Abstract
Artificial intelligence (AI) has become increasingly prevalent and significant across many industries, including the dental field. AI has shown accuracy and precision in detecting, evaluating, and predicting diseases. It can imitate human intelligence to carry out sophisticated predictions and decision-making in the health-care industry, especially in endodontics. AI models have demonstrated a wide range of applications in the field of endodontics. These include examining the anatomy of the root canal system, predicting the survival of dental pulp stem cells, gauging working lengths, identifying per apical lesions and root fractures, and predicting the outcome of retreatment treatments. Future uses of this technology were discussed in terms of robotic endodontic surgery, drug–drug interactions, patient care, scheduling, and prognostic diagnosis.
Keywords: Computer-aided design, intelligence, root canal therapy, smiling
Introduction
When we consider artificial intelligence (AI), the first thing that comes to mind is “Can a machine think?” Scientists and researchers have long been fascinated by “THE BRAIN,” one of the most fascinating parts of the human body. The scientific community has never fully grasped how to develop an ideal model that perfectly replicates the human brain.[1,2] Despite numerous challenges, “AI” has become increasingly significant in all spheres of life due to its unstoppable advancement.[3,4] The term AI refers to the ability of a machine or software to replicate human intellect for specific tasks through technology.[5,6,7,8] To help with the early detection of dental conditions such as cavities, periodontal disease, and oral cancers, AI-powered algorithms can analyze enormous amounts of dental images and patient data faster than a dentist can blink. By quickly and accurately identifying abnormalities, dentists can intervene at an early stage, leading to more effective and minimally invasive treatment outcomes [Figure 1].[1,9,10] The prognosis for the patient is improved, and fewer expensive procedures and treatments are required as a result. In the fields of endodontics and esthetic dentistry, AI presents a wide range of advantages, including the ability to detect morphological abnormalities, errors in the location of new canals, working length (WL) determination, retreatment procedures, reduction of root fractures, regenerative endodontic procedures, improved diagnosis and treatment planning, and personalized treatment and prosthetics, virtual simulation, and augmented reality, and smile designing.[11,12,13]
Figure 1.
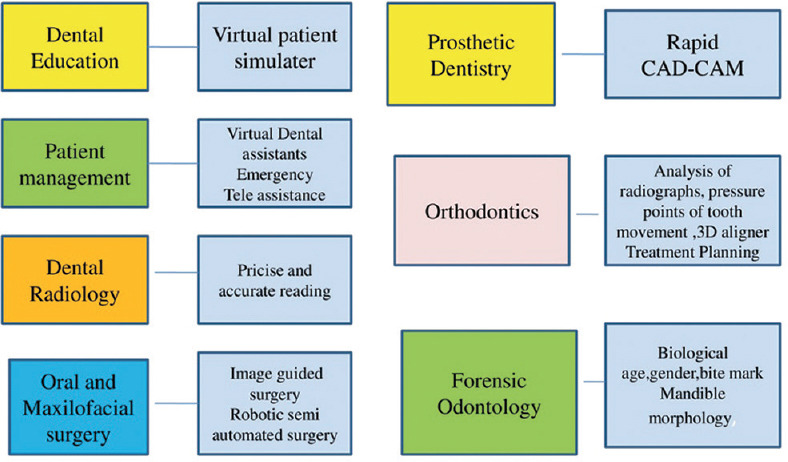
Various applications of artificial intelligence in dentistry.[1] 3D: Three-dimensional, CAD: Computer-aided design, CAM: Computer-aided manufacturing
To fully comprehend the potential of AI in endodontics, it is essential to understand the concepts of deep learning, machine learning, big data, and scientific data. Deep learning is a subset of machine learning that aims to mimic the human brain’s neural networks. It involves training algorithms on large datasets to make accurate predictions or classifications. Machine learning, on the other hand, is a broader concept that encompasses various algorithms and techniques for analyzing and interpreting data. Big data refers to the massive volume of structured and unstructured data that is generated in endodontic practice, including patient records, clinical notes, imaging data, and more. By utilizing big data, AI algorithms can extract valuable insights and patterns that may be difficult for humans to identify. Scientific data, in the context of endodontics, refers to the research and empirical evidence gathered in the field. This data includes studies, clinical trials, and experimental data that inform evidence-based practice in endodontics. Understanding and leveraging deep learning, machine learning, big data, and scientific data in the field of endodontics is crucial for harnessing the full potential of AI in improving diagnosis, treatment planning, and outcomes for patients [Figure 2].[14]
Figure 2.
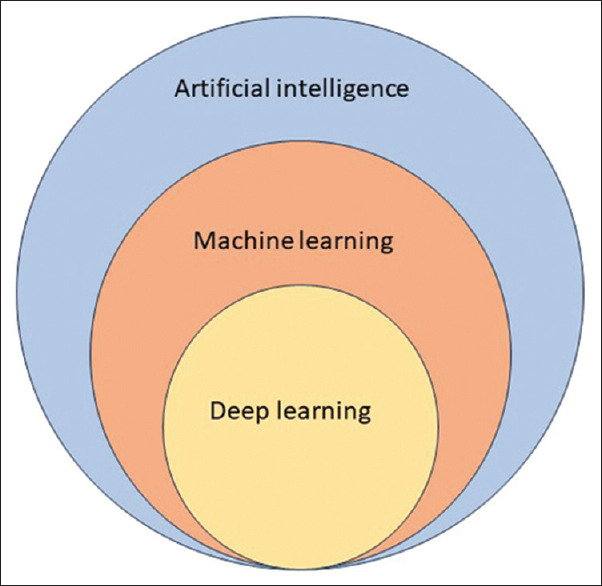
Key element of artificial intelligence[14]
Hence, the present article will enlighten in the application, limitations, advantages, and gaps in the field of AI in endodontics.
Application of Artificial Intelligence in Endodontics
AI is becoming more and more important in endodontics. It is currently becoming more important for diagnosing diseases and planning endodontic treatments.[13,14] AI-based networks can detect even minute to insignificant changes at the level of a single pixel that the human eye might miss.[15,16] A few of its applications in endodontics are mentioned in Figure 3. AI models such as convolutional neural networks (CNNs) and artificial neural networks (ANNs) have been used in endodontics to study root canal system anatomy, determine WL measurements, detect periapical lesions and root fractures, and predict the success of retreatment procedures. CNNs are well-suited for image-related tasks, such as segmentation and pattern recognition, while ANNs are valuable for decision support, predictive modeling, and integrating diverse datasets. Combining these approaches can enhance the overall understanding and management of the root canal system in endodontics.[2,4] ANN learns from input data and adjusts connection weights to minimize errors between predicted and actual outcomes. CNN is specialized for processing visual data like images. It comprises convolutional layers, pooling layers, and fully connected layers. These layers to extract features from input images, followed by pooling layers to reduce dimensionality.[17]
Figure 3.
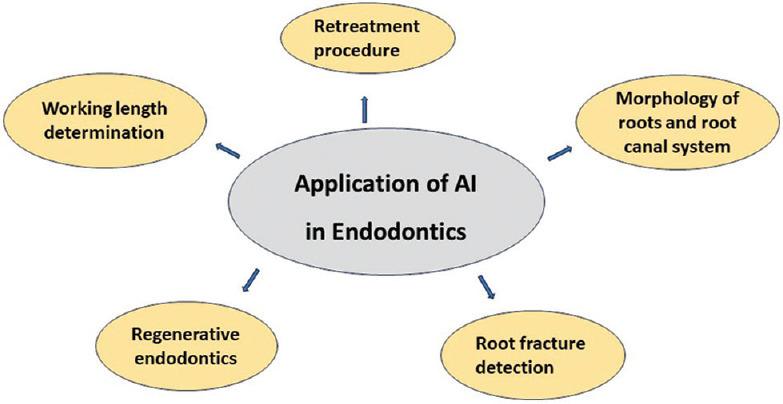
Artificial intelligence application in endodontic dentistry.[15,16,17] AI: Artificial intelligence
Morphology of root and root canal system
The success of nonsurgical root canal therapy depends critically on an understanding of the various kinds of roots and root canal systems. Periapical radiography and cone-beam computed tomography imaging have frequently been used for this purpose.[18,19] Radiological imaging is tightly associated with endodontic treatment because it is used to clinically examine the morphology of the root canal. Panoramic radiographs – A two-dimensional (2D) imaging technique – may be insufficient to comprehend the morphology of root canals. Two distinct CNN algorithms were developed and their estimation performances were compared in a study that sought to estimate the number of distal roots of mandibular first molars on panoramic radiographs. These teeth are single in most of the population and occasionally may have accessory canals. The two performers’ performances did not differ significantly from one another.[20,21]
Working length determination
Choosing the appropriate WL is essential to guarantee the effectiveness of root canal therapy. Inadequate WL determination frequently results in flare-ups, periapical foreign body reactions, inadequate microbiological control, and instrumentation beyond the apical foramen.[11,22] There are several methods for determining the apical foramen and WL, including radiography, digital tactile sense, and the patient’s reactions to a file or paper point.[23,24] Digital technology has shown advantages in locating the apical foramen as well as disadvantages in terms of errors. Consequently, research has been done on the application of ANNs to estimate the correct WL of teeth. Saghiri et al.[25,26] stated that ANNs can act as a second opinion to locate the Apical foramen (AF) on radiographs to enhance the accuracy of WL determination by radiography. In addition, ANN can function as a decision-making system in various similar clinical situations. ANN technique in a human cadaver model to the WL demonstrated an outstanding accuracy of 96%, which is higher than the accuracy of expert endodontists (76%). These findings matched those of another study by the same author and his associates, who used feature extraction processes from radiographs before processing the data with an ANN. The study found that finding the minor apical foramen was 93% accurate.[27,28]
Retreatment procedures
The system’s ability to accurately predict the outcome of the retreatment is one of its strongest points. The limitation was that the system’s accuracy could only correspond with the data.[29,30] While predicting the outcome of retreatment through AI is a valuable aspect for clinical decision-making, it is essential to acknowledge and address the limitations to ensure responsible and informed application in real-world health-care scenarios. Case-based reasoning is developing solutions to problems based on prior experiences with related problems. Relevant knowledge and information may be included by locating related situations. This system may have the issue of variability and the prevalence of different approaches.[31,32] AI plays a significant role in advancing endodontic retreatment procedures, offering innovative solutions to enhance precision, efficiency, and outcomes. Here’s how AI is integrated into the retreatment processes in endodontics: image analysis and diagnosis, automated treatment planning, root canal system segmentation, predictive outcomes modeling, patient-specific risk assessment, posttreatment follow-up, and evaluation.
The integration of AI in endodontic retreatment procedures holds promise for improving diagnostics, treatment planning, and overall decision-making. The ability of AI to process complex datasets and provide valuable insights contributes to a more precise and personalized approach to endodontic retreatment.[2,4]
Root fracture detection
Radiographs and cone-beam computed tomography (CBCT) imaging help detect a vertical root fracture (VRF), which can be difficult to diagnose. Furthermore, if a definitive diagnosis is not made, unnecessary surgery or tooth extraction may result. When it comes to identifying VRFs, traditional radiography’s low sensitivity and clinical presentation typically restrict a clinician’s diagnostic options.[33,34] According to Fukuda et al., the utilization of a CNN could serve as a beneficial means for detecting VRFs in panoramic radiographs. In an alternate investigation, a neural network underwent training to distinguish VRFs in teeth, encompassing both intact and root-filled conditions, by analyzing periapical radiographs and CBCT images.[34,35,36,37] They discovered that fracture identification of roots on CBCT images is superior in terms of specificity, accuracy, and sensitivity when compared to images from 2D radiographs. Shah et al. created an innovative approach capable of automatically detecting, quantifying, and pinpointing cracks in high-resolution CBCT (hr-CBCT) scans of teeth. This method utilizes steerable wavelets and learning techniques. Initial outcomes were derived from hr-CBCT scans of both healthy teeth and teeth with artificially induced longitudinal cracks. These mathematical operations allow weak signal recovery from noisy settings in a machine learning method. Steerable wavelets were successfully used to identify fractures in hr-CBCT images, despite the small sample size.[38]
Regenerative Endodontics
The integration of AI into regenerative endodontics signifies a transformative approach toward enhancing treatment efficacy and patient outcomes. AI-driven research accelerates the development of novel techniques and materials in regenerative endodontics, fostering continual innovation, and refinement of treatment modalities. In a study, Bindal et al. evaluated the stem cells taken from the pulp of teeth in various regenerative therapies using the neuro fuzzy inference method. This approach predicted the outcome by measuring the stem cells’ survival after being treated with bacterial lipopolysaccharides in a clinical scenario model.[36] To forecast cell survival following a range of regeneration processes susceptible to microbial infection, the neuro-fuzzy inference system was suggested as a useful instrument.[39,40] The scientists gave pulp stem cells lipopolysaccharide to cause an inflammatory response, and then they tested the cells’ viability. The accuracy of the prediction was then assessed by the researchers using adaptive neuro-fuzzy interferences to predict the survival of these stem cells after microbial invasion.[41,42]
Shortcoming and Gaps in Artificial Intelligence and Endodontics
The health-care system requires a standard programming technology for organizing appointments, managing patients, and periodic recall. This system also has to be updated regularly to keep up with the changes occurring in the health-care sector
The cost of setting up an AI-based system in the independent clinic would not be feasible
The availability of patient data using individual health records can prove to be useful in informing dentists about adverse reactions to the use of certain drugs and/or the adjustments required in the treatment protocol. However, this can be a disadvantage, as misuse of information can also occur through the AI channels
No protocol has been devised yet to provide a precise diagnosis that would affect the prediction of outcomes or determination of the prognosis. The clarity of this diagnosis would be based on the clinical findings
Dynamic navigations in endodontic surgery can be improved with the help of AI, very minimal number of studies investigate these techniques and it is highly recommended that further studies be done to check and assess robotically guided placement endodontics.[17,41,42]
Benefits to Doctors and Patients
AI demonstrated accuracy and precision in terms of detection, determination, and disease prediction in endodontics. AI can contribute to the improvement of diagnosis and treatment and can lead to an increase in the success of endodontic treatment outcomes. The future of this technology was discussed in light of helping with scheduling, treating patients, drug–drug interactions, diagnosis with prognostic values, and robotic-assisted endodontic surgery.[17]
Conclusion
The integration of AI in endodontics marks a transformative paradigm, enhancing diagnostic precision and treatment efficacy. From the nuanced analysis of root canal system anatomy to predicting outcomes of retreatment procedures, AI brings unprecedented advancements. The potential to detect minute anomalies and optimize WL determination showcases its invaluable role. While challenges such as standardization and ethical considerations persist, AI’s trajectory promises to revolutionize endodontic practices, ushering in an era of personalized, efficient, and technologically augmented dental care. As AI continues to evolve, its collaborative synergy with dental professionals holds the key to further refining and advancing endodontic outcomes.
ANNs, CNNs, and other advanced techniques play pivotal roles in diagnosing various aspects of endodontic conditions, including canal morphology, retreatment, WL determination, regenerative endodontics, and root fractures.
The increasing popularity of interdisciplinary dentistry in the upcoming decades makes it imperative to evaluate the value of AI and its potential applications in endodontics. AI and other modified bioengineering components could change the course of the highly researched field of endodontics. The integration of AI across diverse fields of knowledge has the potential to enhance patient care. The integration of AI technology with traditional methods can reduce the possibility of interpreting errors and be easily implemented into regular clinical practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Agrawal P, Nikhade P. Artificial intelligence in dentistry: Past, present, and future. Cureus. 2022;14:e27405. doi: 10.7759/cureus.27405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boreak N. Effectiveness of artificial intelligence applications designed for endodontic diagnosis, decision-making, and prediction of prognosis: A systematic review. J Contemp Dent Pract. 2020;21:926–34. [PubMed] [Google Scholar]
- 3.Tandon D, Rajawat J. Present and future of artificial intelligence in dentistry. J Oral Biol Craniofac Res. 2020;10:391–6. doi: 10.1016/j.jobcr.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aminoshariae A, Kulild J, Nagendrababu V. Artificial intelligence in endodontics: Current applications and future directions. J Endod. 2021;47:1352–7. doi: 10.1016/j.joen.2021.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Schwendicke F, Samek W, Krois J. Artificial intelligence in dentistry: Chances and challenges. J Dent Res. 2020;99:769–74. doi: 10.1177/0022034520915714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shan T, Tay FR, Gu L. Application of artificial intelligence in dentistry. J Dent Res. 2021;100:232–44. doi: 10.1177/0022034520969115. [DOI] [PubMed] [Google Scholar]
- 7.Ossowska A, Kusiak A, Świetlik D. Artificial intelligence in dentistry-narrative review. Int J Environ Res Public Health. 2022;19:3449. doi: 10.3390/ijerph19063449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asiri AF, Altuwalah AS. The role of neural artificial intelligence for diagnosis and treatment planning in endodontics: A qualitative review. Saudi Dent J. 2022;34:270–81. doi: 10.1016/j.sdentj.2022.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leslie-Mazwi TM, Lev MH. Towards artificial intelligence for clinical stroke care. Nat Rev Neurol. 2020;16:5–6. doi: 10.1038/s41582-019-0287-9. [DOI] [PubMed] [Google Scholar]
- 10.Pauwels R, Brasil DM, Yamasaki MC, Jacobs R, Bosmans H, Freitas DQ, et al. Artificial intelligence for detection of periapical lesions on intraoral radiographs: Comparison between convolutional neural networks and human observers. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131:610–6. doi: 10.1016/j.oooo.2021.01.018. [DOI] [PubMed] [Google Scholar]
- 11.Khanagar SB, Al-Ehaideb A, Maganur PC, Vishwanathaiah S, Patil S, Baeshen HA, et al. Developments, application, and performance of artificial intelligence in dentistry –A systematic review. J Dent Sci. 2021;16:508–22. doi: 10.1016/j.jds.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laureano-Cruces AL, El Alami M, de Arriaga F, Ramírez-Rodríguez J, Sánchez-Guerrero L. Artificial intelligence: Milestones and currents. Int J Innov Sci Eng Technol. 2020;7:332–51. [Google Scholar]
- 13.Bhattacharya S, Pradhan KB, Bashar MA, Tripathi S, Semwal J, Marzo RR, et al. Artificial intelligence enabled healthcare: A hype, hope or harm. J Family Med Prim Care. 2019;8:3461–4. doi: 10.4103/jfmpc.jfmpc_155_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahzad U. Prediction of probabilistic transient stability using support vector regression. Aust J Electr Electron Eng. 2023;20:35–49. [Google Scholar]
- 15.Seidberg BH, Alibrandi BV, Fine H, Logue B. Clinical investigation of measuring working lengths of root canals with an electronic device and with digital-tactile sense. J Am Dent Assoc. 1975;90:379–87. doi: 10.14219/jada.archive.1975.0059. [DOI] [PubMed] [Google Scholar]
- 16.Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc Neurol. 2017;2:230–43. doi: 10.1136/svn-2017-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marwaha J. Artificial intelligence in conservative dentistry and endodontics: A game-changer. J Conserv Dent Endod. 2023;26:514–8. doi: 10.4103/JCDE.JCDE_7_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kröner PT, Engels MM, Glicksberg BS, Johnson KW, Mzaik O, van Hooft JE, et al. Artificial intelligence in gastroenterology: A state-of-the-art review. World J Gastroenterol. 2021;27:6794–824. doi: 10.3748/wjg.v27.i40.6794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johari M, Esmaeili F, Andalib A, Garjani S, Saberkari H. Detection of vertical root fractures in intact and endodontically treated premolar teeth by designing a probabilistic neural network: An ex vivo study. Dentomaxillofac Radiol. 2017;46:20160107. doi: 10.1259/dmfr.20160107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen HY, Ge P, Liu JY, Qu JL, Bao F, Xu CM, et al. Artificial intelligence: Emerging player in the diagnosis and treatment of digestive disease. World J Gastroenterol. 2022;28:2152–62. doi: 10.3748/wjg.v28.i20.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fahim S, Maqsood A, Das G, Ahmed N, Saquib S, Lal A, et al. Augmented reality and virtual reality in dentistry: Highlights from the current research. Appl Sci. 2022;12:3719. [Google Scholar]
- 22.Chen YW, Stanley K, Att W. Artificial intelligence in dentistry: Current applications and future perspectives. Quintessence Int. 2020;51:248–57. doi: 10.3290/j.qi.a43952. [DOI] [PubMed] [Google Scholar]
- 23.Vodanović M, Subašić M, Milošević D, SavićPavičin I. Artificial intelligence in medicine and dentistry. Acta Stomatol Croat. 2023;57:70–84. doi: 10.15644/asc57/1/8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Putra RH, Doi C, Yoda N, Astuti ER, Sasaki K. Current applications and development of artificial intelligence for digital dental radiography. Dentomaxillofac Radiol. 2022;51:20210197. doi: 10.1259/dmfr.20210197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saghiri MA, Garcia-Godoy F, Gutmann JL, Lotfi M, Asgar K. The reliability of artificial neural network in locating minor apical foramen: A cadaver study. J Endod. 2012;38:1130–4. doi: 10.1016/j.joen.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Saghiri MA, Asgar K, Boukani KK, Lotfi M, Aghili H, Delvarani A, et al. A new approach for locating the minor apical foramen using an artificial neural network. Int Endod J. 2012;45:257–65. doi: 10.1111/j.1365-2591.2011.01970.x. [DOI] [PubMed] [Google Scholar]
- 27.Noorbakhsh-Sabet N, Zand R, Zhang Y, Abedi V. Artificial intelligence transforms the future of health care. Am J Med. 2019;132:795–801. doi: 10.1016/j.amjmed.2019.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Handelman GS, Kok HK, Chandra RV, Razavi AH, Lee MJ, Asadi H. EDoctor: Machine learning and the future of medicine. J Intern Med. 2018;284:603–19. doi: 10.1111/joim.12822. [DOI] [PubMed] [Google Scholar]
- 29.Bhatt P, Liu J, Gong Y, Wang J, Guo Y. Emerging artificial intelligence-empowered mhealth: Scoping review. JMIR Mhealth Uhealth. 2022;10:e35053. doi: 10.2196/35053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou LQ, Wang JY, Yu SY, Wu GG, Wei Q, Deng YB, et al. Artificial intelligence in medical imaging of the liver. World J Gastroenterol. 2019;25:672–82. doi: 10.3748/wjg.v25.i6.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zinchenko V, Chetverikov S, Akhmad E, Arzamasov K, Vladzymyrskyy A, Andreychenko A, et al. Changes in software as a medical device based on artificial intelligence technologies. Int J Comput Assist Radiol Surg. 2022;17:1969–77. doi: 10.1007/s11548-022-02669-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdalla-Aslan R, Yeshua T, Kabla D, Leichter I, Nadler C. An artificial intelligence system using machine-learning for automatic detection and classification of dental restorations in panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130:593–602. doi: 10.1016/j.oooo.2020.05.012. [DOI] [PubMed] [Google Scholar]
- 33.Hiraiwa T, Ariji Y, Fukuda M, Kise Y, Nakata K, Katsumata A, et al. A deep-learning artificial intelligence system for assessment of root morphology of the mandibular first molar on panoramic radiography. Dentomaxillofac Radiol. 2019;48:20180218. doi: 10.1259/dmfr.20180218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fukuda M, Inamoto K, Shibata N, Ariji Y, Yanashita Y, Kutsuna S, et al. Evaluation of an artificial intelligence system for detecting vertical root fracture on panoramic radiography. Oral Radiol. 2020;36:337–43. doi: 10.1007/s11282-019-00409-x. [DOI] [PubMed] [Google Scholar]
- 35.Mitsala A, Tsalikidis C, Pitiakoudis M, Simopoulos C, Tsaroucha AK. Artificial intelligence in colorectal cancer screening, diagnosis and treatment. A new era. Curr Oncol. 2021;28:1581–607. doi: 10.3390/curroncol28030149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bindal P, Bindal U, Lin CW, Kasim NH, Ramasamy TS, Dabbagh A, et al. Neuro-fuzzy method for predicting the viability of stem cells treated at different time-concentration conditions. Technol Health Care. 2017;25:1041–51. doi: 10.3233/THC-170922. [DOI] [PubMed] [Google Scholar]
- 37.Wang CW, Huang CT, Lee JH, Li CH, Chang SW, Siao MJ, et al. Abenchmark for comparison of dental radiography analysis algorithms. Med Image Anal. 2016;31:63–76. doi: 10.1016/j.media.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Shah H, Hernandez P, Budin F, Chittajallu D, Vimort JB, Walters R, et al. Automatic quantification framework to detect cracks in teeth. Proc SPIE Int Soc Opt Eng. 2018;10578:105781K. doi: 10.1117/12.2293603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guo K, Yang Z, Yu CH, Buehler MJ. Artificial intelligence and machine learning in design of mechanical materials. Mater Horiz. 2021;8:1153–72. doi: 10.1039/d0mh01451f. [DOI] [PubMed] [Google Scholar]
- 40.Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial intelligence in surgery: Promises and perils. Ann Surg. 2018;268:70–6. doi: 10.1097/SLA.0000000000002693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fontenele RC, Gerhardt MD, Pinto JC, Van Gerven A, Willems H, Jacobs R, et al. Influence of dental fillings and tooth type on the performance of a novel artificial intelligence-driven tool for automatic tooth segmentation on CBCT images – A validation study. J Dent. 2022;119:104069. doi: 10.1016/j.jdent.2022.104069. [DOI] [PubMed] [Google Scholar]
- 42.Vodanović M, Subašić M, Milošević DP, Galić I, Brkić H. Artificial intelligence in forensic medicine and forensic dentistry. J Forensic Odontostomatol. 2023;41:30–41. [PMC free article] [PubMed] [Google Scholar]


