Abstract
Plantar fasciitis, or plantar heel pain, causes inflammation of the plantar fascia due to various causes, with no clear consensus on the treatment protocol. Standard first-line treatment includes non-steroidal anti-inflammatory drugs and physiotherapy. Second-line treatment prior to surgery includes extracorporeal shockwave therapy (ESWT), ultrasound-guided (USG) therapy, corticosteroid injection (CSI), and platelet-rich plasma (PRP) injection. Recently, the use of acupuncture treatment has been gaining popularity, with increasing published evidence showing its effectiveness in treating plantar fasciitis. The objective of this study was to determine whether acupuncture intervention was a viable alternative treatment method for managing plantar fasciitis when compared to ESWT, USG therapy, CSI, and PRP injection. Data sources from PubMed, Google Scholar, Scopus, Science Direct, and China National Knowledge Infrastructure were reviewed. Clinical trials were searched from their inception over the period of January 2000 to October 2020. A total of 32 relevant papers were included for analysis, totaling 2390 samples. Visual Analog Scale (VAS) scores measuring pain were analyzed in terms of outcome after one and three months of treatment. Each time point was analyzed separately through a network meta-analysis using the frequentist approach. VAS scores for each intervention at baseline and the two-time points (i.e., one and three months) were included in the comprehensive meta-analysis. Then, differences in VAS scores were calculated in R studio (V4.1.2; RStudio: Integrated Development for R, RStudio, Inc., Boston, USA) using the netmeta package. The netmeta package was also used to perform the network meta-analysis and generate corresponding figures. Direct and indirect effects were assessed and visualized through a direct evidence plot and a node-splitting forest plot. Randomized controlled trials (RCTs) and non-RCTs involving treatments of acupuncture, ESWT, USG therapy, CSI, or PRP injection, either in comparison with each other or with a placebo, were included in our review. Our meta-analysis showed that at one month, VAS scores for acupuncture treatment had the highest mean difference (MD) of -1.33 (95% confidence interval (95% CI) = -2.19 to -0.46) compared to placebo, indicating that acupuncture treatment was more effective than other treatment arms when compared to placebo. Analysis at threemonths showed that the highest-ranked treatment was PRP injection, with an MD of -2.67 (95% CI = -6.23 to 0.89). However, the CI for the net effect of all treatments crossed the null effect on the forest plot, indicating no statistically significant difference between the treatment and placebo. Acupuncture treatment should be considered as a second-line treatment for treatment of plantar fasciitis together with other common treatment options such as ESWT, PRP injection, CSI, and USG therapy. Further long-term studies measuring acupuncture treatment outcomes would be beneficial in the future.
Keywords: acupuncture therapy, corticosteroid injection, extracorporeal shockwave therapy, network analysis, plantar fasciitis, plantar heel pain, platelet-rich plasma (prp), recalcitrant plantar fasciitis, ultrasound foot
Introduction and background
Plantar fasciitis, a form of inflammation of the plantar fascia, is a common condition, especially affecting working adults with prolonged standing. Presentation usually involves pain and discomfort over the medial aspect of the inferior heel region. Patients with plantar fasciitis often complain of severe excruciating pain upon weight-bearing after rising from their bed in the early morning, with the pain and discomfort eventually subsiding after taking a certain number of steps.
Diagnosis of plantar fasciitis is made by ruling out other pathologies involving heel pain. This condition is a type of overuse injury that is typically associated with intrinsic and extrinsic factors [1]. Extrinsic factors include environmental factors such as poor biomechanics, hard surface ambulation, prolonged weight-bearing, inadequate stretching, and poor footwear. Intrinsic factors are divided into anatomic and biomechanics factors. Anatomic factors include obesity, pes planus, pes cavus, and a tight Achilles tendon, whereas biomechanical factors include overpronation, weak intrinsic muscles of the foot, and weak plantar flexor muscles.
The presence of calcaneal spurs, osseous prolongations located at the medial process of the plantar calcaneal tuberosity, has been previously suggested as an intrinsic factor contributing to plantar fasciitis. However, the presence of heel spur is not diagnostic of plantar fasciitis. In a study of radiographic images involving 1000 patients, only 5.2% with heel spurs had symptoms of plantar fasciitis [2].
Treatment of plantar fasciitis is divided into non-surgical and surgical management. There is a wide range of non-surgical management options available, including rest and activity modification, various stretching techniques, weight-loss therapy, anti-inflammatory medication with shoe wear modification, night splints, and specific physical therapies [3-5]. Physical therapy may include eccentric stretches and deep myofascial massage. More advanced physiotherapy equipment recently used to enhance tissue healing includes ultrasound-guided (USG) therapy and extracorporeal shock wave therapy (ESWT). The use of injections, such as corticosteroid injection (CSI) or platelet-rich plasma (PRP) injection, has gained popularity in managing plantar fasciitis. These modes of treatment are usually compared to other types of conservative treatment or among themselves. Acupuncture treatment has shown promising results in successfully managing plantar fasciitis when other modes have failed. However, there has not been a direct comparison between acupuncture, USG therapy, ESWT, and prolotherapy.
The concept of acupuncture treatment is different from dry needling, where understanding the cause of heel pain in Traditional Chinese Medicine (TCM) theory is essential in the former. Acupuncture uses a meridian reference with an additional Ashi point or trigger point, whereas dry needling only utilizes trigger points.
The objective of this study was to perform a network meta-analysis comparing five modes of treatment for plantar fasciitis: acupuncture, USG therapy, ESWT, CSI, and PRP injection. In a literature search specifically looking at second-line treatment for plantar fasciitis, the results showed that treatments such as USG therapy, ESWT, and CSI were the most frequently studied and compared in randomized controlled trials (RCTs) [6-22]. There were very few studies comparing these treatments to acupuncture treatment for plantar fasciitis. There was especially no literature that used a network meta-analysis method to compare acupuncture intervention against USG therapy, ESWT, or prolotherapy to manage plantar fasciitis. However, there have been meta-analysis studies comparing USG therapy, ESWT, and prolotherapy with dry needling [8,23-25]. This study is the first network meta-analysis using specific direct and indirect methods to compare these interventions. To strengthen the statistical power of the analysis, non-randomized prospective studies were included.
Review
Materials and methods
Study Eligibility Criteria
Types of patients: This study included adult patients who were ≥18 years of age and diagnosed clinically by a physician to have plantar fasciitis. Studies not clearly stating the diagnosis of plantar fasciitis or related to plantar fasciitis as a diagnosis were not included.
Types of studies: The meta-analysis included RCTs and non-randomized prospective studies. Case reports, case series, reviews, and retrospective studies were excluded.
Types of intervention: The meta-analysis included studies comparing interventions that consisted of acupuncture, USG therapy, ESWT, CSI, and PRP injection as part of treatment. Electro-acupuncture was included, as it falls under acupuncture with tonifying effect.
Primary outcome: Studies were included if their primary outcome measure was the Visual Analog Scale (VAS) score used to indicate pain. In this study, VAS scores were adjusted to a centimeter scale ranging from 0 to 10 cm, where 0 represented painless status, and 10 represented unbearable pain. Short-term outcomes were measured at the one-month and three-month marks. We did not include secondary outcomes because they can vary significantly between studies in terms of definition, measurement methods, and reporting. This variability can introduce additional heterogeneity, complicate the synthesis of results, and potentially reduce the reliability of the findings.
Information Sources and Search Strategy
PubMed, Science Direct, Scopus, Google Scholar, and China National Knowledge Infrastructure (CKNI) database were searched with an established method for randomized and non-randomized trials with similar end results for USG therapy, ESWT, CSI, PRP injection, and acupuncture intervention. The search terminologies included “plantar fasciitis,” “plantar fasciopathy,” “plantar fasciosis,” “plantar heel pain (PHP),” and “acupuncture” or “electro-acupuncture” or “ultrasound” or “USG” or “extracorporeal shock wave therapy” or “ESWT” or “corticosteroid” or “steroid injection” or “platelet rich plasma” or “PRP” and “randomized controlled trial” or “RCT” or “controlled clinical trial” or “non-randomized controlled trial.” The bibliographies of relevant review articles and selected articles were examined for additional potentially relevant trials.
Study Selection
All duplicated literature was removed manually. Titles and abstracts were reviewed by two authors (IA and BV) independently. Studies that did not meet the eligibility criteria were removed. The full texts of the remaining studies were then reviewed by the two authors independently. Studies meeting eligibility were included after this process. If there was disagreement between the two authors regarding any study, it was then reviewed by another author (CS). No automation tools were used.
Data Extraction
Both the above-mentioned authors (IA and BV) independently extracted the following data from eligible studies: first author, year of publication, area, study duration, sample size, age, percentage of gender difference, inclusion/exclusion criteria, detailed intervention in each group, number of patients in each group, follow-up time, and outcomes in each group. If required data were unavailable for a study, its authors were contacted directly.
Study Risk of Bias Assessment
Two authors (IA and BV) independently assessed the risk of bias for the selected studies by using the ROBINS-I (Risk Of Bias In Non-randomised Studies - of Interventions) bias assessment tool (Table 1) [26]. This assessment was further verified and confirmed by the supervising author (CS).
Table 1. ROBINS-I bias assessment tool.
ROBINS-I: Risk Of Bias In Non-randomised Studies - of Interventions
| Bias Due to Confounding | Bias in the Selection of Participants in the Study | Bias Due to Classification of Interventions | Bias Due to Deviations From Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result | Overall risk of Bias | User Notes | Title |
| Low | Moderate | Moderate | Low | Low | Low | Low | Low | - | Akinoglu et al., 2017 [7] |
| Moderate | Low | Low | Low | Low | Low | Low | Low | - | Xu et al., 2020 [20] |
| Moderate | Low | Moderate | Moderate | Low | Low | Low | Low | - | Ho et al., 2021 [23] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Abdihakin et al., 2012 [27] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Acosta-Olivo et al., 2017 [28] |
| Moderate | Serious | Moderate | Serious | Low | Moderate | Moderate | Moderate | - | Ashahin et al., 2012 [29] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Buchbinder et al., 2002 [30] |
| Moderate | Low | Low | Low | Low | Low | Low | Low | - | Eslamian et al., 2016 [31] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Gerdesmeyer et al., 2008 [32] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Haake et al., 2003 [33] |
| Low | Low | Moderate | Low | Low | Low | Low | Low | - | Hammer et al., 2003 [34] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Ibrahim et al., 2010 [35] |
| Moderate | Low | Low | Low | Moderate | Low | Low | Low | - | Jain et al., 2015 [36] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Karagounis et al., 2011 [37] |
| Moderate | Low | Low | Low | Low | Low | Low | Low | - | Konjen et al., 2015 [38] |
| Moderate | Moderate | Low | Low | Low | Low | Low | Low | - | Krukowska et al., 2016 [39] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Kudo et al., 2006 [40] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Kumnerddee et al., 2012 [41] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Lai et al., 2018 [42] |
| Moderate | Moderate | Moderate | Moderate | Moderate | Low | Low | Moderate | - | Mahindra et al., 2016 [43] |
| Moderate | Low | Low | Low | Low | Low | Low | Low | - | Mardani-Kivi et al., 2015 [44] |
| Low | Low | Low | Low | Moderate | Low | Low | Low | - | Marks et al., 2008 [45] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Omar et al., 2012 [46] |
| Moderate | Moderate | Moderate | Moderate | Low | Low | Low | Moderate | - | Sahoo et al., 2020 [47] |
| Moderate | Moderate | Moderate | Moderate | Low | Low | Low | Moderate | - | Say et al., 2014 [48] |
| Moderate | Moderate | Moderate | Moderate | Low | Low | Low | Moderate|||Low | - | Speed et al., 2003 [49] |
| Moderate | Serious | Moderate | Low | Low | Low | Low | Moderate | - | Tabrizi et al., 2020 [50] |
| Low | Low | Low | Low | Low | Low | Low | Low | - | Theodore et al., 2004 [51] |
| Low | Low | Low | Low | Moderate | Low | Low | Low | - | Tiwari and Bhargava, 2013 [52] |
| Moderate | Serious | Moderate | Moderate | Moderate | Low | Low | Moderate | - | Wang et al., 2012 [53] |
| Moderate | - | Moderate | Moderate | Low | Low | Low | Moderate | - | Yucel et al., 2010 [54] |
| Low | Low | Moderate | Low | Low | Low | Low | Low | - | Yucel et al., 2013 [55] |
Statistical Analysis
Network meta-analysis using the frequentist approach was used to compare the direct and indirect effects of different treatment arms on VAS scores. The efficacy of the interventions was assessed by analyzing the change in VAS score from baseline and two-time points: one and three months. Each time point was analyzed separately through a network meta-analysis using the frequentist approach. The data were extracted and cleaned in an Excel file (Microsoft® Corp., Redmond, USA), and the mean difference (MD) between the baseline and the two-time points of each intervention was calculated using a comprehensive meta-analysis. Then, changes in the MDs of the VAS score were calculated in R studio (V4.1.2; RStudio: Integrated Development for R, RStudio, Inc., Boston, USA) using the netmeta package. The netmeta package also was used to perform the network meta-analysis and generate corresponding figures. Direct and indirect effects were assessed and visualized through a direct evidence plot and a node-splitting forest plot. Additionally, a net heat plot was used to assess heterogeneity by comparing both fixed and random effects. After the validity of the network was assessed, a forest plot of the network was used to show the rank and net effect of each intervention in comparison to placebo, and a network graph showed the connections between treatments and a number of studies for each comparison. Moreover, a table containing a matrix of all possible comparisons was produced to check the estimates of each comparison.
Risk of Bias Assessment
Publication bias was assessed using a comparison-adjusted funnel plot. The p-values were calculated with Egger's test, and the publication bias was considered significant when p < 0.05.
Results
Literature Search and Study Selection Results
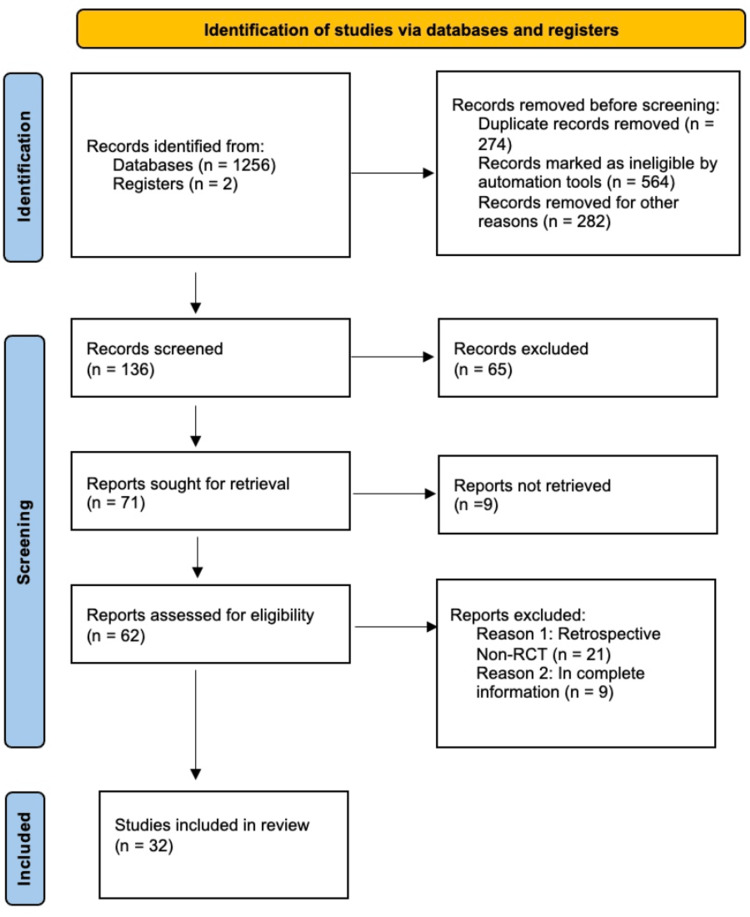
A total of 1258 studies were initially searched from PubMed, Scopus, Google Scholar, Science Direct, CKNI, and an additional search from other resources. Out of 1258 studies, 136 studies were screened; others were eliminated initially due to being duplicate studies, systemic reviews, or not meeting the inclusion criteria. Finally, a total of 32 suitable studies were selected for analysis, with a total of 2390 samples from the selected studies. Figure 1 shows a flow diagram of the literature search as recommended in Preferred Reporting Items for Systematic Reviews and Meta-Analyses [26].
Figure 1. PRISMA flow chart of the study process.
PRISMA: Preferred Reporting Items for Systemic review and Meta-Analyses; RCT: Randomized controlled trial
Characteristics of the Studies
Characteristics of the studies included in the meta-analysis are shown in Table 2. After the elimination of studies from the search due to eligibility criteria and duplications, we included 32 studies with 2390 samples [7,22,23,27-55]. Out of the 32 studies, one study had three interventions and a placebo, whereas the remaining studies had two interventions. Fifteen studies had placebo comparisons. Among the 32 studies, 16 were double-blinded, five were single-blinded, two were open-label, and the remaining nine trials did not mention their blinding method. Out of the 2390 total samples analyzed, 714 were placebo, 840 were EWST, 473 were CSI, 216 were PRP injection, 94 were acupuncture, and 53 were USG therapy.
Table 2. Characteristics of studies.
ACU: Acupuncture; USG: Ultrasound; ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CS: Corticosteroid injection; T1: Treatment 1; T2: Treatment 2; T3: Treatment 3; NA: Not available; BMI: Body mass index
| S. No. | Author, Year | Blinding | Follow-up (months) | T1 | Cases | Male/Female | Age (years) | BMI (kg/m²) | T2 | Cases | Male/Female | Age (years) | BMI (kg/m²) | T3 | Cases | Male/Female | Age (years) | BMI (kg/m²) |
| 1 | Akinoglu et al., 2017 [7] | Single | 1 | ESWT | 18 | NA | 50.0 | 28.6 | USG | 18 | NA | 50.1 | 28.5 | - | - | - | - | - |
| 2 | Xu et al., 2020 [22] | NA | 6 | ESWT | 49 | 13/37 | 48.5 | 23.7 | CS | 47 | 19/31 | 47.2 | 23.1 | - | - | - | - | - |
| 3 | Ho et al., 2021 [23] | NA | 2 | ACU | 40 | 6/34 | 59.4 | 23.7 | PL | 40 | 6/34 | 60.0 | 57.7 | - | - | - | - | - |
| 4 | Abdihakin et al., 2012 [27] | Double | 2 | CS | 47 | 23/24 | 41.0 | 31.7 | PL | 41 | 19/22 | 45.1 | 31.7 | - | - | - | - | - |
| 5 | Acosta-Olivo et al., 2017 [28] | Double | 4 | CS | 14 | NA | 44.8 | NA | PRP | 14 | NA | 44.8 | NA | - | - | - | - | - |
| 6 | Ashahin et al., 2012 [29] | NA | 6 | CS | 30 | 12/18 | 46.4 | 32.77 | PRP | 30 | 13/17 | 45.7 | 29.6 | - | - | - | - | - |
| 7 | Buchbinder et al., 2002 [30] | Double | 3 | ESWT | 80 | 34/46 | 52.2 | 29.4 | PL | 81 | 33/47 | 54.2 | 28.7 | - | - | - | - | - |
| 8 | Eslamian et al., 2016 [31] | Single | 2 | ESWT | 20 | 2/18 | 41.5 | NA | CS | 20 | 5/15 | 42.9 | NA | - | - | - | - | - |
| 9 | Gerdesmeyer et al., 2008 [32] | Double | 12 | ESWT | 125 | NA | 52.4 | 27.2 | PL | 118 | NA | 52.0 | 28.0 | - | - | - | - | - |
| 10 | Haake et al., 2003 [33] | Double | 12 | ESWT | 127 | 37/98 | 53.1 | 29.4 | PL | 129 | 30/106 | 52.9 | 29.7 | - | - | - | - | - |
| 11 | Hammer et al., 2003 [34] | NA | 24 | ESWT | 25 | 5/19 | 51 | 29.6 | PL | 24 | 10/13 | 48 | 28.7 | - | - | - | - | - |
| 12 | Ibrahim et al., 2010 [35] | Double | 6 | ESWT | 25 | 7/18 | 56.6 | NA | PL | 25 | 11/14 | 49.1 | NA | - | - | - | - | - |
| 13 | Jain et al., 2015 [36] | NA | 12 | PRP | 23 | 16/30 | 55.6 | NA | CS | 23 | 6/28 | 44.7 | 29.1 | - | - | - | - | - |
| 14 | Karagounis et al., 2011 [37] | Single | 2 | ACU | 19 | NA | 36.8 | 23.21 | PL | 19 | NA | 36.8 | 23.74 | - | - | - | - | - |
| 15 | Konjen et al., 2015 [38] | Double | 6 | US | 15 | 2/13 | 45 | 26.67 | ESWT | 15 | 4/11 | 45.6 | 26.03 | - | - | - | - | - |
| 16 | Krukowska et al., 2016 [39] | Open Label | 0.5 | USG | 20 | 20/13 | 51.1 | NA | ESWT | 27 | 4/11 | 51.4 | NA | - | - | - | - | - |
| 17 | Kudo et al., 2006 [40] | Double | 3 | ESWT | 53 | 18/40 | 51.1 | NA | PL | 52 | 23/33 | 48.8 | NA | - | - | - | - | - |
| 18 | Kumnerddee et al., 2012 [41] | Open Label | 1.5 | ACU | 15 | 3/12 | 52.4 | 25.2 | PL | 15 | 0/15 | 53.8 | 25.3 | - | - | - | - | - |
| 19 | Lai et al., 2018 [42] | NA | 3 | ESWT | 47 | 21/26 | 54.53 | NA | CS | 50 | 22/28 | 54.58 | NA | - | - | - | - | - |
| 20 | Mahindra et al., 2016 [43] | Double | 3 | PRP | 25 | 8/17 | 30.7 | NA | CS | 25 | 12/13 | 33.9 | NA | PL | 25 | 11/14 | 35.48 | NA |
| 21 | Mardani-Kivi et al., 2015 [44] | Double | 3 | ESWT | 43 | 5/29 | 43.9 | 30.2 | CS | 41 | 6/28 | 44.7 | 29.1 | - | - | - | - | - |
| 22 | Marks et al., 2008 [45] | Double | 6 | ESWT | 16 | 7/9 | 52 | NA | PL | 9 | 4/5 | 51.9 | NA | - | - | - | - | - |
| 23 | Omar et al., 2012 [46] | Double | 3 | PRP | 15 | 0/15 | 42.5 | NA | CS | 15 | 0/15 | 44.5 | NA | - | - | - | - | - |
| 24 | Sahoo et al., 2020 [47] | NA | 6 | PRP | 39 | 14/25 | 39.4 | NA | CS | 38 | 17/17 | 38.3 | NA | - | - | - | - | |
| 25 | Say et al., 2014 [48] | NA | 6 | CS | 25 | 5/20 | 47 | NA | PRP | 25 | 6/19 | 48.6 | NA | - | - | - | - | |
| 26 | Speed et al., 2003 [49] | Double | 6 | ESWT | 46 | 20/26 | 51.7 | NA | PL | 42 | 17/25 | 52.5 | NA | - | - | - | - | |
| 27 | Tabrizi et al., 2020 [50] | Single | 24 | CS | 16 | 1/15 | 31.7 | 32.4 | PRP | 15 | 1/14 | 33.6 | 33.9 | - | - | - | - | |
| 28 | Theodore et al., 2004 [51] | Double | 12 | ESWT | 76 | 14/62 | 50 | NA | PL | 74 | 24/47 | 53 | NA | - | - | - | - | |
| 29 | Tiwari and Bhargava, 2013 [52] | Double | 6 | PRP | 30 | NA | NA | NA | CS | 30 | NA | NA | NA | - | - | - | - | |
| 30 | Wang et al., 2012 [53] | NA | NA | ACU | 20 | 10/10 | 47.0 | NA | ESWT | 20 | 0/20 | 40.5 | NA | - | - | - | - | |
| 31 | Yucel et al., 2010 [54] | Single | 1 | CS | 20 | 4/16 | 45.6 | 30.8 | PL | 20 | 4/16 | 47.4 | 29.3 | - | - | - | - | |
| 32 | Yucel et al., 2013 [55] | Double | 3 | CS | 33 | 5/28 | 44.7 | NA | ESWT | 28 | 13/14 | 42.9 | NA | - | - | - | - |
Change in VAS Score After One Month
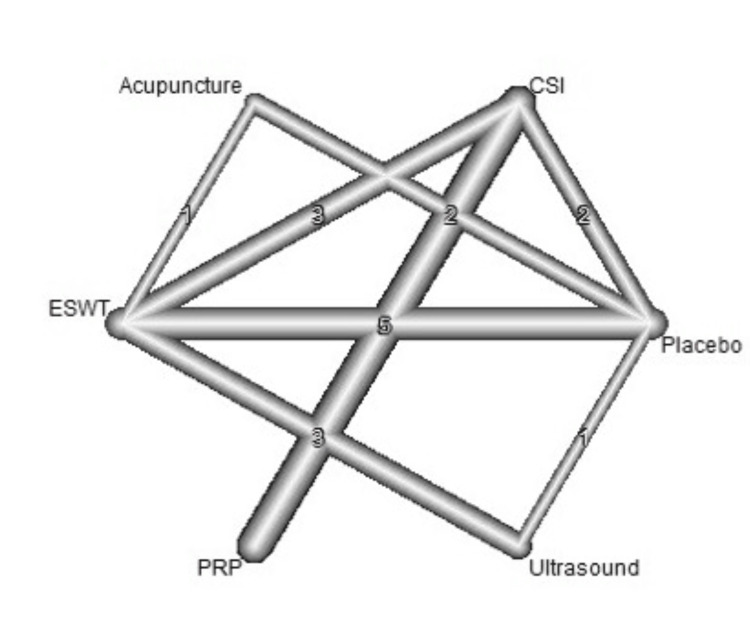
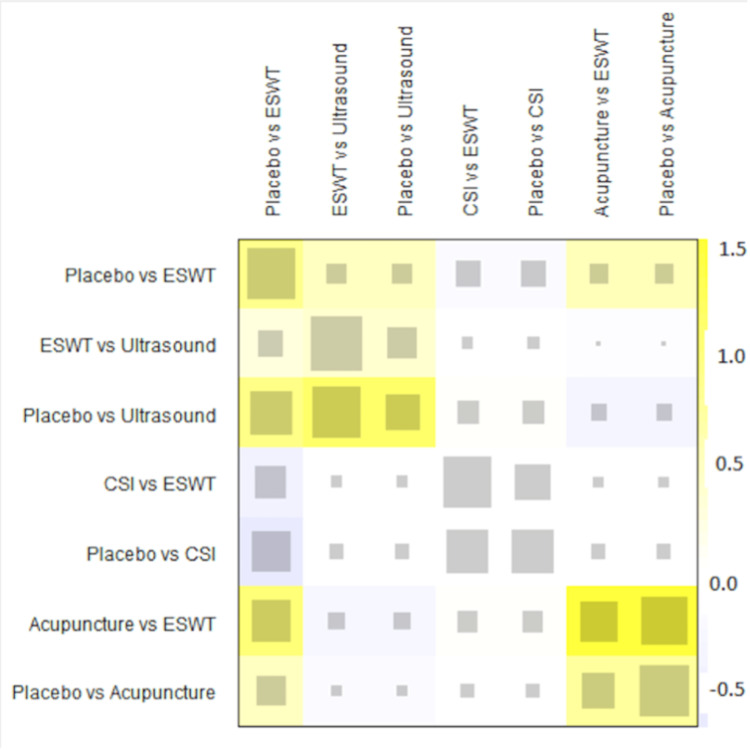
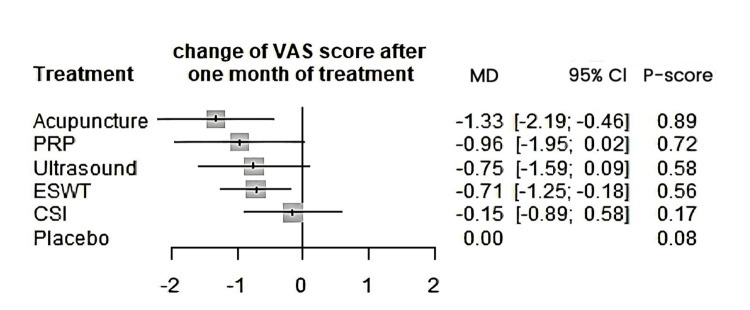
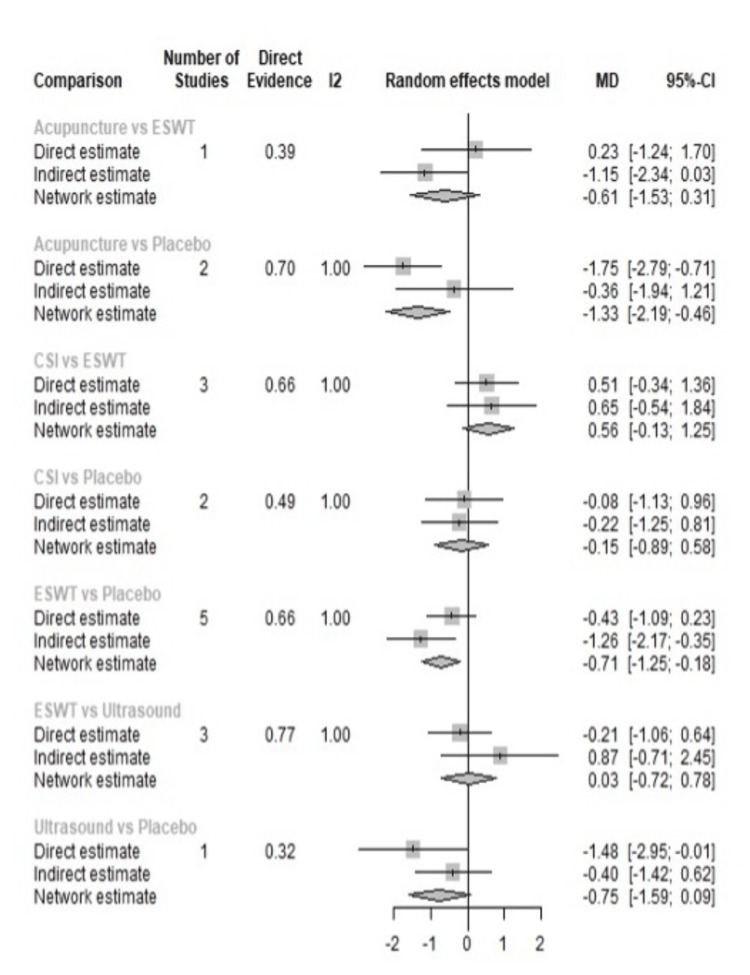
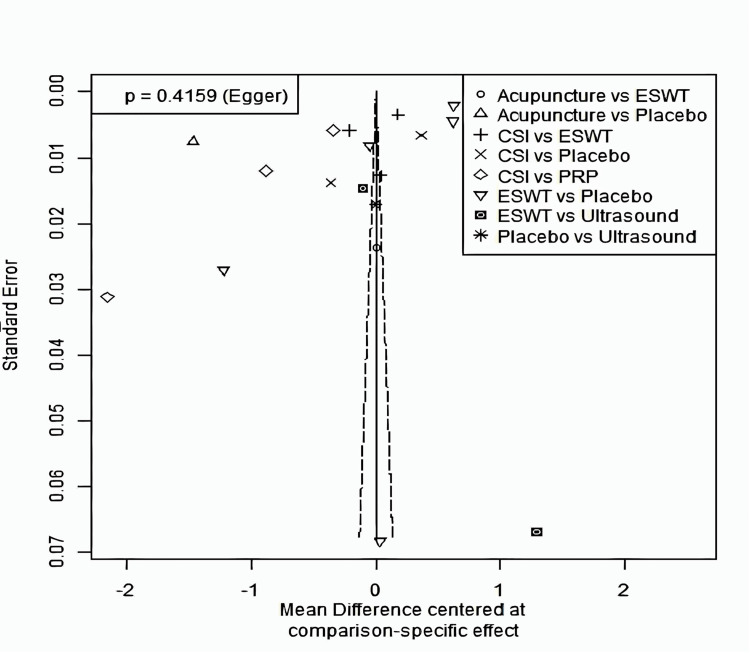
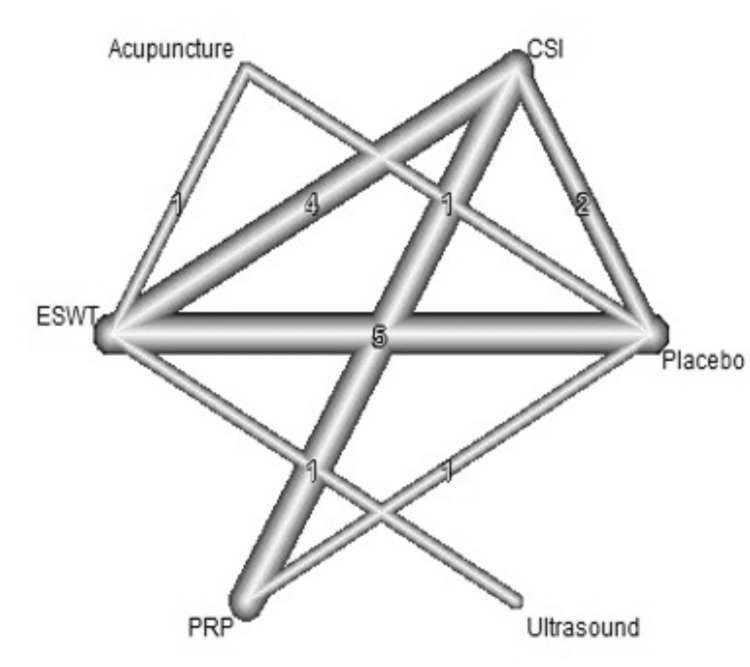
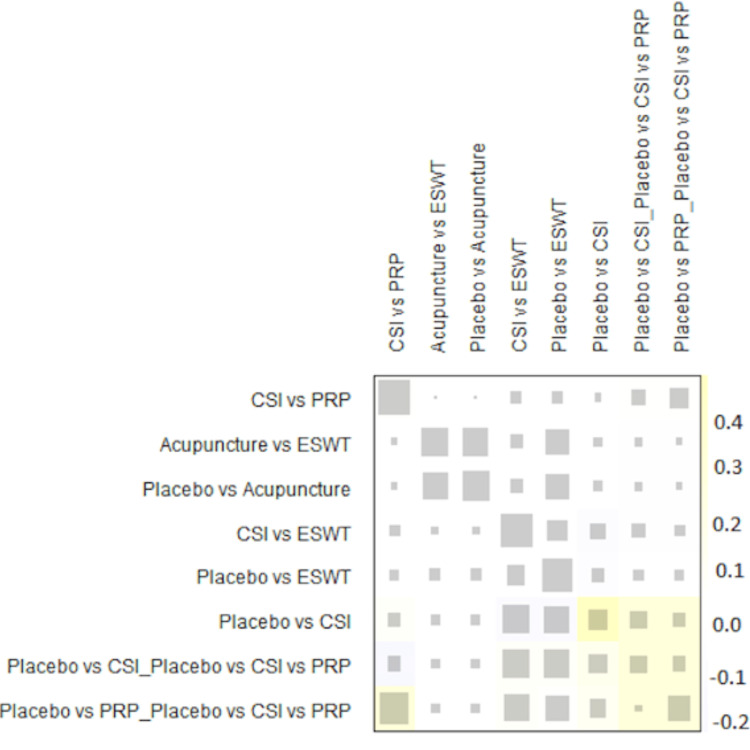
A total of 20 studies were included in the analysis of change in VAS score between six different treatment modalities (acupuncture, CSI, ESWT, PRP injection, USG therapy, and placebo). The most common comparison was between ESWT and placebo (Figure 2). The net heat plot showed significant heterogeneity when using a fixed-effect model, which was reduced when a random-effects model was used (Figure 3). The results of the network meta-analysis showed that acupuncture was associated with the highest reduction in pain compared to placebo, with an MD of -1.33 (95% confidence interval (95% CI) = -2.19 to -0.46) compared to placebo. All other treatments also showed moderate reduction in pain when compared to placebo, with CSI showing the least reduction in pain with an MD of -0.15 (95% CI = -0.89 to 0.58), as seen in Figure 4. Despite an insignificant MD between all treatment arms and placebo, the direct and indirect comparisons showed deviation from the null effect, indicating pain reduction when compared to placebo, as seen in Figure 5. Figure 6 further illustrates these direct and indirect effects, and all possible comparisons are shown in Table 3. Moreover, the funnel plot showed no significant publication bias, as Egger’s test resulted in a p-value of 0.42 (Figure 6).
Table 3. Matrix of comparisons for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
| S. No. | V1 | V2 | V3 | V4 | V5 | V6 |
| 1 | Acupuncture | - | 0.23 (-1.24; 1.70) | -1.75 (-2.79; -0.71) | - | - |
| 2 | -1.17 (-2.26; -0.09) | CSI | 0.51 (-0.34; 1.36) | -0.08 (-1.13; 0.96) | 0.81 (0.15; 1.47) | - |
| 3 | -0.61 (-1.53; 0.31) | 0.56 (-0.13; 1.25) | ESWT | -0.43 (-1.09; 0.23) | - | -0.21 (-1.06; 0.64) |
| 4 | -1.33 (-2.19; -0.46) | -0.15 (-0.89; 0.58) | -0.71 (-1.25; -0.18) | Placebo | - | 1.48 (0.01; 2.95) |
| 5 | -0.36 (-1.63; 0.91) | 0.81 (0.15; 1.47) | 0.25 (-0.70; 1.21) | 0.96 (-0.02; 1.95) | PRP | - |
| 6 | -0.58 (-1.73; 0.57) | 0.59 (-0.40; 1.58) | 0.03 (-0.72; 0.78) | 0.75 (-0.09; 1.59) | -0.22 (-1.41; 0.97) | Ultrasound |
Figure 2. Network graph showing the connections between interventions and number of studies for each comparison for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
Figure 3. Net heat plot showing the consistency of the network for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; CSI: Corticosteroid injection; VAS: Visual analog scale
Figure 4. Forest plot comparing the mean difference of all interventions with placebo for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale; MD: Mean deviation; CL: Confidence interval
Figure 5. Forest plot showing the direct and indirect comparisons between interventions for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; CSI: Corticosteroid injection; VAS: Visual analog scale; MD: Mean deviation; CL: Confidence interval
Figure 6. Funnel plot for change of VAS score after one month.
ESWT: Extracorporeal shock wave therapy; CSI: Corticosteroid injection; VAS: Visual analog scale
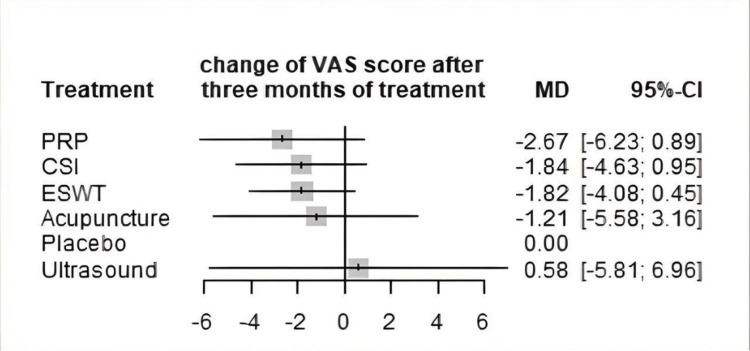
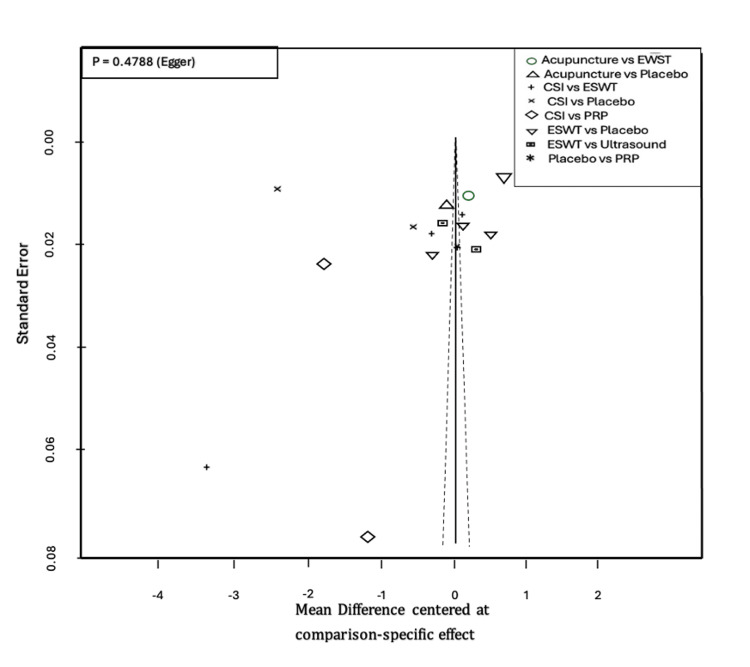
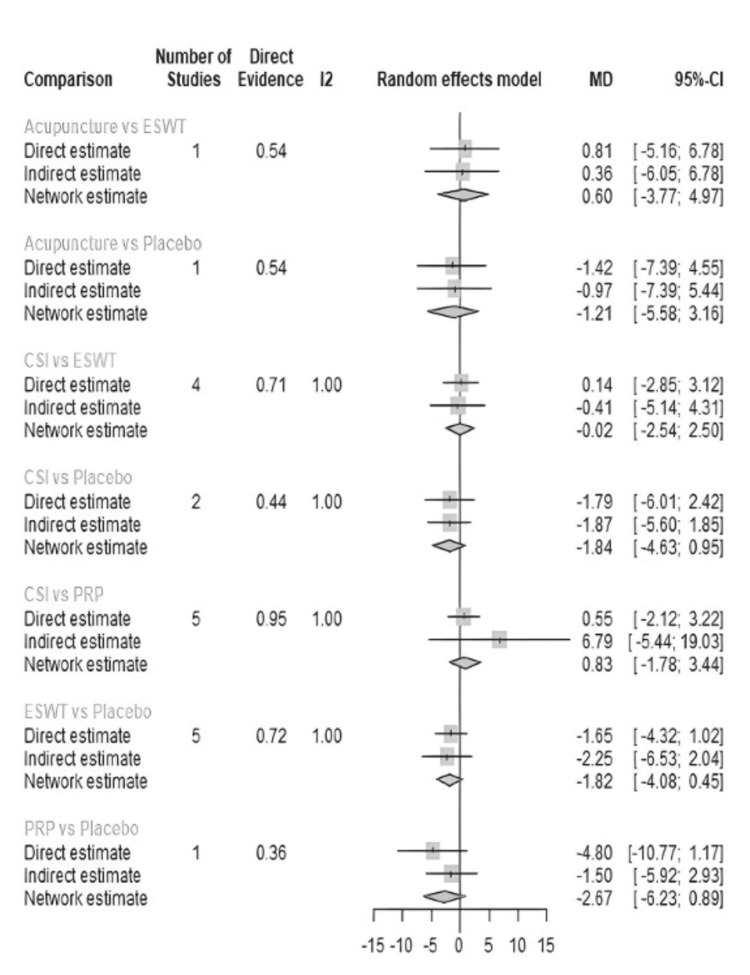
Change in VAS Score After Three Months
VAS score was measured at three months in 18 studies (Table 4). The most common comparisons were between ESWT against placebo and CSI with five and four studies, respectively (Figure 7). Similar to the one-month analysis, a random effects model was used to calculate the effect consistency of the network change of VAS score at three months using a net heat plot (Figure 8). The results of a Forrest plot comparing the MDs of treatments showed that the highest reduction in pain levels and effect size was achieved by PRP injection, with an MD of -2.67 (95% CI = -6.23 to 0.89; p = 0.77) compared to placebo, followed by CSI, with an MD of -1.84 (95% CI = -4.63 to 0.95; p = 0.61), and finally ESWT, acupuncture, and USG therapy (Figure 9). The node-splitting plot shown in Figure 9 indicates a consistent network via Egger’s test (p = 0.48), indicating no statistically significant publication bias (Figure 10). When treatment arms were compared with each other, the confidence interval of net effects of all treatments showed no or minimal deviation from the null effect, indicating no superiority between treatments (Figure 11).
Table 4. Matrix of comparisons for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
| S. No. | V1 | V2 | V3 | V4 | V5 | V6 |
| 1 | Acupuncture | - | 0.81 (-5.16; 6.78) | -1.42 (-7.39; 4.55) | - | - |
| 2 | 0.62 (-4.23; 5.48) | CSI | 0.14 (-2.85; 3.12) | -1.79 (-6.01; 2.42) | 0.55 (-2.12; 3.22) | - |
| 3 | 0.60 (-3.77; 4.97) | -0.02 (-2.54; 2.50) | ESWT | -1.65 (-4.32; 1.02) | - | -2.39 (-8.36; 3.57) |
| 4 | -1.21 (-5.58; 3.16) | -1.84 (-4.63; 0.95) | -1.82 (-4.08; 0.45) | Placebo | 4.80 (-1.17; 10.77) | - |
| 5 | 1.46 (-3.92; 6.83) | 0.83 (-1.78; 3.44) | 0.85 (-2.62; 4.32) | 2.67 (-0.89; 6.23) | PRP | - |
| 6 | -1.79 (-9.18; 5.61) | -2.41 (-8.89; 4.06) | -2.39 (-8.36; 3.57) | -0.58 (-6.96; 5.81) | -3.25 (-10.15; 3.66) | Ultrasound |
Figure 7. Network graph showing the connections between interventions and number of studies for each comparison for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
Figure 8. Net heat plot showing the consistency of the network for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
Figure 9. Forest plot comparing the mean difference of all interventions with placebo for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale; MD: Mean deviation; CL: Confidence interval
Figure 10. Funnel plot for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale
Figure 11. Forest plot showing the direct and indirect comparisons between interventions for change of VAS score after three months.
ESWT: Extracorporeal shock wave therapy; PRP: Platelet-rich plasma; CSI: Corticosteroid injection; VAS: Visual analog scale; MD: Mean deviation; CL: Confidence interval
Efficacy of Outcomes
In terms of efficacy for short-term VAS reduction, the acupuncture treatment arm had a better effect on VAS score reduction compared to the placebo and other treatment arms at the one-month mark. Acupuncture ranked highest in the forest plot in terms of MD, followed by PRP injection, USG therapy, ESWT, and CSI. However, at the three-month mark, acupuncture treatment was ranked below PRP injection, CSI, and ESWT, with PRP injection ranking the highest. There were no significant differences between treatments when compared against each other (Figure 11).
Discussions
Acupuncture Intervention
In TCM theory, plantar fasciitis is classified as part of heel pain diagnosis in the syndrome differentiation category. According to TCM, heel pain is due to the stagnation of qi and blood in certain channels or due to kidney deficiency. Repetitive stress and trauma to the heel due to inappropriate movement will cause stagnation of qi and blood in the channels, resulting in pain [56]. The kidney dominates bones, and the kidney meridian flows to the heel covering most of the sole. When the kidney becomes weak, the heel will lack nourishment from the kidney meridian, resulting in injury or wear and tear [57]. The acupuncturist decides on needling points depending on the cause of the heel pain and related meridian(s). Once decided, the needling is done by either the reinforcing or reducing technique depending on the cause of heel pain. Use of the reinforcing technique is more common, as heel pain is related to kidney deficiency or due to stagnation of qi and blood. This technique can be done either manually with an acupuncture needle or with the help of electro-acupuncture. When relating acupuncture to modern medicine to manage pain, numerous mechanisms have been described, including central opioid pain inhibition [57], the anti-inflammation effect [58], and diffuse noxious inhibitory control (DNIC) [59]. Needle insertion may alleviate pain by central opioid pain inhibition or DNIC, and provide an anti-inflammatory effect. However, this mechanism cannot be related directly to the specific sites where the needle is inserted, which varies based on diagnosis and pathology.
The current literature and studies suggest that acupuncture is an effective mode of treatment for plantar fasciitis [60]. One of the earliest English-language studies was published by Tillu and Gupta in 1998. They reviewed 18 patients who had failed standard first-line treatment and were treated with acupuncture intervention for six weeks and found a significant reduction in VAS pain score [61]. In an RCT by Kumnerddee and Pattapong on the efficacy of electro-acupuncture in chronic plantar fasciitis, 30 patients who failed conservative treatment for at least six weeks were selected [41]. The control group received five weeks of standard treatment, and the acupuncture group received five weeks of acupuncture sessions at least twice a week. After these patients were followed up for six weeks, 80% reported successful pain control. Similarly, a 2018 systematic review by Clark and Tighe on the effectiveness of acupuncture in plantar heel pain also concluded that this mode of treatment was effective and comparable to other treatments such as stretching and the use of splints [62].
Analysis Method
A network meta-analysis is a complex statistical analysis comparing the effectiveness of several treatment arms directly and indirectly, which is especially important when comparing treatment arms for a condition where there is no definitive management or one single effective treatment. Combining both direct and indirect evidence can estimate the relative effect of each treatment, and by including indirect evidence, there is an increase in the estimated effect size. Network meta-analysis has several important benefits. First, it allows available information to be extracted from several sets of studies into one analysis. Second, it can incorporate indirect evidence in a network, which cannot be done using conventional network meta-analysis. Finally, assuming all assumptions are met, and the results conclusive, network meta-analysis can determine the type of treatment preferable for the target population [63,64].
Network meta-analysis is sometimes criticized because of its use of indirect evidence in cases where evidence for direct comparison is available. The important point in network meta-analysis is the participants in randomized trials were randomly allocated to one treatment arm, treatment A or treatment B, but the trial condition was not selected using this network method [65].
The use of a frequentist framework is still more common than a Bayesian framework, as the results of the former are more easily understood. Frequentist focuses on direct comparisons between treatments and combines them using a random effects model. It also uses indirect comparisons, but interpretation in a frequentist framework uses p-values and CIs. In the Bayesian approach, instead of just point estimates, it provides full posterior distributions for each treatment effect, allowing for more nuanced comparisons. For example, it can give the probability that one treatment is the best among all, which is not directly available from a frequentist analysis. However, the disadvantage of using this model is that it does not support meta-regression. Frequentism uses a theoretical approach to interpret the probability of an event; when the process is repeated multiple times, the probability of the event in terms of how often it is expected to occur is established [66,67].
The frequentist method uses a p-score to rank treatment, which is equivalent to the surface under the cumulative ranking analysis (SUCRA) score used in the Bayesian method. In this method, when the MD shows a negative value or effect size, this indicates that the treatment is effective [66-68].
This network meta-analysis study did have some limitations. We only used the VAS score as a pain parameter, as this is the most frequently used parameter in most studies; we were unable to use foot function parameters (e.g., foot function index), as few studies used them. In addition, many studies were excluded from our meta-analysis because they failed to meet the inclusion criteria, limiting the total number of included studies.
Acupuncture as a Viable Treatment Option
As this network meta-analysis was mainly used to compare the use of acupuncture as an alternative to other non-surgical treatment options, we faced various challenges in finding high-quality studies to include. Studies involving acupuncture are seldom published in mainstream or English-language journals. Even with the use of the CKNI database, we were only able to include one study with an average-sized sample. Studies involving acupuncture treatment are impossible to do double-blinded, which affects their quality. Another problem we faced was the complexity and nuances of acupuncture treatment. In a condition like plantar fasciitis, syndrome differentiation is variable according to TCM. Therefore, the point of treatment selected for each patient was individualized according to the syndrome and not able to be synchronized among all patients. Although certain studies mention the use of certain points on all patients, this approach is potentially debatable.
The initial proposal to study the long-term effect of acupuncture was unable to be met due to the unavailability of long-term studies, which limited our analysis to the short-term effects of acupuncture treatment and other modalities such as ESWT, USG therapy, CSI, and PRP injection. Although long-term results would be preferable to assist clinicians in decision-making, this study could only conclude the effectiveness of acupuncture in the short term.
Many of the above-mentioned treatments were compared as a single treatment modality and not in combination with other forms of treatment. However, in reality, a combination treatment is most likely to be performed. For example, patients can be prescribed ESWT weekly in combination with acupuncture treatment or PRP injection. As a combination treatment model usually leads to better outcomes, we suggest that more studies using combination treatment be performed and published.
One drawback of acupuncture treatment is that it is not readily available in most modern hospitals. In addition, the learning curve to master an acupuncture treatment is steep and requires years of knowledge and clinical practice compared to treatment options such as CSI or PRP injection, which can be learned in one setting. In contrast, EWST and USG treatment options are readily available in most hospitals and usually performed by a trained physiotherapist.
Conclusions
Acupuncture treatment for plantar fasciitis is effective in short-term management and should be prescribed by well-trained clinicians. It should be considered a second-line treatment for plantar fasciitis together with other common treatment options such as ESWT, PRP injection, CSI, and USG therapy. Further long-term studies should be done to effectively determine the long-term outcomes of acupuncture treatment.
Acknowledgments
The authors of this study would like to thank Mr. Suyash Pravin Dhoot for his expert statistical advice on this study.
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Acquisition, analysis, or interpretation of data: Danny Kit Chung Wong, Indrarajah Asokumaran, Mohd Idham B. Hasan, Bavithaa Sufina Verasamy, Siew Siew Ong, Shih Chau Ng
Drafting of the manuscript: Danny Kit Chung Wong, Indrarajah Asokumaran, Mohd Idham B. Hasan, Bavithaa Sufina Verasamy, Siew Siew Ong, Shih Chau Ng
Critical review of the manuscript for important intellectual content: Danny Kit Chung Wong, Indrarajah Asokumaran, Mohd Idham B. Hasan, Bavithaa Sufina Verasamy, Siew Siew Ong, Shih Chau Ng
Concept and design: Indrarajah Asokumaran, Mohd Idham B. Hasan, Bavithaa Sufina Verasamy, Siew Siew Ong, Shih Chau Ng
Supervision: Mohd Idham B. Hasan, Bavithaa Sufina Verasamy, Siew Siew Ong, Shih Chau Ng
References
- 1.Role of mechanical factors in the clinical presentation of plantar heel pain: implications for management. Sullivan J, Pappas E, Burns J. Foot (Edinb) 2020;42:101636. doi: 10.1016/j.foot.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Prevalence of non-painful heel spur and its relation to postural foot position. Shama SS, Kominsky SJ, Lemont H. J Am Podiatry Assoc. 1983;73:122–123. doi: 10.7547/87507315-73-3-122. [DOI] [PubMed] [Google Scholar]
- 3.Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Landorf KB, Keenan AM, Herbert RD. Arch Intern Med. 2006;166:1305–1310. doi: 10.1001/archinte.166.12.1305. [DOI] [PubMed] [Google Scholar]
- 4.Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Lee SY, McKeon P, Hertel J. Phys Ther Sport. 2009;10:12–18. doi: 10.1016/j.ptsp.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 5.To study the effect of eccentric loading exercises of calf muscles in plantar fasciitis. An interventional study. Rupareliya D, Shukla Y, Bhise A, Prabhakar M. Physiotherapy. 2015;1:1303–1304. [Google Scholar]
- 6.Complications of plantar fascia rupture associated with corticosteroid injection. Acevedo JI, Beskin JL. Foot Ankle Int. 1998;19:91–97. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 7.Comparison of the acute effect of radial shock wave therapy and ultrasound therapy in the treatment of plantar fasciitis: a randomized controlled study. Akinoglu B, Köse N, Kirdi N, Yakut Y. Pain Med. 2017;18:2443–2452. doi: 10.1093/pm/pnx113. [DOI] [PubMed] [Google Scholar]
- 8.Extracorporeal shockwave therapy versus ultrasound therapy for plantar fasciitis: a systematic review and meta-analysis. Al-Siyabi Z, Karam M, Al-Hajri E, Alsaif A, Alazemi M, Aldubaikhi AA. Cureus. 2022;14:0. doi: 10.7759/cureus.20871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steroid injection for heel pain: evidence of short-term effectiveness. A randomized controlled trial. Crawford F, Atkins D, Young P, Edwards J. Rheumatology (Oxford) 1999;38:974–977. doi: 10.1093/rheumatology/38.10.974. [DOI] [PubMed] [Google Scholar]
- 10.How effective is therapeutic ultrasound in the treatment of heel pain? Crawford F, Snaith M. Ann Rheum Dis. 1996;55:265–267. doi: 10.1136/ard.55.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Injected corticosteroids for treating plantar heel pain in adults. David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. Cochrane Database Syst Rev. 2017;6:0. doi: 10.1002/14651858.CD009348.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Intense therapeutic ultrasound for treatment of chronic plantar fasciitis: a pivotal study exploring efficacy, safety, and patient tolerance. Heigh E, Bohman L, Briskin G, Slayton M, Amodei R, Compton K, Baravarian B. J Foot Ankle Surg. 2019;58:519–527. doi: 10.1053/j.jfas.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Corticosteroid injection is the best treatment in plantar fasciitis if combined with controlled training. Johannsen FE, Herzog RB, Malmgaard-Clausen NM, Hoegberget-Kalisz M, Magnusson SP, Kjaer M. Knee Surg Sports Traumatol Arthrosc. 2019;27:5–12. doi: 10.1007/s00167-018-5234-6. [DOI] [PubMed] [Google Scholar]
- 14.Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinç TT. J Am Podiatr Med Assoc. 2009;99:108–113. doi: 10.7547/0980108. [DOI] [PubMed] [Google Scholar]
- 15.Additive effect of therapeutic ultrasound in the treatment of plantar fasciitis: a randomized controlled trial. Katzap Y, Haidukov M, Berland OM, Itzhak RB, Kalichman L. J Orthop Sports Phys Ther. 2018;48:847–855. doi: 10.2519/jospt.2018.8110. [DOI] [PubMed] [Google Scholar]
- 16.Incidence of plantar fascia ruptures following corticosteroid injection. Kim C, Cashdollar MR, Mendicino RW, Catanzariti AR, Fuge L. Foot Ankle Spec. 2010;3:335–337. doi: 10.1177/1938640010378530. [DOI] [PubMed] [Google Scholar]
- 17.Therapeutic heat and cold. Lehmann JF, Warren CG, Scham SM. Clin Orthop Relat Res. 1974:207–245. doi: 10.1097/00003086-197403000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Therapeutic ultrasound: its effects on the cellular and molecular mechanisms of inflammation and repair. Maxwell L. Physiotherapy. 1992;78:421–426. [Google Scholar]
- 19.Ultrasound guided corticosteroid injection for plantar fasciitis: randomised controlled trial. McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. BMJ. 2012;344:0. doi: 10.1136/bmj.e3260. [DOI] [PubMed] [Google Scholar]
- 20.Therapeutic ultrasound. ter Haar G. Eur J Ultrasound. 1999;9:3–9. doi: 10.1016/s0929-8266(99)00013-0. [DOI] [PubMed] [Google Scholar]
- 21.Extracorporeal shockwave therapy in musculoskeletal disorders. Wang CJ. J Orthop Surg Res. 2012;7:11. doi: 10.1186/1749-799X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Comparison between extracorporeal shock wave therapy and local corticosteroid injection for plantar fasciitis. Xu D, Jiang W, Huang D, et al. Foot Ankle Int. 2020;41:200–205. doi: 10.1177/1071100719891111. [DOI] [PubMed] [Google Scholar]
- 23.Efficacy of electroacupuncture plus warm needling therapy for plantar heel pain: a randomised waitlist-controlled trial. Ho LF, Guo Y, Ching JY, et al. Acupunct Med. 2021;39:283–291. doi: 10.1177/0964528420946048. [DOI] [PubMed] [Google Scholar]
- 24.Therapeutic efficacy of platelet-rich plasma injection compared to corticosteroid injection in plantar fasciitis: a systematic review and meta-analysis. Mohammed W, Farah S, Nassiri M, McKenna J. J Orthop. 2020;22:124–134. doi: 10.1016/j.jor.2020.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comparison of efficacy of eight treatments for plantar fasciitis: a network meta-analysis. Li H, Lv H, Lin T. J Cell Physiol. 2018;234:860–870. doi: 10.1002/jcp.26907. [DOI] [PubMed] [Google Scholar]
- 26.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.A randomised controlled trial of steroid injection in the management of plantar fasciitis. Abdihakin M, Wafula K, Hasan S, MacLeod J. http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S1681-150X2012000400005&lng=en&nrm=iso SA Orthopaedic Journal. 2012;11:33–38. [Google Scholar]
- 28.Plantar fasciitis-a comparison of treatment with intralesional steroids versus platelet-rich plasma (a randomized, blinded study) Acosta-Olivo C, Elizondo-Rodriguez J, Lopez-Cavazos R, Vilchez-Cavazos F, Simental-Mendia M, Mendoza-Lemus O. J Am Podiatr Med Assoc. 2017;107:490–496. doi: 10.7547/15-125. [DOI] [PubMed] [Google Scholar]
- 29.The comparison of the effect of corticosteroids and platelet-rich plasma (PRP) for the treatment of plantar fasciitis. Akşahin E, Doğruyol D, Yüksel HY, Hapa O, Doğan O, Celebi L, Biçimoğlu A. Arch Orthop Trauma Surg. 2012;132:781–785. doi: 10.1007/s00402-012-1488-5. [DOI] [PubMed] [Google Scholar]
- 30.Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. JAMA. 2002;288:1364–1372. doi: 10.1001/jama.288.11.1364. [DOI] [PubMed] [Google Scholar]
- 31.Extra corporeal shock wave therapy versus local corticosteroid injection in the treatment of chronic plantar fasciitis, a single blinded randomized clinical trial. Eslamian F, Shakouri SK, Jahanjoo F, Hajialiloo M, Notghi F. Pain Med. 2016;17:1722–1731. doi: 10.1093/pm/pnw113. [DOI] [PubMed] [Google Scholar]
- 32.Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Gerdesmeyer L, Frey C, Vester J, et al. Am J Sports Med. 2008;36:2100–2109. doi: 10.1177/0363546508324176. [DOI] [PubMed] [Google Scholar]
- 33.Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. Haake M, Buch M, Schoellner C, et al. BMJ. 2003;327:75. doi: 10.1136/bmj.327.7406.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Hammer DS, Adam F, Kreutz A, Kohn D, Seil R. Foot Ankle Int. 2003;24:823–828. doi: 10.1177/107110070302401103. [DOI] [PubMed] [Google Scholar]
- 35.Chronic plantar fasciitis treated with two sessions of radial extracorporeal shock wave therapy. Ibrahim MI, Donatelli RA, Schmitz C, Hellman MA, Buxbaum F. Foot Ankle Int. 2010;31:391–397. doi: 10.3113/FAI.2010.0391. [DOI] [PubMed] [Google Scholar]
- 36.Platelet rich plasma versus corticosteroid injection for plantar fasciitis: a comparative study. Jain K, Murphy PN, Clough TM. Foot (Edinb) 2015;25:235–237. doi: 10.1016/j.foot.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Treatment of plantar fasciitis in recreational athletes: two different therapeutic protocols. Karagounis P, Tsironi M, Prionas G, Tsiganos G, Baltopoulos P. Foot Ankle Spec. 2011;4:226–234. doi: 10.1177/1938640011407320. [DOI] [PubMed] [Google Scholar]
- 38.A comparison of the effectiveness of radial extracorporeal shock wave therapy and ultrasound therapy in the treatment of chronic plantar fasciitis: a randomized controlled trial. Konjen N, Napnark T, Janchai S. https://www.ncbi.nlm.nih.gov/pubmed/25764613. J Med Assoc Thai. 2015;98 Suppl 1:0–56. [PubMed] [Google Scholar]
- 39.A comparative analysis of analgesic efficacy of ultrasound and shock wave therapy in the treatment of patients with inflammation of the attachment of the plantar fascia in the course of calcaneal spurs. Krukowska J, Wrona J, Sienkiewicz M, Czernicki J. Arch Orthop Trauma Surg. 2016;136:1289–1296. doi: 10.1007/s00402-016-2503-z. [DOI] [PubMed] [Google Scholar]
- 40.Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. J Orthop Res. 2006;24:115–123. doi: 10.1002/jor.20008. [DOI] [PubMed] [Google Scholar]
- 41.Efficacy of electro-acupuncture in chronic plantar fasciitis: a randomized controlled trial. Kumnerddee W, Pattapong N. Am J Chin Med. 2012;40:1167–1176. doi: 10.1142/S0192415X12500863. [DOI] [PubMed] [Google Scholar]
- 42.Ultrasonography and clinical outcome comparison of extracorporeal shock wave therapy and corticosteroid injections for chronic plantar fasciitis: a randomized controlled trial. Lai TW, Ma HL, Lee MS, Chen PM, Ku MC. https://pubmed.ncbi.nlm.nih.gov/29504578/ J Musculoskelet Neuronal Interact. 2018;18:47–54. [PMC free article] [PubMed] [Google Scholar]
- 43.Chronic plantar fasciitis: effect of platelet-rich plasma, corticosteroid, and placebo. Mahindra P, Yamin M, Selhi HS, Singla S, Soni A. Orthopedics. 2016;39:0–9. doi: 10.3928/01477447-20160222-01. [DOI] [PubMed] [Google Scholar]
- 44.Treatment outcomes of corticosteroid injection and extracorporeal shock wave therapy as two primary therapeutic methods for acute plantar fasciitis: a prospective randomized clinical trial. Mardani-Kivi M, Karimi Mobarakeh M, Hassanzadeh Z, et al. J Foot Ankle Surg. 2015;54:1047–1052. doi: 10.1053/j.jfas.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 45.Extracorporeal shock-wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. https://www.ncbi.nlm.nih.gov/pubmed/18411608. Acta Orthop Belg. 2008;74:98–101. [PubMed] [Google Scholar]
- 46.Egyptian Society for Joint Diseases and arthritis local injection of autologous platelet rich plasma and corticosteroid in treatment of lateral epicondylitis and plantar fasciitis: randomized clinical trial. Omar AS, Said M, Emad M, Sayed A. Egypt Rheumatol. 2012;34:43–49. [Google Scholar]
- 47.Effectiveness of single injection of platelet-rich plasma over corticosteroid in the treatment of plantar fasciitis - a randomized, comparative study. Sahoo PK, Ujade NA, Sakti P. J Musculoskelet Surg Res. 2020;4:187–193. [Google Scholar]
- 48.Comparison of platelet-rich plasma and steroid injection in the treatment of plantar fasciitis. Say F, Gürler D, İnkaya E, Bülbül M. Acta Orthop Traumatol Turc. 2014;48:667–672. doi: 10.3944/AOTT.2014.13.0142. [DOI] [PubMed] [Google Scholar]
- 49.Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. Speed CA, Nichols D, Wies J, Humphreys H, Richards C, Burnet S, Hazleman BL. J Orthop Res. 2003;21:937–940. doi: 10.1016/S0736-0266(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 50.The effect of corticosteroid local injection versus platelet-rich plasma for the treatment of plantar fasciitis in obese patients: a single-blind, randomized clinical trial. Tabrizi A, Dindarian S, Mohammadi S. J Foot Ankle Surg. 2020;59:64–68. doi: 10.1053/j.jfas.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 51.Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Theodore GH, Buch M, Amendola A, Bachmann C, Fleming LL, Zingas C. Foot Ankle Int. 2004;25:290–297. doi: 10.1177/107110070402500503. [DOI] [PubMed] [Google Scholar]
- 52.Platelet rich plasma therapy: a comparative effective therapy with promising results in plantar fasciitis. Tiwari M, Bhargava R. J Clin Orthop Trauma. 2013;4:31–35. doi: 10.1016/j.jcot.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clinical effectiveness of extracorporeal shock wave treatment combined with electric acupuncture for chronic plantar fasciitis [Article in Chinese] Wang JH, Xu YH, Wang G, Li HF, Zhu XH, Xie J. http://www.zgkfzz.com/ch/reader/view_abstract.aspx?file_no=20120311 Chin J Rehabil. 2012;27:191–193. [Google Scholar]
- 54.Comparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitis. Yucel I, Ozturan KE, Demiraran Y, Degirmenci E, Kaynak G. J Am Podiatr Med Assoc. 2010;100:105–110. doi: 10.7547/1000105. [DOI] [PubMed] [Google Scholar]
- 55.Full-length silicone insoles versus ultrasound-guided corticosteroid injection in the management of plantar fasciitis: a randomized clinical trial. Yucel U, Kucuksen S, Cingoz HT, Anliacik E, Ozbek O, Salli A, Ugurlu H. Prosthet Orthot Int. 2013;37:471–476. doi: 10.1177/0309364613478328. [DOI] [PubMed] [Google Scholar]
- 56.Acupuncture treatment of heel pain. Hu JS. J Tradit Chin Med. 2009;29:150–152. doi: 10.1016/s0254-6272(09)60053-4. [DOI] [PubMed] [Google Scholar]
- 57.Acupuncture and endorphins. Han JS. Neurosci Lett. 2004;361:258–261. doi: 10.1016/j.neulet.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 58.Anti-inflammatory actions of acupuncture. Zijlstra FJ, van den Berg-de Lange I, Huygen FJ, Klein J. Mediators Inflamm. 2003;12:59–69. doi: 10.1080/0962935031000114943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Acupuncture mechanisms for clinically relevant long-term effects - reconsideration and a hypothesis. Carlsson C. Acupunct Med. 2002;20:82–99. doi: 10.1136/aim.20.2-3.82. [DOI] [PubMed] [Google Scholar]
- 60.How effective is acupuncture for reducing pain due to plantar fasciitis? Thiagarajah AG. Singapore Med J. 2017;58:92–97. doi: 10.11622/smedj.2016143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Effect of acupuncture treatment on heel pain due to plantar fasciitis. Tillu A, Gupta S. Acupunct Med. 1998;16:66–68. [Google Scholar]
- 62.The effectiveness of acupuncture for plantar heel pain: a systematic review. Clark RJ, Tighe M. Acupunct Med. 2012;30:298–306. doi: 10.1136/acupmed-2012-010183. [DOI] [PubMed] [Google Scholar]
- 63.The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Bucher HC, Guyatt GH, Griffith LE, Walter SD. J Clin Epidemiol. 1997;50:683–691. doi: 10.1016/s0895-4356(97)00049-8. [DOI] [PubMed] [Google Scholar]
- 64.A guide and pragmatic considerations for applying GRADE to network meta-analysis. Izcovich A, Chu DK, Mustafa RA, Guyatt G, Brignardello-Petersen R. BMJ. 2023;381:0. doi: 10.1136/bmj-2022-074495. [DOI] [PubMed] [Google Scholar]
- 65.Simultaneous comparison of multiple treatments: combining direct and indirect evidence. Caldwell DM, Ades AE, Higgins JP. BMJ. 2005;331:897–900. doi: 10.1136/bmj.331.7521.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Frequentist and Bayesian approaches to data analysis: evaluation and estimation. Pek J, Van Zandt T. Psychol Learn Teach. 2020;19:21–35. [Google Scholar]
- 67.Ranking treatments in frequentist network meta-analysis works without resampling methods. Rücker G, Schwarzer G. BMC Med Res Methodol. 2015;15:58. doi: 10.1186/s12874-015-0060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Regularization in regression: comparing Bayesian and frequentist methods in a poorly informative situation. Celeux G, Anbari ME, Marin J, Robert CP. https://www.researchgate.net/publication/47342016_Regularization_in_Regression_Comparing_Bayesian_and_Frequentist_Methods_in_a_Poorly_Informative_Situation Bayesian Anal. 2012;7:477–502. [Google Scholar]