Summary
Background
Climate-change-induced extreme precipitation events have attracted global attention; however, the associated excess deaths burden has been insufficiently explored and remains unclear.
Methods
We first defined an extreme precipitation event for each county when the daily total precipitation exceeded the county-specific 99·5th percentile of the daily precipitation from 1986 to 2005; then we estimated the associations between extreme precipitation events and cause-specific deaths in 280 Chinese counties using a two-stage time-series model. Second, we projected the excess deaths related to extreme precipitation events by combining the bias-corrected multi-model precipitation predictions derived under different combined emission-population scenarios of three representative concentration pathways (RCPs; RCP2·6, RCP4·5, and RCP8·5) and three shared socioeconomic pathways (SSP2, a business-as-usual scenario) populations (S1, low fertility rate; S2, medium fertility rate; and S3, high fertility rate). We quantified the climate and population contributions to the changes of future excess deaths nationwide and by climatic zones.
Findings
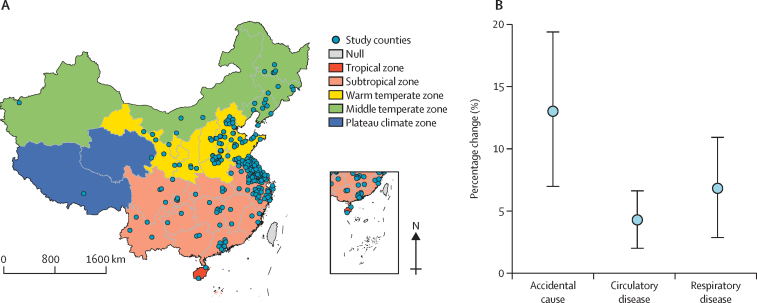
Compared with the non-extreme precipitation days, the percentage increase of deaths associated with exposure to extreme precipitation days is 13·0% (95% CI 7·0–19·3) for accidental cause, 4·3% (2·0–6·6) for circulatory disease, and 6·8% (2·8–10·9) for respiratory disease. The number of annual average excess deaths related to extreme precipitation events during 1986–2005 was 2644 (95% CI 1496–3730) for accidental cause, 69 (33–105) for circulatory disease, and 181 (79–279) for respiratory disease. In the 2030s, the total number of excess deaths of these three causes will increase by 1244 (43%), 1756 (61%), and 2008 (69%) under RCP2·6, RCP4·5, and RCP8·5 scenarios combined with a medium-fertility-rate population (SSP2-S2), respectively, but will decrease by 3% under RCP2·6–SSP2-S2 and increase by 25% under RCP8·5–SSP2-S2 in the 2090s. Humid and water-limited regions in subtropical, middle-temperate, and plateau climate zones will face highly increased risks. Climate and population factors contributed disproportionally among the five climate zones.
Interpretation
This study is the largest integrated projection exploring the disease burden associated with extreme precipitation events. The excess deaths will be amplified by climate and population changes. Improving mitigation and adaptation capacities is crucial when responding to precipitation extremes.
Funding
National Natural Science Foundation of China and Wellcome Trust.
Introduction
Precipitation is one of four key indicators of the climate system. The effect of the changing climate on the global water cycle has driven a wide variety in the frequency, intensity, and spatial extent of heavy rainfall, leading to an increasing trend of extreme precipitation events.1, 2 According to the sixth report of the Intergovernmental Panel on Climate Change, extreme precipitation events increased to 1·3 times in the majority of land regions compared with the 1850–1900 average. As reported, 66·4% of stationary historical records derived in global grids exhibited positive daily extreme precipitation trends from 1964 to 2013.3 Global annual precipitation over land is projected to increase by an average of 8·3% (0·9 to 12·9) under the high-carbon scenario and by 2·4% (−0·2 to 4·7) even under the low-carbon scenario up until the end of the 21st century relative to the 1995−2014 period. Notably, China suffered from the heaviest recorded extreme precipitation in the last decade: on 20−21 July, 2012, Beijing was hit by heavy rainfall, with over 90% of the city having precipitation exceeding 100 mm, causing over 60 direct deaths and a 34% higher risk of all-cause mortality;4 on 20−21 July, 2021, multiple cities in Henan Province were hit by record-breaking rainfall,5 resulting in 302 deaths due to flooding and tens of billions of US$ in property losses.6 Because extreme precipitation events can cause devastating fatalities,7 it is important to focus on the disease burden from the perspectives of guiding climate change adaptation planning and public health preventive measures.8
Research in context.
Evidence collected before this study
We searched articles published until January, 2022 in PubMed, Web of Science, and the China National Knowledge Infrastructure using keywords including “extreme precipitation”, “heavy rainfall”, “precipitation” or “rainfall”, “projection” or “predict”, “disease burden”, “health risk”, “mortality”, or “excess deaths”, and “climate change”. By screening the title, abstract, and main text of the articles, we found a small number of previous studies that projected the disease burden associated with extreme precipitation events; however, these previous studies mainly concentrated on the regional burdens of infectious or allergic diseases. To date, the associated disease burden corresponding to accidental and non-accidental causes, including circulatory and respiratory diseases, has, we believe, been insufficiently explored and thus remains unclear.
Added value of this study
In this study, we did an integrated projection of the future excess deaths associated with extreme precipitation events in China. This study is an initiative of the Lancet Countdown Asia Centre, which aims to provide multidimensional projections of the future health risks resulting from climate change in China. We first applied a time-series study to explore the associations between cause-specific mortality and extreme precipitation events in the warm season using a 6-year multicentre dataset; on the basis of this dataset, we assessed the baseline and future excess deaths attributed to extreme precipitation events by using changes in precipitation under climate change and population development. We found significant associations between extreme precipitation events and accidental and non-accidental deaths. The near-term future excess deaths will increase in the 2030s under all three climate-population scenarios, respectively. But this deaths burden may decrease under the low-carbon scenario of representative concentration pathway 2.6 in the 2090s.
Implications of all the available evidence
This is the first evidence representing the accidental, circulatory, and respiratory disease death burdens related to extreme precipitation events. Our projections indicate that extreme precipitation events will be exacerbated in China in the future. The associated excess deaths of accidental, circulatory, and respiratory diseases will be amplified under a changing climate; these results provide objectives for public health intervention responding to extreme weather disasters.
However, the health effects related to extreme precipitation events have remained unclear thus far. Very few previous studies have projected the disease burden associated with extreme precipitation events, instead mainly focusing on waterborne infection emergencies9 or subsequent flood-related health risks.10 However, few of these studies provided any integrated conclusions because the authors applied a single climate change scenario, focused only on infectious disease, or studied only a single city or region. The widespread health effects of extreme precipitation events on accidental or environmentally sensitive outcomes (eg, respiratory and circulatory diseases) have thus been insufficiently explored,11 and nationwide high-resolution projections under different climate change scenarios have rarely been reported, leading to a gap in the evidence when trying to understand the disease burden associated with extreme precipitation events and the policy implications associated with the planning of response strategies.
Here, we did an integrated study on future projections of extreme precipitation event-associated excess deaths in China. We first applied a time-series analysis to obtain the association between cause-specific mortality and extreme precipitation events using a 6-year multicentre dataset. Then, we assessed the numbers of excess deaths attributed to extreme precipitation events at baseline and in the future by using changes in precipitation under climate change and population development. This study is an initiative of the Lancet Countdown Asia Centre, which aims to provide multidimensional projections of the future health risks resulting from climate change in China. The latest available high-resolution climate data (at a 0·25° resolution) from regional circulation models are used; for the population data, the latest birth rate trends reported after the issuance of the so-called three-child policy are employed.
Methods
Historical precipitation
Historical daily total precipitation observations recorded from Jan 1, 1986 to Dec 31, 2005 were obtained from the China Meteorological Data Service Center. The original data had a 25 km × 25 km grid resolution, based on which we extracted the county-level daily total precipitation by calculating the mean value of all grid cells within the boundaries of each certain county. We used this dataset to define county-specific precipitation thresholds.
Future precipitation
The future daily total precipitation simulations are derived from RegCM4.4 climate simulations over the CORDEX-East Asia domain by use of three climate models from the Coupled Model Intercomparison Project Phase 5 ensembles:12 MOHC-HadGEM2-ES, MPI-ESM-MR, and NorESM1-M. These three general climate models (GCMs) can provide available daily total precipitation data on 0·25° × 0·25° latitude−longitude grids in both the historical period (1986–2005) and the future period (2021–2100) under three representative concentration pathway (RCP) scenarios, RCP2·6, RCP4·5, and RCP8·5. These RCPs describe three different 21st century pathways of greenhouse gas emissions in the future: RCP2·6 is representative of a stringent mitigation scenario that keeps global warming below 2°C by the end of this century relative to the pre-industrial global averaged temperature; RCP8·5 is a very high-emission scenario representing high greenhouse gas emission with global warming probably exceeding 2°C; and RCP4·5 is an intermediate scenario with a relatively lower greenhouse gas emission compared with RCP8·5.
To eliminate possible biases in the simulated precipitation data, we applied a bias-correction step recommended in a previous study to adjust the simulations of three GCMs.13 Briefly, we matched the daily historical observations and the historical simulations derived for the same period within the same month and obtained the monthly biases between these values using a non-linear function.14 Then, we assumed that these biases remain the same between the future observations and simulations, and, on the basis of these biases, we corrected the outputs of the three models to obtain the future adjusted daily precipitation amounts.
Definition of an extreme precipitation event
In this study, we applied a relative threshold to define extreme precipitation events. Because there is not an internationally consistent definition of extreme precipitation event, we first applied five definitions using different thresholds including: daily precipitation exceeded the 99·5th threshold, daily precipitation exceeded the 99th threshold, daily precipitation exceeded the 98·5th threshold, daily precipitation exceeded the 98th threshold, or daily precipitation exceeded 50 mm (an absolute threshold). On the basis of associations between extreme precipitation events and cause-specific mortality (appendix p 6), we chose the 99·5th threshold because of its largest effect estimated among all those five definitions. Then we calculated the 99·5th percentile of daily total precipitation in each county from 1986 to 2005 using historical observations, and these high values were set as county-specific thresholds. Then, we defined an extreme precipitation event as the day with daily total precipitation exceeding the thresholds. In this way, we identified the extreme event days in the baseline years (1986–2005) as well as the three future 20-year periods including 2021–40, 2051–70, and 2081–2100 under RCP2·6, RCP4·5, and RCP8·5 on the basis of the bias-corrected precipitation simulations from the three GCMs.
Exposure–response relationship between extreme precipitation events and mortality
In this study, we analysed the associations between exposure to extreme precipitation events and cause-specific mortality by applying a nationwide two-stage time-series study. We focused on accidental deaths and non-accidental causes including circulatory (ICD-10 code I00-I99) and respiratory diseases (ICD-10 code J00-J99), which are two leading causes of deaths in the Chinese population and recognised as climate-sensitive diseases.15 The daily counts of accidental mortality and two main non-accidental causes of mortality, including circulatory and respiratory diseases, were collected in 280 Chinese counties during 2013–18 from the Death Surveillance Points of the Chinese Center for Disease Control and Prevention. These counties were selected because they met the inclusion criteria including an average mortality rate greater than 0·45% in 2013–18, and an annual fluctuation of death rate of less than 20%. Therefore, we tried to reduce the uncertainty in estimating the exposure relationship by ensuring the quality of mortality data. These 280 counties covered about 0·19 billion population, accounting for nearly 13·9% of the total Chinese population recorded in the 2010 census (1·37 billion).
In addition, we also obtained county-level historical daily total precipitation levels from 2013 to 2018 to identify extreme precipitation events for each county. We then ensembled the dataset by matching the daily extreme precipitation events with the daily cause-specific death counts in each county. In the first stage, we constructed a generalised linear model with a quasi-Poisson distribution to estimate the association separately for each county. The main model is listed here:
| (1) |
In this model, EP, an extreme precipitation event, was set as a dichotomous variable (1=extreme precipitation day, 0=non-extreme precipitation day); considering the possible influence from temperature and relative humidity on mortality, the natural cubic spline function (ns) with two degrees of freedom (df) was used to control for the potential confounding effects of temperature (Temp) and relative humidity (RH); the low correlations between extreme precipitation events and these two meteorological factors did not show collinearity (temperature: coefficient 0·057, p<0·01; relative humidity: coefficient 0·10, p<0·01); a natural cubic spline of time with four dfs per year was used to control for long-term mortality trends; and the day of the week (DOW) was used to exclude the mortality variations that occur among different days of the week. To obtain the robust estimation of associations between extreme precipitation days and cause-specific mortality, we then limited the analysis to the warm period lasting from May to October, because the monthly averaged extreme precipitation exposure mainly concentrated during this period (appendix p 7). We examined the lagged effect of extreme precipitation event exposure by considering up to a maximum lag of 7 days (lag1 to lag7). In the second stage, we used the county-level estimates from the first stage to pool the overall associations at nation level by fitting random effect meta-regression models, which allows us to analyse the substantial heterogeneity among different counties. The results were reported as percentage change in daily deaths associated with exposure to extreme precipitation day with 95% CIs for accidental, circulatory, and respiratory mortality. In this study, we used the pooled estimate to approximately represent the association between extreme precipitation events and mortality for the whole country, which enables us to project the future excess deaths at the national level. But as a supplement, we did a multivariate meta-regression analysis to explain the heterogeneity from multiple socioeconomic factors including baseline mortality, the proportion of the older population, the proportion of urban residents, gross domestic product, and the number of hospitals among counties.
To test the robustness of the main model, we did sensitivity analyses of multiple dimensions, including changing the dfs of the meteorological factors and time, using a linear function to control for meteorological factors, removing the relative humidity variable, adding wind speed and atmospheric pressure as confounders, using different definitions of extreme precipitation days, using the whole year exposure instead of warm season exposure, and to examine the possible health effects from extreme precipitation events with longer duration, we also identified events defined as the daily precipitation exceeding the 99·5th threshold for at least 2 days.
Mortality rate and population projection
The nation-level baseline mortality rates of accidental cause, circulatory disease, and respiratory disease were calculated by dividing the sum of annual average deaths by the total census populations reported for the 280 counties in 2010. We assumed that these baseline rates would remain stable in the future. We then applied three population scenarios under the considered shared socioeconomic pathways (SSPs) from 2021 to 2040 (2030s), 2051 to 2070 (2060s), and 2081 to 2100 (2090s), including SSP2 (a business-as-usual scenario)-S1 (low fertility rate), SSP2-S2 (moderate fertility rate), and SSP2-S3 (high fertility rate). SSP2 was considered to be the scenario closest to the current development trend of the Chinese population, and the gridded population at a 1 km × 1 km resolution was derived from previous work;16 the future yearly Chinese population was extracted and reanalysed on the basis of global population projection by considering the recent fertility-promoting policies (eg, the three-child policy) implemented in China. The gridded population was then calculated at the county level by summing the populations in all grid cells within each county.
Assessment of excess deaths
The excess deaths associated with exposure to extreme precipitation events were assessed as follows:
| (2) |
where ED indicates the number of county-level excess deaths resulting from a certain cause; Y is the baseline mortality rate associated with that certain cause (approximately 380 per 100 000 people for accidental mortality, 28 per 100 000 people for circulatory disease, and 47 per 100 000 people for respiratory disease); AF is the risk fraction of a certain cause attributed to extreme precipitation events (AF=(RR−1)/RR, where the 95% CI value of AF was adopted herein); RR is the relative risk; POPi is the yearly county-level population in each period in county i; and Di is the yearly sum of extreme precipitation days in county i.
By applying equation 2, we quantified the cause-specific, extreme precipitation event-related excess deaths across the country during the baseline period of 1986–2005 and in three future periods under combined climate change (RCP2·6, RCP4·5, and RCP8·5) and population (SSP2-S1, SSP2-S2, and SSP2-S3) scenarios. We first separately assessed the excess deaths using the exposure datasets provided by the three GCMs; we then ensembled these results on the basis of different GCMs by averaging the numbers of excess deaths. Both point estimation and their 95% CIs were reported in this study.
To decompose changes in the number of excess deaths in the future compared with the baseline level, we estimated the contributions of two driving factors: climate change and population size. We first estimated the annual average number of excess deaths using the baseline population and number of extreme precipitation days (denoted as EDbaseline); we then projected the excess deaths using the baseline population and future extreme precipitation days derived under three RCPs (denoted as EDclimate); and we further projected the excess deaths under the SSP2-S2 scenario population and future extreme precipitation days under the three analysed RCPs (denoted as EDfuture). We quantified the contribution rate of climate change using (EDclimate − EDbaseline)/(EDfuture − EDbaseline) and quantified that of the population using (EDfuture − EDclimate)/(EDfuture − EDbaseline). We provided these contribution rates nationwide and by five climatic regions, including tropical, subtropical, warm-temperate, middle-temperate, and plateau climate zones.
Role of the funding source
The funders of the study were not involved in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Figure 1A displays the spatial distribution of the 280 analysed counties, indicating the full coverage of the five different climatic regions. We ultimately included 392 305 accidental, 2 499 280 circulatory, and 666 401 respiratory disease deaths (table) during 2013–18, in which 197 896 accidental, 1 104 475 circulatory, and 275 464 respiratory disease deaths occurred in the warm season. 2985 extreme precipitation days were identified on the basis of 99·5th thresholds across 280 counties. All three causes of death were significantly associated with an extreme precipitation event with similar lag patterns (appendix p 8). For accidental mortality, risk increased on the current day of the extreme precipitation exposure and eventually declined from lag1 to lag7; whereas mortality risk for circulatory and respiratory diseases began increasing from lag0 to lag1 and then declined from lag2 to lag7. Compared with the non-extreme precipitation days, exposure to extreme precipitation days is associated with a daily death increase of 13·0% (95% CI 7·0–19·3%; lag0) for accidental cause, 4·3% (2·0–6·6%; lag1) for circulatory disease, and 6·8% (2·8–10·9%; lag1) for respiratory disease. Results of the sensitivity analysis suggested the robustness of the main model (appendix p 1), whereas a decline in both of the effect estimates and significance when changing the time df in the main model indicated that the time trend should be a crucial potential confounder to be controlled. Results (appendix p 6) presented the associations between cause-specific death and extreme precipitation events defined by different thresholds, which indicated the rationale of the main analysis. We also observed higher risk related to the extreme precipitation events with longer duration than that of the 1-day events (appendix p 1). According to the meta-regression results (appendix p 2), we found that the higher proportion of urban residents (level of urbanisation) can be significantly related to the lower effect of accidental mortality associated with extreme precipitation events. We did not observe any strong relationships between the estimated effects and other socioeconomic factors. We found that older people presented a higher risk in all three diseases (appendix p 3). For consistency, we finally applied the highest effect estimation for each cause of death in the projection, namely lag0 for accidental deaths and lag1 for circulatory and respiratory diseases.
Figure 1.
Map of 280 counties (A) and estimation of percentage change in cause-specific mortality associated with exposure to extreme precipitation events (B)
Table.
Summary statistics on the daily deaths and extreme precipitation event days across 280 counties, 2013–18
| Total count |
Daily mean count |
||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Minimum | 25th percentile | 75th percentile | Maximum | ||
| Cause-specific mortality | |||||||
| Accidental cause | 392 305 | 0·8 | 1·1 | 0 | 0 | 1 | 94 |
| Circulatory disease | 2 499 280 | 4·9 | 4·0 | 0 | 2 | 7 | 166 |
| Respiratory disease | 666 401 | 1·3 | 1·7 | 0 | 0 | 2 | 33 |
| Exposure | |||||||
| Extreme precipitation days | 2985 | 0·01 | 0·08 | 0 | 0 | 0 | 1 |
The three GCMs presented generally spatiotemporally consistent future precipitation trends but with some variances in detail. Generally, precipitation tended to rise the most under RCP8·5 and the least under RCP2·6 (appendix p 9); additionally, higher precipitation levels were observed in the subtropical and tropical climate zones under the three RCPs (appendix pp 10–12). However, the precipitation trend simulated by MPI-ESM-MR under RCP2·6 indicates a decrease in the future, and this finding is quite different from the outputs of the other two GCMs. This discrepancy enables us to derive the projection uncertainties sourced from the model simulations. An annual average of 5180 extreme precipitation days were found in the baseline period across China, and this number was predicted to increase to 6947, 7547, and 9015 until the end of this century under RCP2·6, RCP4·5, and RCP8·5, respectively (appendix p 4). Anomalies in the county-level number of extreme precipitation days tended to increase under RCP8·5 in the mid-term and long-term future periods (appendix p 13). The spatial distribution of county-level extreme precipitation days indicated widespread increasing trends across the country (figure 2), especially in the subtropical zone, in the northern region within the middle temperate zone, and in the plateau zone, compared with which fewer extreme precipitation days would be seen in the tropical zone.
Figure 2.
Extreme precipitation days in future periods under different scenarios
RCP= representative concentration pathway. Extreme precipitation days=days with daily total precipitation exceeding the 99·5th threshold.
The annual average number of excess deaths attributed to extreme precipitation days in the baseline period of 1986–2005 was 2644 (95% CI 1496–3730), 69 (33–105), and 181 (79–279) for accidental, circulatory, and respiratory diseases (appendix p 14). Compared with the baseline period, the increases in excess deaths predicted in the near-term period were higher than the increases projected in the mid-term and long-term periods under all RCP–SSP scenarios (figure 3A). The total number for the annual average excess deaths associated with the above 1-day extreme event was higher than the extreme event with longer duration (appendix p 5), which might be due to the higher frequency of 1-day extreme events than those lasting for 2 or more days. Detailed results for three different GCMs to show the model-specific trend are given in the appendix (p 15). In the 2030s, the total number of excess deaths of the three causes will increase by 43%, 61%, and 69% under RCP2·6, RCP4·5, RCP8·5 scenarios combined with a medium-fertility-rate population (SSP2-S2), respectively (figure 3B). In detail, the percentage changes in the numbers of excess deaths predicted under all RCPs and population scenarios exhibited differences. As shown under the RCP2·6–SSP2–S2 scenario, excess deaths of accidental, circulatory, and respiratory diseases are projected to increase by 1136 (643–1603; approximately 43%), 30 (14–45) (approximately 43%), and 78 (34–120; approximately 43%) in the 2030s, but decrease by 401 (227–565), 11 (5–16), and 27 (12–42) in the 2090s under the low-fertility-rate population scenario (SSP2-S1), respectively. In contrast, the total number of excess deaths of these three causes is expected to increase by 9–69% in all future periods under the RCP8·5 scenario. Figure 4 presents the spatial features of the county-level percentage changes in excess deaths: in the near-term period, excess deaths were projected to widely increase in each climatic zone under all three RCPs, and in the long-term period, only the northwest region of the middle-temperate zone, the southern region of Tibet, and the subtropical zone were still expected to face large increases in excess death rates. The statistical distribution of county-level number of excess deaths under different RCP–SSP scenarios based on three GCMs, which indicate a higher possibility of extreme high risk under the RCP8·5 scenario, is shown in the appendix (p 16).
Figure 3.
Projected changes in excess deaths related to extreme precipitation events under combined RCP and population scenarios (A) and percentage changes of excess deaths compared with the baseline of 1986–2005 (B)
Note that scales on y axes differ between plots in panel A. Low, medium, and high=low-fertility-rate, medium-fertility-rate, and high-fertility-rate population scenarios, respectively. RCP=representative concentration pathway.
Figure 4.
Spatial distribution of changes in the total number of excess deaths from accidental, circulatory, and respiratory diseases under RCP-SSP2-S2 scenarios
RCP=representative concentration pathway.
Figure 5 presents the decomposed contributions of the climate and population factors to future changes in excess death rates. Across the whole country, the increase in excess deaths resulting from climate change could offset the reductions resulting from the decreasing populations under RCP2·6 and RCP8·5 in the 2060s and 2090s, leading to net increases in deaths ranging from 16·2% to 56·3%. The excess deaths vary among the climatic zones in response to the positive contribution of climate change, but the negative contribution of population declines, except in the tropical zone, where the increases in excess deaths induced by population changes could offset the reductions in excess deaths due to climate change under the RCP2·6 scenario in the near-term and mid-term periods. Furthermore, despite the declining population trend, the subtropical zone was found to be the only region facing net increases in excess deaths under all scenarios and in all three future periods.
Figure 5.
Contribution rate of climate change and population change to the excess deaths associated with extreme precipitation events under RCP-SSP2-S2 scenarios among the climatic zones
Discussion
In this study, we did an integrated projection of nationwide cause-specific excess deaths related to extreme precipitation events by combining the outputs of multiple GCMs under multiple RCP population scenarios. To the best of our knowledge, this study contains the first reported evidence of the accidental, circulatory, and respiratory diseases deaths burden related to extreme precipitation events. Our projections indicate that extreme precipitation events in China will be exacerbated in the future, based on which the associated deaths burden of accidental, circulatory, and respiratory diseases will be amplified unevenly under the changing climate. The spatiotemporal trends of these increased risks might vary among the five analysed climatic zones, indicating regional differences in the degrees of the population size and climate change contributions.
Our estimations of the increased percentage changes in the mortality risks of accidental, circulatory, and respiratory disease provide evidence that exposure to extreme precipitation events can also drive unignorable effects on non-communicable outcomes. Previous studies have effectively reported on the association between heavy rainfall and infectious diseases, including waterborne and vectorborne diseases,17, 18, 19 and some studies have shown that extreme precipitation can increase overall mortality4, 20 and allergic respiratory morbidity.21, 22 As reported in previous studies, the number of allergic rhinitis outpatients can increase by 7·5% (95% CI 1·8–13·2) during heavy rainfall events.22 We found a consistent 6·8% (2·8–10·9) increase trend in respiratory mortality, and we also observed that the heath effect on respiratory diseases could last from lag0 to lag7. This trend might be explained by the fact that rainwater can increase high concentrations of bioaerosols, such as bacteria, fungus, mold, virus particles, and pollens, thus increasing allergy and respiratory tract issues. The significant increase in respiratory mortality observed on exposure on lag5 to lag7 days might indicate the health effect of bioaerosols concentrations peaking after rainfall events. However, few studies have focused on circulatory disease. We found only one study reporting an extreme precipitation-related increase of 4% in ischaemic stroke hospitalisation obtained by applying a province-level analysis.23 Although these results were not similar to our results, our findings regarding the associations between extreme precipitation and circulatory mortality contribute to the conclusion that these chronic diseases might also be sensitive to extreme precipitation exposure. The possible mechanisms for this correlation might include the following: extreme precipitation events can bring stress to the human body leading to abnormal responses of the cardiopulmonary system and exacerbating the initiation process of acute cardiac events;4 and the disasters can cause heart attacks or cardiac arrests by disrupting medical treatment, such as delayed on-time hospitalisation due to the destruction of facilities and transportation obstacles. With the increasing intensity of extreme precipitation events, the associated health effects on environment-sensitive diseases might arouse more concern, thus requiring additional research to support disease prevention and control when extreme events occur. Our results (appendix p 3) suggest paying special attention to older people who present higher mortality risks and could be vulnerable to extreme precipitation exposure.
We found that extreme precipitation is expected to greatly affect various regions in the near-term and mid-term periods under all three analysed RCPs; additionally, the local daily extreme precipitation series indicates an upward trend that agrees with the findings of previous studies done at the global and national levels.1, 3, 24, 25, 26 The distribution of increased extreme precipitation was found to be uneven across the country, with more extremes concentrated in the northern arid temperate region, in the central-eastern region of the plateau climate zone, and in most regions in the subtropical climate zone. These spatial variations are in accordance with previous studies in the following two aspects. First, despite the precipitation increases predicted in humid regions within the subtropical zone, arid regions in northwest and northeast China are also expected to face increased extreme precipitation days, and this was consistent with the previously reported change trend stating that northwest China has had the largest increase of 9·7% (7·2–12·2) in the number of critically extreme (exceeding the 99th threshold of precipitation) precipitation events27 during the warm season, as well as the highly increasing change observed in the northeast region.25 Second, under high-emission scenarios, more intense extremes are predicted in the plateau climate zone,28 and these higher temperature increases might accelerate precipitation in this area, as was reported in a previous study,25 leading to higher exposure risks in this vulnerable region due to its fragile ecology. As the number of extreme precipitation events is likely to increase by 7% with an additional 1°C global warming (according to the Intergovernmental Panel on Climate Change), the humid and water-limited zones listed above might suffer from high risk24, 29 but low resilience; thus, preparedness for heavy precipitation and subsequent floods should be strengthened in these regions to minimise the public health effects.
Our integrated projections of the numbers of excess deaths resulting from accidental, circulatory, and respiratory diseases provide initial evidence of the future nationwide disease burden associated with extreme precipitation events. According to the only published study in which extreme precipitation-related health risks were reported,9 extreme precipitation-related gastroenteritis emergency visits are expected to increase by a minimum of 1·7 to 1·9 per 100 000 people in MI, USA under a dire climate change scenario. Our study reported that the accidental, circulatory, and respiratory disease excess death rates are expected to increase from 1·99 to 3·44 per 100 000 people in the 2030s under RCP8·5 with a medium-sized population. Although we could not directly compare these estimations, our study emphasises that, in addition to infectious outbreaks, respiratory and circulatory diseases might also be amplified by future extreme precipitation changes. In addition, we estimated 5·8 excess deaths per event-day for respiratory diseases and 2·2 excess deaths per event-day for circulatory diseases during the baseline period. However, previous studies reported 122 cold spell-related excess deaths per event-day for circulatory diseases and 45 for respiratory diseases in 2018,30 as well as 31 heatwave-related excess deaths per event-day of circulatory diseases in 2017 in China.31 Furthermore, in our study, we found that although excess death increases are expected to be widespread across the country in the 2030s under all three RCPs, most of the analysed regions were projected to have large decreases in excess deaths in the 2090s under RCP2·6 (the low-carbon scenario). Therefore, the continuous mitigation of carbon emissions is expected to result in considerable health cobenefits.32
Consistent with the death projection findings obtained for other climatic extremes,7, 33 regions with excess death increases over 75% were found to be basically distributed similarly to those facing more extreme days and densely populated regions. The northwest region of the middle-temperate zone, the southern region of the plateau climate zone, and the densely populated subtropical zone corresponded to the highest excess deaths increases under all scenarios. These regions were identified as high-risk areas. Furthermore, climate change and population development disproportionately affect the exposure and health risks in different regions. Previous studies have reported that population changes might amplify heat-related deaths by 2·3–5·8 times, contributing to trends at the national level. Our results are consistent with previously reported conclusions that the death increases resulting from the changing climate might offset the death declines induced by future population decreases under high-carbon development.33, 34, 35, 36 However, this situation varies among different zones: in tropical regions, which commonly have high rainfall levels, population changes dominate the increased death burden, possibly due to the increased population size and the ageing structure of the region;36 in contrast, in the plateau climate zone, despite the positive contribution of climate change, population changes are expected to continuously induce death burden decreases of almost the same magnitude after the 2030s. In the other three climate zones, climate change was projected to amplify the increased death burdens. Overall, our spatial analysis results might support the identification of priorities for current and future extreme precipitation disaster response planning.
This study represents an initial attempt to project the number of future excess deaths resulting from accidental, circulatory, and respiratory diseases attributed to extreme precipitation events. There are several advantages of this work. First, compared with the little previous research on this topic, this study represents the first reporting of the death burdens of accidental, circulatory, and respiratory diseases attributed to extreme precipitation events rather than infectious diseases. We did these projections on the basis of exposure–response relationships obtained using a large data sample in a time-series analysis. These findings might contribute to the recognition of the potential health effects of extreme precipitation and might guide public health intervention measures to fully cover high-risk populations. Second, we quantified the disease burden by integrating different GCMs, RCPs, and SSPs, thus reducing the projection uncertainties and providing CIs for the future exposure risks and disease burdens. Third, we provided zone-specific analytical results regarding the contributions of climate and population changes in driving the death burden changes with regard to the derived baseline. The high-risk regions and their priority contributors in each period were identified.
Several limitations of this study should also be addressed. First, since we lacked exposure–response relationships specific to each age group, we did not consider the age structure of the population; therefore, we could not provide the disease burden contribution resulting from ageing, which might lead to underestimation of the future deaths burden. Second, we assumed that the mortality rates of the three analysed causes would remain constant across the country in the future due to the lack of region-specific mortality rate predictions, and this assumption might have introduced uncertainty in the resulting numbers of regional future excess deaths. Third, when estimating exposure–response relationships, the counties considered in this study were distributed unevenly, in particular, we did not include enough sites in the western part of China, which might have led to bias in estimating the exposure–response relationship. However, the large sample considered should ensure the statistical power of our results. Fourth, we applied overall estimation of the association between extreme precipitation events and mortality for each county rather than using location-specific estimations. This could bring uncertainty into the evaluation of total number of excess deaths and reduce the spatial diversity of future excess deaths burden. But it can enable us to project the future excess deaths at the national level rather than the 280 counties. Fifth, we cannot take future adaptation into the risk projection because of little evidence on the health effect of adaptation to extreme precipitation under climate change, which might have caused overestimates of excess deaths in this study. Sixth, the effect of socioeconomic status (SES) is also an important factor in estimating health effects and should be considered when comparing the differences between different climatic zones in the changes in excess deaths; however we did not introduce socioeconomic status into our models due to the consideration of reducing possible uncertainties. Further studies should address the effect of the SES factor.
In conclusion, this integrated projection filled the research gap regarding the disease burdens associated with extreme precipitation events in countries with large populations. We provided an improved understanding of the sensitive disease risk imposed by extreme precipitation to accidental, respiratory, and circulatory mortality. The excess deaths attributed to extreme precipitation in the future presented an upward trend over the next three decades; however, low-carbon development could achieve more health benefits in the long term rather than the continuously increasing death burden found under the high-carbon scenario. Climate change mitigation measures and the implementation of better adaptations should play important roles in reducing the disease burden associated with extreme precipitation.
Contributors
Data sharing
Historical daily total precipitation is available from the China Meteorological Data Share Service Center (http://data.cma.cn). Other data will be made available on reasonable request to the corresponding author (litiantian@nieh.chinacdc.cn).
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This research was funded by the National Natural Science Foundation of China (82425051, 82241051) and Wellcome Trust (209734/Z/17/Z).
Editorial note: The Lancet Group takes a neutral position with respect to territorial claims in published maps.
Acknowledgments
TL, WC, and ZL contributed to the study design and coordination. WC, PG, and YLu set up the collaborative work, designed the research framework, and were in charge of supervision. PG, YLu, and TL contributed to study supervision. JB, KL, JH, YLi, XG, YX, YC, CW, YLu, JZ, ZZ, and CZ contributed to data process. JB and KL wrote and revised the manuscript. JB, ZL, WC, JH, and TL contributed to manuscript review and revision. All authors had full access to all the data in the study and accept responsibility to submit for publication. JB, KL, and TL accessed and verified the data.
Supplementary Material
References
- 1.Tabari H. Climate change impact on flood and extreme precipitation increases with water availability. Sci Rep. 2020;10 doi: 10.1038/s41598-020-70816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Meteorological Organization . World Meteorological Organization; Geneva: 2021. WMO atlas of mortality and economic losses from weather, climate and water extremes (1970–2019) (WMO-No. 1267) [Google Scholar]
- 3.Papalexiou SM, Montanari A. Global and regional increase of precipitation extremes under global warming. Water Resour Res. 2019;55:4901–4914. [Google Scholar]
- 4.Yan M, Wilson A, Peel JL, et al. Community-wide mortality rates in Beijing, China, during the July 2012 flood compared with unexposed periods. Epidemiology. 2020;31:319–326. doi: 10.1097/EDE.0000000000001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dorina C, Lifu H, Xiuming W, Shuang C. Fine observation characteristics and thermodynamic mechanisms of extreme heavy rainfall in Henan on 20 July 2021. J Appl Meteorol Sci. 2022;33:1–15. [Google Scholar]
- 6.Zhang S, Ma Z, Li Z, et al. Using CYGNSS Data to map flood inundation during the 2021 extreme precipitation in Henan province, China. Remote Sens (Basel) 2021;13 [Google Scholar]
- 7.Franzke CLE, Torelló i Sentelles H. Risk of extreme high fatalities due to weather and climate hazards and its connection to large-scale climate variability. Clim Change. 2020;162:507–525. [Google Scholar]
- 8.Diaz JH. The influence of global warming on natural disasters and their public health outcomes. Am J Disaster Med. 2007;2:33–42. [PubMed] [Google Scholar]
- 9.Gronlund CJ, Cameron L, Shea C, O'Neill MS. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041-2070. Environ Health. 2019;18:40. doi: 10.1186/s12940-019-0483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J, Xu W, Liao X, Zong S, Liu B. Global mortality risk assessment from river flooding under climate change. Environ Res Lett. 2021;16 [Google Scholar]
- 11.Portier C, Thigpen Tark K, Carter S, et al. Environmental Health Perspectives/National Institute of Environmental Health Sciences; NC: 2010. A human health perspective on climate change: a report outlining the research needs on the human health effects of climate change. [Google Scholar]
- 12.Gao X, Wu J, Shi Y, et al. Future changes in thermal comfort conditions over China based on multi-RegCM4 simulations. Atmos Oceanic Sci Lett. 2018;11:291–299. [Google Scholar]
- 13.Gudmundsson L, Bremnes JB, Haugen JE, Engen-Skaugen T. Technical note: downscaling RCM precipitation to the station scale using quantile mapping: a comparison of methods. Hydrol Earth Syst Sci. 2012;9:6185–6201. [Google Scholar]
- 14.Hempel S, Frieler K, Warszawski L, Schewe J, Piontek F. A trend-preserving bias correction – the ISI-MIP approach. Earth Syst Dyn. 2013;4:219–236. [Google Scholar]
- 15.Watts N, Adger WN, Agnolucci P, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Guo F, Wang J, Cai W, Wang C, Wang K. Provincial and gridded population projection for China under shared socioeconomic pathways from 2010 to 2100. Sci Data. 2020;7:83. doi: 10.1038/s41597-020-0421-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlton EJ, Eisenberg JNS, Goldstick J, Cevallos W, Trostle J, Levy K. Heavy rainfall events and diarrhea incidence: the role of social and environmental factors. Am J Epidemiol. 2014;179:344–352. doi: 10.1093/aje/kwt279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mertens A, Balakrishnan K, Ramaswamy P, et al. Associations between high temperature, heavy rainfall, and diarrhea among young children in rural Tamil Nadu, India: a prospective cohort study. Environ Health Perspect. 2019;127 doi: 10.1289/EHP3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drayna P, McLellan SL, Simpson P, Li S-H, Gorelick MH. Association between rainfall and pediatric emergency department visits for acute gastrointestinal illness. Environ Health Perspect. 2010;118:1439–1443. doi: 10.1289/ehp.0901671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ingole V, Juvekar S, Muralidharan V, Sambhudas S, Rocklöv J. The short-term association of temperature and rainfall with mortality in Vadu Health and Demographic Surveillance System: a population level time series analysis. Glob Health Action. 2012;5:44–52. doi: 10.3402/gha.v5i0.19118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park KJ, Moon JY, Ha JS, et al. Impacts of heavy rain and typhoon on allergic disease. Osong Public Health Res Perspect. 2013;4:140–145. doi: 10.1016/j.phrp.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D'Amato G, Cecchi L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin Exp Allergy. 2008;38:1264–1274. doi: 10.1111/j.1365-2222.2008.03033.x. [DOI] [PubMed] [Google Scholar]
- 23.Tang C, Liu X, He Y, et al. Association between extreme precipitation and ischemic stroke in Hefei, China: hospitalization risk and disease burden. Sci Total Environ. 2020;732 doi: 10.1016/j.scitotenv.2020.139272. [DOI] [PubMed] [Google Scholar]
- 24.Donat MG, Lowry AL, Alexander LV, O'Gorman PA, Maher N. More extreme precipitation in the world's dry and wet regions. Nat Clim Chang. 2016;6:508–513. [Google Scholar]
- 25.Chong-Hai X, Ying X. The projection of temperature and precipitation over China under RCP Scenarios using a CMIP5 multi-model ensemble. Atmos Ocean Sci Lett. 2012;5:527–533. [Google Scholar]
- 26.Sun Q, Zhang X, Zwiers F, Westra S, Alexander LVA. Global, continental, and regional analysis of changes in extreme precipitation. J Clim. 2021;34:243–258. [Google Scholar]
- 27.Chang M, Liu B, Martinez-Villalobos C, Ren G, Li S, Zhou T. Changes in extreme precipitation accumulations during the warm season over continental China. J Clim. 2020;33:10799–10811. [Google Scholar]
- 28.Khadgarai S, Kumar V, Pradhan PK. The connection between extreme precipitation variability over monsoon Asia and large-scale circulation patterns. Atmosphere (Basel) 2021;12 [Google Scholar]
- 29.Donat MG, Angélil O, Ukkola AM. Intensification of precipitation extremes in the world's humid and water-limited regions. Environ Res Lett. 2019;14 [Google Scholar]
- 30.Sun Q, Sun Z, Chen C, et al. Health risks and economic losses from cold spells in China. Sci Total Environ. 2022;821 doi: 10.1016/j.scitotenv.2022.153478. [DOI] [PubMed] [Google Scholar]
- 31.Yan M, Xie Y, Zhu H, Ban J, Gong J, Li T. Cardiovascular mortality risks during the 2017 exceptional heatwaves in China. Environ Int. 2023;172 doi: 10.1016/j.envint.2023.107767. [DOI] [PubMed] [Google Scholar]
- 32.Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang J, Zhou M, Ren Z, et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat Commun. 2021;12 doi: 10.1038/s41467-021-21305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen K, Fiore AM, Chen R, et al. Future ozone-related acute excess mortality under climate and population change scenarios in China: a modeling study. PLoS Med. 2018;15 doi: 10.1371/journal.pmed.1002598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones B, O'Neill BC, McDaniel L, McGinnis S, Mearns LO, Tebaldi C. Future population exposure to US heat extremes. Nat Clim Chang. 2015;5:652–655. [Google Scholar]
- 36.Li T, Horton RM, Bader DA, et al. Aging will amplify the heat-related mortality risk under a changing climate: projection for the elderly in Beijing, China. Sci Rep. 2016;6 doi: 10.1038/srep28161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Historical daily total precipitation is available from the China Meteorological Data Share Service Center (http://data.cma.cn). Other data will be made available on reasonable request to the corresponding author (litiantian@nieh.chinacdc.cn).