Abstract
Objective:
Recently, different serum markers have been used for the diagnosis and prognosis of acute heart diseases in emergency departments. To determine such a role, the present study was designed and conducted.
Methods:
This is an analytical cross-sectional study conducted on patients with syncope complaints. The patients enrolled in the study based on the inclusion and exclusion criteria and underwent initial evaluations, including collecting a history, physical examination, ECG, blood sugar measurement, and, if necessary, brain CT scan, Doppler echocardiography, and CTA.
Results:
This study included 100 participants who complained of syncope. The results showed that 19% and 81% of the subjects suffered from cardiac and non-cardiac syncope, respectively. The average Pro BNP of the studied individuals was 196.06±128.45 pg/mL. According to the results, age and length of hospitalization had a positive and significant relationship with the average Pro BNP (p<0.01). Individuals with positive TPI, cardiac syncope, and abnormal ECG or Doppler findings had significantly higher average Pro BNP levels (p<0.01). The results of the diagnostic value of Pro BNP in diagnosing cardiac syncope also showed that its sensitivity and specificity were 94.73% and 56.79%, respectively.
Conclusion:
The results of this study showed that the increase in the Pro BNP values was associated with age, length of hospitalization, and ECG abnormalities. In addition, as an independent marker, Pro BNP had optimal acceptability in identifying cardiac syncope cases.
Key Words: Syncope, Emergency department, BNP, Prognosis
Introduction
Syncope is a sudden decrease in the consciousness level and the loss of muscle tone, which is caused by a temporary decrease in cerebral perfusion and followed by spontaneous recovery [1]. It is the most prevalent diagnosis in emergency departments and hospital admissions [2], which might be symptomless or with symptoms such as light-headedness, dizziness, nausea, feeling hot, and tunnel vision in the pre-syncope type [1, 3]. The prevalence of syncope in the general population is 3% in men and 3.5% in women [1, 3, 4]. Besides, more than 5% of the patients, who were referred to the emergency department, complain of syncope, with 1-6% of whom being hospitalized [3, 5].
Management of syncope patients is time-consuming and costly. Therefore, diagnostic interventions and tests to detect syncope cases contribute to improving patient survival and prognosis [6]. Nevertheless, the investigation and evaluation of syncope in patients referring to the emergency room is complicated and difficult due to the existence of different pathophysiological processes and multiple causes of occurrence [7, 8]. Although some causes of syncope have a good prognosis, others, such as cardiac arrhythmias, myocardial infarction, pulmonary embolism, and obscure hemorrhage, are associated with high mortality and disability rates. Thus, early diagnosis of the cause and prognosis of syncope cases contributes to a lower death rate and disease complications [9-11].
In recent years, several non-invasive methods with appropriate sensitivity and specificity to identify cases of cardiac syncope have been identified, including serum markers [12]. The Pro-BNP (Brain-type Natriuretic Peptide) serum marker, which is one of the main factors in the diagnosis of heart failure, is considered to be an important neutralizing mechanism that causes sodium excretion, weakens the growth of abnormal vascular cells, and increases vascular expansion by inhibiting renin-angiotensin-aldosterone and sympathetic nerve activity [6, 13, 14]. Evidence suggested that Pro-BNP was associated with HF (Heart Failure), cardiac-related mortality, and deaths following heart surgeries [15-17]. In addition, data demonstrates that the increased pro-BNP reflects the existence of structural heart disease. Recently, the BNP serum marker has been used in emergency departments due to its widespread acceptability in the diagnosis and prognosis of acute heart diseases [6, 18]. The use of Pro-BNP in cases of cardiac syncope is a viable option for diagnosing the disease and determining its prognosis due to the reduction of cardiac efficiency associated with hemodynamic arrhythmias and damage caused by structural changes in the heart [6]. Few studies have been conducted worldwide to investigate the usefulness and efficacy of the BNP serum marker and its other precursors in the diagnosis and prognosis of the patients with cardiac syncope. Therefore, the present study was designed to investigating the association between BNP serum levels and the diagnosis and prognosis of cardiac syncope in the patients referred to the emergency departments.
Materials and Methods
This analytical cross-sectional study was designed in accordance with the cross-sectional reporting guidelines in the epidemiology checklist and STROBE standard [19]. The study was approved by the Organizational Ethics Committee of Mashhad University of Medical Sciences (code: IR.MUMS.MEDICAL.REC.1399.194). The participants were the patients with complaints of syncope who were referred to the emergency departments of Imam Reza, Quaem, and Hasheminejad Hospitals (Mashhad, Iran). The research objectives were explained to the patients, their companions, or their legal guardians, and written informed consent was obtained from the patients prior to enrolling in the study. The convenience sampling method was applied, and eligible patients were recruited into the study until the required number of samples was achieved.
All the patients with complaints of syncope who were over the age of 18 were included in the study, and the ones with renal failure (Crt≥1.5, BUN≥30 or GFR≤70), lung diseases (COPD, pneumonia, ARDS), and conditions of increased cardiac outputs (such as cirrhosis, sepsis, and hyperthyroidism) were excluded.
The patients underwent an initial evaluation, including collecting the history, physical examination, ECG, blood sugar measurement, and brain CT scan, as well as a tilt-test in the case of being suspicious of reflex-mediated syncope. An emergency medicine resident took the blood samples and other tests under the supervision of the research team, and the samples were transferred to the laboratory for serum Pro-BNP analysis and measurement. All patients, including those who were hospitalized or discharged, underwent diagnostic examinations such as ECG, CBC, TPI measurement, echocardiography, and Brain CT scan (depending on the patient’s history), as well as Holter monitoring, Doppler ultrasound, and CT angiography (according to the cardiologist’s opinion). The patients were subsequently classified into cardiac and non-cardiac syncope (neurological, reflex-mediated, and unknown) groups. The results of the BNP levels in the two groups were compared based on the possible outcomes, including MI, life-threatening arrhythmia, need for pacemaker implantation, or pulmonary thromboembolism.
Statistical Analysis
The data were described using descriptive statistics, such as mean and standard deviation. The Chi-square and Fisher Exact tests were also used to examine the association between two categorical variables. An independent t-test was utilized to examine the mean differences between the two independent groups. Furthermore, the univariate and multivariate logistic regressions were applied to investigate the effective risk factors in the prognosis of cardiac syncope. Thus, the variables with a significance level of <0.2 in the univariate model were included in the final multivariate model, and the area under the ROC curve was used to assess the fit of the model. To evaluate the diagnostic value of BNP in the diagnosis of cardiac syncope, the researchers used sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). DOR (Diagnostic Odds Ratio) was also used to evaluate the performance of BNP in the diagnosis of cardiac syncope (calculation of DOR based on equations 1, 2, and 3). The statistical analysis was performed using the Stata software version 12 (Corp, College Station, Texas). The significance level was considered p<0.05.
Equation (1):
Equation (2):
Equation (3):
Results
A total of 100 patients with complaints of syncope and a mean age of 49.56±16.55 years were included in this study. The mean Pro-BNP level in the studied subjects was 196.06 pg/mL, ranging from 30 to 661 pg/mL. 47% of the subjects (n=47) were women, and 53% were men, indicating a significant difference according to the Pro-BNP (p=0.018). The results showed that 11% and 89% of the studied subjects had positive and negative TPIs, respectively, indicating a significant difference between the two groups with the Pro-BNP levels above and below 150 pg/mL (p=0.042).
The average length of hospitalization of the patients was 3.59 days, with 4.47 days in the Pro-BNP>150 pg/mL and 2.59 days in the Pro-BNP<150 pg/mL groups, showing a statistically significant difference (p=0.004). The study found that 33.96% of the people with Pro BNP>150 pg/mL had cardiac syncope, and 97.87% of those with Pro BNP<150 pg/ml experienced non-cardiac syncope, which was a statistically significant difference (p=0.001). Furthermore, the ECG analysis showed that 69.81% of the patients with Pro BNP>150 pg/mL had abnormal ECG, and 63.83% of those with Pro BNP<150 pg/mL had normal ECG. This difference was statistically significant (p=0.001) (Table 1).
Table 1.
Clinical and basic information of the study subjects
| P value | Pro-BNP | Overall | Variables | |
|---|---|---|---|---|
| <150 pg/mL | >150 pg/mL | |||
| 0.025a | 45.65±2.39 | 53.01±2.20 | 49.56±16.55 | Age (year) |
| Gender | ||||
| 0.018b | 19 (40.42%) | 34 (64.15%) | 53 (53%) | Male |
| 28 (59.58%) | 19 (35.85%) | 47 (47%) | Female | |
| 0.375a | 12.09±0.37 | 12.45±0.32 | 12.24±2.47 | Hb |
| 0.004a | 2.59±0.367 | 4.47±0.51 | 3.59±0.33 | Hospitalization (day) |
| TPI | ||||
| 0.042b | 2 (4.25%) | 9 (16.98%) | 11 (11%) | Positive |
| 45 (95.75%) | 44 (83.02%) | 89 (89%) | Negative | |
| PMH | ||||
| 0.241b | 7 (15.91%) | 6 (13.64%) | 13 (13.54%) | IHD |
| 5 (11.36%) | 9 (20.45%) | 14 (14.58) | HTN | |
| 8 (18.18%) | 10 (22.73%) | 18 (18.75%) | DM | |
| 4 (9%) | 12 (27.27%) | 16 (16.67%) | Other | |
| 20 (45.46%) | 15 (34.09%) | 35 (36.46%) | No PMH | |
| Syncope | ||||
| 0.001b | 1 (2.13%) | 18 (33.96%) | 19 (19%) | Cardiac |
| 46 (97.87%) | 35 (66.04%) | 81 (81%) | Non-Cardiac | |
| Echocardiography | ||||
| 0.201b | 2 (11.12%) | 7 (26.92%) | 9 (20.46%) | Normal |
| 16 (98.88%) | 19 (73.08%) | 35 (79.54%) | Abnormal | |
| Brain CT | ||||
| 0.240b | 5 (19.23%) | 3 (8.82%) | 8 (13.34%) | Normal |
| 21 (80.77%) | 31 (91.18%) | 52 (86.66%) | Abnormal | |
| ECG | ||||
| 0.001b | 37 (69.81%) | 17 (36.17%) | 54 (54%) | Normal |
| 16 (30.19%) | 30 (63.83%) | 46 (46%) | Abnormal | |
aIndependent T-test; bFisher Exact tests and Chi-square
The results of assessing the diagnostic value of Pro BNP in identifying cardiac syncope in values above 150 pg/mL (according to the studies) are presented in Table 2, which showed that the sensitivity and specificity of Pro BNP in detecting cardiac syncope were 94.73% and 56.79 %, respectively. The positive and negative predictive values of Pro BNP for detecting cardiac syncope were 33.96% and 97.87%, respectively. The positive and negative likelihood ratios of Pro BNP were 2.19 and 0.095, respectively, and its DOR was 23.80 (Table 2). The ROC curve clearly demonstrated the diagnostic value of Pro BNP in cardiac syncope cases (Figure 1).
Table 2.
Diagnostic value of Pro-BNP >150 pg/mL in the diagnosis of cardiac syncope and ECG abnormalities
| DOR | NPV | PPV | Specificity | Sensitivity | Groups |
|---|---|---|---|---|---|
| 23.80 | 97.87% | 33.96% | 56.79% | 94.73% | Cardiac Syncope |
| 4.06 | 63.82% | 69.81% | 65.21% | 68.51% | Abnormal ECG |
Fig. 1.
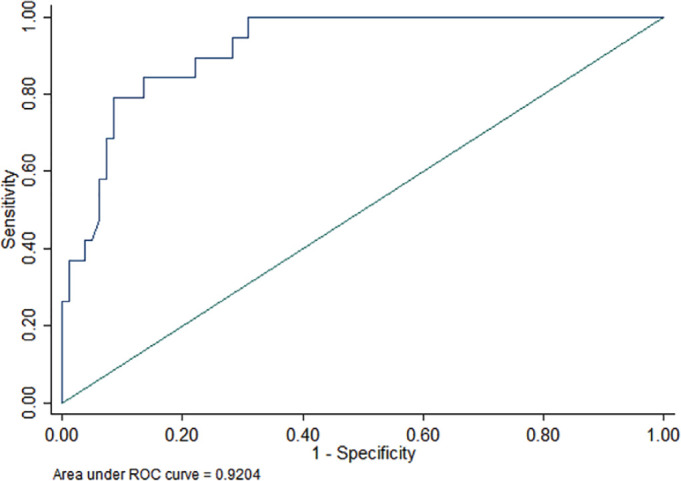
The area under the ROC curve in the multivariate logistic regression model fit.
Univariate logistic regression revealed a significant relationship between variables such as age, Hb, TPI, length of hospitalization, the presence of ECG abnormalities, and the occurrence of cardiac syncope in the patients (p<0.05). Therefore, the increase in age, Hb, TPI, length of hospitalization, and the presence of ECG abnormalities increased the risk of cardiac syncope.
On the other hand, the Pro-BNP levels of more than 150 pg/mL were associated with an increased risk of cardiac syncope in the patients (OR=23.65, p=0.001). The results of the multivariate model showed that there was a significant relationship between cardiac syncope in patients with positive TPI and the presence of ECG abnormalities and the Pro-BNP>150 pg/mL (p<0.05). In other words, the risk of cardiac syncope increased with the increase of the Pro-BNP value (Table 3).
Table 3.
Results of univariate and multivariate logistic regressions between the prognosis of cardiac syncope and Pro-BNP levels and the studied variables
| Multivariate | Univariate | Variables | ||||
|---|---|---|---|---|---|---|
| P value b | 95% Confidence Interval | Odds Ratio | P value z | 95% Confidence Interval | Odds Ratio | |
| 0.955 | 0.954-1.04 | 0.998 | 0.018 | 1.01-1.07 | 1.04 | Age |
| - | - | - | 0.590 | 0.936-1.03 | 0.986 | Sex (Male) |
| 0.030 | 1.22-52.93 | 8.06 | 0.001 | 2.85-44.22 | 11.22 | TPI (Positive) |
| 0.081 | 0.978-1.45 | 1.19 | 0.001 | 1.12-1.51 | 1.31 | Hospitalization |
| - | - | - | 0.940 | 0.79-18.80 | 3.86 | Abnormal Echocardiography |
| - | - | - | 0.574 | 0.059-4.79 | 0.532 | Abnormal Brain CT |
| PMH | ||||||
| - | - | - | 0.242 | 0.569-9.35 | 2.30 | DM |
| - | - | - | 0.924 | 0.184-6.46 | 1.09 | IHD |
| - | - | - | 0.252 | 0.537-10.72 | 2.40 | HTN |
| - | - | - | 0.864 | 0.147-4.97 | 0.857 | Other |
| 0.022 | 1.46-144.02 | 14.50 | 0.003 | 2.86-176.67 | 22.50 | Abnormal ECG |
| 0.014 | 1.84-223.39 | 20.31 | 0.001 | 3.01-185.81 | 23.65 | Pro-BNP >150 pg/ml |
zUnivariate Logistic regression; bMultivariate Logistic regression
The results of examining the diagnostic value of Pro BNP in identifying ECG abnormalities showed that the sensitivity and specificity of Pro BNP in identifying abnormal ECGs were 68.51% and 65.21%, respectively. Besides, the positive and negative predictive values of Pro BNP in detecting cardiac syncope were 69.81% and 63.82%, respectively. The positive and negative likelihood ratios of Pro BNP were 1.96 and 0.482, respectively, and its DOR was 4.06 as well (Table 2).
Discussion
The results of this multicenter study, which was conducted on patients with syncope who were referred to the emergency department, showed that Pro-BNP was an independent predictive factor suitable for identifying cardiac syncope cases. Hence, the Pro-BNP values greater than 150 pg/mL had a sensitivity of 94.73% in identifying cardiac syncope cases. In addition, the findings of this study showed that Pro-BNP was associated with increased hospitalizations, ECG abnormalities, and positive TPI, which was in line with other studies conducted in this field.
Cardiac causes of syncope are the most important factors in determining the prognosis and classifying the risk of death in patients with syncope, hence, the prevalence of death from these causes is much higher than other ones. Evidence has well shown that Pro-BNP is a predictive factor of the survival rate of patients with aortic stenosis, in-hospital mortality of patients with heart failure, all deaths related to non-cardiac surgeries, and the deaths of adults due to congenital heart diseases [20-23]. Determining the prognosis and risk of cardiac syncope associated with Pro-BNP levels in people who were referred to emergency departments was one of the main factors related to the survival of the patients [24]. However, the application of such evidence and determining the risk and probability of occurrence is time-consuming.
Several studies were conducted to investigate the role of Pro-BNP in cardiac syncope [18, 25-27]. In this regard, evidence showed that the mortality rate of the patients undergoing coronary artery surgery who were divided into high-risk groups based on serum markers such as Pro-BNP was also reduced, indicating that Pro-BNP has a prognostic role of Pro-BNP in the appropriate prognosis of these patients [28]. In addition, the present study indicated that patients with cardiac syncope had considerably higher levels of Pro-BNP. Furthermore, the Pro-BNP levels were found to be significantly associated with the ECG results, with an increase in ECG abnormalities. Some studies investigated the role of Pro-BNP in the prognosis of cardiac events in preeclampsia patients and stated that Pro-BNP could be used as an important predictor of cardiac events in such patients [29]. Tanimoto et al., used Pro BNP levels to distinguish cardiac from non-cardiac syncope and showed that its sensitivity and specificity were 82% and 92%, respectively [30]. This was consistent with the findings of the present study, which found that the sensitivity and specificity of Pro-BNP in identifying cardiac from non-cardiac syncope in cut-off BNP >150 pg/mL were 94.73% and 56.79%, respectively.
A significant relationship between the ages of the patients suffering from cardiac syncope was also found in their study, which was in line with the results of the present research. In other words, as the ages of the studied people increased, the amounts of Pro BNP increased as well. The relationship between age and pro-BNP level could be attributed to the increased cardiovascular risk factors at older ages. In their study, Pfister et al., showed that Pro-BNP levels were significantly higher in the cardiac syncope group (1147 pg/mL) than in the non-cardiac syncope one (139 pg/mL) [15]. On the other hand, the ages of the people with cardiac syncope were significantly higher than the non-cardiac syncope ones, which was in line with the results of the present study. The cut-off value of 156 pg/mL, which they specified for cardiac syncope, had a sensitivity of 89.7% and a specificity of 51.8%, which was consistent with the findings of this study. Therefore, the sensitivity and specificity of the Pro BNP in values greater than 150 pg/mL were 94.73% and 56.79%, respectively. Although the values of Pro BNP in the cardiac syncope group in a study by Pfister et al., were significantly higher than in the present research, structural and demographic differences in the populations were among the most relevant causes for this discrepancy.
Although this study had some strengths, there were some limitations as follows. Due to the limitations that occurred during the COVID-19 pandemic, it was not possible to take more samples and follow up with the patients for more than 30 days; consequently, the sample size was reduced. In addition, considering that the most common symptom of syncope in some cases was tachycardia stress, and only with this symptom allowed the possibility of differentiating cardiac and non-cardiac causes, all cases of tachycardia stress were inevitably classified as abnormal ECG.
The findings of this study well indicated that the serum levels of Pro BNP were significantly higher in the patients referring to cardiac syncope complaints. Furthermore, the high average BNP in people with ECG abnormalities was a good indication of the prognostic role of pro-BNP in heart disease patients. On the other hand, the findings of investigating the diagnostic value of Pro BNP in identifying cardiac syncope showed that the BNP levels greater than 150 pg/mL had a sensitivity of 94.73% and a specificity of 56.79% in identifying cardiac syncope cases, with an optimal acceptability.
Declaration
Ethics approval and consent to participate:
Ethical permission was granted by Mashhad University of Medical Science (IR.MUMS.MEDICAL.REC.1399.194).
Availability of data and materials:
Data will be made available upon reasonable request.
Funding:
Mashhad University of Medical Sciences
Consent for publication:
Not applicable
Conflict of interest:
The authors declared that they had no conflict of interest.
References
- 1.Chu I, Vaca F, Stratton S, Chakravarthy B, Hoonpongsimanont W, Lotfipour S. Geriatric trauma care: challenges facing emergency medical services. Cal J Emerg Med. 2007;8(2):51–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Chkhaberidze N, Axobadze K, Kereselidz M, Pitskhelauri N, Jorbenadze M, Chikhladze N. Study of Epidemiological Characteristics of Fatal Injuries Using Death Registry Data in Georgia. Bull Emerg Trauma. 2023;11(2):75–82. doi: 10.30476/beat.2023.97931.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soltani SM, Rezvani Kakhki B, Mousavi SM, Zakeri H, Ahmadi Koupaei SR, Sadrzadeh SM, et al. Epidemiology and etiology of hospitalized pediatric trauma: An experience from the referral trauma hospital of Iran. Archives of Trauma Research. 2024;13(1):43–8. [Google Scholar]
- 4.Hosseini M, Shayan L, Yadollahi M, Karajizadeh M. Characteristics of Traumatic Patients Referring to the Emergency Department and their Association with Mortality and Incidence of Surgery Performance. Bull Emerg Trauma. 2023;11(3):132–7. doi: 10.30476/beat.2023.97729.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moran CG, Lecky F, Bouamra O, Lawrence T, Edwards A, Woodford M, et al. Changing the System - Major Trauma Patients and Their Outcomes in the NHS (England) 2008-17. EClinicalMedicine. 2018;2-3:13–21. doi: 10.1016/j.eclinm.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabbe BJ, Simpson PM, Sutherland AM, Wolfe R, Fitzgerald MC, Judson R, et al. Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg. 2012;255(6):1009–15. doi: 10.1097/SLA.0b013e31824c4b91. [DOI] [PubMed] [Google Scholar]
- 7.Kang BH, Jung K, Kim S, Youn SH, Song SY, Huh Y, et al. Accuracy and influencing factors of the Field Triage Decision Scheme for adult trauma patients at a level-1 trauma center in Korea. BMC Emerg Med. 2022;22(1):101. doi: 10.1186/s12873-022-00637-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyoshi Y, Kondo Y, Hirano Y, Ishihara T, Sueyoshi K, Okamoto K, et al. Characteristics, injuries, and clinical outcomes of geriatric trauma patients in Japan: an analysis of the nationwide trauma registry database. Sci Rep. 2020;10(1):19148. doi: 10.1038/s41598-020-76149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonne S, Schuerer DJ. Trauma in the older adult: epidemiology and evolving geriatric trauma principles. Clin Geriatr Med. 2013;29(1):137–50. doi: 10.1016/j.cger.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Jiang L, Zheng Z, Zhang M. The incidence of geriatric trauma is increasing and comparison of different scoring tools for the prediction of in-hospital mortality in geriatric trauma patients. World J Emerg Surg. 2020;15(1):59. doi: 10.1186/s13017-020-00340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naraynsingh R, Sammy I, Paul JF, Nunes P. Trauma in the elderly in Trinidad and Tobago: a cross-sectional study. Eur J Emerg Med. 2015;22(3):219–21. doi: 10.1097/MEJ.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 12.Hendrickson SA, Osei-Kuffour D, Aylwin C, Fertleman M, Hettiaratchy S. ‘Silver’trauma: predicting mortality in elderly major trauma based on place of injury. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2015;23:1. [Google Scholar]
- 13.Bozzette A, Aeron-Thomas A. Reducing trauma deaths in the UK. Lancet. 2013;382(9888) doi: 10.1016/S0140-6736(13)61597-4. [DOI] [PubMed] [Google Scholar]
- 14.Vaishya R, Vaish A. Falls in Older Adults are Serious. Indian J Orthop. 2020;54(1):69–74. doi: 10.1007/s43465-019-00037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gioffrè-Florio M, Murabito LM, Visalli C, Pergolizzi FP, Famà F. Trauma in elderly patients: a study of prevalence, comorbidities and gender differences. G Chir. 2018;39(1):35–40. doi: 10.11138/gchir/2018.39.1.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pfister R, Scholz M, Wielckens K, Erdmann E, Schneider CA. Use of NT-proBNP in routine testing and comparison to BNP. Eur J Heart Fail. 2004;6(3):289–93. doi: 10.1016/j.ejheart.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 17.Tada H, Ito S, Shinbo G, Tadokoro K, Ito I, Hashimoto T, et al. Significance and utility of plasma brain natriuretic peptide concentrations in patients with idiopathic ventricular arrhythmias. Pacing Clin Electrophysiol. 2006;29(12):1395–403. doi: 10.1111/j.1540-8159.2006.00553.x. [DOI] [PubMed] [Google Scholar]
- 18.Badertscher P, du Fay de Lavallaz J, Hammerer-Lercher A, Nestelberger T, Zimmermann T, Geiger M, et al. Prevalence of Pulmonary Embolism in Patients With Syncope. J Am Coll Cardiol. 2019;74(6):744–54. doi: 10.1016/j.jacc.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 20.Bergler-Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G, Gabriel H, et al. Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation. 2004;109(19):2302–8. doi: 10.1161/01.CIR.0000126825.50903.18. [DOI] [PubMed] [Google Scholar]
- 21.Huang YT, Tseng YT, Chu TW, Chen J, Lai MY, Tang WR, et al. N-terminal pro b-type natriuretic peptide (NT-pro-BNP) -based score can predict in-hospital mortality in patients with heart failure. Sci Rep. 2016;6:29590. doi: 10.1038/srep29590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Popelová JR, Kotaška K, Tomková M, Tomek J. Usefulness of N-Terminal Pro-Brain Natriuretic Peptide to Predict Mortality in Adults With Congenital Heart Disease. Am J Cardiol. 2015;116(9):1425–30. doi: 10.1016/j.amjcard.2015.07.070. [DOI] [PubMed] [Google Scholar]
- 23.Álvarez Zurro C, Planas Roca A, Alday Muñoz E, Vega Piris L, Ramasco Rueda F, Méndez Hernández R. High levels of preoperative and postoperative N terminal B-type natriuretic propeptide influence mortality and cardiovascular complications after noncardiac surgery: A prospective cohort study. Eur J Anaesthesiol. 2016;33(6):444–9. doi: 10.1097/EJA.0000000000000419. [DOI] [PubMed] [Google Scholar]
- 24.Reed MJ, Gibson L. The effect of syncope on brain natriuretic peptide. Emerg Med J. 2011;28(12):1066–7. doi: 10.1136/emj.2010.106955. [DOI] [PubMed] [Google Scholar]
- 25.Badertscher P, Nestelberger T, de Lavallaz JDF, Than M, Morawiec B, Kawecki D, et al. Prohormones in the Early Diagnosis of Cardiac Syncope. J Am Heart Assoc. 2017;6:12. doi: 10.1161/JAHA.117.006592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costantino G, Solbiati M, Pisano G, Furlan R. NT-pro-BNP for differential diagnosis in patients with syncope. Int J Cardiol. 2009;137(3):298–9; author reply 9. doi: 10.1016/j.ijcard.2008.05.051. [DOI] [PubMed] [Google Scholar]
- 27.Isbitan A, Hawatmeh A, Elnahar Y, Patel K, Altheeb Z, Debari V, et al. Utility of brain natriuretic peptide assay as a predictor of short term outcomes in patients presenting with syncope to the emergency department. Cardiovasc Diagn Ther. 2016;6(3):234–40. doi: 10.21037/cdt.2016.03.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Polineni S, Parker DM, Alam SS, Thiessen-Philbrook H, McArthur E, DiScipio AW, et al. Predictive Ability of Novel Cardiac Biomarkers ST2, Galectin-3, and NT-ProBNP Before Cardiac Surgery. J Am Heart Assoc. 2018;7:14. doi: 10.1161/JAHA.117.008371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghomian N, Vakilian F, Shahri B, Rostaminejad V, Khadem-Rezaiyan M. Can brain natriuretic peptide predict cardiovascular complications in severe preeclampsia? A case-control study. Int J Reprod Biomed. 2019;17(4):271–8. doi: 10.18502/ijrm.v17i4.4552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunda S, Kanmanthareddy A, Atkins D, Bommana S, Pimentel R, Drisko J, et al. Role of yoga as an adjunctive therapy in patients with neurocardiogenic syncope: a pilot study. Journal of Interventional Cardiac Electrophysiology. 2015;43:105–10. doi: 10.1007/s10840-015-9996-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available upon reasonable request.