Abstract
Introduction and significance
Hepatopulmonary fusion is a rare congenital malformation associated with right-sided diaphragmatic hernia. Often diagnosed during surgery, it carries a high mortality rate.
Case presentation
We present a case of a full-term infant who exhibited shortness of breath from birth. Radiological examinations confirmed a right congenital diaphragmatic hernia, and subsequent surgery revealed hepatopulmonary fusion.
Clinical discussion
While hepatopulmonary fusion is uncommon, it should be considered in the differential diagnosis of right-sided congenital diaphragmatic hernia (CDH). Preoperative evaluation for vascular malformations and meticulous surgical planning are essential.
Conclusion
Managing hepatopulmonary fusion poses significant challenges for surgeons. Its association with pulmonary malformations increases surgical complexity, risk, and adversely impacts prognosis, as exemplified in our case.
Keywords: Case report, Hepatopulmonary, Fusion, Pulmonary hypoplasia, Bochdalek
Highlights
-
•
Hepatopulmonary fusion associated with right congenital diaphragmatic hernia is a rare malformation.
-
•
The majority of hepatopulmonary fusion cases are incidentally discovered during surgical repair of right congenital diaphragmatic hernia.
-
•
Associated vascular abnormalities increase surgical risk.
-
•
Hepatopulmonary fusion associated with right congenital diaphragmatic hernia can lead to pulmonary hypoplasia, which is often fatal.
-
•
That it is the first reported instance of hepatopulmonary involvement in the abdomen with pulmonary fragmentation.
1. Introduction
The incidence of congenital diaphragmatic hernia (CDH) is estimated at approximately 2.4–4.2 per 10,000 births. This anomaly arises from abnormal diaphragm development during fetal life, resulting in a diaphragmatic defect that allows abdominal contents to herniate into the thoracic cavity, compressing thoracic structures (1).The left side of the diaphragm is most commonly affected, accounting for approximately 80 % of cases (2). CDH classification varies based on defect location. Anterior defects are termed Morgagni hernias, while posterolateral defects, the most common type, are known as Bochdalek hernias. In rare instances, right-sided CDH can be complicated by hepatopulmonary fusion (HPF), a condition that significantly impacts clinical management and outcomes, occurring in approximately 3 cases per 1000 cases of right-sided CDH ([3], [4]). This case is described in accordance with the criteria of SCARE (5).
2. Presentation of case
2.1. Patient information
We present the case of a male infant with a gestational age of approximately 39 weeks born via Cesarean section without complications during pregnancy or delivery. Birth weight was 3 kg, and Apgar score was 7. Since birth, the infant exhibited respiratory distress, cyanosis, and poor feeding. The mother reported no maternal disorders during pregnancy or family history of congenital anomalies or tumors.
3. Clinical findings
Upon hospital admission on the fifth day of life, The infant presented with respiratory distress and central cyanosis, auscultation of the right chest revealed complete absence of breath sounds. Vital signs included a pulse of 155 beats per minute, blood pressure of 60/34 mmHg, and oxygen saturation of 92 % on 3 L/min oxygen via mask. Physical examination revealed decreased air entry in the right chest, a scaphoid abdomen, and a shifted cardiac impulse to the left. Arterial blood gas analysis showed a pH of 7.52, pCO2 of 53 mmHg, HCO3 of 22.3 mmol/L, pO2 of 55 %, and base excess of 1.3 mmol/L.
4. Diagnostic assessment
Laboratory tests were within normal limits.
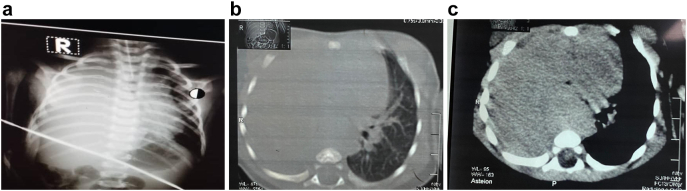
Chest X-ray demonstrated a dense opacity occupying the right hemithorax with mediastinal shift to the left (Fig. 1A).
Fig. 1.
A Preoperative chest X-ray demonstrating increased density in the right hemithorax with mediastinal shift to the contralateral side.
B. Axial CT scan showing hepatic tissue within the right thoracic cavity extending above the level of the tracheal bifurcation.
C. Axial CT scan demonstrating hepatic tissue occupying the upper right hemithorax with mediastinal shift to the left.
Echocardiogram revealed moderate heart failure, a small patent foramen ovale, right aortic arch, and severe pulmonary hypertension.
Computed tomography (CT) scan confirmed a large right-sided congenital diaphragmatic hernia occupying half of the right chest and containing the majority of the liver. No right pulmonary tissue was identified (Fig. 1B-C).
5. Therapeutic intervention
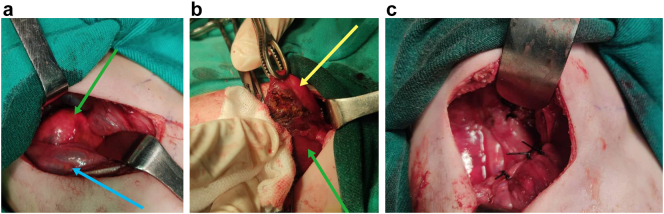
Given the patient's unstable condition and previous findings, surgical repair of the right congenital diaphragmatic hernia was indicated. Under general anesthesia, a right posterolateral fifth intercostal incision was made. A central congenital diaphragmatic hernia containing liver segments seven and eight, and part of segment four, was identified without other abdominal contents. A small portion of lung tissue adhered closely to liver segment seven (Fig. 2A).
Fig. 2.
A. Intraoperative image revealing pulmonary dysplasia with a small area of lung adhered to the liver (green arrow) and hepatic tissue (blue arrow).
B. Intraoperative image depicting isolated pulmonary tissue from the hepatic lobe with ligation of abnormal vessels. C: Intraoperative image demonstrating complete closure of the diaphragmatic defect and return of the liver to the abdomen. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
An attempt at hepatopulmonary fusion separation commenced with dissection of pulmonary parenchyma from the liver and ligation of small vessels (Fig. 2B). However, complete separation was not feasible. The vessels supplying the pulmonary tissue were ligated. The liver was repositioned into the abdomen, and the diaphragmatic defect was closed primarily (Fig. 2C). A chest tube was placed, and the chest cavity was closed (Fig. 3A).
Fig. 3.

A. Postoperative chest X-ray showing a chest tube in the right hemithorax with mediastinal structures returning to their normal position and the right hemidiaphragm in place.
Postoperatively, the patient was transferred to the intensive care unit and required mechanical ventilation for two weeks before succumbing to circulatory shock and thrombotic complications.
6. Discussion
Congenital diaphragmatic hernia (CDH) arises from an abnormal diaphragm formation during fetal development, preventing complete fusion of fetal leaflets. This results in a diaphragmatic defect, allowing abdominal organs to herniate into the thorax, either unilaterally or bilaterally. Right-sided CDH can be associated with the rare and potentially fatal condition of hepatopulmonary fusion (HPF), a fibrovascular fusion between the liver and lung. HPF severity varies from simple to complete fusion (4).
Given the divergent developmental pathways of the liver and lung, researchers have proposed theories to explain HPF. The first theory suggests that HPF occurs initially, subsequently impacting diaphragm development and leading to right-sided CDH. The second theory posits that CDH is the primary event, creating an abnormal thoracic environment that facilitates HPF.
Most HPF cases present with neonatal respiratory distress, although some remain asymptomatic and are incidentally discovered ([6], [7]). The majority of reported HPF cases have been diagnosed during CDH repair surgery (8).
Prenatal ultrasound is a valuable tool for diagnosing CDH by identifying the presence of abdominal organs in the thorax. However, ultrasound cannot confirm or exclude the presence of associated HPF (9). Magnetic resonance imaging (MRI) is the preferred method for diagnosing HPF, as it can reveal abnormal venous drainage between the lung and the inferior vena cava via the liver (10). HPF is often associated with abnormal pulmonary vasculature, including aberrant arterial supply to the lung, as seen in our case, or direct pulmonary drainage into the inferior vena cava via the liver (11).
This case represents the first reported instance in the medical literature of hepatopulmonary involvement in the abdomen with pulmonary fragmentation. The lung in this case received direct arterial supply from the aorta, with complete absence of the right lung.
Echocardiography is essential in CDH cases to identify pre-operative vascular anomalies, aiding in determining arterial supply and abnormal venous drainage, potential indicators of associated HPF. Advanced radiological imaging may be necessary to confirm any accompanying vascular abnormalities, significantly influencing treatment outcomes.
CDH is an important indicator for surgical intervention and the presence of HPF increases the difficulty of surgery. .However, optimal timing remains controversial, with no consensus on early versus delayed surgery. While early surgery within 24 h has been proposed, conclusive evidence of its benefit is lacking. Delaying surgery until patient stabilization is often preferred, especially when respiratory and circulatory systems are unstable (12,13). Stabilization criteria include oxygen saturation, blood pressure relative to gestational age, lactate levels, and urine output. Some advocate for 24–48 h stabilization prior to surgery, guided by echocardiography (14).
Surgical aims include reducing thoracic abdominal content and repairing the diaphragmatic defect (15). HPF management varies based on fusion severity, ranging from thin fibrous membranes to complete fusion without separable tissue layers (16). Surgical approaches for HPF include electrocautery, tissue resection (e.g., pulmonary lobectomy, partial hepatectomy), or sharp dissection (17). Surgery can be staged or performed in a single procedure.
HPF carries a poor prognosis, with perioperative mortality rates around 50 % (18). Contributing factors include lung hypoplasia, cardiac malformations, pulmonary vascular anomalies, and postoperative complications like pulmonary failure and pulmonary hypertension. While postoperative outcomes have been reported (8,18), the impact of timing surgery on prognosis remains unclear.
7. Conclusion
The physiological mechanisms underlying this deformity remain poorly understood, and surgical management is complicated by associated pulmonary and vascular anomalies, contributing to a poor prognosis.
Abbreviations
- HPF
hepatopulmonary fusion
Consent
Written informed consent was obtained from the patient's parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Ethical approval for this study (Ethical Committee N° NAC 207) was provided by the Ethical Committee NAC of Pediatric University Hospitals, Damascus, SYRIA on 20 August 2024.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Kamar Shaker and khaled Alomar: Conceptualization, resources, who wrote, original drafted, edited, visualized, validated, literature reviewed the manuscript.
Omar Shaker and Youssef chouman: Supervision, visualization, validation, resources, and review of the manuscript.
Mohammed Abd Alkader: pediatric surgeon, who performed and supervised the operation.
Nader Eid: Professor in neonatology,Head of NICU in Children Hospital.
Guarantor
Kamar shaker.
Research registration number
None.
Conflict of interest statement
The authors declare that they have no competing interests.
Contributor Information
Kamar Shaker, Email: Qamar.shaker@damascusuniversity.edu.sy.
Khaled Alomar, Email: Khaled.alomar@damascusuniversity.edu.sy.
Mohammed Abd Alkader, Email: Mohammad.Abdalkader@damascusuniversity.edu.sy.
Nader Eid, Email: nader.eid@damascusuniversity.edu.sy.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because the Data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.
References
- 1.Patel S., Rael J. Right-sided congenital diaphragmatic hernia caused by hepatopulmonary fusion. Case Rep. Pediatr. 2020;2020 doi: 10.1155/2020/8851341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olenik D., Codrich D., Gobbo F., et al. Hepatopulmonary fusion in a newborn. An uncommon intraoperatory finding during right congenital diaphragmatic hernia surgery: case description and review of literature. Hernia. 2014;18(3):417–421. doi: 10.1007/s10029-012-1042-y. [DOI] [PubMed] [Google Scholar]
- 3.Al-Zaiem M., Alzahrani A., Raml E.I., Alsulaimani N., Alzahrani L., Turki A. Right congenital diaphragmatic hernia associated with hepatic pulmonary fusion. J Pediatr Surg Case Rep. 2023;89 doi: 10.1016/j.epsc.2022.102540. [DOI] [Google Scholar]
- 4.Taide D., Bendre P., Kirtane J., et al. Hepatic pulmonary fusion – a rare case. Afr. J. Paediatr. Surg. 2010;7:28–29. doi: 10.4103/0189-6725.59357. [DOI] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., Collaborators The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. (Lond. Engl.) 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keller R.L., Aaroz P.A., Hawgood S., et al. MR imaging of hepatic pulmonary fusion, in neonates. AJR Am. J. Roentgenol. 2003;180:438–440. doi: 10.2214/ajr.180.2.1800438. [DOI] [PubMed] [Google Scholar]
- 7.Gander J.W., Kadenhe-Chiweshe A., Fisher J.C., et al. Hepatic pulmonary fusion in an infant with a right-sided congenital diaphragmatic hernia and contralateral mediastinal shift. J. Pediatr. Surg. 2010;45:265–268. doi: 10.1016/j.jpedsurg.2009.10.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olenik D., Codrich D., Gobbo F., Travan L., Zennaro F., Dell’Oste C., et al. Hepatopulmonary fusion in a newborn. An uncommon intraoperatory finding duringright congenital diaphragmatic hernia surgery: case description and review of literature [internet] Hernia. 2014;18(3):417–421. doi: 10.1007/s10029-012-1042-y. https://pubmed.ncbi.nlm.nih.gov/23324869/ Available from: [DOI] [PubMed] [Google Scholar]
- 9.Castle S.L., Naik-Mathuria B.J., Torres M.B. Right-sided congenital diaphragmatic hernia, hepatic pulmonary fusion, duodenal atresia, and imperforate anus in an infant. J. Pediatr. Surg. 2011;46:1432–1434. doi: 10.1016/j.jpedsurg.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 10.Chandrashekhara S.H., Seith Bhalla A., Gupta A.K., et al. Hepatic pulmonary fusion: case report with review of literature. J. Pediatr. Surg. 2011;46:e23–e27. doi: 10.1016/j.jpedsurg.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson D.M. Hepatopulmonary fusion: a rare variant of congenital diaphragmatic hernia [internet] J. Pediatr. Surg. 2020;55(9):1903–1907. doi: 10.1016/j.jpedsurg.2019.09.037. https://pubmed.ncbi.nlm.nih.gov/31708208/ Available from: [DOI] [PubMed] [Google Scholar]
- 12.Moyer V.A., Moya F.R., Tibboel D., et al. Late versus early surgical correction for congenital diaphragmatic hernia in newborn infants. Cochrane Database Syst. Rev. 1996;2000(3) doi: 10.1002/14651858.CD001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langer J.C., Filler R.M., Bohn D.J., et al. Timing of surgery for congenital diaphragmatic, hernia: is emergency operation necessary? J. Pediatr. Surg. 1988;23:731–734. doi: 10.1016/s0022-3468(88)80413-5. [DOI] [PubMed] [Google Scholar]
- 14.Almaramhy H.H. Hepatopulmonary fusion associated with right-sided congenital diaphragmatic hernia: management of this rare anomaly and a review of the literature. J. Int. Med. Res. 2018;46(12):5278–5284. doi: 10.1177/0300060518759892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsai J., Sulkowski J., Adzick N.S., Hedrick H.L., Flake A.W. Patch repair for congenital diaphragmatic hernia: is it really a problem? J. Pediatr. Surg. 2012;47(4):637–641. doi: 10.1016/j.jpedsurg.2011.11.054. [DOI] [PubMed] [Google Scholar]
- 16.Olenik D., Codrich D., Gobbo F., et al. Hepatopulmonary fusion in a newborn. An uncommon intraoperatory finding during right congenital diaphragmatic hernia surgery: case description and review of literature. Hernia. 2014;18:417–421. doi: 10.1007/s10029-012-1042-y. [DOI] [PubMed] [Google Scholar]
- 17.Laamiri R., Belhassen S., Ksia A., et al. Right congenital diaphragmatic hernia associated with hepatic pulmonary fusion: a case report. J. Neonatal Surg. 2016;5:35. doi: 10.21699/jns.v5i3.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almaramhy H.H. Hepatopulmonary fusion associated with right-sided congenital diaphragmatic hernia: management of this rare anomaly and a review of the literature [internet] J. Int. Med. Res. 2018;46(12):5278–5284. doi: 10.1177/0300060518759892. https://pubmed.ncbi.nlm.nih.gov/30352531/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available because the Data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.