Abstract
Advantages of the low transverse Pfannenstiel incision include lower rates of incisional hernia, wound infection, hematoma formation, direct postoperative pain and distinctly improved aesthetic appearance. Relative disadvantages include insufficient intraoperative exposure of the upper abdomen and an increased incidence of superficial nerve entrapment. Incisional hernia following Pfannenstiel incision is a rare event with a reported incidence of between 0 and 0.5% while in contrast midline vertical incisions are considerably more common with a reported incidence of 5 to 30%. Symptomatology of Pfannenstiel incisional hernia has been reported to include: bulging, pain or discomfort, and distention of the surgical area. We report an unusual case of early postpartum unilateral vulvar edema, which led to imaging diagnosis of Pfannenstiel incisional hernia in a 41 year-old woman on Day 2 following Cesarean delivery due to preeclampsia with worsening severe features, at 30 weeks’ gestation.
Keywords: Cesarean delivery, Pffanenstiel incision, Postpartum, Incisional hernia, Computed tomography, Vulvar edema
Introduction
Advantages of the low transverse Pfannenstiel incision include lower rates of incisional hernia, wound infection, hematoma formation, direct postoperative pain and distinctly improved aesthetic appearance [[1], [2], [3]]. Relative disadvantages include insufficient intraoperative exposure of the upper abdomen and an increased incidence of superficial nerve entrapment [1]. Nerve entrapment may result from incision of the nerve followed by neuroma formation, incorporation of the nerve by a suture during closure of the fascia, or tethering or constriction of the nerve (resulting in iliohypogastric and/or ilioinguinal neuralgia in surrounding postoperative scar tissue) [1].
Incisional hernia following Pfannenstiel incision is a rare event with a reported incidence of between 0% and 0.5%, while in contrast midline vertical incisional hernias are considerably more common with a reported incidence of 5% to 30% [[3], [4], [5], [6]]. Symptomatology of Pfannenstiel incisional hernia has been reported to include: bulging, pain or discomfort, and distention of the surgical area [3]. We report an unusual case in which early postpartum unilateral vulvar edema led to the diagnosis of Pfannenstiel incisional hernia in a 41 year-old woman on postoperative Day 2, following Cesarean delivery due to preeclampsia with worsening severe features, at 30 weeks’ gestation.
Case report
A 41 year-old P4 (with 4 previous spontaneous vaginal births of appropriate for gestational age neonates) late registrant for prenatal care was seen for her initial prenatal visit at 28 and 5/7 weeks’ gestation. She reported previous uncomplicated cosmetic breast surgery and abdominoplasty. Her current BMI was 38. Following notation of elevated blood pressure of 190/96 mmHg in association with a headache, she was admitted for evaluation and management of preeclampsia with severe manifestations. Intravenous antihypertensive medications (Labetalol 20 mg followed by separate increasing doses of 40 and 80 mg, respectively) were administered. She received IV Magnesium sulfate for seizure prophylaxis and IM antenatal corticosteroids to decrease prematurity-associated neonatal morbidities, should preterm delivery become indicated. Laboratory tests indicated: Hemoglobin = 10.7 gr%, hematocrit = 32%, and serum electrolytes, glucose, BUN, creatinine, albumin, liver function tests (AST/ALT), platelets, fibrinogen, and PT/PTT, which were all within normal limits. A 24 hour proteinuria = 418 mg. Ultrasound assessment disclosed a singleton fetus with reassuring fetal testing (BPP 10/10). Sonographic estimated fetal weight = 980 grams (12th centile for gestational age) and abdominal circumference (AC) = sixth centile for gestational age. Umbilical artery systolic diastolic ratio (S/D)= 2.6 (within normal limits).
Given the premature gestational age, in an attempt to prolong the pregnancy, oral antihypertensive medication (Procardia 30 mg XL/day) was initiated. Subsequent blood pressure measurements ranged between 130-150 / 70-90 mmHg. With the continued stable maternal condition and reassuring fetal status, and unless indicated earlier (for any worsening maternal or fetal condition), delivery was planned for 34 weeks’ gestation.
On hospital day #10, at 30 weeks’ gestation serum AST and ALT values increased to > 3 times the normal values, and with the diagnosis of preeclampsia now with worsening severe features, delivery was decided upon following completion of rescue IM antenatal corticosteroids, and IV magnesium sulfate for fetal neuroprotection. Due to an unstable fetal lie, primary Cesarean delivery was performed under spinal anesthesia through a Pfannenstiel incision. A male infant was delivered atraumatically (“en caul”) through a low transverse uterine incision. Birth weight = 1150 grams, Apgar scores were 4, and 8 at 1 and 5 minutes, respectively. Umbilical artery pH = 7.21, and base excess = -8.3. The infant was admitted to the neonatal intensive care unit (NICU) and received intratracheal surfactant, and CPAP. The surgical procedure was considered uneventful. Fascia was closed in a continuous 0 Vicryl suture, and quantified blood loss (QBL) = 800 mL.
The patient's immediate postoperative course was uneventful. IV Magnesium Sulfate for seizure prophylaxis was continued for 24 hours. On postoperative Day 1, she complained of increasing left vulvar pain and swelling. On examination, her abdomen was soft, nontender, nondistended with a normal-appearing incision. Despite placement of an ice pack, the patient continued to complain of worsening left vulvar tenderness and swelling. Unilateral swelling of the left labia majora, measuring approximately 4-8 cm in size was noted. Computed tomography with intravenous contrast depicted a lower abdominal ventral wall defect (rectus sheath dehiscence and fascia defect) with herniation of loops of small bowel and mesentery extending into the soft tissues of the inferior mons pubis, with marked edema of the left labia majora (Fig. 1, Fig. 2, Fig. 3). No signs of bowel strangulation or bowel obstruction were noted. General surgery was consulted and confirmed the need for surgical intervention.
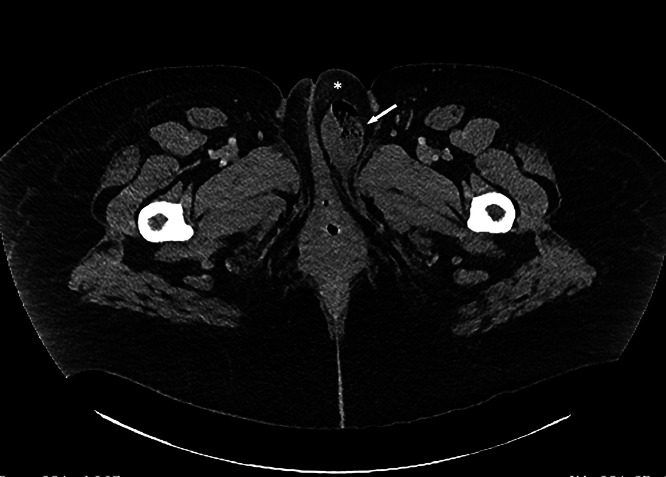
Fig. 1.
Axial CT scan with intravenous (IV) contrast demonstrates unilateral left vulvar edema with asterisk (*), containing loops of small bowel (arrow), displacing the midline.
Fig. 2.
CT Scan with IV contrast, coronal reconstruction. Note loops of small bowel (b) and mesentery (m) herniating through fascia defect, located within enlarged edematous left vulva marked with asterisk (*). Note displacement of the midline.
Fig. 3.
CT scan with IV contrast, sagittal reconstruction. Note the bowel (b) and mesentery (m) herniated through the fascia defect (arrow).
Incisional hernia was confirmed at exploratory laparotomy, with a 2 cm fascial defect on the left medial aspect of the prior fascia closure with omentum clearly herniating through the rectus sheath and fascia defect (replacing the previous herniating small bowel and mesentery) Resection of a 12.5 × 6 cm segment of herniated omentum and repair of the prior fascia incision, were performed. The patient's unilateral left vulvar edema and associated symptomatology abated following the corrective surgery and she was discharged on postoperative Day #2 in good general health. Pathology of the resected tissue confirmed tan-yellow fibro-fatty tissue, consistent with omentum with acute surface inflammation.
Discussion
Possible causes of vulvar edema include pregnancy, preeclampsia, nephrotic syndrome, cellulitis, bacterial vaginosis, sexually transmitted diseases (including but not limited to filariasis), allergies, drug toxicity (Methotrexate, tocolysis), physical irritation, surgical and nonsurgical trauma, ascites, cancer, inguinal hernia, ovarian hyperstimulation and Crohn's disease [[7], [8], [9], [10], [11], [12], [13], [14], [15], [16]]. Rare reported miscellaneous conditions reported in association with vulvar edema include: rhabdomyolysis, obesity with prolonged immobility, and septic pubic symphysitis complicating pregnancy [[17], [18], [19]].
It appears that while the relatively dependent vulvar tissue may become distended during pregnancy with excessive fluid such as in cases of hypoalbuminemia (preeclampsia or nephrotic syndrome), in our case the unilateral distention and associated marked edema resulted from the presence of displaced herniated small bowel and mesentery (as depicted in Fig. 1, Fig. 2, Fig. 3), with rapid resolution of the associated vulvar edema following corrective surgical repair of the incisional hernia.
Systematic review of the English literature (PubMed, Google Scholar, and Medline, 1966-2024) using the search terms “Cesarean delivery”, “Pfannenstiel incision”, and “vulvar edema”, confirm that vulvar edema leading to the diagnosis of Pfannenstiel incisional hernia has not been reported previously.
This care demonstrates that although rare, Pfannenstiel incisional hernia should be considered in the differential diagnosis of immediate post Cesarean delivery unilateral vulvar edema.
Patient consent
We have obtained our patient's informed consent for publishing our case report entitled: Early postpartum unilateral vulvar edema leading to diagnosis of a Pfannenstiel incisional hernia following cesarean delivery.
Footnotes
Competing Interests: The authors acknowledge that we have no competing interests to report regarding our case report entitled: Early postpartum unilateral vulvar edema leading to diagnosis of a pfannenstiel incisional hernia following cesarean delivery.
References
- 1.Luijendijk RW, Jeekle J, Stirm RK, Schutte PJ, Hop WC, Drogendijk AC, et al. The low transverse Pfannenstiel incision and the prevalence of inscional hernia and nerve entrapment. Ann Surg. 1997;225(4):365–369. doi: 10.1097/00000658-199704000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loos MJA, Scheltinga MRM, Roumen RMH. Surgical management of ingiunal neuralgia after a low transverse Pfannenstiel incision. Ann Surg. 2008;248(5):880–885. doi: 10.1097/SLA.Ob013e318185da2e. [DOI] [PubMed] [Google Scholar]
- 3.Sakoglu N, Firat A. Risk factors for Pfannenstiel incisional hernia following Cesarean delivery and outcomes after laparoscopic and open surgical repair. Clin Exp Obstet Gynecol. 2024;51(3):62. doi: 10.31083/j.ceog5103062. [DOI] [Google Scholar]
- 4.Paulsen CB, Zetner D, Rosenberg J. Incisional hernia after cesarean section: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2020;244:128–133. doi: 10.1016/j.ejogrb.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Shand AW, Chen JS, Schnitzler M, Roberts CL. Incisional hernia repair after caesarean section: a population-based study. Aust NZ J Obstet Gynaecol. 2015;55(2):170–175. doi: 10.1111/ajo.12270. [DOI] [PubMed] [Google Scholar]
- 6.Larkin JO, Awan FN, McArdle AC, McCormick PH. Mehigan. Partial herniation through the peritoneal defect of a pfannenstiel incision: a rare complication of non-closure. J Obstet Gynaecol Can. 2011;33(6):625–627. doi: 10.1016/S1701-2163(16)34912-X. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez Cervantes BY, Almager Acevedo F, Martinez Lopez D, Guzman Lambert R, Rodriguez M. Our first Pfannenstiel incisional hernia: a case report. J Surg Case Rep. 2022;2022(11):rajc546. doi: 10.1093/jscr/rjac546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amankwah Y, Haefner H. Vulvar edema. Dermatol Clin. 2010;28(4):765–777. doi: 10.1016/j.det.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Kiram H, Bouab M, Jalal M, Lamrissi A, Bouhya S. Massive vulvar edema during pregnancy: a case report. Int J Surg Case Rep. 2022;99 doi: 10.1016/j.jscr.2022.107674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daporite A, Skentou H, Dimopoulos KD, Kallitsaris A, Messinis I. Massive vulvar edema in a woman with preeclampsia: a case report. J Reprod Med. 2007;52(11):1067–1069. [PubMed] [Google Scholar]
- 11.Cantero MG, Valtuena J, Ruiz-Sànchez D, López PM, Pérez-Bustillo A. Vulvar edema: diagnostic clue to Crohn's disease. Dematol Online J. 2021;27(2) [PubMed] [Google Scholar]
- 12.Jia G, Chai WC, Liu X, Cui YW, Gong F. Low-dose methotrexate-induced vulvar edema: a case report. Medicine (Baltimore) 2019;98(35):e16895. doi: 10.1097/MD0000000000016895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trive L, Bennert H, Stubblefield PG. Massive vulvar edema complicating tocolysis in patient with twins. J Rerod Med. 1996;41(2):121–124. [PubMed] [Google Scholar]
- 14.Padoe G, Vavilis D, Pantazis K, Agorastos T, Bontis J. Unilateral vulvar edema after operative laparoscopy: a case report and literature review. Fertil Steril. 2005;83(2):471–473. doi: 10.1016/j.fertnstert.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 15.Zuccaro B, Perillo G, De Giorgi V. Massive vulvar edema: a sign of nephrotic syndrome. Am J Med. 2024;137(7):595–596. doi: 10.1016/j.amjmed.2024.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Nelson EL, Parker AN, Dudley DJ. Spontaneous vulvar hematoma during pregnancy: a case report. J Reprod Med. 2012;57(1-2):74–76. [PubMed] [Google Scholar]
- 17.Khamsi N, Menez MD, Rojas-Mendez P, Sanchez S, Reddy S. Unilateral labial edema in a female adolescent: a gynecologic presentation of rhabdomyolysis. L Pediatr Adolesc Gynecol. 2018;31(6):644–647. doi: 10.1016/j.jpag.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 18.McCluggage WG, Nielsen GP, Young RH. Massive vulval edema secondary to obesity and immobilization: a potential mimic of aggressive angiomyxoma. Int J Gynecol Pathol. 2008;27(3):447–452. doi: 10.1097/PGP.Ob013e31816017a7. [DOI] [PubMed] [Google Scholar]
- 19.Lawford AM, Scott K, Lust K. A case of massive vulvar oedema due to septic pubic symphysitis complicating pregnancy. Aust NZ J Obstet Gynecol. 2010;50(6):576–577. doi: 10.1111/j.1479-828X.2010.01227.x. [DOI] [PubMed] [Google Scholar]