: schizophrenia spectrum disorder, major depression, bipolar disorder, and alcohol/substance use disorder according to ICD-9 (see Supplementary Materials Table 1). We then selected records from the four-year periods surrounding the L’ Aquila earthquake (6th of April 2009, examined period: 2008–2011) and the COVID-19 lockdown/first wave (April 2020, examined period: 2019–2022). We conventionally referred to April 2020 as the 2020 COVID-19 lockdown/first wave period to compare the same timeframe across years.
Statistical analysis
We described the composition of the overall samples (2008–2011 period: n = 1195; 2019–2022 period: n = 1085) by perfoming frequency analyses on gender (male, female), age range (18–25 years, 26–40 years, 41–60 years, > 60 years), and compulsory admission (yes, no).
We calculated the frequencies of weekly admissions for each diagnosis within the reference periods. Subsequently, each year was divided in four trimesters (1st trimester: January-February-March, 2nd trimester: April-May-June, 3rd trimester: July-August-September, 4th trimester: October-November-December), giving rise to a total of sixteen trimesters within each four-year period.
In line with the aims of the study, we analysed the relationship between the frequency of weekly admissions (dependent variable) and trimesters (predictor) for each psychiatric diagnosis employing Generalised Linear Models. Poisson distribution was employed due to the count nature of the data [34] after verifying that all models’ equidispersion assumption was satisfied (χ2/df ranging from 0.90 to 1.15) [35].
To verify potential differences in psychiatric unit admission rates before/after the traumatic event, the trimester including the earthquake (6th trimester: April-May-June 2009) or COVID-19 lockdown (6th trimester: April-May-June 2020) was used as the reference level for the trimester factor.
Finally, the mean weekly hospitalisation length was derived from admission and discharge dates. Generalised Linear Models were performed to analyse the association between weekly hospitalisation length (dependent variable) and trimesters (predictor) for each psychiatric diagnosis.
All models were fitted using the “GAMLj” (version 3.0.0) R module [36], which has also been employed to compute estimated marginal means and standard errors for graphical representation purposes (see Figs. 1 and 2). All tests were two-tailed, and a p-value < 0.05 was considered significant.
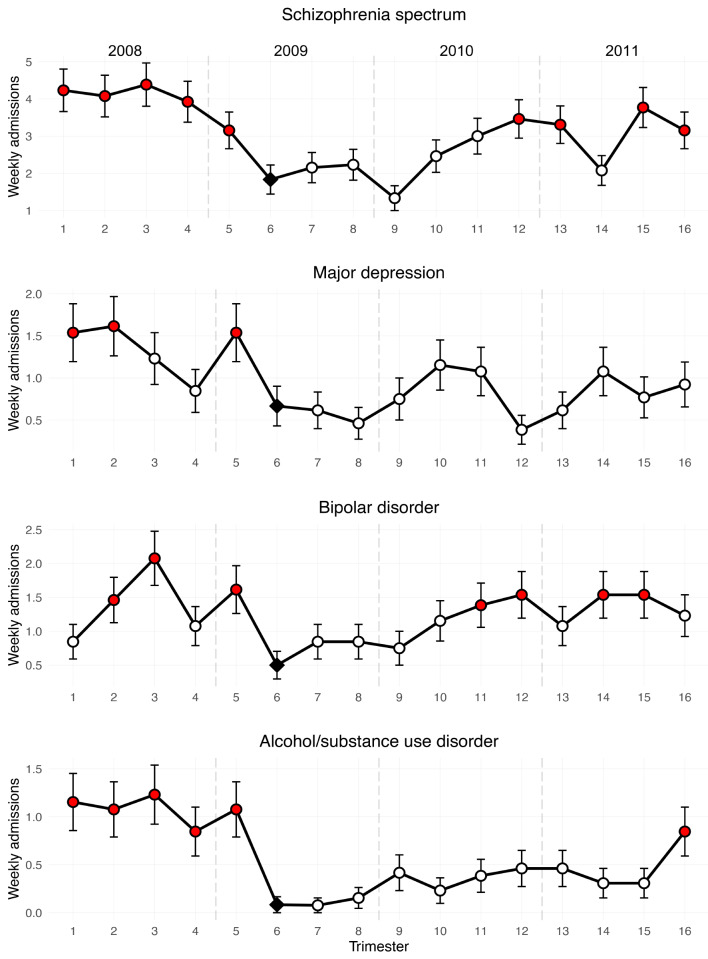
Fig. 1.
Trends in psychiatric unit admissions over a 4-year period surrounding the L’ Aquila Earthquake (trimester 6). Notes Figure reports estimated marginal means (and standard errors) from Poisson generalised linear models. Red dots indicate significant differences (p < 0.05) compared with the reference level (trimester 6, black square)
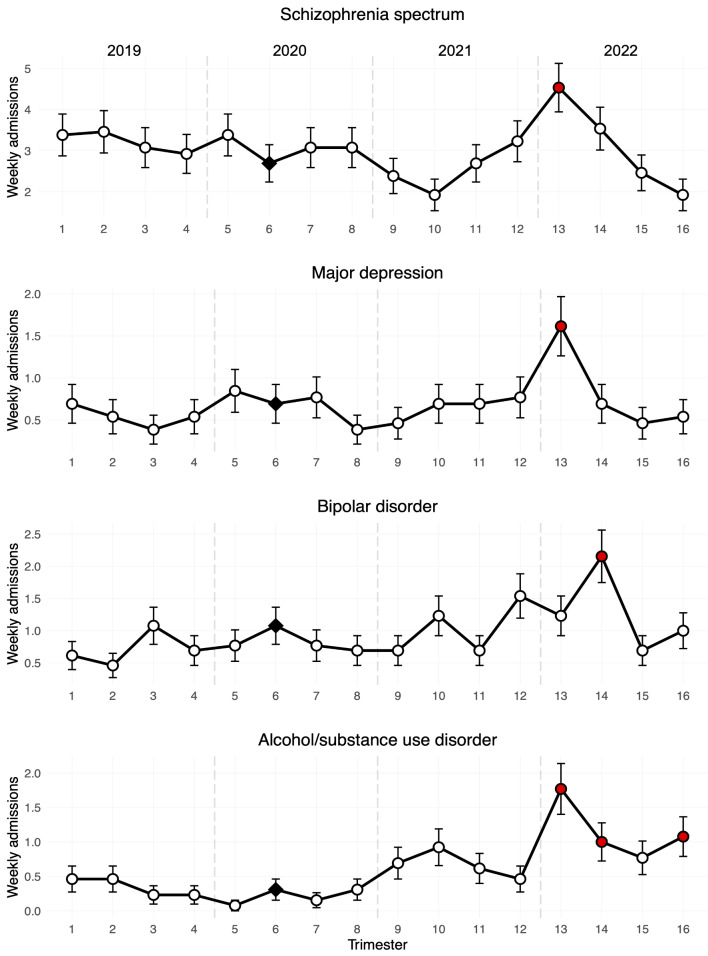
Fig. 2.
Trends in psychiatric unit admissions over a 4-year period surrounding the COVID-19 lockdown (trimester 6). Notes Figure reports estimated marginal means (and standard errors) from Poisson generalised linear models. Red dots indicate significant differences (p < 0.05) compared with the reference level (trimester 6, black square)
Results
Frequency analyses on gender, age range, and compulsory admission describing the composition of the overall samples were reported in Table 1.
Table 1.
Demographic composition of the analysed samples
| Schizophrenia spectrum | Major depression | Bipolar disorder | Alcohol/substance use disorder | Total | |
|---|---|---|---|---|---|
| 2008–2011 period [N (%)] | |||||
| Gender | |||||
| Female | 259 (41.2) | 119 (60.4) | 134 (53.2) | 31 (26.3) | 543 (45.4) |
| Male | 367 (58.4) | 77 (39.1) | 118 (46.8) | 86 (72.9) | 648 (54.2) |
| Missing | 2 (0.3) | 1 (0.5) | 0 (0) | 1 (0.8) | 4 (0.3) |
| Age (years) | |||||
| 18–25 | 43 (6.8) | 9 (4.6) | 19 (7.5) | 11 (9.3) | 82 (6.9) |
| 26–40 | 208 (33.1) | 41 (20.8) | 51 (20.2) | 38 (32.2) | 338 (28.3) |
| 41–60 | 237 (37.7) | 68 (34.5) | 107 (42.5) | 38 (32.2) | 450 (37.7) |
| > 60 | 104 (16.6) | 65 (33) | 62 (24.6) | 22 (18.6) | 253 (21.2) |
| Missing | 36 (5.7) | 14 (7.1) | 13 (5.2) | 9 (7.6) | 72 (6.0) |
| Compulsory admission | |||||
| Yes | 67 (10.7) | 18 (9.1) | 19 (7.5) | 9 (7.6) | 113 (9.5) |
| No | 561 (89.3) | 179 (90.9) | 233 (92.5) | 109 (92.4) | 1082 (90.5) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hospitalization length by weekly admission [mean days (standard deviation)] | |||||
| 13.8 (9.6) | 16.1 (10.4) | 16.0 (11.2) | 12.3 (12.5) | 14.8 (7.6) | |
| 2019–2022 period [N (%)] | |||||
| Gender | |||||
| Female | 248 (39.9) | 72 (51.4) | 93 (46.5) | 52 (41.9) | 465 (42.9) |
| Male | 373 (60.1) | 68 (48.6) | 107 (53.5) | 72 (58.1) | 620 (57.1) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Age (years) | |||||
| 18–25 | 78 (12.6) | 17 (12.1) | 21 (10.5) | 23 (18.5) | 139 (12.8) |
| 26–40 | 189 (30.4) | 33 (23.6) | 60 (30.0) | 41 (33.1) | 323 (29.8) |
| 41–60 | 256 (41.2) | 62 (44.3) | 76 (38.0) | 44 (35.5) | 438 (40.4) |
| > 60 | 98 (15.8) | 28 (20) | 43 (21.5) | 16 (12.9) | 185 (17.1) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Compulsory admission | |||||
| Yes | 104 (16.8) | 18 (12.9) | 35 (17.5) | 15 (12.1) | 104 (8) |
| No | 398 (64.1) | 93 (66.4) | 115 (57.5) | 61 (49.2) | 398 (64.1) |
| Missing | 119 (19.2) | 29 (20.7) | 50 (25.0) | 48 (38.7) | 119 (19.2) |
| Hospitalization length by weekly admission [mean days (standard deviation)] | |||||
| 14.5 (13.9) | 14.8 (17.1) | 14.3 (11.5) | 12.5 (16.3) | 14.3 (11.1) | |
Poisson models evaluating the association between weekly admissions and trimesters in the four years surrounding the L’ Aquila earthquake (2008–2011) were significant for all diagnoses (schizophrenia spectrum disorder: R2 = 0.25, p < 0.001; major depression: R2 = 0.13, p = 0.01; bipolar disorder: R2 = 0.10, p = 0.03; alcohol/substance use disorder: R2 = 0.26, p < 0.001), indicating variations in the hospitalisation frequency over the analysed period.
Overall, analyses showed that weekly admissions for all diagnoses in the earthquake trimester (6th ) were significantly lower than in the previous trimester (5th ) (Table 2; Fig. 1).
Table 2.
Results of the Poisson models [exp(b) and p-value] evaluating the association between weekly admissions and trimesters in the four-year period surrounding the L’ Aquila earthquake (2008–2011)
| 2008–2011 trimesters | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| Schizophrenia spectrum disorder | |||||||||||||||
| exp(b) | 2.31 | 2.22 | 2.39 | 2.14 | 1.72 | 1.17 | 1.22 | 0.73 | 1.34 | 1.64 | 1.89 | 1.80 | 1.13 | 2.06 | 1.72 |
| p | < 0.001 | 0.002 | < 0.001 | 0.003 | 0.04 | 0.57 | 0.49 | 0.33 | 0.29 | 0.06 | 0.01 | 0.02 | 0.66 | 0.01 | 0.04 |
| Major depression | |||||||||||||||
| exp(b) | 2.31 | 2.42 | 1.85 | 1.27 | 2.31 | 0.92 | 0.69 | 1.13 | 1.73 | 1.62 | 0.58 | 0.92 | 1.62 | 1.15 | 1.38 |
| p | 0.046 | 0.03 | 0.16 | 0.61 | 0.046 | 0.87 | 0.50 | 0.81 | 0.21 | 0.28 | 0.33 | 0.87 | 0.28 | 0.76 | 0.48 |
| Bipolar disorder | |||||||||||||||
| exp(b) | 1.69 | 2.92 | 4.15 | 2.15 | 3.23 | 1.69 | 1.69 | 1.50 | 2.31 | 2.77 | 3.08 | 2.15 | 3.08 | 3.08 | 2.46 |
| p | 0.30 | 0.02 | 0.002 | 0.12 | 0.01 | 0.30 | 0.30 | 0.44 | 0.08 | 0.03 | 0.02 | 0.12 | 0.02 | 0.02 | 0.06 |
| Alcohol/substance use disorder | |||||||||||||||
| exp(b) | 13.9 | 12.90 | 14.80 | 10.20 | 12.90 | 0.92 | 1.85 | 5.00 | 2.77 | 4.62 | 5.54 | 5.54 | 3.69 | 3.69 | 10.20 |
| p | 0.01 | 0.01 | 0.01 | 0.03 | 0.01 | 0.95 | 0.62 | 0.14 | 0.38 | 0.16 | 0.11 | 0.11 | 0.24 | 0.24 | 0.03 |
Notes: Trimester 6 was used as a reference level. Bold values indicate statistical significance at the p < 0.05 level
In detail, weekly admissions for schizophrenia spectrum disorder in the 6th trimester were also lower compared to all previous trimesters (1st – 4th ). Admissions remained stable 5 trimesters after the earthquake and increased again from the 12th trimester.
For major depression, weekly admissions for the 6th trimester were also lower than those for the 1st and 2nd trimesters, remaining relatively stable over the examined period (7th – 16th trimesters).
As far as the bipolar disorder diagnoses are concerned, weekly admissions in the 6th trimester were also lower compared to the 2nd and 3rd trimesters. The earthquake-related reduction of admission rates persisted until the 11th trimesters, with exceptions for the 13th and 16th quarters.
Admissions for alcohol/substance use disorder were also lower in the 6th trimester than in the 1st —4th. No statistical differences were identified between the 6th and subsequent trimesters. Therefore, admission rates remained substantially steady in the long run, although the 16th trimester was characterised by increased admissions.
On the other hand, Generalised Linear Models analysing the association between weekly hospitalisation length and trimesters were not significant for all psychiatric diagnoses (schizophrenia spectrum disorder: R2 = 0.09, p = 0.24; major depression: R2 = 0.15, p = 0.08; bipolar disorder: R2 = 0.14, p = 0.15; alcohol/substance use disorder: R2 = 0.09, p = 0.95), suggesting no variation in the hospitalisation duration within the 4 years surrounding the L’ Aquila Earthquake.
Poisson models evaluating the association between weekly hospitalisations and trimesters in the four years surrounding the COVID-19 lockdown (2019–2022) were significant for all diagnoses (schizophrenia spectrum disorder: R2 = 0.13, p = 0.02; major depression: R2 = 0.09, p = 0.045; bipolar disorder: R2 = 0.12, p = 0.005; alcohol/substance use disorder: R2 = 0.24, p < 0.001), suggesting differences in the admission frequency within the analysed 4-year period.
Specifically, analyses showed no significant differences between the first lockdown trimester (6th ) and others except for an increase in the 13th trimester for schizophrenia spectrum disorder, major depression, alcohol/substance use disorder, and in the 14th for bipolar disorder (Table 3; Fig. 2). For alcohol/substance use disorder, weekly admissions for the 14th and the 16th trimester were also higher compared to the 6th trimester.
Table 3.
Results of the Poisson models [exp(b) and p-value] evaluating the association between the weekly admissions and trimesters in the four-year period surrounding the COVID-19 lockdown (2019–2022)
| 2019–2022 trimesters | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| Schizophrenia spectrum disorder | |||||||||||||||
| exp(b) | 1.26 | 1.29 | 1.14 | 1.09 | 1.26 | 1.14 | 1.14 | 0.89 | 0.71 | 1.00 | 1.20 | 1.69 | 1.31 | 0.91 | 0.71 |
| p | 0.31 | 0.26 | 0.56 | 0.73 | 0.31 | 0.56 | 0.56 | 0.62 | 0.20 | 1.00 | 0.43 | 0.01 | 0.22 | 0.71 | 0.20 |
| Major depression | |||||||||||||||
| exp(b) | 1 | 0.78 | 0.56 | 0.78 | 1.22 | 1.11 | 0.56 | 0.67 | 1.00 | 1.00 | 1.11 | 2.33 | 1.00 | 0.67 | 0.78 |
| p | 1 | 0.62 | 0.29 | 0.62 | 0.66 | 0.82 | 0.29 | 0.44 | 1.00 | 1.00 | 0.82 | 0.03 | 1.00 | 0.44 | 0.62 |
| Bipolar disorder | |||||||||||||||
| exp(b) | 0.57 | 0.43 | 1.00 | 0.64 | 0.71 | 0.71 | 0.64 | 0.64 | 1.14 | 0.64 | 1.43 | 1.14 | 2.00 | 0.64 | 0.93 |
| p | 0.21 | 0.08 | 1.00 | 0.30 | 0.42 | 0.42 | 0.30 | 0.30 | 0.72 | 0.30 | 0.31 | 0.72 | 0.03 | 0.30 | 0.85 |
| Alcohol/substance use disorder | |||||||||||||||
| exp(b) | 1.50 | 1.50 | 0.75 | 0.75 | 0.25 | 0.50 | 1.00 | 2.25 | 3.00 | 2.00 | 1.50 | 5.75 | 3.25 | 2.50 | 3.50 |
| p | 0.53 | 0.53 | 0.71 | 0.71 | 0.21 | 0.42 | 1.00 | 0.18 | 0.06 | 0.26 | 0.53 | 0.001 | 0.04 | 0.12 | 0.03 |
Notes Trimester 6 was used as a reference level. Bold values indicate statistical significance at the p < 0.05 level
Therefore, this data pattern suggested that overall admissions remained substantially stable before and after the COVID-19 lockdown period, except for a consistent increase for all diagnoses in the first part of 2022.
Finally, analyses on the relationship between hospitalisation length and trimesters were not significant for all diagnoses (schizophrenia spectrum disorder: R2 = 0.07, p = 0.51; major depression: R2 = 0.17, p = 0.39; bipolar disorder: R2 = 0.16, p = 0.21; alcohol/substance use disorder: R2 = 0.16, p = 0.59), indicating stable admission duration over the examined period.
Discussion
In this observational study, we analysed and compared the trend of hospitalisations by diagnosis at L’ Aquila Hospital (Italy) during the four-year periods 2008–2011 and 2019–2022, with a focus on the second quarter (6th ) of 2009 (L’ Aquila earthquake) and 2020 (2020 COVID-19 lockdown/first pandemic wave).
When considering the type of diagnosis at admission, results showed a substantially stable trend between the two events, with schizophrenia spectrum disorder as the most represented diagnosis, followed by bipolar disorder, major depression, and alcohol/substance abuse disorder.
Regarding the total number of admissions, results showed how the post-earthquake year was associated with a transient reduction in hospitalisations (see Fig. 1). Such findings align with the study conducted by Beaglehole et al. (2015) after the Christchurch earthquake in New Zealand [10]. They could be potentially attributable to the population’s post-traumatic resilience development [37] or even clinical improvement in the aftermath of a disaster [38], especially for schizophrenia [39]. Indeed, in the months following the event, the territorial mental health center also reduced the rate of referrals [40].
Resilience has always been considered the most important protective factor in counteracting the traumatic effects of disasters and mitigating the impact of long-term psychological symptomatology [15, 37]. However, factors related to the immediate management of the 2009 earthquake emergency, such as structural and organisational changes in the psychiatric service and the relocation of part of the population, may have significantly impacted the utilisation of mental health services and, therefore, should be considered as additional reasons for the observed transient reduction in hospitalisations.
Interestingly, in our study, admissions for schizophrenia spectrum and bipolar disorder, the most represented diagnoses, rose again after 21 and 18 months, respectively, after the 2009 earthquake. This observation is also in line with previous evidence that the reduction in hospitalisation rates following a natural disaster occurs only in the first period after the traumatic event [10], and it could be followed by a subsequent increase in 1 or 2 years after the event itself [12].
On the other hand, results concerning the COVID-19 pandemic period over the four years 2019–2022 showed that the number of hospitalisations remained generally stable for all diagnoses, except for a substantial increase in the first half of 2022 (see Fig. 2) in correspondence with the cessation of the restrictions imposed to counteract the virus spread, which occurred about 24 months after the pandemic outbreak. This finding seems coherent with the observations made after the Ash Wednesday fires of 1983, where many individuals sought care more than two years after the event [41]. The effective onset of psychiatric disorders may take time to reach levels of severity requiring assistance; manifestations may be delayed, suggesting a possible long-term impact of traumatic events [12]. Therefore, in the context of the COVID-19 pandemic, our results indicate that the potential effects on mental health manifested upon the final cessation of restrictive measures and the return to normalisation of local health management. Similarly, the study of Dionisie et al. (2022) showed an increase in the number of hospitalisations for affective and psychotic disorders after the release of restrictive measures [32]. However, unlike previous observations [28, 32], our results did not show a substantial decrease in hospital admissions during the COVID-19 emergency. Although Boldrini’s multicentre study analyses some data on hospitalisations from the same territory [28], some fundamental methodological and sample differences hinder comparing our results. A detailed analysis of data yielded by the present monocentric study on the progression of hospitalisations over a longer time frame suggests that the trend of hospitalisations in the long run during the pandemic period remains essentially stable. A possible explanation for this finding could be related to the specific characteristics of our examined population, as it has been overexposed to traumatic events. Therefore, it is not possible to rule out the cumulative effects of disaster exposure on mental health that may partially explain the lack of decrease in hospitalisations during the subsequent COVID-19 emergency.
Nevertheless, consistent with our findings, a study analysing hospital admissions and psychiatric emergency presentations during the COVID-19 first wave period in Germany compared to the pre-COVID-19 period observed no significant changes in overall psychiatric presentations and admissions [42]. Similarly, Vukojevic and colleagues found no rise in emergency psychiatric admissions for Spanish influenza and the COVID-19 pandemic [33].
The effect of both traumatic events must also be taken into account concerning any new-onset or relapse disorders, considering the increased rates of psychological distress and psychiatric disorders following natural disasters [8]. In addition, the cumulative effects of traumatic events should also be considered as an influencing factor for hospitalisations, especially for schizophrenia spectrum disorder, bipolar disorder, major depression, and alcohol/substance abuse disorder [43–47].
Differences between the 2009 earthquake and the COVID-19 pandemic as traumatic events can be considered when comparing admission rates in the two reporting periods. In particular, the marked decrease in admissions in the peri-traumatic 2009 period may be partly attributable to significant changes in territorial organisation, with a logistical rearrangement of the community in the immediate aftermath. Notably, the earthquake caused severe damage to San Salvatore Hospital in L’ Aquila, and the day after, the psychiatric service was relocated to two tents in the field hospital [20]. It was finally moved back to a restored hospital section only three months later [20]. After the event, there was a massive logistical rearrangement of the community, with approximately 40,000 individuals accommodated in tented camps [20]. Therefore, while the disruption of routine healthcare management may have impacted help-seeking, such a collectively experienced emergency could also have played a role in fostering social connections and support among individuals at a local community level, thus promoting interpersonal resilience resources in the population, with a potentially protective role for individuals’ mental health [48, 49], especially in the first phase of the emergency. In contrast, the immediate psychological impact of the pandemic, paralleled by a substantial prolonged reduction in social interactions, may have exerted long-term adverse effects on mental health, particularly in at-risk populations [50]. As previously reported during the COVID-19 s wave in Germany, the pandemic period may also have led to increases in new-onset psychiatric disorders, mainly due to indirect sequelae of the health emergency, such as social isolation and work and financial insecurity [51].
Limitations and suggestions for future research
Several limitations must be considered in the present study. The retrospective single-site assessment leads to results that cannot be extended to the general population or specific clinical groups. Moreover, the decrease in population due to dislocation after the earthquake [20] might have led to biased results regarding the number of admissions in the time frame between 2008 and 2011. In addition, the present study does not evaluate the possible use of counselling and psychotherapeutic services that have the potential to alleviate symptoms at the onset. A possible limitation of our study was the use of ICD-9 as the classification system for diagnoses since our regional health information system is updated to this version of the ICD. Nevertheless, although this may appear to be a limitation, this classification allowed for greater comparability of data considering the vast period analysed. Another limitation to consider is that we have not delved into the relationship between traumatic events and the type of recurrence of bipolar disorder episodes, manic or depressive. Another limitation is represented by the fact that we have not included a diagnosis of post-traumatic stress disorder in this study and suicide behaviour or aggressive behaviour was not assessed. Furthermore, previous possible COVID-19 disease could also not be assessed as a possible contributing factor in admission. We also acknowledge that the low number of compulsory admissions precluded reliable statistical analyses for this category. As a result, our findings primarily reflect trends observed in voluntary admissions, limiting the generalizability of our results. Future studies should include a larger sample of compulsory admissions to understand better the full spectrum of psychiatric hospitalisation trends following major events.
None of the analyses were significant regarding the length of stay, indicating a stable length of hospitalisation over the two 4-year periods analysed. These data contrast other studies conducted during the COVID-19 pandemic, which showed differences in length of stay with specific diagnoses [52]. Furthermore, the study by Moitinho de Almeida et al. showed an increase in the length of stay in the earthquake’s immediate aftermath, which was not detected in our study [53].
On the other hand, our study’s average length of stay of psychiatric patients appears slightly lower than the Italian average of 17.9 days [54].
Finally, it is important to acknowledge that we exclusively focused on inpatient admissions, which represent a minor proportion of overall mental health service users. A significant portion of individuals experiencing psychiatric conditions during major crises seek help through emergency departments (ED) and outpatient services, which were not covered in our analysis. Emergency visits and outpatient treatments are crucial components of mental health care and often capture a broader spectrum of psychiatric conditions, including Acute Stress Disorders and Posttraumatic Stress Disorder. These conditions, which can be exacerbated by major events such as earthquakes and pandemics, might lead individuals to seek immediate and recurrent assistance in ED or outpatient settings rather than inpatient admissions. We recognise that our study’s focus on inpatient data may not fully reflect the comprehensive impact of these crises on mental health. Therefore, future research should aim to investigate the rates and patterns of ED visits and specific outpatient treatments. This would provide a more holistic understanding of how major events affect mental health service utilisation and the broader spectrum of psychiatric morbidity.
On the other hand, the strength of this study is represented by the naturalistic design over a long period across two distinct catastrophic events. Therefore, considering the existing literature, our findings suggest a possible long-term adverse effect of major health crises on mental health, peaking between 18 and 24 months after the event [12]. In this regard, our study emphasises the need for further studies to evaluate patterns of psychiatric hospitalisation following major health crises in the long term [55]. In addition, considering the possible delayed onset of psychiatric disorders following a traumatic event can help plan interventions targeted to those in need of support to prevent long-term health crises -related psychiatric morbidity.
Conclusions
The present study confirms the role of major health crises in influencing psychiatric ward admissions patterns. Specifically, analysing two major emergencies in Italy, we observed a transient reduction of weekly admissions at L’ Aquila Hospital during the 2009 earthquake trimester, while psychiatric hospitalizations remained substantially stable around the COVID-19 lockdown. However, a consistent long-term hospitalisation increase for all diagnoses characterised the period corresponding to the cessation of anti-COVID-19 measures in Italy. These findings suggest that exposure to major emergencies can have both short—and long-term effects on psychiatric ward admission. The present study could be particularly informative for decision-makers to target interventions for mental health and future emergency management strategies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Table 1 Categories analysed according to ICD-9 codes.
Acknowledgements
None.
Abbreviations
- ICD-9
Classification of Diseases Version 9
- ED
Emergency Departments
Author contributions
TB, FP, and FS conceived and designed the project idea. TB, GR, FS, and AR acquired and analysed the data. TB, CDA, and VS drafted the manuscript. ET, FS, and AR drew figures and tables. All authors edited the draft and approved the final manuscript.
Funding
None.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were conducted ethically, adhering to the institutional guidelines and the 1964 Declaration of Helsinki, including subsequent updates. The Ethics Committee obtained ethical approval from the Internal Review Board of the University of L’ Aquila on 18/10/2016, Sequence No: 05/2016. The participant consent requirement was waived because of the retrospective design, based on data from the records of the San Salvatore Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reifels L, Mills K, Dückers MLA, O’Donnell ML. Psychiatric epidemiology and disaster exposure in Australia. Epidemiol Psychiatr Sci. 2019;28(3):310–320. doi: 10.1017/S2045796017000531. Epub 2017 Sep 27. PMID: 28950925; PMCID: PMC7032773. [DOI] [PMC free article] [PubMed]
- 2.Seddighi H. COVID-19 as a natural disaster: focusing on exposure and vulnerability for response. Disaster Med Public Health Prep. 2020;14(4):e42–3. 10.1017/dmp.2020.279. Epub 2020 Jul 27. PMID: 32713408; PMCID: PMC7492580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alpert EA, Jaffe E, EMS Catastrophic Events. 2022 Sep 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30422515. [PubMed]
- 4.Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35:169 – 83. 10.1146/annurev-publhealth-032013-182435. Epub 2013 Oct 25. PMID: 24159920. [DOI] [PubMed]
- 5.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. PMID: 7738325. [PubMed] [Google Scholar]
- 6.McFarlane AC, Williams R. Mental health services required after disasters: learning from the lasting effects of disasters. Depress Res Treat. 2012;2012:970194. doi: 10.1155/2012/970194. Epub 2012 Jul 1. PMID: 22811897; PMCID: PMC3395273. [DOI] [PMC free article] [PubMed]
- 7.North CS. Disaster Mental Health Epidemiology: Methodological Review and Interpretation of Research Findings. Psychiatry. 2016 Summer;79(2):130–146. 10.1080/00332747.2016.1155926. PMID: 27724836. [DOI] [PubMed]
- 8.Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716–722. 10.1192/bjp.2018.210. Epub 2018 Oct 10. PMID: 30301477. [DOI] [PubMed]
- 9.Haker H, Lauber C, Malti T, Rössler W. Is there an impact of global and local disasters on psychiatric inpatient admissions? Eur Arch Psychiatry Clin Neurosci. 2004;254(5):330-4. 10.1007/s00406-004-0507-0. PMID: 15365709. [DOI] [PubMed]
- 10.Beaglehole B, Bell C, Beveridge J, Frampton C. Psychiatric admissions fall following the Christchurch earthquakes: an audit of inpatient data. Aust N Z J Psychiatry. 2015;49(4):346–50. Epub 2014 Dec 5. PMID: 25480653. [DOI] [PubMed] [Google Scholar]
- 11.Jones E, Woolven R, Durodie W, et al. Public panic and morale: a reassessment of civilian reactions during the Blitz and World War 2. J Social History. 2004;17:463–79. [Google Scholar]
- 12.McFarlane AC, Van Hoof M. The counterintuitive effect of a disaster: the need for a long-term perspective. Aust N Z J Psychiatry. 2015;49(4):313-4. 10.1177/0004867415576393. PMID: 25802180. [DOI] [PubMed]
- 13.Sakuma A, Ueda I, Rengi S, Shingai T, Matsuoka H, Matsumoto K. Increase in the number of admissions to psychiatric hospitals immediately after the Great East Japan Earthquake. Asia Pac Psychiatry. 2018;10(3):e12307. 10.1111/appy.12307. Epub 2017 Dec 28. PMID: 29285896; PMCID: PMC6175335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aoki A, Aoki Y, Harima H. The impact of the Great East Japan earthquake on mandatory psychiatric emergency hospitalizations in Tokyo: a retrospective observational study. Transl Psychiatry. 2012;2(10):e168. 10.1038/tp.2012.98. PMID: 23032944; PMCID: PMC3565828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi R, Socci V, Gregori E, Talevi D, Collazzoni A, Pacitti F, Stratta P, Rossi A, Di Lorenzo G, ResilienCity. Resilience and psychotic-like experiences 10 years after L’ Aquila Earthquake. Front Psychiatry. 2020;11:77. 10.3389/fpsyt.2020.00077. PMID: 32180736; PMCID: PMC7059251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stratta P, de Cataldo S, Bonanni R, Valenti M, Masedu F, Rossi A. Mental health in L’ Aquila after the earthquake. Ann Ist Super Sanita. 2012;48(2):132-7. 10.4415/ANN_12_02_05. PMID: 22751555. [DOI] [PubMed]
- 17.Gigantesco A, Mirante N, Granchelli C, Diodati G, Cofini V, Mancini C, Carbonelli A, Tarolla E, Minardi V, Salmaso S, D’Argenio P. Psychopathological chronic sequelae of the 2009 earthquake in L’ Aquila, Italy. J Affect Disord. 2013;148(2–3):265 – 71. doi: 10.1016/j.jad.2012.12.006. Epub 2013 Jan 1. PMID: 23287524. [DOI] [PubMed]
- 18.Rossi A, di Tommaso S, Stratta P, Riccardi I, Daneluzzo E. How much stress is needed to increase vulnerability to psychosis? A community assessment of psychic experiences (CAPE) evaluation 10 months after an earthquake in L’ Aquila (Italy). Eur Arch Psychiatry Clin Neurosci. 2012;262(3):265–8. 10.1007/s00406-011-0258-7. Epub 2011 Sep 20. PMID: 21932082. [DOI] [PubMed] [Google Scholar]
- 19.Casacchia M, Bianchini V, Mazza M, Pollice R, Roncone R. Acute stress reactions and associated factors in the help-seekers after the L’ Aquila earthquake. Psychopathology. 2013;46(2):120–30. 10.1159/000339459. Epub 2012 Aug 21. PMID: 22922557. [DOI] [PubMed] [Google Scholar]
- 20.Casacchia M, Pollice R, Roncone R. The narrative epidemiology of L’ Aquila 2009 earthquake. Epidemiol Psychiatric Sci. 2012;21(1):13–21. 10.1017/S2045796011000801. [DOI] [PubMed] [Google Scholar]
- 21.Pollice R, Bianchini V, Conti MC, Mazza M, Roncone R, Casacchia M. Cognitive impairment and perceived stress in schizophrenic inpatients with post-traumatic stress disorder. Eur J Inflamm. 2010;8:211–9. [Google Scholar]
- 22.Barlattani T, D’Amelio C, Capelli F, Mantenuto S, Rossi R, Socci V, Stratta P, Di Stefano R, Rossi A, Pacitti F. Suicide and COVID-19: a rapid scoping review. Ann Gen Psychiatry. 2023;22(1):10. 10.1186/s12991-023-00441-6. PMID: 36932453; PMCID: PMC10020759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pacitti F, Socci V, D’Aurizio G, Jannini TB, Rossi A, Siracusano A, Rossi R, Di Lorenzo G. Obsessive-compulsive symptoms among the general population during the first COVID-19 epidemic wave in Italy. J Psychiatr Res. 2022;153:18–24. Epub 2022 Jun 28. PMID: 35792342; PMCID: PMC9239523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, Di Marco A, Rossi A, Siracusano A, Di Lorenzo G. COVID-19 pandemic and Lockdown Measures Impact on Mental Health among the General Population in Italy. Front Psychiatry. 2020;11:790. 10.3389/fpsyt.2020.00790. PMID: 32848952; PMCID: PMC7426501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Romano V, Ancillotti M, Mascalzoni D, et al. Italians locked down: people’s responses to early COVID-19 pandemic public health measures. Humanit Soc Sci Commun. 2022;9:342. 10.1057/s41599-022-01358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ambrosetti J, Macheret L, Folliet A, Wullschleger A, Amerio A, Aguglia A, Serafini G, Prada P, Kaiser S, Bondolfi G, Sarasin F, Costanza A. Impact of the COVID-19 pandemic on Psychiatric admissions to a large Swiss Emergency Department: an observational study. Int J Environ Res Public Health. 2021;18(3):1174. 10.3390/ijerph18031174. PMID: 33525740; PMCID: PMC7908206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonello F, Zammit D, Grech A, Camilleri V, Cremona R. Effect of COVID-19 pandemic on mental health hospital admissions: comparative population-based study. BJPsych Open. 2021;7(5):e141. 10.1192/bjo.2021.975. PMID: 34340723; PMCID: PMC8365103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boldrini T, Girardi P, Clerici M, Conca A, Creati C, Di Cicilia G, Ducci G, Durbano F, Maci C, Maone A, Nicolò G, Oasi O, Percudani M, Polselli GM, Pompili M, Rossi A, Salcuni S, Tarallo F, Vita A, Lingiardi V, Italian Network for Research on Mental Health during COVID-19 Pandemic. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatry. 2021;110:110304. 10.1016/j.pnpbp.2021.110304. Epub 2021 Mar 16. PMID: 33737215; PMCID: PMC8569419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross CA, Kara S, Ferrer GF. COVID-19 and Psychiatric admissions: a comparative study of pre-pandemic and post-pandemic psychosis admissions in a South Florida Emergency Department. Cureus. 2023;15(6):e40989. 10.7759/cureus.40989. PMID: 37503505; PMCID: PMC10370826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanner B, Kurdyak P, de Oliveira C. Adult Psychiatric Hospitalizations in Ontario, Canada before and during the COVID-19 pandemic. Can J Psychiatry. 2023;68(12):925–32. doi: 10.1177/07067437231167386. Epub 2023 Apr 3. PMID: 37006178; PMCID: PMC10657583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clerici M, Durbano F, Spinogatti F, Vita A, de Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. 2020;37(4):283–90. 10.1017/ipm.2020.29. Epub 2020 May 5. PMID: 32368994; PMCID: PMC7264453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dionisie V, Ciobanu AM, Moisa E, Manea MC, Puiu MG. The impact of the COVID-19 pandemic on Inpatient admissions for psychotic and affective disorders: the experience of a large Psychiatric Teaching Hospital in Romania. Healthc (Basel). 2022;10(8):1570. 10.3390/healthcare10081570. PMID: 36011227; PMCID: PMC9407826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vukojević J, Đuran N, Žaja N, Sušac J, Šekerija M, Savić A. 100 years apart: Psychiatric admissions during spanish flu and COVID-19 pandemic. Psychiatry Res. 2021;303:114071. 10.1016/j.psychres.2021.114071. Epub 2021 Jun 24. PMID: 34217101; PMCID: PMC8525540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coxe S, West SG, Aiken LS. The analysis of count data: a gentle introduction to poisson regression and its alternatives. J Pers Assess. 2009;91:121–36. 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- 35.Payne EH, Gebregziabher M, Hardin JW, Ramakrishnan V, Egede LE. An empirical approach to determine a threshold for assessing overdispersion in Poisson and negative binomial models for count data. Commun Stat Simul Comput. 2018;47:1722. 10.1080/03610918.2017.1323223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gallucci M, GAMLj:. January GLM, Mixed, Generalized and Generalized mixed models for jamovi. Available online: https://github.com/gamlj/gamlj (accessed on 20 2024).
- 37.Stratta P, Capanna C, Dell’Osso L, Carmassi C, Patriarca S, Di Emidio G, et al. Resilience and coping in trauma spectrum symptoms prediction: a structural equation modeling approach. Pers Individ Dif. 2015;77:55–61. 10.1016/j.paid.2014.12.035. ISSN 0191–8869. [Google Scholar]
- 38.Katz CL, Pellegrino L, Pandya A, Ng A, DeLisi LE. Research on psychiatric outcomes and interventions subsequent to disasters: a review of the literature. Psychiatry Res. 2002;110(3):201 – 17. 10.1016/s0165-1781(02)00110-5. PMID: 12127471. [DOI] [PubMed]
- 39.Stratta P, Rossi A. Subjective adjustment of individuals with psychiatric disorders in the aftermath of the L’ Aquila earthquake. Am J Psychiatry. 2010;167(3):352-3. 10.1176/appi.ajp.2009.09081173. PMID: 20194493. [DOI] [PubMed]
- 40.Stratta P, de Cataldo S, Bonanni RL, Rossi A. Community mental health service utilization after the L’ Aquila earthquake. Community Ment Health J. 2015;51(4):504–8. 10.1007/s10597-014-9822-8. Epub 2014 Dec 25. PMID: 25540028. [DOI] [PubMed] [Google Scholar]
- 41.McFarlane AC. Posttraumatic morbidity of a disaster. A study of cases presenting for psychiatric treatment. J Nerv Ment Dis. 1986;174(1):4–14. 10.1097/00005053-198601000-00002. PMID: 3484516. [DOI] [PubMed]
- 42.Goldschmidt T, Kippe Y, Finck A, Adam M, Hamadoun H, Winkler JG, Bermpohl F, Schouler-Ocak M, Gutwinski S. Psychiatric presentations and admissions during the first wave of Covid-19 compared to 2019 in a psychiatric emergency department in Berlin, Germany: a retrospective chart review. BMC Psychiatry. 2023;23(1):38. 10.1186/s12888-023-04537-x. Erratum in: BMC Psychiatry. 2023;23(1):164. doi: 10.1186/s12888-023-04629-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aldinger F, Schulze TG. Environmental factors, life events, and trauma in the course of bipolar disorder. Psychiatry Clin Neurosci. 2017;71(1):6–17. 10.1111/pcn.12433. Epub 2016 Sep 21. PMID: 27500795; PMCID: PMC7167807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gibson LE, Alloy LB, Ellman LM. Trauma and the psychosis spectrum: a review of symptom specificity and explanatory mechanisms. Clin Psychol Rev. 2016;49:92–105. 10.1016/j.cpr.2016.08.003. Epub 2016 Aug 31. PMID: 27632064; PMCID: PMC5157832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Basedow LA, Kuitunen-Paul S, Roessner V, Golub Y. Traumatic events and Substance Use disorders in adolescents. Front Psychiatry. 2020;11:559. 10.3389/fpsyt.2020.00559. PMID: 32625122; PMCID: PMC7314975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guinle MIB, Sinha R. The role of stress, trauma, and negative affect in Alcohol Misuse and Alcohol Use Disorder in Women. Alcohol Res. 2020;40(2):05. 10.35946/arcr.v40.2.05. PMID: 32832310; PMCID: PMC7431322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Flory JD, Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin Neurosci. 2015;17(2):141–50. 10.31887/DCNS.2015.17.2/jflory. PMID: 26246789; PMCID: PMC4518698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McGuire AP, Gauthier JM, Anderson LM, Hollingsworth DW, Tracy M, Galea S, Cofey SF. Social support moderates efects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: efects for displaced and nondisplaced residents. J Trauma Stress. 2018;31(2):223–33. 10.1002/jts.22270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cruwys T, Macleod E, Heffernan T, Walker I, Stanley SK, Kurz T, Greenwood LM, Evans O, Calear AL. Social group connections support mental health following wildfire. Soc Psychiatry Psychiatr Epidemiol. 2024;59(6):957–67. 10.1007/s00127-023-02519-8. Epub 2023 Jul 10. PMID: 37428193; PMCID: PMC11116249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murphy L, Markey K, O’ Donnell C, Moloney M, Doody O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: a scoping review. Arch Psychiatr Nurs. 2021;35(4):375–94. 10.1016/j.apnu.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adam M, Moran JK, Kippe YD, Schouler-Ocak M, Bermpohl F, Gutwinski S, Goldschmidt T. Increase in presentations with new-onset psychiatric disorders in a psychiatric emergency department in Berlin, Germany during the second wave of the COVID-19 pandemic - a retrospective cross-sectional study. Front Psychiatry. 2023;14:1240703. 10.3389/fpsyt.2023.1240703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Russolillo A, Carter M, Guan M, Singh P, Kealy D, Raudzus J. Adult psychiatric inpatient admissions and length of stay before and during the COVID-19 pandemic in a large urban hospital setting in Vancouver, British Columbia. Front Health Serv. 2024;4:1365785. 10.3389/frhs.2024.1365785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moitinho de Almeida M, Schlüter BS, van Loenhout JAF, et al. Changes in patient admissions after the 2015 earthquake: a tertiary hospital-based study in Kathmandu, Nepal. Sci Rep. 2020;10:4956. 10.1038/s41598-020-61901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dimitri G, Giacco D, Bauer M, Bird VJ, Greenberg L, Lasalvia A, Lorant V, Moskalewicz J, Nicaise P, Pfennig A, Ruggeri M, Welbel M, Priebe S. Predictors of length of stay in psychiatric inpatient units: Does their effect vary across countries? Eur Psychiatry. 2018;48:6–12. doi: 10.1016/j.eurpsy.2017.11.001. Epub 2018 Jan 10. PMID: 29331601. [DOI] [PubMed]
- 55.Beaglehole B, Boden JM, Bell C, Mulder RT, Dhakal B, Horwood LJ. The long-term impacts of the Canterbury earthquakes on the mental health of the Christchurch Health and Development Study cohort. Aust N Z J Psychiatry. 2023;57(7):966–74. Epub 2022 Nov 29. PMID: 36448198. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Table 1 Categories analysed according to ICD-9 codes.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.