Abstract
Background: Relative fat mass (RFM) represents a newly developed sex-specific anthropometric formula to estimate total body fat percentage. Nonetheless, research examining the correlation between RFM and the risk of diabetes remains scarce. This research assessed the link between RFM and DM risk within the Japanese demographic. Methods: From 2004 to 2015, 15,462 Japanese individuals without diabetes underwent physical evaluations at Murakami Memorial Hospital. The relationship between RFM and the onset of diabetes was analyzed separately using Cox proportional-hazards regression models. This study employed Cox proportional hazards regression incorporating cubic spline functions and smooth curve fitting to detect non-linear associations between RFM and new cases of diabetes, categorized by sex. Sensitivity analyses were performed to confirm the robustness of the link between RFM and incident diabetes. Results: After controlling for confounding factors, a significant positive correlation between RFM and diabetes risk was found in women (HR: 1.13, 95%CI: 1.04–1.24, P = 0.0061), while the association in men was not statistically significant (HR: 1.05, 95%CI: 0.98–1.13, P = 0.1511). Additionally, a non-linear relationship between RFM and the incidence of diabetes was detected in both genders. The RFM threshold was identified at 39.23 for women and 23.08 for men. For women, HR was 1.11 (95%CI: 1.01–1.21) below the threshold and 1.39 (95%CI: 1.17–1.65) above it. In men, an RFM above 23.08 was positively related to diabetes risk (HR: 1.16, 95%CI: 1.06–1.28, P = 0.0012), whereas an RFM below this point did not show a significant association (HR: 0.98, 95%CI: 0.91–1.06, P = 0.5899). Conclusion: Our findings suggest a non-linear relationship and threshold effect between RFM and the risk of diabetes. These findings imply that maintaining RFM at lower levels may be beneficial in mitigating the onset of DM.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-74635-7.
Keywords: Relative fat mass, Adiposity, Waist circumference, Diabetes mellitus, Non-linear
Subject terms: Diseases, Endocrinology, Diabetes, Obesity
Introduction
Diabetes mellitus (DM) poses a significant global public health challenge, with its prevalence reaching epidemic proportions. The International Diabetes Federation reports that approximately 463 million adults currently have DM, a number projected to rise to 700 million by 20451. The increasing burden of diabetes underscores the need to identify and understand modifiable risk factors to inform effective prevention and management strategies.
Obesity is a well-established risk factor for DM, accounting for roughly 90% of all cases2. Traditional obesity metrics, such as body mass index (BMI), are widely used in epidemiological studies but have notable limitations. BMI does not distinguish between fat and lean mass and overlooks fat distribution, which is crucial for assessing metabolic risk. Relative Fat Mass (RFM) is a novel anthropometric index developed by Woolcott and Bergman in 2018 as a response to the limitations of BMI3. RFM considers both height and waist circumference, offering a more nuanced assessment of body composition. It is calculated using a straightforward equation: RFM = 64 - [20 × (height/waist circumference)] for males, and RFM = 76 - [20 × (height/waist circumference)] for females3. This formula was derived from a large, diverse sample using dual-energy X-ray absorptiometry (DXA) as the reference standard. RFM provides a more accurate estimation of an individual’s body fat percentage compared to traditional metrics like BMI3. Recent studies using RFM as an adiposity measure have demonstrated its predictive ability for dyslipidemia, severe liver disease, all-cause mortality, metabolic syndrome, hypertension, and cardiovascular disease4–8. However, except for one small sample study from the Netherlands, research on the relationship between RFM and diabetes is minimal9. No associations have been reported in the Japanese population, and the potential non-linear relationship between RFM and diabetes remains unexplored. To address this research gap, we conducted a large-sample retrospective cohort study to elucidate the relationship between RFM and diabetes mellitus among the Japanese.
Methods
Data source
This research utilized open-source data from the NAGALA (NAFLD in Gifu Area, Longitudinal Analysis) database, serving as a secondary analysis within a medical examination program. The center responsible for these programs, established in 1994, conducted over 8,000 medical examinations annually, with approximately 60% of participants undergoing one to two examinations per year. Owing to the high frequency of repeated examinations, the original study cohort included all individuals who participated in repeated examinations between 2004 and 2015. Researchers can freely obtain and access the original study data from the Dryad Digital Repository (https://datadryad.org/). This dataset (DOI: 10.5061/dryad.8q0p192) includes data from 15,464 participants who were free of diabetes at baseline10. Complying with Dryad’s terms of service, we utilized this dataset for secondary analysis. Our research entailed a secondary examination of publicly accessible medical examination program data.
Study participants
Informed written consent was obtained from all participants during the primary study, which received approval from the Clinical Research Ethics Committee at Murakami Memorial Hospital10. Additionally, ethical approval for this study was granted by the Shenzhen Dapeng New District Nan’ao People’s Hospital Ethics Committee. The research protocol adhered to the Helsinki Declaration’s principles and was conducted in strict accordance with applicable regulations and guidelines.
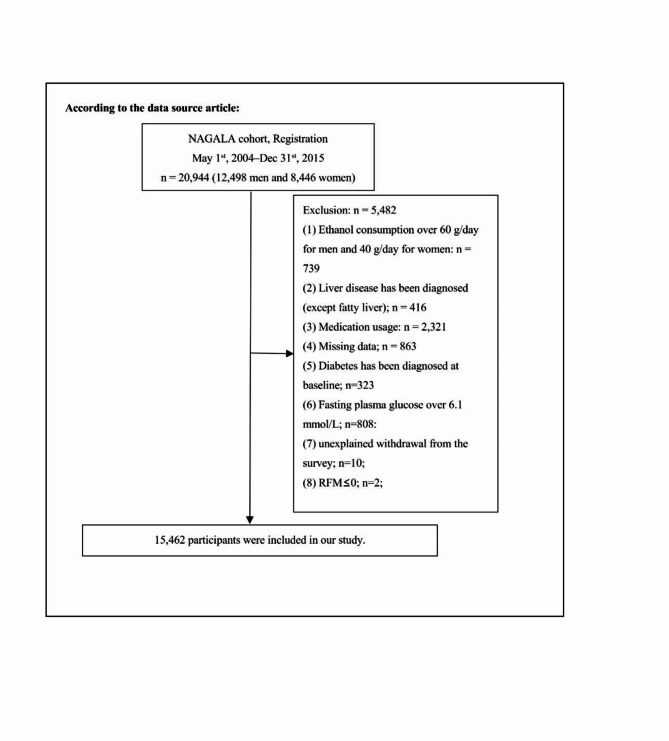
We acquired data from a database made available by the Murakami Memorial Hospital in Japan, encompassing 20,944 participants who underwent medical examinations between 2004 and 2015. The exclusion criteria established in the initial research were as follows: (1) alcohol consumption over 60 g/day for men and 40 g/day for women, (2) presence of viral hepatitis, indicated by the detection of hepatitis B antigen or hepatitis C antibody at baseline, (3) usage of any medication at baseline, (4) diagnosed diabetes at baseline, (5) missing covariate data, (6) fasting plasma glucose levels of ≥ 6.1 mmol/L, and (7) unexplained withdrawal from the survey. Consequently, the original study included 15,464 participants. In our secondary analysis, we excluded an additional 2 subjects whose RFM was ≤ 0. Ultimately, our study’s data analysis comprised 15,462 individuals, consisting of 8,428 males and 7,034 females (Fig. 1).
Fig. 1.
Study population.
Covariates
Clinical expertise and previous research findings informed the selection of Covariates for this investigation5,6,9,11–15. The considered factors included: (1) continuous variables: triglycerides (TG), glycosylated hemoglobin (HbA1c), alanine aminotransferase (ALT), total cholesterol (TC), gamma-glutamyl transferase (GGT), FPG, systolic blood pressure (SBP), aspartate aminotransferase (AST), age, BMI, high-density lipoprotein cholesterol (HDL-C) diastolic blood pressure (DBP) and alcohol consumption; (2) categorical variables: smoking status, exercise habits, and gender. Participants’ lifestyle and medical history details were collected using a standardized questionnaire from the initial study. Trained professionals accurately measured waist circumference (WC), weight, height, and blood pressure. The original research team gathered laboratory test results using a consistent protocol under controlled conditions.
Relative fat mass
RFM is a recently developed anthropometric index designed to estimate an individual’s body fat percentage based on their height and waist circumference. The RFM formula addresses several limitations associated with traditional BMI by emphasizing waist measurement, which is a more accurate indicator of adiposity and associated health risks. The formulas used to calculate RFM are gender-specific, reflecting physiological differences in fat distribution. For males, RFM is calculated as: RFM = 64-[20×height/waist circumference] for males, and RFM = 76-[20×height/waist circumference] for females3,4,16,17.
Diagnosis of incident diabetes
Diabetes was diagnosed through one of the following criteria: fasting plasma glucose levels of 7 mmol/L or above, glycosylated hemoglobin levels of 6.5% or higher18, or a self-reported diagnosis during the follow-up period.
Statistical analysis
We performed statistical analysis using Empower-Stats. Participants’ characteristics were categorized by diabetes status. Continuous variables with skewed and normal distributions were presented as median (quartile) and mean ± standard deviation, respectively. Group differences were analyzed using the Wilcoxon rank-sum test (for skewed distributions), two-sample t-tests (for normal distributions), and the χ2 test (for categorical variables).
Univariate Cox regression analysis evaluated the impact of individual variables on diabetes risk. Multivariate Cox regression analysis explored the specific association between RFM and DM risk. Model 1 was unadjusted. Model 2 adjusted for gender, age, BMI, alcohol intake, smoking status, exercise habits, SBP, and DBP. Model 3 included all adjustments from Model 2 plus TG, ALT, HbA1c, HDL-C, AST, FPG, GGT, and TC. Hazard ratios (HR) and 95% confidence intervals (CI) were meticulously documented.
Given that RFM is a continuous variable, we examined potential nonlinear relationships between RFM and DM using Cox proportional hazards regression with cubic spline functions and smooth curve fitting. If a nonlinear connection was identified, a two-piecewise Cox proportional hazards regression model was applied to determine the inflection point. Log-likelihood ratio analysis selected the most appropriate model for RFM and DM connection.
The validity of our findings was confirmed through sensitivity analyses. RFM was categorized by quartile, and a P-value for trend was calculated to validate the results from RFM as a continuous variable. Additional sensitivity analyses excluded individuals with hypertensive (SBP ≥ 140 mmHg and DBP ≥ 90 mmHg) or aged ≥ 65 years to evaluate RFM’s association with diabetes risk. The study adhered to the STROBE statement for all outcomes19. Statistical significance was determined using two-tailed tests with a threshold of P < 0.05.
Results
Characteristics of participants
This study analyzed data from 15,089 participants without DM and 373 with DM. The average age of the cohort was 43.71 ± 8.90 years, with males comprising 54.51% of the sample. Table 1 presents the results, highlighting significant differences between non-DM and DM groups across various metrics. The DM group had notably higher levels of blood pressure, BMI, RFM, WC, alcoholic intake, age, AST, ALT, GGT, TC, TG, FPG, and HbA1c. Additionally, the DM cohort had a higher proportion of males, smokers, and drinkers. Conversely, the DM group showed reduced levels of HDL-C and a lower prevalence of regular exercise compared to the non-DM group.
Table 1.
The baseline characteristics of participants.
| Baseline characteristic | Non-DM | DM | P-value |
|---|---|---|---|
| Participants | 15,089 | 373 | |
| Gender | < 0.001 | ||
| Female | 6947 (46.04%) | 87 (23.32%) | |
| Male | 8142 (53.96%) | 286 (76.68%) | |
| Age(years) | 43.62 ± 8.89 | 47.14 ± 8.52 | < 0.001 |
| Alcoholic intake (g/wk) | 1 (0–60) | 4.20 (0–90) | 0.006 |
| Smoking status | < 0.001 | ||
| Never-smoker | 8886 (58.89%) | 145 (38.87%) | |
| Ex-smoker | 2874 (19.05%) | 77 (20.64%) | |
| Current-smoker | 3329 (22.06%) | 151 (40.48%) | |
| Exercise habits | 0.048 | ||
| No | 12,432 (82.39%) | 322 (86.33%) | |
| Yes | 2657 (17.61%) | 51 (13.67%) | |
| SBP (mmHg) | 114.31 ± 14.91 | 122.03 ± 15.59 | < 0.001 |
| DBP (mmHg) | 71.44 ± 10.47 | 77.18 ± 10.23 | < 0.001 |
| BMI (kg/m2) | 22.05 ± 3.07 | 25.03 ± 3.82 | < 0.001 |
| WC (cm) | 76.26 ± 8.97 | 85.08 ± 10.20 | < 0.001 |
| RFM | 25.75 ± 6.75 | 27.14 ± 6.82 | < 0.001 |
| ALT (IU/L) | 17 (13–23) | 24 (18–39) | < 0.001 |
| AST (IU/L) | 17 (14–21) | 20 (16–26) | < 0.001 |
| GGT (IU/L) | 15 (11–22) | 24 (17–36) | < 0.001 |
| HDL-C (mmol/L) | 1.47 ± 0.40 | 1.19 ± 0.33 | < 0.001 |
| TG (mmol/L) | 0.72 (0.49–1.11) | 1.21 (0.86–1.93) | < 0.001 |
| TC (mmol/L) | 5.12 ± 0.86 | 5.43 ± 0.90 | < 0.001 |
| HbA1c (%) | 5.16 ± 0.32 | 5.53 ± 0.37 | < 0.001 |
| FPG (mmol/L) | 5.15 ± 0.41 | 5.61 ± 0.36 | < 0.001 |
Values are n (%) or mean ± SD or median (quartile)
RFM: relative fat mass; BMI: body mass index; WC: waist circumference; SBP: systolic blood pressure; DBP: diastolic blood pressure; ALT: alanine aminotransferase; AST: aspartate aminotransferase; GGT: gamma-glutamyl transferase; HDL-C: high-density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides; HbA1c: hemoglobin A1c; FPG: fasting plasma glucose
Univariate analysis
The univariate analysis results are displayed in Table 2. The findings indicated that higher levels of DBP, SBP, age, WC, BMI, RFM, TG, HbA1c, TC, FPG, ALT, GGT, and AST, along with increased alcohol consumption and smoking, were associated with an elevated risk of diabetes. Conversely, HDL-C was inversely related to diabetes risk. Additionally, males exhibited a greater propensity for diabetes compared to females.
Table 2.
The results of the univariate analysis.
| Statistics | HR (95% CI) | P value | |
|---|---|---|---|
| Gender | |||
| Female | 7034 (45.492%) | ref | |
| Male | 8428 (54.508%) | 2.522 (1.984, 3.207) | < 0.0001 |
| Age(years) | 43.709 ± 8.898 | 1.056 (1.044, 1.069) | < 0.0001 |
| Alcoholic intake (g/wk) | 47.741 ± 82.321 | 1.002 (1.001, 1.003) | 0.0012 |
| Smoking status | |||
| Never-smoker | 9031 (58.408%) | ref | |
| Ex-smoker | 2951 (19.085%) | 1.655 (1.255, 2.182) | 0.0004 |
| Current-smoker | 3480 (22.507%) | 2.583 (2.056, 3.244) | < 0.0001 |
| Exercise habits | 0.0641 | ||
| No | 12,754 (82.486%) | ref | |
| Yes | 2708 (17.514%) | 0.756 (0.563, 1.016) | |
| SBP (mmHg) | 114.497 ± 14.974 | 1.032 (1.026, 1.037) | < 0.0001 |
| DBP (mmHg) | 71.581 ± 10.506 | 1.049 (1.040, 1.058) | < 0.0001 |
| BMI (kg/m2) | 22.117 ± 3.127 | 1.242 (1.216, 1.268) | < 0.0001 |
| WC (cm) | 76.475 ± 9.098 | 1.093 (1.083, 1.103) | < 0.0001 |
| RFM | 25.788 ± 6.758 | 1.044 (1.028, 1.060) | < 0.0001 |
| ALT (IU/L) | 19.989 ± 14.344 | 1.006 (1.005, 1.007) | < 0.0001 |
| AST (IU/L) | 18.401 ± 8.642 | 1.008 (1.006, 1.010) | < 0.0001 |
| GGT (IU/L) | 20.309 ± 18.136 | 1.011 (1.009, 1.013) | < 0.0001 |
| HDL-C (mmol/L) | 1.461 ± 0.404 | 0.148 (0.109, 0.202) | < 0.0001 |
| TG (mmol/L) | 0.912 ± 0.655 | 1.798 (1.681, 1.923) | < 0.0001 |
| TC (mmol/L) | 5.126 ± 0.864 | 1.493 (1.342, 1.661) | < 0.0001 |
| HbA1c (%) | 5.172 ± 0.322 | 54.273 (39.491, 74.588) | < 0.0001 |
| FPG (mmol/L) | 5.161 ± 0.413 | 25.377 (18.710, 34.421) | < 0.0001 |
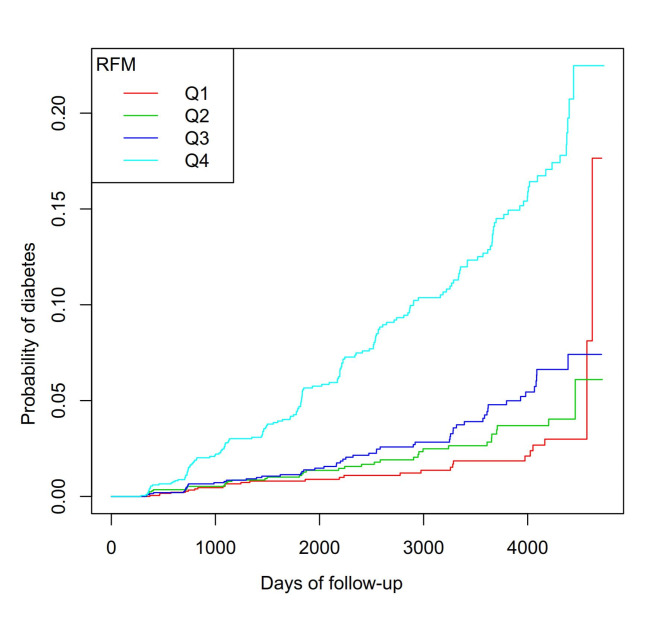
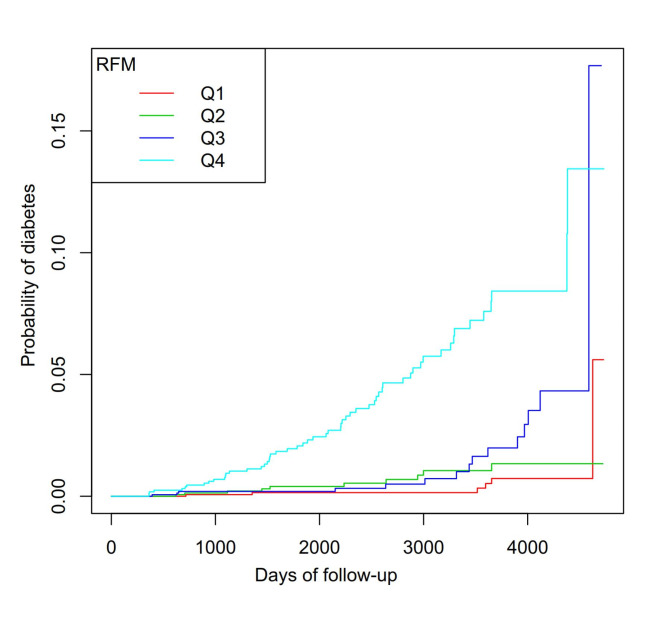
Figures 2 and 3 display Kaplan-Meier curves of diabetes likelihood, stratified by RFM quartiles according to sex. The probability of diabetes varied significantly among RFM groups in both genders (log-rank test, P < 0.001), with the risk progressively increasing with higher RFM levels. This trend suggests that individuals in the highest RFM quartile had the highest diabetes risk.
Fig. 2.
Kaplan–Meier event-free survival curve. Kaplan–Meier analysis of incident diabetes based on RFM quartiles in males (log-rank, P < 0.0001).
Fig. 3.
Kaplan–Meier event-free survival curve. Kaplan–Meier analysis of incident diabetes based on RFM quartiles in females (log-rank, P < 0.0001).
The incidence rate of DM
As illustrated in Table 1S, over a median follow-up period of 6.04 years, 373 participants developed DM. The cumulative incidence rates of DM were 3.99 per 1,000 person-years for the entire cohort, 2.10 for females, and 5.48 for males. The incidence rates were 2.41% for the overall study population, 1.24% for women, and 3.39% for men. Within the female subgroup, the cumulative incidence rates of DM for the four quartiles of RFM (Q1, Q2, Q3, Q4) were 0.52, 0.95, 1.52, and 5.91 per 1,000 person-years, respectively. Correspondingly, the incidence rates were 0.34%, 0.57%, 0.85%, and 3.18%. A significant positive correlation was observed between higher RFM values and increased incidence rates of DM in females. This pattern was similarly observed among male participants.
The connection between RFM and DM risk
Table 3 illustrates the Cox proportional hazards regression analysis, detailing the HR and 95%CI to elucidate the relationship between RFM and diabetes risk. The analysis includes three models: unadjusted (Model 1) and two adjusted (Models 2 and 3). A significant positive association was found between RFM and diabetes incidence in the unadjusted Model 1 (HR: 1.28, 95%CI: 1.22–1.33, P < 0.0001 for females; HR: 1.22, 95%CI: 1.18–1.26, P < 0.0001 for males). This association remained in Model 2, which adjusted for age, smoking status, BMI, alcohol intake, exercise habits, SBP, and DBP, with similar results (HR: 1.19, 95%CI: 1.09–1.30, P < 0.0001 for females; HR: 1.11, 95%CI: 1.04–1.18, P = 0.0023 for males). In Model 3, following adjustments for covariates from Model 2 along with TG, ALT, HbA1c, HDL-C, AST, FPG, GGT, and TC, the HR for the relationship between RFM levels and diabetes risk was 1.13 for females and 1.05 for males (HR: 1.13, 95%CI: 1.04–1.24, P = 0.0061 for females; HR: 1.05, 95%CI: 0.98–1.13, P = 0.1511 for males).
Table 3.
Relationship between RFM and incident diabetes in different models.
| Variable | Model 1 (HR,95%CI, P) | Model 2 (HR,95% CI, P) | Model 3 (HR,95% CI, P) | |
|---|---|---|---|---|
| All | RFM | 1.24 (1.21, 1.27) < 0.0001 | 1.13 (1.08, 1.19) < 0.0001 | 1.08 (1.02, 1.14) 0.0055 |
| RFM (quartile) | ||||
| Q1 | ref | ref | ref | |
| Q2 | 2.01 (1.46, 2.76) < 0.0001 | 0.98 (0.69, 1.38) 0.9003 | 0.72 (0.51, 1.03) 0.0719 | |
| Q3 | 5.19 (3.79, 7.11) < 0.0001 | 1.32 (0.87, 2.00) 0.1972 | 0.96 (0.63, 1.47) 0.8539 | |
| Q4 | 19.03 (12.27, 29.53) < 0.0001 | 1.65 (0.84, 3.25) 0.1484 | 1.18 (0.58, 2.39) 0.6543 | |
| P for trend | < 0.0001 | 0.1033 | 0.6038 | |
| Female | RFM | 1.28 (1.22, 1.33) < 0.0001 | 1.19 (1.09, 1.30) < 0.0001 | 1.13 (1.04, 1.24) 0.0061 |
| RFM (quartile) | ||||
| Q1 | ref | ref | ref | |
| Q2 | 2.11 (0.76, 5.81) 0.1502 | 1.40 (0.50, 3.90) 0.5190 | 1.34 (0.48, 3.75) 0.5814 | |
| Q3 | 3.59 (1.39, 9.29) 0.0084 | 1.61 (0.60, 4.29) 0.3442 | 1.28 (0.47, 3.49) 0.6335 | |
| Q4 | 14.42 (6.17, 33.68) < 0.0001 | 2.86 (1.04, 7.88) 0.0419 | 1.63 (0.56, 4.72) 0.3711 | |
| P for trend | < 0.0001 | 0.0240 | 0.3942 | |
| Male | RFM | 1.22 (1.18, 1.26) < 0.0001 | 1.11 (1.04, 1.18) 0.0023 | 1.05 (0.98, 1.13) 0.1511 |
| RFM (quartile) | ||||
| Q1 | ref | ref | ref | |
| Q2 | 1.40 (0.86, 2.30) 0.1791 | 0.96 (0.58, 1.60) 0.8867 | 0.60 (0.36, 1.01) 0.0547 | |
| Q3 | 1.99 (1.26, 3.15) 0.0034 | 0.97 (0.59, 1.59) 0.9002 | 0.50 (0.30, 0.85) 0.0107 | |
| Q4 | 6.09 (4.05, 9.15) < 0.0001 | 1.76 (1.04, 3.00) 0.0367 | 0.82 (0.47, 1.46) 0.5031 | |
| P for trend | < 0.0001 | 0.0085 | 0.7088 |
Model 1: we did not adjust for any covariants.
Model 2: we adjusted for gender, age, BMI, alcoholic intake, smoking status, exercise habits, SBP, and DBP.
Model 3: we adjusted for gender, age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
Note: The models were not adjusted for gender variables in both male and female models.
HR: hazard ratio; CI: confidence interval; Ref: Reference; RFM: relative fat mass.
We also transformed RFM from continuous data to a definite format and incorporated it into Model 3. Compared to the Q1 reference group of RFM, the HR (95% CI) for the Q2, Q3, and Q4 groups were 0.72 (0.51–1.03), 0.96 (0.63–1.47), and 1.18 (0.58–2.39), respectively, indicating no statistically significant relationship between categorically transformed RFM and diabetes.
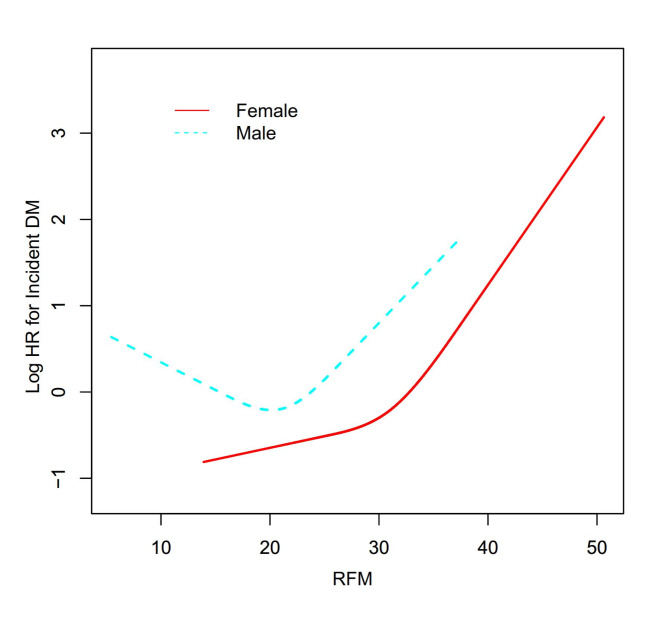
The analyses of the non-linear relationship
Figure 4 illustrates the nonlinear connection between RFM and DM risk. Table 4 further highlights this nonlinear association in both male and female cohorts after adjusting for confounders. This research applied a segmented Cox proportional hazards regression model to determine the inflection points for RFM, which were 39.23 in females and 23.08 in males (P for log-likelihood ratio test = 0.009 for females, 0.002 for males). For females, the HR was 1.11 (95% CI: 1.01–1.21) to the left of the inflection point, increasing to 1.39 (95% CI: 1.17–1.65) to the right. In males, the RFM exceeding 23.08 demonstrated a positive association with diabetes risk (HR: 1.16, 95% CI: 1.06–1.28), whereas an RFM below 23.08 did not show a statistically significant correlation (HR: 0.98, 95% CI: 0.91–1.06).
Fig. 4.
The nonlinear relationship between RFM and incident diabetes stratified by gender. The nonlinear relationship was detected after adjusting for age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
Table 4.
The result of the two-piecewise Cox proportional hazards regression model by gender.
| Incident DM | All participants (HR, 95%CI, P) |
Female (HR, 95%CI, P) |
Male (HR, 95%CI, P) |
|---|---|---|---|
| Fitting model by standard linear regression | 1.08 (1.02, 1.14) 0.0055 | 1.13 (1.04, 1.24) 0.0061 | 1.05 (0.98, 1.13) 0.1511 |
| Fitting model by two-piecewise Cox proportional hazards regression | |||
| The inflection point of RFM | 22.06 | 39.23 | 23.08 |
| ≤ Inflection point | 0.97 (0.90, 1.05) 0.4941 | 1.11 (1.01, 1.21) 0.0256 | 0.98 (0.91, 1.06) 0.5899 |
| > Inflection point | 1.12 (1.06, 1.19) 0.0002 | 1.39 (1.17, 1.65) 0.0002 | 1.16 (1.06, 1.28) 0.0012 |
| P for log-likelihood ratio test | 0.002 | 0.009 | 0.002 |
Note 1: In all participants, we adjusted gender, age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
Note 2: For female and male subgroups, we adjusted for age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
HR: hazard ratios; CI: confidence; DM: diabetes mellitus; RFM: relative fat mass
Sensitive analysis
We conducted sensitivity analyses on participants under 65 to validate our findings, carefully adjusting for multiple potential confounders. The results confirmed a nonlinear relationship between RFM and diabetes risk in both sexes (Table 5, Model 4). We refined our analysis by excluding individuals with hypertension (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg). After applying similar adjustments for confounding variables, we observed similar results in both females and males (Table 5, Model 5).
Table 5.
The relationship between RFM and incident diabetes is analyzed using a two-piecewise Cox proportional hazards regression model in different sensitivity analyses.
| Incident DM | Female (HR, 95%CI, P) |
Male (HR, 95%CI, P) |
All participants (HR, 95%CI, P) |
|---|---|---|---|
| Model 4 | |||
| Fitting model by standard linear regression | 1.15 (1.05, 1.27) 0.0026 | 1.06 (0.99, 1.13) 0.1181 | 1.08 (1.03, 1.14) 0.0033 |
| Fitting model by two-piecewise Cox proportional hazards regression | |||
| The inflection point of RFM | 38.99 | 21.54 | 21.08 |
| ≤ Inflection point | 1.12 (1.02, 1.23) 0.0141 | 0.95 (0.87, 1.04) 0.2724 | 0.96 (0.88, 1.05) 0.3448 |
| > Inflection point | 1.40 (1.18, 1.67) 0.0002 | 1.15 (1.05, 1.25) 0.0018 | 1.12 (1.06, 1.19) 0.0001 |
| P for log-likelihood ratio test | 0.011 | 0.002 | 0.003 |
| Model 5 | |||
| Fitting model by standard linear regression | 1.13 (1.03, 1.24) 0.0104 | 1.04 (0.97, 1.12) 0.2628 | 1.07 (1.01, 1.14) 0.0143 |
| Fitting model by two-piecewise Cox proportional hazards regression | |||
| The inflection point of RFM | 38.66 | 23.29 | 22.29 |
| ≤ Inflection point | 1.10 (1.00, 1.20) 0.0525 | 0.97 (0.89, 1.05) 0.4154 | 0.97 (0.89, 1.05) 0.3934 |
| > Inflection point | 1.42 (1.19, 1.68) < 0.0001 | 1.17 (1.06, 1.29) 0.0025 | 1.12 (1.05, 1.19) 0.0005 |
| P for log-likelihood ratio test | 0.003 | 0.001 | 0.001 |
Model 4 was a sensitivity analysis in participants with age < 65 years.
Model 5 was a sensitivity analysis conducted on participants with SBP < 140mmHg and DBP < 90mmHg.
Note 1: In all participants, we adjusted gender, age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
Note 2: For female and male subgroups, we adjusted for age, BMI, alcoholic intake, smoking status, exercise habits, SBP, DBP, ALT, AST, GGT, HDL-C, TC, TG, HbA1c, and FPG.
HR: hazard ratios; CI: confidence; DM: diabetes mellitus; RFM: relative fat mass
Discussion
In this retrospective cohort study, we identified a correlation between elevated RFM and incident diabetes in females after adjusting for confounding factors. The analysis revealed a nonlinear relationship between RFM levels and diabetes onset, differentiated by gender, with inflection points at 39.23 for females and 23.08 for males. Sensitivity analyses further validated the robustness of these findings.
The prevalence of diabetes has been rising globally in recent decades, placing significant economic strain on national healthcare systems20,21. Obesity is a major risk factor for diabetes development22. Although BMI is commonly used to diagnose obesity, it has limitations as it cannot differentiate between weight gain due to muscle and that due to fat23. Recently, RFM has been a novel metric for estimating body fat percentage based on sex, WC, and height. RFM emerged as the most accurate and user-friendly measure in a comprehensive analysis of 365 anthropometric metrics3. In recent years, RFM has garnered increasing attention, with numerous studies demonstrating its close association with diabetes mellitus, dyslipidemia, metabolic syndrome, severe liver disease, hypertension, and cardiovascular disease4–9. In a cross-sectional study including 20,167 patients, RFM was more predictive of various dyslipidemias and metabolic syndrome than BMI6. In a cross-sectional study including 3,406 individuals from China, RFM was strongly associated with hypertension risk after adjusting for confounders (HR:2.032, 95%CI: 1.567–2.634)4. Furthermore, a prospective longitudinal study from the Netherlands involving 7,961 participants found that a one-unit increment in RFM corresponded to a 119% higher risk of DM (HR:2.19, 95%CI: 1.96–2.44) after adjusting for prevalent hypertension, smoking, age, sex, and family history of diabetes9. This retrospective analysis demonstrated a gender-specific correlation between RFM and diabetes incidence. A significant positive association was observed in females, whereas male subjects exhibited no statistically meaningful relationship. After adjusting for confounding factors, each unit increase in RFM raised the diabetes risk by 13% in females. Sensitivity analyses confirmed the robustness of these findings, demonstrating a consistent link between RFM and diabetes risk. These results provide clinical guidelines for RFM-level interventions to reduce diabetes risk.
This study was the first to examine the nonlinear connection between RFM and diabetes across genders. After controlling for confounding covariates, the smooth curve analysis revealed a nonlinear relationship in both sexes. Using a two-piecewise Cox proportional hazards regression model, we identified RFM inflection points: 39.23 for females and 23.08 for males. In females, a one-unit increment in RFM below 39.23 was associated with an 11% increase in diabetes risk (HR: 1.11, 95% CI: 1.01–1.21), while above 39.23, the risk increased by 39% (HR: 1.39, 95% CI: 1.17–1.65). In males, RFM above 23.08 correlated with a 16% increase in diabetes risk (HR: 1.16, 95% CI: 1.06–1.28), whereas RFM below 23.08 showed no significant correlation (HR: 0.98, 95% CI: 0.91–1.06). Therefore, our findings suggest that maintaining lower RFM levels can reduce the risk of diabetes.
The relationship between RFM, a metric that accounts for body fat percentage, and the development of diabetes is not well understood. This association may be linked to excess fatty tissue’s metabolic and inflammatory effects. Adipose tissue, particularly visceral fat, secretes a variety of bioactive molecules known as adipokines and inflammatory cytokines, which can induce insulin resistance and impair glucose metabolism24. Adipose tissue contributes to chronic low-grade inflammation, affecting the signal transduction pathways of neighboring cells, including eosinophils, macrophages, B-regulatory cells, and T cells (including invariant natural killer cells)25. These interactions further exacerbate metabolic disturbances, leading to pancreatic β-cell dysfunction, reduced insulin sensitivity, and ultimately contribute to the development of diabetes26.
Our study has several notable strengths. Firstly, we identified the nonlinear relationship between RFM and diabetes, accurately pinpointing the optimal inflection point for RFM’s impact on diabetes by gender. Secondly, our results underwent rigorous statistical adjustments to minimize confounding effects, enhancing their credibility. Thirdly, the robustness of our conclusions was confirmed through sensitivity analyses, which included transforming RFM and reevaluating the RFM-diabetes relationship after excluding participants with a BMI ≥ 24 kg/m2 or hypertension.
However, this investigation has some limitations. Firstly, the investigation was limited to the Japanese population, restricting the generalizability of our findings to other ethnic and geographical groups. Secondly, the original research excluded individuals with ≥ 6.1 mmol/L those with viral hepatitis, those exhibiting excessive alcohol consumption, those using any medications at baseline, and those with missing covariate data. Such exclusion criteria may have influenced the representativeness of the sample. In future research, we aim to design a study that includes a more diverse population with a larger sample size to validate our findings and enhance their generalizability. Thirdly, as with all retrospective studies, unmeasured or uncontrolled confounding variables, such as dietary patterns or family history of diabetes, could influence our results despite efforts to account for known covariates. Fourthly, In the original study upon which our secondary analysis is based, participants with impaired fasting glucose (IFG) were excluded, and data on glucose tolerance tests or glycated hemoglobin levels were not available. Consequently, we were unable to identify or include individuals with impaired glucose tolerance (IGT) or IFG in our current analysis. In the future, we will undertake future research that will include participants with both IFG and IGT. This will enable a more comprehensive evaluation of the risk associated with RFM during these intermediary stages. Lastly, our study measured baseline WC and height without considering changes over time. Future research should include more comprehensive monitoring of confounding factors, including fluctuations in WC and height during follow-up, to explore the impact of changes in RFM on future diabetes risk.
Conclusion
Our study elucidated a nonlinear relationship and threshold effect between RFM and diabetes risk, stratified by gender. Specifically, we observed that RFM levels exceeding 39.23 were strongly associated with an increased risk of diabetes in females. In contrast, in males, only RFM levels above 23.08 were linked to an elevated risk of diabetes. These findings underscore the critical importance of maintaining lower RFM levels as a strategy to mitigate diabetes risk, thereby providing a theoretical foundation for targeted intervention measures.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- RFM
Relative fat mass
- DM
Diabetes mellitus
- BMI
Body mass index
- WC
Waist circumference
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- GGT
Gamma-glutamyl transferase
- HDL-C
High-density lipoprotein cholesterol
- TC
Total cholesterol
- TG
Triglycerides
- HbA1c
Glycosylated hemoglobin
- FPG
Fasting plasma glucose
- HR
Hazard ratio
- SD
Standard deviation
- CI
Confidence interval
Author contributions
Binhui Xiao, and Changchun Cao contributed to the study concept and design, researched and interpreted the data, and drafted the manuscript. Yong Han, Haofei Hu, and Yongcheng He analyzed the data and reviewed the manuscript. Binhui Xiao and Changchun Cao oversaw the project’s progress, contributed to the discussion and reviewed the manuscript. Yong Han, Yong Han, Haofei Hu, and Yongcheng He are the guarantors of this work and, as such, had full access to all the data in the study and took responsibility for the data’s integrity and the data analysis’s accuracy. All authors read and approved the final manuscript.
Data availability
The raw data can be downloaded from the ‘DATADRYAD’ database (www.Datadryad.org). Dryad Digital Repository. https://datadryad.org/stash/dataset/doi:10.5061%2Fdryad.8q0p192.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
In the initial study, informed written consent was obtained from all participants after receiving approval from the Clinical Research Ethics Committee at Murakami Memorial Hospital. In addition, the study has also been approved by the Ethics Committee of the Shenzhen Dapeng New District Nan’ao People’s Hospital (2022082201) and was conducted under the ethical principles of the Declaration of Helsinki.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Binhui Xiao, and Changchun Cao have contributed equally to this work.
Contributor Information
Yong Han, Email: hanyong511023@163.com.
Haofei Hu, Email: huhaofei0319@126.com.
Yongcheng He, Email: heyongcheng640815@126.com.
References
- 1.Williams, R. et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 162, 108072 (2020). [DOI] [PubMed] [Google Scholar]
- 2.Abdullah, A., Peeters, A., de Courten, M. & Stoelwinder, J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res. Clin. Pract. 89 (3), 309–319 (2010). [DOI] [PubMed] [Google Scholar]
- 3.Woolcott, O. O. & Bergman, R. N. Relative fat mass (RFM) as a new estimator of whole-body fat percentage horizontal line a cross-sectional study in American adult individuals. Sci. Rep. 8 (1), 10980 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu, P., Huang, T., Hu, S. & Yu, X. Predictive value of relative fat mass algorithm for incident hypertension: A 6-year prospective study in Chinese population. BMJ Open. 10 (10), e38420 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andreasson, A., Carlsson, A. C., Onnerhag, K. & Hagstrom, H. Predictive capacity for mortality and severe liver disease of the relative fat mass algorithm. Clin. Gastroenterol. Hepatol. 17 (12), 2619–2620 (2019). [DOI] [PubMed] [Google Scholar]
- 6.Kobo, O., Leiba, R., Avizohar, O. & Karban, A. Relative fat mass is a better predictor of dyslipidemia and metabolic syndrome than body mass index. Cardiovasc. Endocrinol. Metab. 8 (3), 77–81 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woolcott, O. O. & Bergman, R. N. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): Association with mortality in NHANES 1999–2014. Int. J. Obes. (Lond). 44 (6), 1301–1310 (2020). [DOI] [PubMed] [Google Scholar]
- 8.Zwartkruis, V. W. et al. Relative fat mass and prediction of incident atrial fibrillation, heart failure and coronary artery disease in the general population. Int. J. Obes. (Lond). 47 (12), 1256–1262 (2023). [DOI] [PubMed] [Google Scholar]
- 9.Suthahar, N. et al. Associations of relative fat mass, a new index of adiposity, with type-2 diabetes in the general population. Eur. J. Intern. Med. 109, 73–78 (2023). [DOI] [PubMed] [Google Scholar]
- 10.Okamura, T. et al. Ectopic fat obesity presents the greatest risk for incident type 2 diabetes: A population-based longitudinal study. Int. J. Obes. (Lond). 43 (1), 139–148 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Cao, C., Han, Y., Hu, H., He, Y. & Luo, J. Non-linear relationship between pulse pressure and the risk of pre-diabetes: A secondary retrospective Chinese cohort study. BMJ Open. 14 (3), e80018 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao, C. et al. The nonlinear correlation between alanine aminotransferase to high-density lipoprotein cholesterol ratio and the risk of diabetes: a historical Japanese cohort study. BMC Endocr. Disord. 23 (1), 124 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zha, F. et al. The nonlinear correlation between the cardiometabolic index and the risk of diabetes: A retrospective Japanese cohort study. Front. Endocrinol. (Lausanne). 14, 1120277 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cao, C. et al. Non-linear relationship between high-density lipoprotein cholesterol and incident diabetes mellitus: a secondary retrospective analysis based on a Japanese cohort study. BMC Endocr.. Disord. 22 (1), 163 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao, C. et al. Association between central obesity and incident diabetes mellitus among Japanese: A retrospective cohort study using propensity score matching. Sci. Rep. 12 (1), 13445 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paek, J. K., Kim, J., Kim, K. & Lee, S. Y. Usefulness of relative fat mass in estimating body adiposity in Korean adult population. Endocr. J. 66 (8), 723–729 (2019). [DOI] [PubMed] [Google Scholar]
- 17.Shen, W. et al. Associations of relative fat mass, a novel adiposity indicator, with non-alcoholic fatty liver disease and cardiovascular disease: Data from SPECT-China. Diabetes Metab. Syndr. Obes. 16, 2377–2387 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2021. Diabetes Care. 44 (Suppl 1), S15–S33 (2021). [DOI] [PubMed] [Google Scholar]
- 19.von Elm, E. et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 12 (12), 1495–1499 (2014). [DOI] [PubMed] [Google Scholar]
- 20.Guariguata, L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res. Clin. Pract. 103 (2), 137–149 (2014). [DOI] [PubMed] [Google Scholar]
- 21.Cho, N. H. et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281 (2018). [DOI] [PubMed] [Google Scholar]
- 22.Maggio, C. A. & Pi-Sunyer, F. X. Obesity and type 2 diabetes. Endocrinol. Metab. Clin. N. Am. 32 (4), 805–822 (2003). [DOI] [PubMed] [Google Scholar]
- 23.Gomez-Ambrosi, J. et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int. J. Obes. (Lond). 36 (2), 286–294 (2012). [DOI] [PubMed] [Google Scholar]
- 24.Kahn, S. E., Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 444 (7121), 840–846 (2006). [DOI] [PubMed] [Google Scholar]
- 25.Hotamisligil, G. S. Inflammation and metabolic disorders. Nature. 444 (7121), 860–867 (2006). [DOI] [PubMed] [Google Scholar]
- 26.Butler, A. E. et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 52 (1), 102–110 (2003). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data can be downloaded from the ‘DATADRYAD’ database (www.Datadryad.org). Dryad Digital Repository. https://datadryad.org/stash/dataset/doi:10.5061%2Fdryad.8q0p192.