Abstract
Premature ventricular contractions (PVCs) are a common finding in clinical practice, requiring a full diagnostic work-up in order to exclude an underlying cardiomyopathy. Still, in a substantial proportion of patients, these investigations do not identify any substrate, and the PVCs are labelled as idiopathic. Cardiac magnetic resonance (CMR) has proven in the last decades as the method of choice for the exploration of patients with cardiomyopathies, since it can identify subtle changes in the myocardial tissue and help with risk stratification. In patients with idiopathic PVCs and a high PVC burden, several studies report the presence of late gadolinium enhancement (LGE) at CMR, which can offer additional diagnostic and prognostic benefits, as well as assistance in catheter ablation procedures, as the risk for adverse cardiac and risk for arrhythmic events events is higher compared to patients without scar. This paper focuses on the impact of the presence of LGE in patients with idiopathic PVCs, reviewing all the relevant studies published so far, including randomized controlled clinical trials, prospective or retrospective cohort studies, case series and case reports as well as systematic reviews.
Keywords: Premature ventricular contractions, cardiac magnetic resonance, late gadolinium enhancement, risk stratification
Highlights
Cardiac magnetic resonance can detect subtle changes in patients with idiopathic PVCs.
The presence of late gadolinium enhancement in patients with idiopathic PVCs can influence the prognosis of these individuals.
In some patients with idiopathic PVCs, given the characteristics of the scar, cardiac magnetic resonance can help with arrhythmic risk stratification.
Introduction
Premature ventricular contractions (PVCs) are common in patients undergoing long-term cardiological monitoring, accounting for approximately 90% of all ventricular arrhythmias (VAs). They are favored by older age, taller individuals, male sex, and other modifiable factors such as smoking, increased body mass index (BMI), sedentarism, and the use of excitants. Idiopathic PVCs develop in patients without underlying structural cardiac disease or metabolic imbalances thus, no specific treatment is recommended; nevertheless, patients with recurrent PVCs despite antiarrhythmic treatment may represent a challenge for the clinicians and may be referred for catheter ablation.1-4
Greater access to advanced cardiac imaging techniques, like late gadolinium enhancement cardiac magnetic resonance (LGE-CMR), has demonstrated in recent years that in patients who have idiopathic PVCs with a high PVC burden, myocardial scarring is often described by LGE-CMR. Cardiac magnetic resonance imaging is of great importance as it defines with great accuracy the left and right ventricular function and characterizes myocardial tissue by detecting focal fatty infiltration, tissue edema, and areas of necrosis or fibrosis that may be related to early-stage cardiomyopathies which otherwise would not be identified by conventional screening.5-7
Sudden cardiac death (SCD) has been associated with intramural scarring in patients without known coronary artery disease or acute myocardial infarction, regardless of the ejection fraction (EF). This finding supports the idea that the presence of nonischemic scarring may represent a risk factor for developing future arrhythmias and explains the quest for an active search of myocardial scarring in patients who present with idiopathic PVCs.8
This review focuses on the correlation between the presence, localization, and burden of PVCs, and myocardial scarring detected by LGE-CMR. Furthermore, we discuss the prognostic impact of this finding, in terms of SCD and other major cardiovascular outcomes such as VAs.
Mechanisms of Premature Ventricular Contractions
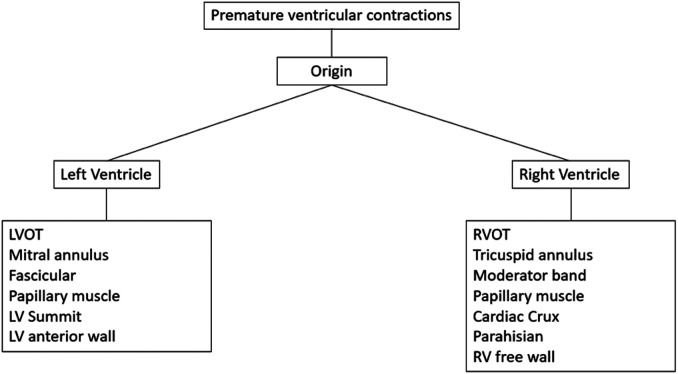
There are 3 primary mechanisms which explain the occurrence of PVCs: triggered activity, enhanced automaticity and re-entry. First of all, triggered activity arises from an elevation in intracellular calcium levels, causing delayed afterdepolarizations or abnormal cardiomyocyte depolarization following the depolarization phase (caffeine or digitalis toxicity). Enhanced automaticity occurs when specific myocardial tissues exhibit an intensified or exaggerated spontaneous generation of electrical impulses within the heart (myocardial ischemia, electrolyte imbalance, and increased adrenergic state). However, re-entry is a distinct mechanism requiring 2 electrical pathways with differential conduction. This mechanism is specific for regions affected by scar tissue and fibrosis, and represents the electrical substrate for monomorphic ventricular tachycardias (VT).9-11 PVCs may originate in all structures of the heart, but the most prevalent PVC location in the general population is still up for debate. Common sites of origin include the right ventricle outflow tract (RVOT), the left ventricle outflow tract (LVOT), as well as the papillary muscles, mitral and tricuspid annulus, left ventricle (LV) summit. and the cardiac crux (Figure 1).3,10
Figure 1.
Types of premature ventricular contractions based on origin. LVOT, left ventricle outflow tract; LV, left ventricle; RVOT, right ventricle outflow tract; RV, right ventricle.
Clinical Studies Evaluating Premature Ventricular Contractions
Initial data regarding the prognostic impact of PVCs supported the idea that PVCs in individuals without structural heart disease do not influence their prognosis. In this regard, in a study conducted in 1985 by Kennedy et al12 a group of 73 asymptomatic healthy participants was closely observed. These individuals were found to have frequent and complex PVCs, which were monitored using 24-hour Holter-ECG monitoring. The asymptomatic healthy status of the participants was confirmed through extensive non-invasive cardiac examinations. However, further investigations through cardiac catheterization in a subset of participants revealed that 19% of them had significant coronary artery disease. Nevertheless, it was concluded that the long-term prognosis for asymptomatic healthy individuals with frequent and complex PVCs is comparable to that of the general healthy population in the United States, indicating no elevated risk of mortality, since using the calculation of a standardized mortality ratio, 7.4 deaths were predicted but only 2 occurred (1 SCD and 1 from cancer).12
In the 90s and 2000s, it was postulated that frequent PVCs could potentially contribute to the development of heart failure in individuals with LV dysfunction, but the significance of frequent PVCs in asymptomatic patients with normal LV function remained uncertain.13,14 To address this, Niwano et al13 conducted a study involving 239 patients who presented with frequent PVCs (defined as more than 1000 beats per day) originating from either the right or LVOT but without any detectable heart disease. Echocardiography and CMR imaging were performed to rule out structural heart disease, and Holter-ECG monitoring was repeated 2 or 3 times to assess the prevalence of PVCs. The findings revealed that over a follow-up period of 5.6 years, none of the patients experienced any significant cardiac events. Although there were no changes in the mean left ventricle ejection fraction (LVEF) and left ventricle diastolic dimension (LVDd) in the entire cohort, a tendency toward a lower EF and a higher LVDd was observed in patients with a high PVC burden (P< .001).13,15 However, Yarlagadda et al16 reached a different conclusion in a smaller cohort study. They enlisted 27 patients with frequent PVCs originating from RVOT (mean burden of 17 624 ± 12 611 PVCs) who underwent assessment of cardiac structure and function (all patients were investigated by echocardiography and 8 patients were also investigated by CMR) before catheter ablation. Following ablation, patients were reassessed with echocardiography and Holter monitoring. Patients with reduced EF tended to be older compared to those with normal function (58 ± 14 years vs. 42 ± 18 years; P = .013). However, the PVC burden was similar between patients with preserved ventricular function (17 859+/–13 488 ectopic beats per 24 hours) and those with impaired function (17 541+/–11 479 ectopic beats per 24 hours; P= .800). A successful ablation procedure was conducted in 23 patients (85%), and among those with reduced EF, an improvement in the EF was observed (from 39 ± 6% to 62 ± 6%; P = .017). This study led to the idea that repetitive PVCs originating from RVOT may be an unrecognized cause of cardiomyopathy.16 Baman et al17, in a study which included 174 patients referred for an ablation procedure for frequent PVC (mean PVC burden of 20% ± 16% determined by 24-hour Holter monitoring) reached a similar conclusion. In total, 57 patients (33%) showed a reduced LVEF, averaging 37% ± 10%. Those with decreased EF had a mean PVCs burden of 33% ± 13%, while those with normal left ventricular function had a burden of 13% ± 12% (P < .0001). A PVC burden greater than 24% effectively separated patients with impaired vs. preserved left ventricular function (sensitivity 79%, specificity 78%, AUC 0.89). The minimum PVC burden leading to reversible cardiomyopathy was found to be 10%, and they concluded that PVC burden emerged as an independent factor associated with PVC-induced cardiomyopathy (HR 1.12, 95% CI 1.08-1.16; P < .01).17
Concerning patients with structural heart disease (SHD), Sarrazin et al18 included in their study 30 patients with myocardial infarction (mean LVEF of 36% ± 12% assessed by transthoracic echocardiography) who were evaluated for implantation of implantable cardioverter defibrillator (ICD). In total, 15 patients with a high PVC burden (at least 5% on 24-h Holter) underwent ablation of PVCs before ICD implantation and the remaining 15 patients served as a control group. Scar burden was evaluated by CMR with late gadolinium enhancement (LGE) in both groups. The PVC ablation procedure was successful in all 15 patients, effectively reducing the average PVC burden from 22% ± 12% to 2.6% ± 5.0% (P< .001). Following the intervention, there was a notable increase in LVEF from 38% ± 10% to 51% ± 9% among the patients who underwent PVC ablation (P = .0001). In contrast, in the control group, LVEF showed no significant change during the same timeframe (34% ± 14% vs. 33% ± 15%; P = .6). Additionally, patients with a higher PVC burden exhibited a smaller scar burden by LGE-CMR in comparison to the control patients.18
Robust data regarding the prognostic impact of PVCs comes from a meta-analysis conducted by Ataklte et al19, which included 11 studies and 106 195 individuals with PVCs, focusing on the relationship between PVCs and SCD. The prevalence of frequent PVCs, defined as more than 1 PVC on a 2-minute ECG recording, in the included studies varied from 1.2% to 10.7%. The overall risk of SCD was found to be 2.64 times higher in individuals with frequent PVCs compared to those without frequent PVCs (HR 2.64, 95% CI 1.93-3.63, P = .469). A limitation of this meta-analysis was that although certain studies aimed at including only patients without structural heart disease, this classification was based only on their clinical history, without additional investigation.19 Dukes et al20 conducted their study on a population-based sample that revealed a correlation between a higher occurrence of PVCs and a decrease in LVEF, an elevated risk of developing congestive heart failure (CHF), and increased mortality. Comparing individuals in the upper quartile of PVC burden to those in the lowest quartile, after a median follow-up of over 13 years, the former group had a 3-fold higher risk of experiencing a 5-year decline in LVEF (OR: 3.10, 95% CI: 1.42-6.77, P = .005), a 48% increased risk of incident CHF (HR: 1.48, 95% CI: 1.08-2.04, P = .02), and a 31% increased risk of death (HR: 1.31, 95% CI: 1.06-1.63, P = .01). Given that PVCs may benefit from medical or ablative therapy, PVCs may represent a modifiable risk factor for developing CHF and mortality.20,21 The origin of the PVCs seems to also play a role as a prognostic marker, since Del Carpio Munoz et al22 observed that PVCs arising from the LV were linked with a significant reduction in LVEF at a PVC burden greater than 20%, while PVCs developing from the right ventricle (RV) were associated with an important reduction in LVEF at a PVC burden of at least 10%.8,22,23
This initial data pointing toward a prognostic impact of “benign” PVCs represents the basis for further research of the electroanatomic substrate of this arrhythmia.
Cardiac Magnetic Resonance and Premature Ventricular Contractions
In the last decades, CMR has been used as a useful imaging technique in a great number of cardiac diseases, being able to precisely and reproducibly determine ventricular volumes, structure, and function.24 Several studies concluded that CMR-detected scar may be associated with ventricular abnormalities and that they might predict adverse outcomes in patients presenting with a greater PVC burden (Table 1).
Table 1.
Correlation between Frequent PVCs and CMR Abnormalities (Literature Review)
| Study | Year | No. of Patients | CMR Abnormalities | PVC Origin | Results |
|---|---|---|---|---|---|
| Aquaro et al26 | 2010 | 396 | 61 (13.8%) | RVOT or higher portion of the interventricular septum | Patients with multiple RV abnormalities had worse outcome than those with no abnormalities (HR: 48.6; 95% CI: 6.1-384.8; P < .001). |
| Yokokawa et al27 | 2017 | 321 | 67 (20%) | LV and RV | The combination of SHD findings by MRI and VT inducibility conferred independently an increased risk of adverse outcome (multivariate hazard ratio 25.73, 95% CI: 6.74-98.20, P < .001). |
| Penela et al28 | 2019 | 70 | 29 (41.4%) | LV and RV | The mass of myocardial scar influences but does not prevent the probability of response to PVC ablation [OR 0.9 (0.81-0.99), P = .04]. |
| Ghannam et al29 | 2020 | 272 | 67 (24.6%) | LV and RV | The presence and the amount of LGE at CMR was related to the risk of VT occurrence independent of EF (HR 18.8 [2.0-176.6], P = .01 and HR 1.4 [1.1-1.7]/cm3 scar, P < .001). |
| Ghannam et al7 | 2020 | 99 | 99 (100%) | LV and RV | Patients with greater scar burden were associated with inducibility of VT independent of EF or prior history of VT (adjusted OR 1.67 [1.24‐2.24]/cm3, P < .01). |
| Muser et al1 | 2020 | 518 | 85 (16%) | LV and RV | Presence of myocardial abnormalities on CMR predict worse clinical outcomes (P < .01). |
| Ghannam et al30 | 2021 | 333 | 112 (34%) | LV and RV | Risk scores can help distinguish between patients at high and low risk for the presence of cardiac scar and worse arrhythmia outcomes based on age (OR 1.02 [1.01-1.04]/year, P = .019) and pre-ablation EF (OR 0.92 [0.89-0.94]/%, P < .001). |
| Nikolaidou et al31 | 2021 | 72 | 39 (54.2%) | LV and RV | Abnormalities revealed by CMR in patients with PVC can be related to PVC induced cardiomyopathy. |
| Hosseini et al32 | 2022 | 255 | 35 (13.7%) | LV and RV | 1 in 7 patients included in the study with frequent PVCs and no known structural heart disease had myocardial abnormality detected on CMR (HR: 4.35; 95% CI: 1.34-14.15; P = .014). |
CMR, cardiac magnetic resonance; EF, ejection fraction; LGE, late gadolinium enhancement; LV, left ventricle; PVC, premature ventricular contraction; RV, right ventricle; RVOT, right ventricle outflow tract; SHD, structural heart disease; VT, ventricular tachycardia.
It has been postulated since the 90s that CMR can demonstrate subtle morphological changes in the myocardium, even in patients with “benign” arrhythmias, such as RVOT tachycardia. To address this issue, Globits et al included 20 patients addressed for catheter ablation of recurrent RVOT tachycardia, who were investigated prior to the procedure by CMR. Ten healthy individuals, matched in terms of both age and sex, were used as control subjects. The effective ablation sites were compared with CMR findings. Among the control subjects, abnormalities in the RV were observed only in 2 out of 10 individuals (prominent fatty deposits). In contrast, CMR scans revealed morphological alterations in the RV free wall in 13 out of 20 patients (65%) with RVOT tachycardia. These changes consisted of the presence of fatty tissue (5 patients), thinning of the wall (9 patients), and dyskinetic wall segments (4 patients). Eight of these patients displayed extra fat deposits, thinning, or a saccular aneurysm in the RV outflow tract and in 6 of these cases, these findings correlated with the location of the ablation site.25
In a study conducted in 2015 in the United States, a group of 1840 participants without clinically apparent cardiovascular disease (mean age 68) underwent LGE-CMR to identify myocardial scars. The results showed that 146 participants (7.9%) had myocardial scars. Surprisingly, 114 (78%) of the patients were classified as “normal” by the electrocardiogram, echocardiography, and clinical examination.33
Cardiac Magnetic Resonance and Late Gadolinium Enhancement in Patients with Premature Ventricular Contractions
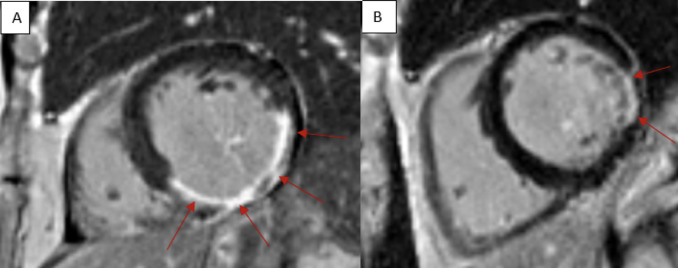
Late gadolinium enhancement cardiac magnetic resonance represents nowadays one of the most valuable imaging tools in modern cardiology, with an impact on the diagnostic and risk stratification of both ischemic and non-ischemic cardiomyopathies. Cardiac magnetic resonance, particularly when used with LGE sequences and quantitative measures like T1-mapping, both native and with extracellular volume fraction measurement, as well as T2-mapping and T2-*mapping, has been validated across a broad spectrum of clinical scenarios through comparison with histological findings. Cardiac magnetic resonance allows for both qualitative and quantitative assessment of individual myocardial scar tissue and fibrosis. Cardiac magnetic resonance techniques proved to be especially valuable in cases where the underlying cause of unclear cardiomyopathy, whether ischemic or non-ischemic, needs to be determined without invasive procedures. By examining the localization and distribution patterns of scars and/or fibrosis, non-invasive CMR can aid in determining the presumed underlying cause (Figure 2).34-36
Figure 2.
Presence of cardiac scar in the inferior and lateral walls of LV (A) and anterolateral wall (B); LV, left ventricle.
With the aim of studying the prevalence of scar detected by CMR in patients without previously known cardiac disease, Ghannam et al included 272 patients with frequent PVCs (mean PVC burden of 20.4% ± 13.0%) and observed that LGE was present in 67 patients (25%). Patients with scar tissue detectable by CMR were older, predominantly male, with comorbidities such as arterial hypertension and chronic obstructive pulmonary disease (COPD). Additionally, they had a lower baseline EF. The majority of these patients, 64 out of 67 (96%), exhibited exclusively intramural scarring. The remaining 3 patients had scar tissue in the papillary muscles, transmural scar on the lateral left ventricular free wall, and epicardial scar near the anterior basal septum. However, the primary scar was predominantly located in the basal septum (62 out of 67, 93%) and all patients with multifocal scar tissue had a component of basal septal scarring. All patients were submitted to programmed ventricular stimulation (PVS) and were observed for the development of VAs. Among the studied group, 7 patients (3%) exhibited inducible VT. The correlation between the extent of LGE-CMR scar and the likelihood of long-term VT occurrence was established, irrespective of EF [HR 18.8 (2.0-176.6), P = .01 and HR 1.4 [1.1-1.7]/cm3 of scar, P < .001, respectively]. The positive and negative predictive value of PVS for VT during long-term follow-up reached percentages of 71% and 100% respectively.29
In a study involving 76 patients with VAs (Lown classification ≥2), who had no known cardiac disease following standard diagnostic procedures, and underwent CMR imaging. Among these patients, 44 out of 76 showed abnormal findings on CMR. Notably, in 24 out of 76 cases, CMR revealed pathology that was not detected by echocardiography and for 20 patients the final diagnosis was based on the CMR pattern. Furthermore, in 7 patients, the location of CMR-detected abnormalities (scars) directly corresponded to the origin of the ventricular arrhythmias. The identification of these CMR findings prompted changes in treatment for 21 patients and/or additional diagnostic procedures for 8 patients. The study concluded that in some patients, subtle changes detected by CMR often serve as significant contributors to VAs, as evidenced by scar morphology.37
In an elaborate study conducted by Andreini et al, a total of 946 patients exhibiting significant ventricular arrhythmias (defined as >1000 PVCs/24 hours, nonsustained VT, sustained ventricular tachycardia, or a history of resuscitated cardiac arrest) and showing no pathological findings on echocardiography were included. The mean age of the participants was 41 ± 16 years, with 64% being men. Cardiac magnetic resonance studies revealed SHD in 241 patients (25.5%) and abnormal findings not specific for a definitive SHD diagnosis in 187 patients (19.7%). The most prevalent conditions were myocarditis (n = 91), arrhythmogenic cardiomyopathy (n = 55), dilated cardiomyopathy (n = 39), ischemic heart disease (n = 22), hypertrophic cardiomyopathy (n = 13), congenital cardiac disease (n = 10), left ventricle noncompaction (n = 5), and pericarditis (n = 5). The study also concluded that CMR imaging could identify SHD in a significant proportion of patients with significant ventricular arrhythmias, despite having normal echocardiography results, based on scar characteristics.38
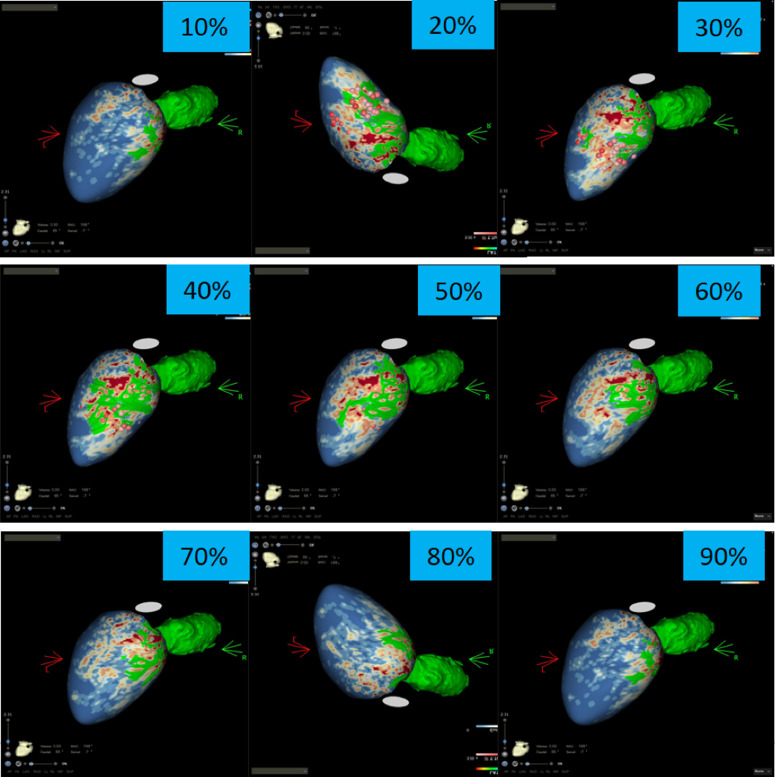
The role of CMR is of extreme importance also for detecting RV pathology in patients with PVCs (Figure 3). In individuals who have both frequent PVCs (defined as at least 5% PVCs in 24 h on any ambulatory ECG monitoring) and multiple RV abnormalities (RVA), such as RV dilatation, fat infiltration, and wall motion abnormalities, experienced poorer outcomes compared to a group without RVA (HR: 48.6; 95% CI: 6.1-384.8; P < .001). Out of the 61 patients in the RVA-2 group, only 6 received a definite diagnosis of arrhythmogenic right ventricular cardiomyopathy (ARVC) based on the 2010 Task Force Criteria. Additionally, individuals with a single imaging criterion for RVA exhibited worse outcomes compared to those without any RVA. Furthermore, patients with wall motion abnormalities in the RV had a higher prevalence of cardiac events compared to the group without RVA (HR: 27.2; 95% CI: 3.0-244.0; P = .03).26,39 In support of this data, in a study published by Hosseini et al32, which included a total of 225 participants with frequent PVCs, 35 had myocardial abnormalities detected by CMR, 28 patients had evidence of LV LGE, out of whom, in 14 patients, the localization of the scar correlated to the origin of the PVCs. They concluded that patients with frequent PVCs who are not known to have any type of structural heart disease but are identified with LGE at CMR have a worse long-term outcome of all-cause mortality, nonfatal episode of ventricular fibrillation or VT, and reduction in LVEF of ≥10% compared to baseline LVEF (HR: 4.35; 95% CI: 1.34-14.15; P = .014).32
Figure 3.
Integration of CMR images for the electroanatomical mapping in a patient with PVCs originating in the RV—extensive epicardial scar tissue at the level of the RVOT.
Myocardial Scar and Major Adverse Cardiac Events
Despite all the data we reported before, there remains the question of whether the presence of LGE in patients with PVCs can be considered a risk factor for future major adverse cardiovascular event (MACE), or just the anatomical substrate. Muser et al1 identified that among the 518 patients included in the study, with at least 1000 PVCs/24 h, otherwise normal 12 lead surface electrocardiogram (ECG), normal transthoracic echocardiography and absence of significant coronary artery disease, myocardial abnormalities were detected by CMR in 85 individuals (16%) who had more than 1000 PVCs within a 24-hour period. After a median follow-up duration of 67 months, a composite endpoint comprising SCD, resuscitated cardiac arrest, nonfatal episodes of ventricular fibrillation or sustained VT that required appropriate implantable cardioverter-defibrillator therapy occurred in 26 patients (5%, P < .01). The incidence of this composite outcome was significantly higher among subjects with myocardial abnormalities observed on CMR imaging, with 25 individuals (29%) experiencing the outcome, compared to only 1 individual (0.2%) without such abnormalities (P < .01).1 In a similar study, Nikolaidou et al 31 included 72 patients with frequent PVCs (>500/24 h) and otherwise normal ECG, echocardiography and no coronary artery disease who were investigated by CMR and reached a similar verdict. Out of the 72 patients, 20.8% were diagnosed with possible PVC-induced cardiomyopathy (P < .001).
In patients with structural heart disease, CMR can help with measuring the ventricular function and volumes, detection, and quantification of LGE, with the aim of better risk stratification. Neilan et al40 included in their study a population of 137 patients with aborted SCD who underwent CMR investigation. Out of the 137 patients, 98 patients had LGE (subendocardial in 47%, transmural in 21%, mid-myocardial in 23%, epicardial in 8%, and at the insertion point of the RV in 1 of the patients), with a median amount of LGE of 9.9% of the LV myocardial mass. In total, 104 patients were discovered with a potential arrhythmic substrate: an infarct-pattern LGE in 60 patients (44%), non-infarct LGE in 21 patients (19%), and active myocarditis in 14 patients (10%). The strongest predictors of recurrent events were the presence of LGE (adjusted HR: 6.7; 95% CI: 2.38-18.85; P < .001) and the extent of LGE (HR: 1.15; 95% CI: 1.11-1.19; P < .001).40
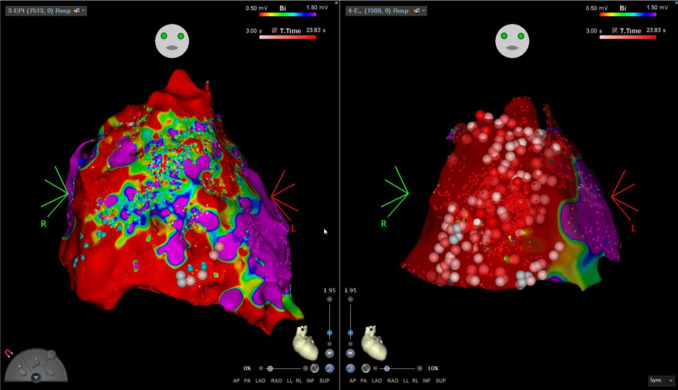
Scar Anatomy and Arrhythmic Risk in Patients with Premature Ventricular Contractions
Apart from the presence of LGE, the anatomy of the scar plays an important role for the management of patients with PVCs. Channels of heterogeneous tissue within the scar, connecting to healthy tissue as identified in LGE-CMR, are more prevalent in patients experiencing VT (88% compared to 33%) (Figure 4). This suggests a potential association with the arrhythmic risk. Subsequent investigations utilizing 3-T scans and specialized imaging software confirmed the effectiveness of LGE-CMR in detecting these channels. This was not only in comparison to electroanatomical voltage maps but also by analyzing electrogram characteristics within the conducting channels. The conducting channels identified by PSI (pixel signal intensity) maps coincided with areas of late potentials in the electroanatomical maps, confirming slow conduction. Additionally, LGE-CMR's ability to distinguish scar tissue within the endocardium, mid-myocardium, and epicardium revealed a 3-dimensional structure of the scar. LGE-CMR demonstrated superior capability in detecting the 3-dimensional pathway of conducting channels, showing higher concordance and improved border zone detection compared to conventional 2-dimensional LGE-CMR.41-43
Figure 4.
Scar analysis (from the endocardium to the epicardium) with dedicated software for the detection of the arrhythmic channels. Blue—normal tissue; red—fibrosis; green—arrhythmic channels.
In a study conducted by Lin et al44, a total of 63 patients with LVEF below 50% and with LGE detected by CMR were included. After a median follow-up period of 1379 days, 8 patients experienced VT/VF episodes, and 14 patients died. Among the CMR-measured parameters, only the likelihood of detecting conducting channels (CCs) via LGE-CMR was higher in patients with VT/VF compared to those without VT/VF (75.0% vs. 16.4%, P < .001). Similarly, the probability of identifying the CC was higher in the group that died (50.0% vs. 16.3%, P = .004). Other LGE-CMR variables did not reach statistical significance. In the univariate Cox regression model, the identification of CC was positively correlated with VT/VF episodes (HR: 27.032, 95% CI: 3.291-222.054, P = .002) and increased overall mortality (HR: 4.766, 95% CI: 1.643-13.824, P = .004). Conversely, LVEF demonstrated an inverse association with VT/VF episodes (HR: 0.119, 95% CI: 0.015-0.977, P = .048) and increased overall mortality (HR: 0.491, 95% CI: 0.261-0.925, P = .028) during the follow-up period and concluded that CC identification using LGE-CMR can help pinpoint heart failure patients at risk for VT/VF.44
In patients with nonischemic cardiomyopathy who presented with intramural scar and who were referred for an ablation procedure of VA (patients with either PVCs and no history of VT or patients with documented VT), the characteristics of the scar influenced the result of the procedure. Patients lacking clinical or inducible VT exhibited smaller overall and core scar dimensions compared to those with a VT history or inducible VT (total scar: 1.12 [0.74‐1.79]/cm3 vs. 7.45 [4.16‐12.21]/cm3, P < .001). A total scar volume of at least 2.78 cm3 correlated with VT inducibility (95% CI [0.89‐0.98], sensitivity 85%, specificity 90%). They concluded that the assessment of scar size in patients with intramural scarring helps in risk evaluation for nonischemic cardiomyopathy and VAs, irrespective of EF or previous VT (adjusted OR 1.67 [1.24‐2.24]/cm3, P < .01).7
Novel Cardiac Magnetic Resonance Sequences for Detecting the Site of Origin of the Premature Ventricular Contractions
Acquiring high-resolution imaging is essential for detecting smaller scar regions and enhancing the assessment of scar geometry in patients undergoing VT or PVCs ablation.45 The incorporation of image acceleration techniques, such as compressed sensing, has facilitated quicker acquisition of 3D imaging with higher spatial resolution (1.2 mm³), maintaining acceptable scan duration and image quality while demonstrating comparable scar characteristics to conventional 3D LGE imaging.46 Additionally, parallel imaging using a stack-of-spirals acquisition technique has enabled rapid 3D LGE acquisitions within a 12-heartbeat breath-hold.47 Three-dimensional free-breathing self-navigating magnetic resonance sequences have been developed to address issues associated with respiratory navigator placement and irregular breathing patterns, enabling high-resolution visualization of scar distribution and improved delineation of scar borders.48 Another emerging technique, super-resolution reconstruction, reconstructs a high-resolution image from multiple low-resolution views of the same volume, demonstrating good agreement with the bipolar voltage range of scar border zone.49 The introduction of dark-blood LGE sequences as a technical solution to suboptimal contrast between scar and the blood pool holds promise for improved substrate assessment. These sequences have been designed to concurrently decrease signal intensity from normal myocardium and the blood pool while enhancing contrast between scar and blood, while also preserving contrast between scar and myocardium. Given that a significant proportion of VTs originate in the sub-endocardial region, improved contrast between scar and the blood pool could enhance substrate detection in these regions.50
Quantification of Scar Volume by Cardiac Magnetic Resonance
The physiological mechanism underlying LGE of myocardial fibrosis results from 2 main factors: an expanded volume of distribution for the contrast agent and a lengthened washout period due to reduced capillary density within the fibrotic myocardial tissue. This combination leads to an elevation in gadolinium concentration within the fibrotic regions, resulting in T1 shortening. Consequently, these areas manifest as bright signal intensity in CMR images using conventional inversion-recovery gradient echo sequences.51,52 Scar volume can influence the arrhythmic risk, as previously described above.
In a study involving 40 patients with hypertrophic cardiomyopathy (mean age 48 years, 30 males) and 20 normal subjects (mean age 38 years, 16 males), who underwent CMR, 3 methods for quantifying LGE were compared. Firstly, the standard deviation (SD) 2 method involved placing a region of interest (ROI) within normal myocardium and defining enhanced myocardium as having signal intensity more than 2 standard deviations above the mean of the ROI. Secondly, the SD 6 method defined enhanced myocardium with a threshold of 6 SD above the mean of the ROI. Thirdly, in the RC method, an ROI was placed in the background of the image, and a Rayleigh curve was generated using the SD of that ROI, serving as an ideal curve for the distribution of signal intensity in perfectly nulled myocardium. Results showed that patients with hypertrophic cardiomyopathy had lower concordance between the measured curve of signal intensity distribution and the Rayleigh curve compared to controls (63.7 ± 12.3% vs. 92.2 ± 2.3%, P < .0001). A concordance cutoff of <82.9% had a sensitivity of 97.1% and specificity of 92.3% in distinguishing hypertrophic cardiomyopathy from controls. The RC method yielded a higher score than the other methods. Although the average extent of enhanced myocardium measured by SD6 and the Rayleigh curve method did not significantly differ, the SD6 method underestimated enhancement in 12% and overestimated it in 5% of hypertrophic cardiomyopathy patients. The conclusion drawn was that quantifying fibrosis in LGE images using a cutoff derived from the Rayleigh curve is more accurate than using a fixed cutoff.53,54
Various methods are available for quantifying cardiac fibrosis volumes, including manual quantification, thresholding by different standard deviations (2, 3, 4, 5, or 6) above remote myocardium, and the full width at half maximum (FWHM) technique.55 In a study led by Flett et al 56 , 60 patients with 3 different causes of LGE were scanned (acute myocardial infarction = 20 patients, chronic myocardial infarction = 20 patients, and hypertrophic cardiomyopathy = 20 patients), and LGE volume was measured using 7 techniques. The study revealed significant variation in LGE volume depending on the quantification method employed. Notably, there was no statistically significant difference between LGE volume measured by the FWHM technique, manual quantification, and the 6-SD or 5-SD techniques. However, the 2-SD technique produced LGE volumes up to twice as high as those obtained with the FWHM, 6-SD, and manual techniques. Additionally, reproducibility was poorer in hypertrophic cardiomyopathy compared to acute myocardial infarction or chronic myocardial infarction. The FWHM technique demonstrated the highest reproducibility across all 3 conditions compared to any other method (P < .001). The conclusion reached by the authors was that irrespective of the underlying disease, the FWHM technique for LGE quantification yields similar results to manual quantification and demonstrates the highest statistical reproducibility, potentially reducing required sample sizes by up to half.56
In different studies which focused on myocarditis,57 mitral valve prolapse,58 and Fabry disease,59 it was concluded that semi-automated grayscale thresholding techniques may be a feasible method for the quantification of cardiac fibrosis.
In a retrospective analysis of the DERIVATE registry, it was investigated whether post-infarct scar identified by LGE-CMR could be quantified fully automatically by machine learning algorithms. They also compared the predictive capabilities of LGE CMR scar analyzed by humans vs. machines in forecasting arrhythmic events. The findings revealed that machine-based assessment of dense or total scar provided additional predictive value beyond the guideline criterion for the association with MACE (AUC: 0.68 vs. 0.63, P = .02 and AUC: 0.67 vs. 0.63, P = .01, respectively). When employing competing risks modeling, dense and total scar showed superior performance compared to the guideline-based risk criteria (AUC: 0.67 vs. 0.61, P = .01 and AUC: 0.66 vs. 0.61, P = .005, respectively). The conclusion reached was that fully automatic machine learning-based analysis of LGE reliably quantifies myocardial scar mass.60
Implications of Late Gadolinium Enhancement Detection for the Catheter Ablation Procedure
In regions where myocardial scar is detected, the presence of viable myocardial fibers within the scar causes the development of slow electrical pathways, creating a proper environment for the formation of reentrant circuits. By either eliminating or isolating this substrate, it is possible to potentially avoid the occurrence of different arrhythmias, especially after integration with the electroanatomical mapping (EAM).61-63
Several studies were conducted in order to determine whether CMR can also help prior to the ablation in the planning phase of the procedure. Ghanam et al30 investigated 333 patients who underwent catheter ablation for PVCs (mean burden of 20.7% ± 13.14) and had no history of sustained ventricular arrhythmias or syncope and were investigated with CMR prior to the ablation. The study found that one-third of the patients referred for PVC ablation had cardiac scar. Through multiple logistic regression analysis, the researchers identified age (OR 1.02 [1.01-1.04]/year, P = .019) and baseline EF as predictive factors for the presence of scar (OR 0.92 [0.89-0.94]/%, P < .001). The study also determined the most common locations from which PVCs originated including: the outflow tracts (34%), intramural locations (17%), epicardial locations (16%), papillary muscle locations (14%), and parahisian locations (5%). Patients with cardiac scar had a lower occurrence of PVCs originating from epicardial and outflow tract sources compared to those without scar (8.0% vs. 20.4%, P = .006 and 25.0% vs. 38.5%, P = .02, respectively). Conversely, intramural sources were more prevalent in patients with scar compared to those without scar (39.3% vs. 6.3%, P < .001). Following the ablation procedure, patients with cardiac scar experienced a higher burden of PVCs and a lower EF post ablation.30,64,65 Penela et al28 included in a study 70 patients with LV dysfunction (mean LVEF = 34%) and frequent PVCs (a mean PVC burden of 23%) who were admitted for catheter ablation procedures. All 70 patients underwent CMR investigation before the ablation procedure and in 29 patients, the LGE sequence identified scar in the myocardium with a median mass of scarring of 10.4 grams. Median scar mass was noticeably smaller in the patients in whom the procedure was a success, but the acute successful ablation rate was similar in the 2 groups (83% in the group with scar and 88% in the group without scar, P = .4).28
In support of this data, Berruezo et al66 included 101 patients with left ventricular scar-related VT defined as the presence of previous myocardial infarction, LV dilatation/systolic dysfunction, or normal LV diameters/systolic function with evidence of ventricular scar on LGE-CMR or EAM. All patients underwent a catheter ablation procedure for VT with conducting channels identification and subsequent channels elimination and concluded that after acquiring CMR images of the scar, scar dechanneling alone results in low recurrence and mortality in 54% of the patients despite the limited ablation extent and recurrences are mainly related to incomplete conducting channels elimination (P = .013).66,67 Andreu et al68 included 30 patients with SHD (defined as the presence of myocardial scar at LGE-CMR) who were referred for VT ablation and compared different CMR methods of the scar. This was done using a navigator-gated 3D sequence (3D-GRE) and conventional 2D imaging techniques, employing either a single-shot inversion-recovery steady-state-free-precession (2D-SSFP) or an inversion-recovery gradient echo (2D-GRE) sequence. The scar components, including the core and border zone, were quantified using different thresholds of maximum pixel intensity (60% and 40%, respectively) in the analysis and each imaging sequence provided a 3D reconstruction of the scar. There were no notable differences in the mass of the scar core between the 2D-GRE, 2D-SSFP, and 3D-GRE sequences (mean values of 7.48 + 6.68, 8.26 + 5.69, and 6.26 + 4.37 grams, respectively; P = .084). However, the mass of the border zone was smaller in the 2D-GRE and 2D-SSFP sequences compared to the 3D-GRE sequence (9.22 + 5.97 and 9.39 + 6.33 vs. 10.92 + 5.98 grams, respectively; P = .042). When comparing the observed critical components in the EAM to the 3D-GRE sequence, a match was found in 79.2% of cases. However, this matching decreased to 61.8% and 37.7% when comparing the EAM to the 2D-GRE and 2D-SSFP sequences.68 In another study published by Yokonawa et al that comprised 321 patients with frequent PVCs, that were investigated by CMR prior to catheter ablation, it was noticed that LGE was present in 60 patients and SHD was present in 64 patients, defined as the LGE pattern of previous myocardial infarction, non-ischemic cardiomyopathy (NICM), RV dilatation and dyskinesis, LV non-compaction, and congenital LV aneurysm. Sustained monomorphic VT was induced in 15 patients. After a median follow-up period of 20 months, the primary endpoint of VT/VF or death occurred in 15. The combination of SHD identified by MRI and VT inducibility granted independently an increased risk of adverse outcome (multivariate HR 25.73, 95% CI: 6.74-98.20, P < .001), concluding that pre-ablation CMR and programmed stimulation can be useful for risk stratification in patients with frequent PVCs.27,69
Using LGE-CMR for planning ablation procedures proves particularly beneficial in assessing scar location and determining the most suitable ablation strategy.41 In this regard, a non-randomized study conducted by Acosta et al70 demonstrated that ischemic patients with epicardial substrate, identified through imaging techniques, who underwent epicardial access experienced superior outcomes in terms of VT recurrence compared to those who solely underwent the endocardial approach. Moreover, the relevance of scar location in NICM patients has also been underscored in guiding the ablation procedure, as it correlates with the type of arrhythmia and the chosen ablation approach.71 This aspect was further validated in a larger study involving 80 patients encompassing both ischemic cardiomyopathy (ICM) and NICM. In this study, the decision between the endocardial or epicardial approach was guided by imaging findings, and access to intramural substrate (within the left and/or right ventricle) was determined based on the proximity of the scar to the left and right endocardium.67
Bogun et al conducted CE-CMR on 29 patients with NICM, identifying scar tissue in 14 patients, 9 of whom experienced monomorphic VTs and 5 expressed PVCs. All 14 patients underwent a catheter ablation, resulting in a successful outcome for 9 of them. Among these 9 patients, 5 solely had endocardial scar, necessitating only endocardial ablation. However, in the remaining 4 patients, the scar was either intramural and epicardial or solely epicardial. Consequently, all 4 patients required an epicardial approach for effective therapy. These findings suggest that CE-CMR's scar localization can lead the decision on whether to pursue epicardial access for catheter ablation of VT.72
Cardiac Magnetic Resonance After the Catheter Ablation Procedure
It was postulated by different authors that CMR may also be used to determine the effectiveness of catheter ablation for VA. Dinov et al noticed that following VA ablation, CMR revealed unenhanced lesions that resembled the no-reflow phenomenon observed in myocardial infarction. They enrolled 25 patients who were studied by CMR before and after a catheter ablation procedure for sustained VT. The dimensions and extent of radiofrequency injury were linked to the energy applied (r = 0.598, P = .002) during ablation and the drop in impedance (r = 0.416, P = .038) and in the failed procedures, the lesions’ volume was insignificantly larger (3.86 ± 3.3% vs. 2.6 ± 1.7%, P = .197), however, it was considerably deeper (86 ± 13% vs. 62 ± 26%, P = 0.03), but the lesions did not appear to be connected to the immediate success of the ablation procedure.73 In addition, Ilg et al74 noticed in a study which included 35 patients without SHD who were addressed for ablation of VAs and investigated before and after the procedure by CMR, that radiofrequency ablation lesions can be detected long term after an ablation procedure targeting ventricular arrhythmias in patients without previous infarction. In 25 of the 35 patients (71%), ablation lesions were identified for a mean of 22 ± 12 months by CMR and the ablation duration correlated with lesion size (r = 0.67, P < .001).74 Dabbagh et al75 observed in a study of 17 patients with repeat ablation procedure for VT, that ablation lesions can be detected by CMR after VT ablation for many months (36 ± 29 months) in post-infarction patients and have a different appearance than scar tissue (confluent subendocardial dark core), with no conductibility in repeat procedures suggesting that dark core may indicate effective ablative lesions, as the CMR dark core was closely correlated with the size of the area of unexcitability (R = 0.98; P< .001).75,76
Conclusion
In conclusion, in recent decades, the perspective on PVCs has shifted as multiple studies have pointed out the role that PVCs may play in the development of LV dysfunction and in the onset or progression of heart failure. Cardiac magnetic resonance developed as an important tool for the detection of subtle structural changes in the myocardium in patients with frequent PVCs, that represent predictors of worse long-term outcomes and can help with risk stratification.
Funding Statement
The authors declare that this study received no financial support.
Footnotes
Ethics Committee Approval: There is no need for ethics approval or informed consent for a narrative review.
Peer-review: Externally peer-reviewed.
Author Contributions: Ș.A., L.Ș., G.S., and C.U. were responsible for the concept and design of the study. C.U. and G.S. were responsible for draft preparation. C.U., G.S., C.S., A.C., and R.A.S. were responsible for the review and editing of the manuscript. C.S., Ș.A., N.S., and L.Ș. were responsible for final draft visualization. C.U., G.S., M.G., and Ș.A. were responsible for the revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Declaration of Interests: The authors have no conflicts of interest to declare.
References
- 1. Muser D, Santangeli P, Castro SA, et al. Risk stratification of patients with apparently idiopathic premature ventricular contractions: a multicenter international CMR registry. JACC Clin Electrophysiol. 2020;6(6):722 735. ( 10.1016/j.jacep.2019.10.015) [DOI] [PubMed] [Google Scholar]
- 2. Nguyen KT, Vittinghoff E, Dewland TA, et al. Ectopy on a single 12-lead ECG, incident cardiac myopathy, and death in the community. J Am Heart Assoc. 2017;6(8). ( 10.1161/JAHA.117.006028) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marcus GM. Evaluation and management of premature ventricular complexes. Circulation. 2020;141(17):1404 1418. ( 10.1161/CIRCULATIONAHA.119.042434) [DOI] [PubMed] [Google Scholar]
- 4. Lee V, Hemingway H, Harb R, Crake T, Lambiase P. The prognostic significance of premature ventricular complexes in adults without clinically apparent heart disease: a meta-analysis and systematic review. Heart (Br Card Soc). 2012;98(17):1290 1298. ( 10.1136/heartjnl-2012-302005) [DOI] [PubMed] [Google Scholar]
- 5. Sassone B, Muser D, Casella M, et al. Detection of concealed structural heart disease by imaging in patients with apparently idiopathic premature ventricular complexes: a review of current literature. Clin Cardiol. 2019;42(12):1162 1169. ( 10.1002/clc.23271) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Muser D, Santangeli P, Selvanayagam JB, Nucifora G. Role of cardiac magnetic resonance imaging in patients with idiopathic ventricular arrhythmias. Curr Cardiol Rev. 2019;15(1):12 23. ( 10.2174/1573403X14666180925095923) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ghannam M, Siontis KC, Cochet H, et al. Risk stratification in patients with nonischemic cardiomyopathy and ventricular arrhythmias based on quantification of intramural delayed enhancement on cardiac magnetic resonance imaging. J Cardiovasc Electrophysiol. 2020;31(7):1762 1769. ( 10.1111/jce.14514) [DOI] [PubMed] [Google Scholar]
- 8. You CX, Liu CF. Premature ventricular contractions and cardiomyopathy. Cardiol Rev. 2019;27(6):322 326. ( 10.1097/CRD.0000000000000262) [DOI] [PubMed] [Google Scholar]
- 9. Tseng AS, Kowlgi GN, DeSimone CV. Management of premature ventricular complexes in the outpatient setting. Mayo Clin Proc. 2023;98(7):1042 1053. ( 10.1016/j.mayocp.2023.01.021) [DOI] [PubMed] [Google Scholar]
- 10. Hoogendijk MG, Géczy T, Yap SC, Szili-Torok T. Pathophysiological mechanisms of premature ventricular complexes. Front Physiol. 2020;11:406. ( 10.3389/fphys.2020.00406) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim YH, Chen SA, Ernst S, et al. 2019 APHRS expert consensus statement on three-dimensional mapping systems for tachycardia developed in collaboration with HRS, EHRA, and LAHRS. J Arrhythm. 2020;36(2):215 270. ( 10.1002/joa3.12308) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kennedy HL, Whitlock JA, Sprague MK, Kennedy LJ, Buckingham TA, Goldberg RJ. Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy. N Engl J Med. 1985;312(4):193 197. ( 10.1056/NEJM198501243120401) [DOI] [PubMed] [Google Scholar]
- 13. Niwano S, Wakisaka Y, Niwano H, et al. Prognostic significance of frequent premature ventricular contractions originating from the ventricular outflow tract in patients with normal left ventricular function. Heart (Br Card Soc). 2009;95(15):1230 1237. ( 10.1136/hrt.2008.159558) [DOI] [PubMed] [Google Scholar]
- 14. Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham Heart Study. Ann Intern Med. 1992;117(12):990 996. ( 10.7326/0003-4819-117-12-990) [DOI] [PubMed] [Google Scholar]
- 15. Sekiguchi Y, Aonuma K, Yamauchi Y, et al. Chronic hemodynamic effects after radiofrequency catheter ablation of frequent monomorphic ventricular premature beats. J Cardiovasc Electrophysiol. 2005;16(10):1057 1063. ( 10.1111/j.1540-8167.2005.40786.x) [DOI] [PubMed] [Google Scholar]
- 16. Yarlagadda RK, Iwai S, Stein KM, et al. Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract. Circulation. 2005;112(8):1092 1097. ( 10.1161/CIRCULATIONAHA.105.546432) [DOI] [PubMed] [Google Scholar]
- 17. Baman TS, Lange DC, Ilg KJ, et al. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm. 2010;7(7):865 869. ( 10.1016/j.hrthm.2010.03.036) [DOI] [PubMed] [Google Scholar]
- 18. Sarrazin JF, Labounty T, Kuhne M, et al. Impact of radiofrequency ablation of frequent post-infarction premature ventricular complexes on left ventricular ejection fraction. Heart Rhythm. 2009;6(11):1543 1549. ( 10.1016/j.hrthm.2009.08.004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ataklte F, Erqou S, Laukkanen J, Kaptoge S. Meta-analysis of ventricular premature complexes and their relation to cardiac mortality in general populations. Am J Cardiol. 2013;112(8):1263 1270. ( 10.1016/j.amjcard.2013.05.065) [DOI] [PubMed] [Google Scholar]
- 20. Dukes JW, Dewland TA, Vittinghoff E, et al. Ventricular ectopy as a predictor of heart failure and death. J Am Coll Cardiol. 2015;66(2):101 109. ( 10.1016/j.jacc.2015.04.062) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Agarwal SK, Simpson RJ, Rautaharju P, et al. Relation of ventricular premature complexes to heart failure (from the Atherosclerosis Risk In Communities [ARIC] Study). Am J Cardiol. 2012;109(1):105 109. ( 10.1016/j.amjcard.2011.08.009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Del Carpio Munoz F, Syed FF, Noheria A, et al. Characteristics of premature ventricular complexes as correlates of reduced left ventricular systolic function: study of the burden, duration, coupling interval, morphology and site of origin of PVCs. J Cardiovasc Electrophysiol. 2011;22(7):791 798. ( 10.1111/j.1540-8167.2011.02021.x) [DOI] [PubMed] [Google Scholar]
- 23. Cheriyath P, He F, Peters I, et al. Relation of atrial and/or ventricular premature complexes on a two-minute rhythm strip to the risk of sudden cardiac death (the Atherosclerosis Risk in Communities [ARIC] study). Am J Cardiol. 2011;107(2):151 155. ( 10.1016/j.amjcard.2010.09.002) [DOI] [PubMed] [Google Scholar]
- 24. Ganesan AN, Gunton J, Nucifora G, McGavigan AD, Selvanayagam JB. Impact of Late Gadolinium Enhancement on mortality, sudden death and major adverse cardiovascular events in ischemic and nonischemic cardiomyopathy: a systematic review and meta-analysis. Int J Cardiol. 2018;254:230 237. ( 10.1016/j.ijcard.2017.10.094) [DOI] [PubMed] [Google Scholar]
- 25. Globits S, Kreiner G, Frank H, et al. Significance of morphological abnormalities detected by MRI in patients undergoing successful ablation of right ventricular outflow tract tachycardia. Circulation. 1997;96(8):2633 2640. ( 10.1161/01.cir.96.8.2633) [DOI] [PubMed] [Google Scholar]
- 26. Aquaro GD, Pingitore A, Strata E, Di Bella G, Molinaro S, Lombardi M. Cardiac magnetic resonance predicts outcome in patients with premature ventricular complexes of left bundle branch block morphology. J Am Coll Cardiol. 2010;56(15):1235 1243. ( 10.1016/j.jacc.2010.03.087) [DOI] [PubMed] [Google Scholar]
- 27. Yokokawa M, Siontis KC, Kim HM, et al. Value of cardiac magnetic resonance imaging and programmed ventricular stimulation in patients with frequent premature ventricular complexes undergoing radiofrequency ablation. Heart Rhythm. 2017;14(11):1695 1701. ( 10.1016/j.hrthm.2017.06.040) [DOI] [PubMed] [Google Scholar]
- 28. Penela D, Martínez M, Fernández-Armenta J, et al. Influence of myocardial scar on the response to frequent premature ventricular complex ablation. Heart (Br Card Soc). 2019;105(5):378 383. ( 10.1136/heartjnl-2018-313452) [DOI] [PubMed] [Google Scholar]
- 29. Ghannam M, Siontis KC, Kim MH, et al. Risk stratification in patients with frequent premature ventricular complexes in the absence of known heart disease. Heart Rhythm. 2020;17(3):423 430. ( 10.1016/j.hrthm.2019.09.027) [DOI] [PubMed] [Google Scholar]
- 30. Ghannam M, Siontis KC, Kim HM, et al. Factors predictive for delayed enhancement in cardiac resonance imaging in patients undergoing catheter ablation of premature ventricular complexes. Heart Rhythm. 2021;2(1):64 72. ( 10.1016/j.hroo.2020.11.004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nikolaidou C, Kotanidis CP, Wijesurendra R, et al. Cardiac magnetic resonance to detect the underlying substrate in patients with frequent idiopathic ventricular arrhythmias. Diagnostics (Basel). 2021;11(6). ( 10.3390/diagnostics11061109) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hosseini F, Thibert MJ, Gulsin GS, et al. Cardiac magnetic resonance in the evaluation of patients with frequent premature ventricular complexes. JACC Clin Electrophysiol. 2022;8(9):1122 1132. ( 10.1016/j.jacep.2022.06.021) [DOI] [PubMed] [Google Scholar]
- 33. Turkbey EB, Nacif MS, Guo M, et al. Prevalence and correlates of myocardial scar in a US cohort. JAMA. 2015;314(18):1945 1954. ( 10.1001/jama.2015.14849) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sohns C, Guckel D, Piran M, Bergau L, El Hamriti M, Sommer P. Treatment of premature ventricular contractions in patients with structural heart disease : insights from imaging. Herzschrittmacherther Elektrophysiol. 2021;32(1):34 40. ( 10.1007/s00399-021-00740-z) [DOI] [PubMed] [Google Scholar]
- 35. Patel AR, Kramer CM. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc Imaging. 2017;10(10 Pt A):1180 1193. ( 10.1016/j.jcmg.2017.08.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kramer CM. Role of cardiac MR imaging in cardiomyopathies. J Nucl Med. 2015;56(suppl 4):39S 45S. ( 10.2967/jnumed.114.142729) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Weisser-Thomas J, Ferrari VA, Lakghomi A, et al. Prevalence and clinical relevance of the morphological substrate of ventricular arrhythmias in patients without known cardiac conditions detected by cardiovascular MR. Br J Radiol. 2014;87(1038):20140059. ( 10.1259/bjr.20140059) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Andreini D, Dello Russo A, Pontone G, et al. CMR for identifying the substrate of ventricular arrhythmia in patients with normal echocardiography. JACC Cardiovasc Imaging. 2020;13(2 Pt 1):410 421. ( 10.1016/j.jcmg.2019.04.023) [DOI] [PubMed] [Google Scholar]
- 39. Marcus FI, Bluemke DA, Calkins H, Sorrell VL. Cardiac magnetic resonance for risk stratification of patients with frequent premature ventricular contractions. J Am Coll Cardiol. 2011;57(15):1636 1638. ( 10.1016/j.jacc.2010.11.039) [DOI] [PubMed] [Google Scholar]
- 40. Neilan TG, Farhad H, Mayrhofer T, et al. Late gadolinium enhancement among survivors of sudden cardiac arrest. JACC Cardiovasc Imaging. 2015;8(4):414 423. ( 10.1016/j.jcmg.2014.11.017) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Roca-Luque I, Mont-Girbau L. Cardiac magnetic resonance for ventricular tachycardia ablation and risk stratification. Front Cardiovasc Med. 2021;8:797864. ( 10.3389/fcvm.2021.797864) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Perez-David E, Arenal A, Rubio-Guivernau JL, et al. Noninvasive identification of ventricular tachycardia-related conducting channels using contrast-enhanced magnetic resonance imaging in patients with chronic myocardial infarction: comparison of signal intensity scar mapping and endocardial voltage mapping. J Am Coll Cardiol. 2011;57(2):184 194. ( 10.1016/j.jacc.2010.07.043) [DOI] [PubMed] [Google Scholar]
- 43. Fernández-Armenta J, Berruezo A, Andreu D, et al. Three-dimensional architecture of scar and conducting channels based on high resolution ce-CMR: insights for ventricular tachycardia ablation. Circ Arrhythm Electrophysiol. 2013;6(3):528 537. ( 10.1161/CIRCEP.113.000264) [DOI] [PubMed] [Google Scholar]
- 44. Lin LY, Su MYM, Chen JJ, et al. Conductive channels identified with contrast-enhanced MR imaging predict ventricular tachycardia in systolic heart failure. JACC Cardiovasc Imaging. 2013;6(11):1152 1159. ( 10.1016/j.jcmg.2013.05.017) [DOI] [PubMed] [Google Scholar]
- 45. Mukherjee RK, Whitaker J, Williams SE, Razavi R, O’Neill MD. Magnetic resonance imaging guidance for the optimization of ventricular tachycardia ablation. Europace. 2018;20(11):1721 1732. ( 10.1093/europace/euy040) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Basha TA, Akçakaya M, Liew C, et al. Clinical performance of high-resolution late gadolinium enhancement imaging with compressed sensing. J Magn Reson Imaging. 2017;46(6):1829 1838. ( 10.1002/jmri.25695) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shin T, Lustig M, Nishimura DG, Hu BS. Rapid single-breath-hold 3D late gadolinium enhancement cardiac MRI using a stack-of-spirals acquisition. J Magn Reson Imaging. 2014;40(6):1496 1502. ( 10.1002/jmri.24494) [DOI] [PubMed] [Google Scholar]
- 48. Rutz T, Piccini D, Coppo S, et al. Improved border sharpness of post-infarct scar by a novel self-navigated free-breathing high-resolution 3D whole-heart inversion recovery magnetic resonance approach. Int J Cardiovasc Imaging. 2016;32(12):1735 1744. ( 10.1007/s10554-016-0963-4) [DOI] [PubMed] [Google Scholar]
- 49. Dzyubachyk O, Tao Q, Poot DHJ, et al. Super-resolution reconstruction of late gadolinium-enhanced MRI for improved myocardial scar assessment. J Magn Reson Imaging. 2015;42(1):160 167. ( 10.1002/jmri.24759) [DOI] [PubMed] [Google Scholar]
- 50. Kellman P, Xue H, Olivieri LJ, et al. Dark blood late enhancement imaging. J Cardiovasc Magn Reson. 2016;18(1):77. ( 10.1186/s12968-016-0297-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol. 2011;57(8):891 903. ( 10.1016/j.jacc.2010.11.013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schalla S, Bekkers SC, Dennert R, et al. Replacement and reactive myocardial fibrosis in idiopathic dilated cardiomyopathy: comparison of magnetic resonance imaging with right ventricular biopsy. Eur J Heart Fail. 2010;12(3):227 231. ( 10.1093/eurjhf/hfq004) [DOI] [PubMed] [Google Scholar]
- 53. Aquaro GD, Positano V, Pingitore A, et al. Quantitative analysis of late gadolinium enhancement in hypertrophic cardiomyopathy. J Cardiovasc Magn Reson. 2010;12(1):21. ( 10.1186/1532-429X-12-21) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Takashio S, Yamamuro M, Uemura T, et al. Correlation between extent of myocardial fibrosis assessed by cardiac magnetic resonance and cardiac troponin T release in patients with nonischemic heart failure. Am J Cardiol. 2014;113(10):1697 1704. ( 10.1016/j.amjcard.2014.02.029) [DOI] [PubMed] [Google Scholar]
- 55. Spiewak M, Malek LA, Misko J, et al. Comparison of different quantification methods of late gadolinium enhancement in patients with hypertrophic cardiomyopathy. Eur J Radiol. 2010;74(3):e149 e153. ( 10.1016/j.ejrad.2009.05.035) [DOI] [PubMed] [Google Scholar]
- 56. Flett AS, Hasleton J, Cook C, et al. Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging. 2011;4(2):150 156. ( 10.1016/j.jcmg.2010.11.015) [DOI] [PubMed] [Google Scholar]
- 57. Gräni C, Eichhorn C, Bière L, et al. Comparison of myocardial fibrosis quantification methods by cardiovascular magnetic resonance imaging for risk stratification of patients with suspected myocarditis. J Cardiovasc Magn Reson. 2019;21(1):14. ( 10.1186/s12968-019-0520-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cecere A, Cipriani A, De Lazzari M, et al. Left ventricular fibrosis in arrhythmic mitral valve prolapse: quantification and comparison of semi-automated techniques assessed by cardiac magnetic resonance. Int J Cardiovasc Imaging. 2024;40(2):275 285. ( 10.1007/s10554-023-03006-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sokolska J, Karolyi M, Bataiosu D, et al. Myocardial fibrosis quantification methods by cardiovascular magnetic resonance imaging with contrast-enhancement in patients with Fabry disease. Eur Heart J Cardiovasc Imaging. 2021;22(suppl 2). ( 10.1093/ehjci/jeab090.022) [DOI] [Google Scholar]
- 60. Ghanbari F, Joyce T, Lorenzoni V, et al. AI cardiac MRI scar analysis aids prediction of major arrhythmic events in the multicenter Derivate registry. Radiology. 2023;307(3):e222239. ( 10.1148/radiol.222239) [DOI] [PubMed] [Google Scholar]
- 61. Muser D, Santangeli P, Liang JJ. Mechanisms of ventricular arrhythmias and implications for catheter ablation. Card Electrophysiol Clin. 2022;14(4):547 558. ( 10.1016/j.ccep.2022.07.006) [DOI] [PubMed] [Google Scholar]
- 62. Di Biase L, Burkhardt JD, Lakkireddy D, et al. Ablation of stable VTs versus substrate ablation in ischemic cardiomyopathy: the VISTA randomized multicenter trial. J Am Coll Cardiol. 2015;66(25):2872 2882. ( 10.1016/j.jacc.2015.10.026) [DOI] [PubMed] [Google Scholar]
- 63. Andreu D, Berruezo A, Ortiz-Pérez JT, et al. Integration of 3D electroanatomic maps and magnetic resonance scar characterization into the navigation system to guide ventricular tachycardia ablation. Circ Arrhythm Electrophysiol. 2011;4(5):674 683. ( 10.1161/CIRCEP.111.961946) [DOI] [PubMed] [Google Scholar]
- 64. Barkagan M, Leshem E, Shapira-Daniels A, et al. Histopathological characterization of radiofrequency ablation in ventricular scar tissue. JACC Clin Electrophysiol. 2019;5(8):920 931. ( 10.1016/j.jacep.2019.05.011) [DOI] [PubMed] [Google Scholar]
- 65. Oebel S, Dinov B, Arya A, et al. ECG morphology of premature ventricular contractions predicts the presence of myocardial fibrotic substrate on cardiac magnetic resonance imaging in patients undergoing ablation. J Cardiovasc Electrophysiol. 2017;28(11):1316 1323. ( 10.1111/jce.13309) [DOI] [PubMed] [Google Scholar]
- 66. Berruezo A, Fernández-Armenta J, Andreu D, et al. Scar dechanneling: new method for scar-related left ventricular tachycardia substrate ablation. Circ Arrhythm Electrophysiol. 2015;8(2):326 336. ( 10.1161/CIRCEP.114.002386) [DOI] [PubMed] [Google Scholar]
- 67. Andreu D, Ortiz-Pérez JT, Boussy T, et al. Usefulness of contrast-enhanced cardiac magnetic resonance in identifying the ventricular arrhythmia substrate and the approach needed for ablation. Eur Heart J. 2014;35(20):1316 1326. ( 10.1093/eurheartj/eht510) [DOI] [PubMed] [Google Scholar]
- 68. Andreu D, Ortiz-Pérez JT, Fernández-Armenta J, et al. 3D delayed-enhanced magnetic resonance sequences improve conducting channel delineation prior to ventricular tachycardia ablation. Europace. 2015;17(6):938 945. ( 10.1093/europace/euu310) [DOI] [PubMed] [Google Scholar]
- 69. Halliday BP, Gulati A, Ali A, et al. Association between midwall late gadolinium enhancement and sudden cardiac death in patients with dilated cardiomyopathy and mild and moderate left ventricular systolic dysfunction. Circulation. 2017;135(22):2106 2115. ( 10.1161/CIRCULATIONAHA.116.026910) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Acosta J, Fernández-Armenta J, Penela D, et al. Infarct transmurality as a criterion for first-line endo-epicardial substrate-guided ventricular tachycardia ablation in ischemic cardiomyopathy. Heart Rhythm. 2016;13(1):85 95. ( 10.1016/j.hrthm.2015.07.010) [DOI] [PubMed] [Google Scholar]
- 71. Piers SR, Tao Q, de Riva Silva M, et al. CMR-based identification of critical isthmus sites of ischemic and nonischemic ventricular tachycardia. JACC Cardiovasc Imaging. 2014;7(8):774 784. ( 10.1016/j.jcmg.2014.03.013) [DOI] [PubMed] [Google Scholar]
- 72. Bogun FM, Desjardins B, Good E, et al. Delayed-enhanced magnetic resonance imaging in nonischemic cardiomyopathy: utility for identifying the ventricular arrhythmia substrate. J Am Coll Cardiol. 2009;53(13):1138 1145. ( 10.1016/j.jacc.2008.11.052) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Dinov B, Oebel S, Hilbert S, et al. Characteristics of the ablation lesions in cardiac magnetic resonance imaging after radiofrequency ablation of ventricular arrhythmias in relation to the procedural success. Am Heart J. 2018;204:68 75. ( 10.1016/j.ahj.2018.06.014) [DOI] [PubMed] [Google Scholar]
- 74. Ilg K, Baman TS, Gupta SK, et al. Assessment of radiofrequency ablation lesions by CMR imaging after ablation of idiopathic ventricular arrhythmias. JACC Cardiovasc Imaging. 2010;3(3):278 285. ( 10.1016/j.jcmg.2009.09.028) [DOI] [PubMed] [Google Scholar]
- 75. Dabbagh GS, Ghannam M, Siontis KC, et al. Magnetic resonance mapping of catheter ablation lesions after post-infarction ventricular tachycardia ablation. JACC Cardiovasc Imaging. 2021;14(3):588 598. ( 10.1016/j.jcmg.2020.08.041) [DOI] [PubMed] [Google Scholar]
- 76. Tao S, Guttman MA, Fink S, et al. Ablation lesion characterization in scarred substrate assessed using cardiac magnetic resonance. JACC Clin Electrophysiol. 2019;5(1):91 100. ( 10.1016/j.jacep.2018.11.001) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a