Abstract
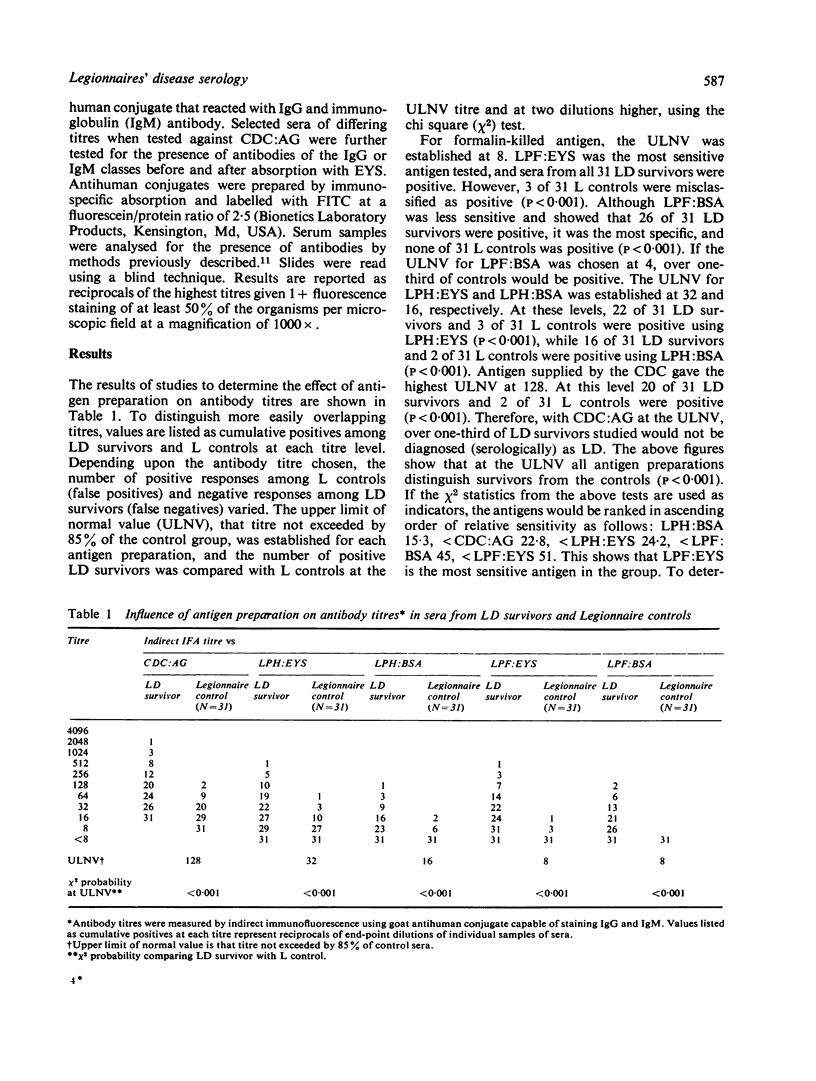
Sera from 31 Legionnaires' disease (LD) survivors of the Philadelphia outbreak, 31 Legionnaire (L) controls, and 300 additional controls were examined for the presence of specific antibodies to five antigen preparations of Legionella pneumophila (serogroup 1) to determine the effect of antigen preparation on the sensitivity and specificity of the indirect immunofluorescence test. Diagnostic levels were determined for each antigen at the upper limit of normal value (ULNV) titre, which established the titre not exceeded by 85% of controls.
Antigens were prepared from formalin-killed L. pneumophila suspended in egg yolk sac (EYS) (LPF:EYS) or bovine serum albumin (BSA) (LPF:BSA); and from heat-killed organisms suspended in EYS (LPH:EYS) or BSA (LPH:BSA). Antigen was also supplied by the Center for Disease Control (CDC:AG).
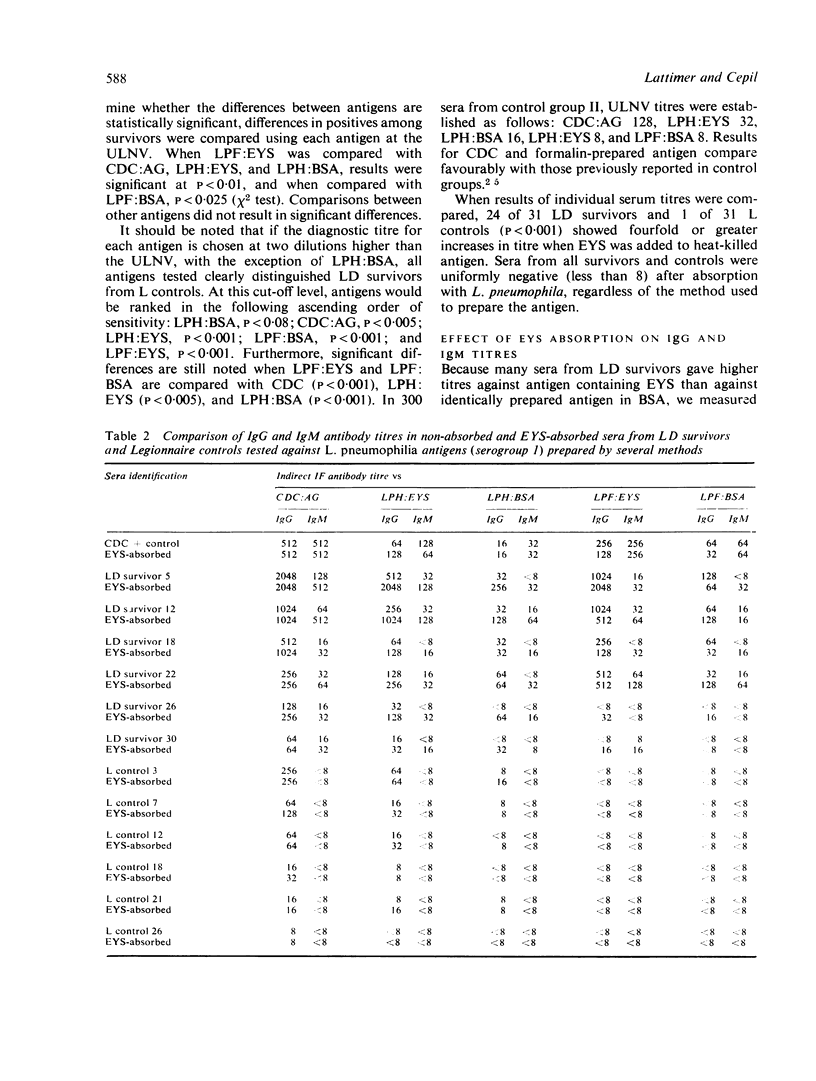
Although there was wide variation in the sensitivity of the antigens, at the ULNV level all antigens tested could be used to differentiate LD survivors from L controls (p<0.001; X2 test). Formalin treatment resulted in the most specific antigen by eliminating titres in L controls. The results of the X2 test, comparing LD survivors with L controls, ranked the antigens in the following ascending order of sensitivity: LPH:BSA 15·3, <CDC:AG 22·8, <LPH:EYS 24·2, <LPF:BSA 45, <LPF:EYS 51. Moreover, when differences in positive results among LD survivors were compared, statistically significant differences were found when LPF:EYS (p<0·01; X2 test) and LPF:BSA (p<0·025; X2 test) were compared with CDC:AG, LPH:EYS, and LPH:BSA antigens. Titres in 300 additional controls paralleled those found in L controls.
It was concluded that formalin treatment of L. pneumophila resulted in a sensitive antigen, which increased the number of positive tests in survivors while decreasing false-positive tests in controls. It should be considered for use in routine testing programmes for diagnosing LD.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beaty H. N., Miller A. A., Broome C. V., Goings S., Phillips C. A. Legionnaires' disease in Vermont, May to October 1977. JAMA. 1978 Jul 14;240(2):127–131. [PubMed] [Google Scholar]
- Brenner D. J., Steigerwalt A. G., McDade J. E. Classification of the Legionnaires' disease bacterium: Legionella pneumophila, genus novum, species nova, of the family Legionellaceae, familia nova. Ann Intern Med. 1979 Apr;90(4):656–658. doi: 10.7326/0003-4819-90-4-656. [DOI] [PubMed] [Google Scholar]
- Cherry W. B., Pittman B., Harris P. P., Hebert G. A., Thomason B. M., Thacker L., Weaver R. E. Detection of Legionnaires disease bacteria by direct immunofluorescent staining. J Clin Microbiol. 1978 Sep;8(3):329–338. doi: 10.1128/jcm.8.3.329-338.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon R. J., Abraham W. H. Scottish experience with the serologic diagnosis of Legionnaires' disease. Ann Intern Med. 1979 Apr;90(4):684–686. doi: 10.7326/0003-4819-90-4-684. [DOI] [PubMed] [Google Scholar]
- Kirby B. D., Snyder K. M., Meyer R. D., Finegold S. M. Legionnaires' disease: clinical features of 24 cases. Ann Intern Med. 1978 Sep;89(3):297–309. doi: 10.7326/0003-4819-89-3-297. [DOI] [PubMed] [Google Scholar]
- Lattimer G. L., Ormsbee R. A., Peacock M. G., Rhodes L. V. Diagnostic specificity of immunoglobulin M (IgM) response in differentiation Legionnaires' disease from psittacosis. Scand J Infect Dis. 1979;11(4):271–273. doi: 10.3109/inf.1979.11.issue-4.03. [DOI] [PubMed] [Google Scholar]
- Lattimer G. L., Rhodes L. V., 3rd, Cepil B. Legionnaires' serotypes. Lancet. 1979 Jan;1(8107):109–109. doi: 10.1016/s0140-6736(79)90103-x. [DOI] [PubMed] [Google Scholar]
- Lattimer G. L., Rhodes L. V., 3rd, Salventi J. S., Galgon J. P., Stonebraker V., Boley S., Haas G. The Philadelphia epidemic of Legionnaire's disease: clinical, pulmonary, and serologic findings two years later. Ann Intern Med. 1979 Apr;90(4):522–526. doi: 10.7326/0003-4819-90-4-522. [DOI] [PubMed] [Google Scholar]
- McDade J. E., Shepard C. C., Fraser D. W., Tsai T. R., Redus M. A., Dowdle W. R. Legionnaires' disease: isolation of a bacterium and demonstration of its role in other respiratory disease. N Engl J Med. 1977 Dec 1;297(22):1197–1203. doi: 10.1056/NEJM197712012972202. [DOI] [PubMed] [Google Scholar]
- Ormsbee R. A., Peacock M. G., Lattimer G. L., Page L. A., Fiset P. Legionnaires' disease: antigenic peculiarities, strain differences, and antibiotic sensitivities of the agent. J Infect Dis. 1978 Aug;138(2):260–264. doi: 10.1093/infdis/138.2.260. [DOI] [PubMed] [Google Scholar]
- Taylor A. G., Harrison T. G., Dighero M. W., Bradstreet C. M. False positive reactions in the indirect fluorescent antibody test for Legionnaires' disease eliminated by use of formolised yolk-sac antigen. Ann Intern Med. 1979 Apr;90(4):686–689. doi: 10.7326/0003-4819-90-4-686. [DOI] [PubMed] [Google Scholar]
- Taylor A. G., Harrison T. G. Legionnaires' disease caused by Legionella pneumophila serogroup 3. Lancet. 1979 Jul 7;2(8132):47–47. doi: 10.1016/s0140-6736(79)90216-2. [DOI] [PubMed] [Google Scholar]
- Tsai T. F., Fraser D. W. The diagnosis of Legionnaires' disease. Ann Intern Med. 1978 Sep;89(3):413–414. doi: 10.7326/0003-4819-89-3-413. [DOI] [PubMed] [Google Scholar]
- Wilkinson H. W., Fikes B. J., Cruce D. D. Indirect immunofluorescence test for serodiagnosis of Legionnaires disease: evidence for serogroup diversity of Legionnaires disease bacterial antigens and for multiple specificity of human antibodies. J Clin Microbiol. 1979 Mar;9(3):379–383. doi: 10.1128/jcm.9.3.379-383.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]


