Abstract
Angiomyolipomas are benign mesenchymal lesions often diagnosed incidentally, composed of adipose tissue, dysmorphic blood vessels, and smooth muscle. They are usually unilateral and symptomatic only when larger than 4 centimeters, posing a risk of spontaneous rupture and severe retroperitoneal hemorrhage. Treatment varies from conservative management to selective embolization or nephrectomy, depending on tumor size and patient condition. This case report describes a 26-year-old female with a giant renal angiomyolipoma treated with angioembolization, who subsequently developed postembolization syndrome.
Keywords: Angiomyolipoma, Therapeutic embolization, Necrosis, Inflammation
Introduction
Angiomyolipomas are benign mesenchymal lesions composed of mature adipose tissue, dysmorphic blood vessels, and smooth muscle. Initially classified as hamartomas, these lesions are now considered part of the perivascular epithelioid cell neoplasm (PEComa) group due to the presence of ectopic tissue within the affected organ [1].
Isolated presentations are usually unilateral and typically appear in the fourth decade of life, representing 80% of cases. The remaining 20% are associated with genetic syndromes, such as lymphangioleiomyomatosis and tuberous sclerosis [2].
Tumors larger than 4 centimeters often become symptomatic and carry a higher risk of spontaneous rupture, leading to severe retroperitoneal hemorrhage, which can be life-threatening without prompt medical care [3]. The therapeutic approach varies based on the tumor's size, morphological characteristics, and the patient's clinical presentation, ranging from conservative management to selective embolization or nephrectomy [4].
Embolization therapy, while effective, can result in complications, such as postembolization syndrome. Although not fully elucidated, this syndrome is thought to arise from an inflammatory response to necrotic tissue postembolization, manifesting clinically as severe pain and fever [5].
In this case report, we present a patient with a giant renal angiomyolipoma who underwent selective angioembolization and subsequently developed postembolization syndrome. This manuscript was reviewed and approved (Approval letter No. 378-2024) by the Institutional Ethics Committee, and informed consent was obtained from the patient.
Clinical case
A 26-year-old female patient with a history of hypertriglyceridemia consulted to the urology department in July 2022 after an upper abdominal ultrasound incidentally revealed an angiomyolipoma measuring approximately 18.5 centimeters. Subsequent nuclear magnetic resonance imaging (MRI) of the abdomen confirmed the diagnosis, reporting a mass measuring 7.2 × 6.5 × 17.7 cm in the left kidney (Fig. 1).
Fig. 1.
Nuclear magnetic resonance of the abdomen. Mass dependent on the cortex of the middle third and lower pole of the left kidney with exophytic growth and intralesional fat, suggestive of an angiomyolipoma measuring 7.2 × 6.5 × 17.7 cm (AP x T x L).
The patient denied irritative or obstructive urinary symptoms, weight loss, or hematuria. Due to the tumor's size, she was considered a candidate for angioembolization and was referred to the interventional radiology department. Using a right femoral approach guided by ultrasound, a left renal arteriography was performed, revealing a large superolateral renal tumor with 3 major arterial afferences: 2 superior and one from the lower interpolar region. These vessels were embolized with 355-500 nonspherical polyvinyl alcohol (PVA) microparticles, and 1 tortuous, dilated superior artery was additionally treated with metallic coils. Approximately 80% of the tumor mass was successfully embolized. The procedure was completed without complications.
Following the procedure, the patient developed epigastric and right hypochondrial pain, associated with leukocytosis, elevated C-reactive protein, tachycardia, and intermittent febrile episodes (temperatures greater than 38°C). Blood and urine cultures were taken due to suspicion of infection, but the results were negative. Empirical antibiotic treatment with Ceftriaxone was initiated. An abdominal ultrasound was performed, which reported changes consistent with postangioembolization necrosis and left pleural effusion associated with basal atelectasis. Analgesic medication was prescribed for pain management.
Due to persistent abdominal pain, the general surgery team evaluated the patient and ordered a computed tomography (CT) scan of the abdomen, which revealed thickened gallbladder walls without stones consistent with acalculous cholecystitis secondary to systemic inflammation. A laparoscopic cholecystectomy was performed to prevent gallbladder rupture, with pathology confirming chronic cholecystitis. The procedure was completed without complications, and pathology confirmed chronic cholecystitis.
The patient was admitted to the intensive care unit (ICU) for postoperative care, where she continued to experience severe pain, leukocytosis, and intermittent fever persisted. An infectious disease specialist determined that the clinical presentation was likely inflammatory rather than infectious, secondary to angiomyolipoma necrosis; thus, antibiotic treatment was discontinued.
The patient then experienced an episode of dyspnea with desaturation and mixed acidosis on arterial blood gases. An initial Angio CT scan ruled out pulmonary thromboembolism. Due to persistent symptoms and abnormal laboratory results, a ventilation/perfusion scan was requested, which indicated abnormal perfusion compatible with subsegmental pulmonary thromboembolism of the upper segment of the left lower lobe; anticoagulation therapy was initiated. Days later, the patient showed clinical improvement and a decrease in acute phase reactants, leading to her discharge.
Since discharge, the patient has been asymptomatic and is monitored with biannual MRIs. The most recent MRI showed a tumor size of 15 × 6.3 × 4.9 cm, reflecting a reduction of approximately 1 centimeter in all dimensions (Fig. 2, Fig. 3).
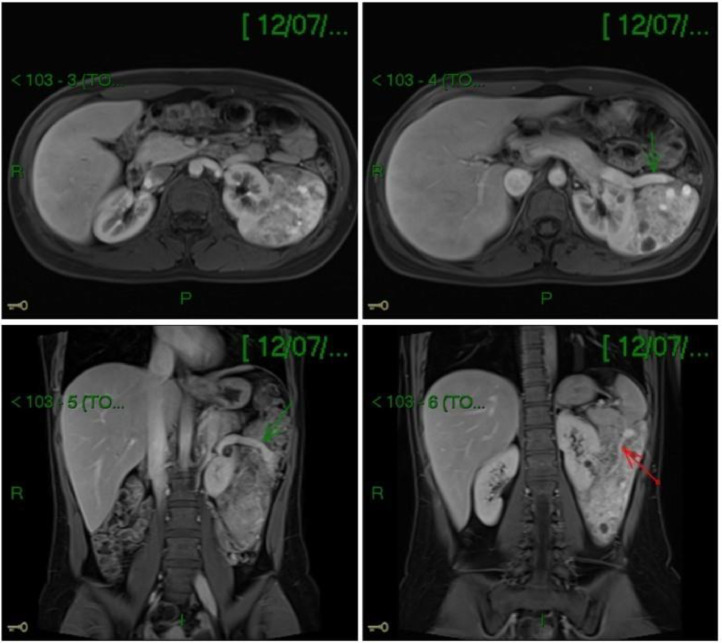
Fig. 2.

Magnetic nuclear resonance of the urinary tract at the first medical follow-up. A pedunculated, exophytic mass dependent on the posterior wall of the left kidney persists, measuring 6.3 × 4.9 × 15 cm (AP × T × L).
Fig. 3.
Magnetic resonance of the abdomen at the second medical follow-up. A mass dependent on the left kidney persists, occupying the left perirenal space, with areas of internal hypointensity related to a history of embolization, measuring 6.5 × 5 × 14.9 cm (AP × T × L).
In February 2024, the patient had an ambulatory consultation with clinical genetics for molecular studies. These studies revealed a variation in the number of copies of the heterozygotic state, gain type, involving exons 4-14 of the FLCN gene, classified as a variant of uncertain significance. This variant has been reported as pathogenic, necessitating a confirmatory Multiplex Ligation dependent Probe Amplification (MLPA) test. If confirmed, it can be considered a hereditary cancer syndrome due to an FLCN mutation.
Discussion
Renal angiomyolipomas, first described in 1951, are considered benign mesenchymal neoplasms originating from adipose tissue, smooth muscle, and dysmorphic blood vessels. Due to their size, particularly those larger than 4 centimeters, there is a significant risk of compressing adjacent structures. The presence of vascular aneurysms, which are thin-walled vessels, necessitates prophylactic or therapeutic arterial embolization due to the elevated risk of rupture and bleeding.
Sporadic angiomyolipomas tend to appear in the fourth decade of life and are typically unilateral, unlike those associated with genetic disorders such as tuberous sclerosis complex and sporadic pulmonary lymphangioleiomyomatosis, which are usually bilateral. These tumors occur mainly in women, with an incidence of 0.3%-3%. Most cases are asymptomatic, leading to incidental diagnosis, except in tumors larger than 4 centimeters, where clinical manifestations such as abdominal pain, a palpable mass, and hematuria may be present. Additionally, hemorrhage can be precipitated by minor trauma or pregnancy; long-term subcapsular hemorrhage could cause chronic ischemic nephropathy due to renal compression. Few cases refer to giant renal angiomyolipomas, defined as those exceeding 10 centimeters, as demonstrated in this case [6].
Therapeutic options include clinical surveillance, selective arterial embolization, ablative therapies, and surgery. The goal of treatment is to avoid complications and preserve kidney function. These therapies are indicated when growth is evident during follow-ups (> 0.25 cm/year), persistent symptoms (intractable pain, hematuria), suspicion of malignancy, risk of retroperitoneal hemorrhage (e.g., women of childbearing age), and a tumor size greater than 4 centimeters [7].
Selective arterial embolization is a minimally invasive treatment that has demonstrated a reduction in tumor size with few complications. However, among its complications is the postembolization syndrome. Its symptoms can develop from 12 hours after the procedure for a period of 2-7 days and present as fever, abdominal pain, nausea, emesis, and general malaise. This syndrome has not been completely defined, but existing theories support that it is secondary to an inflammatory response due to embolized necrotic tissue. It can range from mild clinical manifestations requiring only symptomatic treatment to severe symptoms. Some articles describe that the magnitude of the clinical presentation can be directly related to the size of the treated lesion [8]. In this case, the patient experienced difficult-to-manage pain, nausea, febrile episodes, and reactive pleural effusion, requiring admission to the Intensive Care Unit for clinical surveillance.
Wang et al. reported on 79 patients who underwent transarterial embolization for renal angiomyolipoma, noting that 86% developed postembolization syndrome. However, most patients with mild symptoms recovered with conservative management [9]. Some studies have also included therapy with nonsteroidal anti-inflammatory drugs combined with a proton-pump inhibitor and an analgesic to reduce the symptoms of postembolization syndrome [10]. This indicates that postembolization syndrome is a common complication, and recognizing it promptly can help reduce associated morbidity. While most cases involve mild symptoms, healthcare professionals must be prepared to manage cases that progress to moderate or severe symptoms.
Based on the hypothesis that postembolization syndrome is caused by a systemic inflammatory response triggered by necrotic tissue after embolization—through the release of degradation products, interleukin-6, tumor necrosis factor, and vasoactive substances— [11], different studies have suggested the potential effectiveness of steroids as a prophylactic measure to reduce the incidence, severity, and duration of postembolization syndrome [5,12].
The development of acalculous cholecystitis in this patient may also be linked to the systemic inflammatory response induced by postembolization syndrome. Theories on acalculous cholecystitis pathogenesis include biliary stasis, sepsis, and ischemia of the gallbladder wall. In critically ill patients, hypotension and hypovolemia may lead to ischemia, while the release of pro-inflammatory mediators can exert inflammatory effects on the gallbladder [13].
Conclusion
Renal angiomyolipoma is a rare tumor often diagnosed incidentally due to its asymptomatic nature, small size, and minimal impact on clinical status. However, larger tumors can present with symptoms such as abdominal pain, hematuria, or a palpable mass, and may be at risk for rupture, potentially leading to retroperitoneal hemorrhage and life-threatening hemodynamic instability.
In these cases, minimally invasive techniques such as selective angioembolization are used. However, it is essential to be aware of the risks and complications associated with these techniques—such as postembolization syndrome—through preventive measures and optimal, prompt diagnosis and treatment, to effectively manage negative outcomes in patients.
Patient consent
Written, informed consent for the publication of this case report was obtained from the patient. The patient provided explicit permission for the use of their medical information and case details in this report, ensuring that their privacy and confidentiality are maintained.
CRediT authorship contribution statement
Sebastián Romero-Fernández: Methodology, Investigation, Visualization, Writing – original draft, Writing – review & editing. Valeria García-Ramos: Investigation, Writing – original draft, Writing – review & editing. Valentina García: Investigation, Writing – review & editing. Myriam Lili Ceballos: Investigation, Writing – review & editing, Supervision, Project administration.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: To the Clinical Research Center of the institution for its constant technical and scientific support.
Funding sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Lienert AR, Nicol D. Renal angiomyolipoma. BJU Int. 2012;110(4):25–27. doi: 10.1111/j.1464-410X.2012.11618.x. [DOI] [PubMed] [Google Scholar]
- 2.Rivero Rodríguez WR, Pradilla Valbuena JE, Orozco Levi M. Angiomiolipoma renal gigante y linfangioleiomiomatosis pulmonar esporádica no filiada. A propósito de un caso. Urol Colomb [Internet] 2014;23(3):227–232. www.elsevier.es/uroco Available from: [Google Scholar]
- 3.Rueda L, Torres P, Ballestas C, Segovia J, González A. Angiomiolipoma renal con rotura espontánea (síndrome de wünderlich): presentación de un caso. Revista Colombiana de Radiología. 2015;26(3):4279–4282. [Google Scholar]
- 4.Murad Gutiérrez V, Aponte Barrios WO, Romero Enciso JA. Angiomiolipoma renal: nuevas perspectivas. Vol. 25, Urologia Colombiana. Elsevier Doyma; 2016. p. 16–24.
- 5.Bissler JJ, Racadio J, Donnelly LF, Johnson ND. Reduction of postembolization syndrome after ablation of renal angiomyolipoma. Am J Kidney Dis. 2002;39(5):966–971. doi: 10.1053/ajkd.2002.32770. [DOI] [PubMed] [Google Scholar]
- 6.Razik A, Das CJ, Sharma S. Angiomyolipoma of the kidneys: current perspectives and challenges in diagnostic imaging and image-guided therapy. Curr Problems Diagn Radiol. Mosby Inc. 2019;48:251–261. doi: 10.1067/j.cpradiol.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Álvarez Restrepo JC, Castañeda Millan DA, Riveros Sabogal CA, Puentes Bernal AF, Donoso Donoso W. New Trends and evidence for the management of renal angiomyolipoma. J Kidney Cancer VHL. 2022;9(1):33–41. doi: 10.15586/jkcvhl.v9i1.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nozadze G, Larsen SB, Heerwagen S, Juhl Jensen R, Lönn L, Røder MA. Selective arterial embolization of renal angiomyolipomas: a 10-year experience. BJUI Compass. 2022;3(1):86–92. doi: 10.1002/bco2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C, Yang M, Tong X, Wang J, Guan H, Niu G, et al. Transarterial embolization for renal angiomyolipomas: a single centre experience in 79 patients. J Int Med Res. 2017;45(2):706–713. doi: 10.1177/0300060516684251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rolland R, Loubet A, Bommart S, Monnin-Bares V, Zarqane H, Vanoverschelde J, et al. Safety, efficacy and mid-term outcome for transarterial embolization (TAE) of renal angiomyolipoma (AML) using ethylene vinyl alcohol copolymer liquid embolic agent (EVOH) J Clin Med. 2023;12(10):1–15. doi: 10.3390/jcm12103385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Svarc P, Taudorf M, Nielsen MB, Stroomberg HV, Røder MA, Lönn L. Postembolization syndrome after prostatic artery embolization: a systematic review. Diagnostics. 2020;10(9):1–16. doi: 10.3390/diagnostics10090659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsuchiya S, Saiga A, Yokota H, Kubota Y, Wada T, Akutsu A, et al. Prophylactic steroids for preventing postembolization syndrome after transcatheter arterial embolization of renal angiomyolipoma: a comparative study. Intervention Radiol. 2023;8(1):1–6. doi: 10.22575/interventionalradiology.2021-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mossaab G, Ben Khlifa M, Karim N, Moez B, Oussama J, Hajer N, et al. Acute acalculous cholecystitis in hospitalized patients in intensive care unit: study of 5 cases. Heliyon. 2022;8(11) doi: 10.1016/j.heliyon.2022.e11524. [DOI] [PMC free article] [PubMed] [Google Scholar]