INTRODUCTION
Persons living with cognitive impairment (PLWCI) utilize the ED more often than cognitively intact older adults and are more vulnerable to a decline in health status following emergency department (ED) care.1,2 Caregivers of PLWCI face substantial challenges preceding, during, and after ED care, as caregivers are often responsible for managing acute healthcare needs and providing greater assistance with activities of daily living when cognitive impairment (CI) is present.3 Surges in ED utilization in the months preceding a diagnosis of dementia further suggests caregiver demands may vary by the degree of CI and proximity of an established diagnosis.4
However, little is known regarding the extent of care provided to PLWCI seeking acute care, including those with diagnosed dementia and undiagnosed CI. Our objective was to quantify the daily care hours that informal caregivers provide to patients with diagnosed dementia, undiagnosed CI, and intact cognition. These insights may establish a benchmark for the amount of care provided to persons with varying cognitive status, inform disposition planning for clinicians, and support policymakers seeking to develop novel solutions addressing caregiver burden.
METHODS
We conducted a cross-sectional analysis of caregivers of community-dwelling, English-speaking older adults (65+ years of age) seeking emergency care across four urban EDs within a single healthcare system from 2021 to 2023. Collectively, the four EDs encountered an average of 280,000 visits annually. All EDs received initial Geriatric ED accreditation between April and August 2022 and had varied site-specific access to ancillary support services as well as physician and nurse champions, but none had fellowship-trained geriatric EM physicians. Research assistants (RA) identified a single caregiver for each patient by asking them to identify “an individual who provided any level of care to manage the patient’s health.” Patients without a diagnosis of dementia in the electronic medical record were screened for the presence of undiagnosed CI using the ED-validated caregiver-administered Ascertain Dementia 8 (cAD8), with scores of 2+ indicating CI.5,6 Before the study began, RAs completed initial training in administering the cAD8, followed by observation from study investigators to ensure proficiency. We categorized patients into three groups: diagnosed dementia, undiagnosed CI (cAD8 ≥ 2), and intact cognition (cAD8 < 2).
The primary outcome was the mean self-reported hours of care provided daily by a caregiver preceding the ED visit in response to the question “how many hours of care do you provide to the patient each day?” We used the Mann–Whitney U test to assess for intergroup differences.
RESULTS
Our analytic sample of 453 dyads consisted of 63 patients with diagnosed dementia, 78 with undiagnosed CI, and 312 had intact cognition. Among caregivers of patients with diagnosed dementia and undiagnosed CI, the majority of caregivers were female (76.8%), white (69.3%), and with a mean age 59.2 years.
Mean hours of care per day were significantly greater for caregivers of older adults with diagnosed dementia (13.8 h, p < 0.0001) and undiagnosed CI (9.5 h, p < 0.0001) compared with those with intact cognition (1.7 h) (Figure 1). The majority of older adults with diagnosed dementia (82.5%) resided with their caregiver, whereas most older adults with undiagnosed CI (69.2%) and intact cognition lived independently (86.9%).
FIGURE 1.
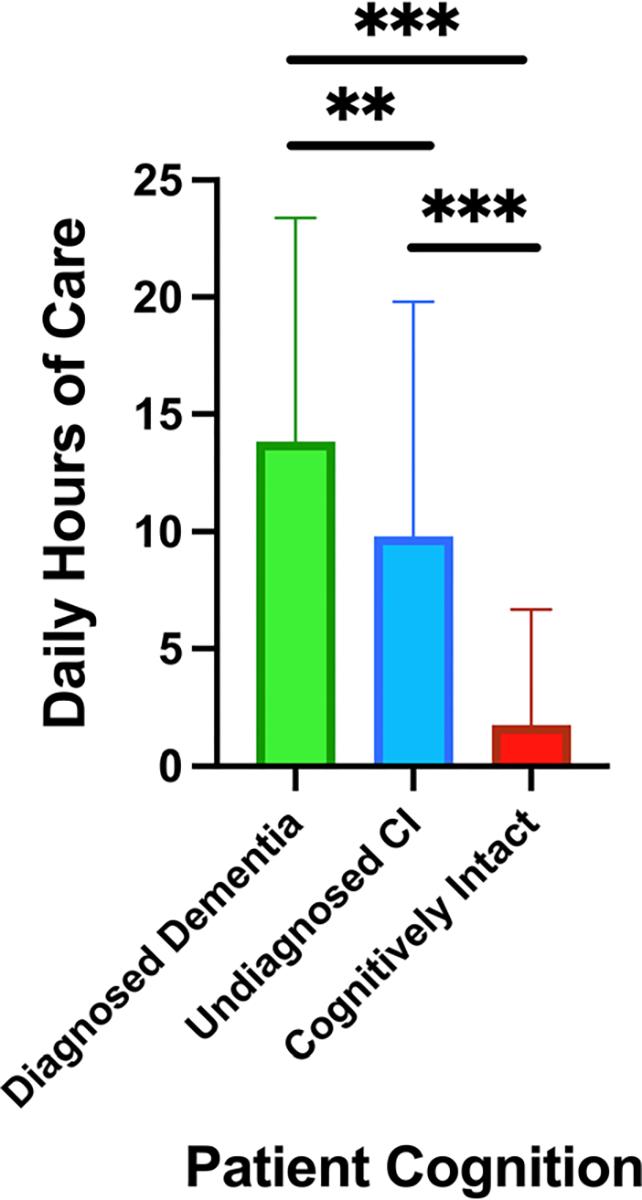
Mean daily hours of care provided by caregivers. CI, cognitive impairment. The significance is reported at the following levels: *p < 0.05; **p < 0.01; ***p < 0.001.
DISCUSSION
Older adults with undiagnosed CI seeking emergency care primarily lived independently, yet received more than five times the amount of daily care from informal caregivers compared with patients with intact cognition. These benchmarking data represent the first quantification of reported support hours provided to older adults seeking acute care and illustrate the significant burden of caregiving in the context of CI. The heightened daily care hours among older adults with undiagnosed CI suggests older adults undergoing cognitive changes may have substantial caregiving needs, nearly mimicking those diagnosed with dementia.
These findings underscore the importance of cognitive screening in the ED and outpatient testing for earlier detection.7 Prior studies have estimated that up to 40% of older ED patients have some form of CI, and more than half of those with dementia lack a formal diagnosis.8,9 Therefore, despite its frequent presentation among older ED patients, dementia often goes unrecognized.1,2,8,9 Concerns regarding the lack of resources to adequately address incident CI may deter EM clinicians from performing cognitive screening assessments, which may be further driven by over-crowded volumes, urgent demands, and pressures to mitigate extended wait times.9,10 Without a diagnosis, patients and caregivers face challenges in qualifying for support services and obtaining referrals from clinicians to receive adequate care, which may worsen their outcomes, including ED utilization.10 Indeed, caregivers of PLWCI (both diagnosed and undiagnosed dementia) have expressed a greater desire for EM clinicians to provide further care coordination and referral facilitation.3 To meet these needs, we suggest that once a screening test positively identifies a person with incident CI, ED clinicians discharging these patients should strongly consider involving family or caregivers in discharge planning and creating partnerships with community resources like memory clinics and home health services. Ensuring clear documentation in electronic health records and discharge paperwork is also essential to promote ambulatory care follow-up and further diagnostic testing.
Our work includes several potential limitations. First, we were unable to conduct a gold standard cognitive assessment to test for the presence of dementia in ED patients. Furthermore, our study assessed daily care needs reported by a single caregiver only present in the ED, potentially overlooking multiple caregivers that offer extensive amounts of care to the older adult. The majority of caregivers were white and recruited from four EDs within a single healthcare system; it is therefore unknown whether our findings extend to other demographic groups and geographic locations. Additionally, the enrollment period occurred during the COVID-19 pandemic, which may have led to higher reported caregiver hours among respondents. Lastly, our results were not adjusted for potential confounders.
In summary, caregivers of older adults with cognitive impairment, whether diagnosed or undiagnosed, provide substantially more hours of care compared with caregivers of older adults with intact cognition. Recognizing cognitive impairment remains pivotal to address challenges experienced by caregivers and an opportunity to provide adequate resource allocation.
Funding information
Doris Duke Charitable Foundation, Grant/Award Number: 2021266; National Institute on Aging, Grant/Award Numbers: P30AG021342, P30AG072931, R01AG079097, R03AG073988, R03AG074038, R33AG058926, R33AG069822, U54AG063546; Emergency Medicine Foundation; Alzheimer’s Association; Yale Center for Clinical Investigation; Dolby Family Ventures; Fridolin Charitable Trust; John A. Hartford Foundation
SPONSOR’S ROLE
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
Footnotes
CONFLICT OF INTEREST STATEMENT
All other authors declare no conflicts of interest that are relevant to this study.
FINANCIAL DISCLOSURE
Dr. Gettel is a Pepper Scholar from the Claude D. Pepper Older Americans Independence Center at the Yale School of Medicine and received support from the National Institute on Aging (NIA) of the National Institutes of Health (NIH; R03AG073988, R33AG058926, P30AG021342, and U54AG063546), the Emergency Medicine Foundation, the Alzheimer’s Association, the COVID-19 Fund to Retain Clinical Scientists at Yale, sponsored by the Doris Duke Charitable Foundation award # 2021266, and the Yale Center for Clinical Investigation. Dr. Hwang is supported by NIA (R33AG058926 and R33AG069822), and the Dolby Family Ventures, Fridolin Charitable Trust, and John A. Hartford Foundation. Dr. Lam has received support from the National Institute on Aging (NIA R03AG074038). Dr. Leggett is funded by the NIA (P30AG072931 and R01AG079097). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
Disclosure of Meeting Presentations and Preprint Status: This work has been accepted for presentation at the Alzheimer’s Association International Conference 2024. This work has not been published as a preprint.
REFERENCES
- 1.Hirschman KB, Paik HH, Pines JM, McCusker CM, Naylor MD, Hollander JE. Cognitive impairment among older adults in the emergency department. West J Emerg Med. 2011;12(1):56–62. [PMC free article] [PubMed] [Google Scholar]
- 2.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency department use among older adults with dementia. Alzheimer Dis Assoc Disord. 2016;30(1):35–40. doi: 10.1097/WAD.0000000000000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gettel CJ, Serina PT, Uzamere I, et al. Emergency department care transition barriers: a qualitative study of care partners of older adults with cognitive impairment. Alzheimers Dement (NY). 2022;8(1):e12355. doi: 10.1002/trc2.12355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seidenfeld J, Runels T, Goulet JL, et al. Patterns of emergency department visits prior to dementia or cognitive impairment diagnosis: an opportunity for dementia detection? Acad Emerg Med. 2023;7. doi: 10.1111/acem.14832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galvin JE, Roe CM, Powlishta KK, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005;65(4):559–564. doi: 10.1212/01.wnl.0000172958.95282.2a [DOI] [PubMed] [Google Scholar]
- 6.Carpenter CR, Bassett ER, Fischer GM, Shirshekan J, Galvin JE, Morris JC. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s screen, short blessed test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med. 2011;18(4):374–384. doi: 10.1111/j.1553-2712.2011.01040.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nowroozpoor A, Dussetschleger J, Perry W, et al. Detecting cognitive impairment and dementia in the emergency department: a scoping review. J Am Med Dir Assoc. 2022;23(8):1314. e31–1314.e88. doi: 10.1016/j.jamda.2022.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amjad H, Roth DL, Sheehan OC, Lyketsos CG, Wolff JL, Samus QM. Underdiagnosis of dementia: an observational study of patterns in diagnosis and awareness in US older adults. J Gen Intern Med. 2018;33(7):1131–1138. doi: 10.1007/s11606-018-4377-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39(3):248–253. doi: 10.1067/mem.2002.122057 [DOI] [PubMed] [Google Scholar]
- 10.Kent T, Lesser A, Israni J, Hwang U, Carpenter C, Ko KJ. 30-day emergency department revisit rates among older adults with documented dementia. J Am Geriatr Soc. 2019;67(11):2254–2259. doi: 10.1111/jgs.16114 [DOI] [PMC free article] [PubMed] [Google Scholar]


