Summary
Background
Obesity represents a major global health challenge with important clinical implications. Despite its recognized importance, the global disease burden attributable to high body mass index (BMI) remains less well understood.
Methods
We systematically analyzed global deaths and disability-adjusted life years (DALYs) attributable to high BMI using the methodology and analytical approaches of the Global Burden of Disease Study (GBD) 2021. High BMI was defined as a BMI over 25 kg/m2 for individuals aged ≥20 years. The Socio-Demographic Index (SDI) was used as a composite measure to assess the level of socio-economic development across different regions. Subgroup analyses considered age, sex, year, geographical location, and SDI.
Findings
From 1990 to 2021, the global deaths and DALYs attributable to high BMI increased more than 2.5-fold for females and males. However, the age-standardized death rates remained stable for females and increased by 15.0% for males. Similarly, the age-standardized DALY rates increased by 21.7% for females and 31.2% for males. In 2021, the six leading causes of high BMI-attributable DALYs were diabetes mellitus, ischemic heart disease, hypertensive heart disease, chronic kidney disease, low back pain and stroke. From 1990 to 2021, low-middle SDI countries exhibited the highest annual percentage changes in age-standardized DALY rates, whereas high SDI countries showed the lowest.
Interpretation
The worldwide health burden attributable to high BMI has grown significantly between 1990 and 2021. The increasing global rates of high BMI and the associated disease burden highlight the urgent need for regular surveillance and monitoring of BMI.
Funding
National Natural Science Foundation of China and National Key R&D Program of China.
Keywords: Obesity, Body mass index, Global Burden of Disease Study, Metabolic risk
Research in context.
Evidence before this study
High BMI has been extensively documented as a major global health issue by sources such as the Global Burden of Disease (GBD) Study and various epidemiological reports. We conducted a comprehensive literature search across PubMed and Scopus databases from January 1990 to May 2024, using terms like “high BMI,” “global burden of disease,” and “obesity.” Our search yielded that varying evidence quality, with some studies exhibiting potential biases or limited generalizability.
Added value of this study
This study provides an updated and comprehensive analysis of global deaths and disability-adjusted life years (DALYs) attributable to high BMI from 1990 to 2021, using the latest GBD 2021 data. It reveals that global deaths and DALYs due to high BMI have more than doubled over this period, with low-middle SDI countries experiencing the highest annual percentage increases in age-standardized DALY rates.
Implications of all the available evidence
The GBD 2021 study highlights the growing global burden of high BMI and significant regional disparities. This indicates a pressing need for targeted interventions and monitoring. The study calls for ongoing surveillance and research to refine strategies and enhance health outcomes across different socio-economic contexts.
Introduction
Obesity is a modifiable metabolic risk factor characterized by chronic positive energy balance that results in excess adiposity.1 The etiology of obesity is multifactorial, involving genetics, environmental, socioeconomic, and behavioral factors. These factors contribute to low-grade chronic inflammation, abnormal hormonal and immune responses, and, ultimately, systemic metabolic dysregulation.1, 2, 3 Obesity is a major public health challenge, impacting over 2 billion individuals, and its prevalence is on the rise globally.4, 5, 6, 7
Obesity significantly increases the risk of developing type 2 diabetes, hypertension, cardiovascular disease (CVD), chronic kidney disease, chronic respiratory disease, cirrhosis, and various types of cancers.8, 9, 10, 11, 12 This significantly strains many countries' health care systems and other social resources, leading to substantial direct and indirect societal costs.13,14 The global medical care costs of obesity were nearly 1.96 trillion, or 2.4% of the global Gross Domestic Product in 2020.13,14 If current trends persist, it is expected that by 2035, the economic impact of obesity could reach nearly 3% of the global Gross Domestic Product.14 Managing obesity is challenging due to the difficulty patients experience maintaining strict dietary and exercise regimens. Obesity pharmacotherapy and bariatric surgery are expensive and may lead to various adverse effects, such as nausea, vomiting, diarrhea, and neuropathy.15
From 1990 to 2017, the global burden attributable to high body mass index (BMI) more than doubled in over 70 countries and is expected to continue increasing.16 It is anticipated that the global prevalence of obesity will increase further across all age groups due to the recent COVID-19 pandemic.17, 18, 19 The measures taken to enforce social distancing during the COVID-19 pandemic have reduced physical activity, increased sedentary behavior, and altered eating habits.20,21 Moreover, people have been more inclined to purchase and consume processed, unhealthy foods.22 Thus, the surveillance of high BMI prevalence is crucial for developing and implementing public health initiatives designed to mitigate or eliminate the occurrence and impact of obesity. As part of the risk factor assessment for the Global Burden of Disease Study (GBD) 2021, we comprehensively analyzed global trends and burden of high BMI from 1990 to 2021, broken down by country. This manuscript presents the updated findings of a systematic analysis conducted for the recent and publicly available GBD 2021 database.
Methods
Data sources
The data regarding the impact of high BMI on the burden of disease was gathered from the Global Health Data Exchange GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool). GBD collaborators developed this tool to conduct a comprehensive evaluation of age- and sex-specific mortality for 288 causes, prevalence and years lived with disability for 371 diseases and injuries, and comparative risks for 88 risk factors across 204 countries and territories and 811 subnational locations from 1990 to 2021. The detailed methodologies of GBD 2021 and the comparative risk assessment specifically for high BMI have been described elsewhere.23,24 The protocol used for GBD 2021 was published on the Institute for Health Metrics and Evaluation website. The GBD study provides the baseline data and methodology, including comprehensive disease categorization and burden estimates. Additional analysis performed by the authors involves applying the GBD framework to specific research questions, focusing on subgroups or regions not extensively covered. All GBD 2021 analyses complied with the Guidelines for Accurate and Transparent Health Estimates Reporting statement.
Definitions
The GBD 2021 study estimated the impact by comparing actual health outcomes to hypothetical outcomes under historical exposure scenarios. High BMI was defined as BMI, calculated by dividing a person's weight in kilograms by the square of their height in meters (kg/m2) and was over 25 kg/m2 for individuals aged 20 years and older.6 Detailed information about the data selection process and inputs have been provided previously.6 In the GBD study, the classification of disease attributable to high BMI is organized into a four-level hierarchical system to ensure comprehensive and precise categorization. Level 1 includes broad groupings such as communicable and non-communicable diseases, and injuries. Level 2 breaks these into 22 specific categories, e.g. cardiovascular diseases within non-communicable diseases. Level 3 further specifies conditions within these categories, e.g. stroke under cardiovascular diseases. Level 4 provides even finer detail, identifying subcategories e.g. ischemic stroke within the general stroke category, allowing for a detailed and exhaustive analysis of global health metrics. This study uses Disability-Adjusted Life Years (DALYs) to measure disease burden. DALYs are a commonly used metric that combines the years of life lost due to premature mortality and the years lived with disability. Typically, DALYs are considered over an extended period, such as a lifetime, but in our analysis, we quantified DALYs annually, specifically for 2021. When referring to “DALY cases” in our study, we refer to the total number of DALYs accumulated within 2021 due to various health conditions. This approach provides a snapshot of the disease burden for that particular year. By focusing on DALYs within a single year, we can assess and compare the immediate impact of health issues and their contribution to the overall disease burden for that period. The quantification of cause-specific deaths and DALYs across various demographics, including age, sex, temporal dimensions, and geographical locations, has been meticulously gathered from an extensive dataset. DALYs serve as a comprehensive metric, encapsulating the total health burden attributable to disease by amalgamating the years of life forfeited through premature mortality and the years spent living with disability. Each DALY is interpreted as a loss of one year of optimal health. In previous GBD studies and in this study, we have focused on the attributable burden of disease using the concept of the theoretical minimum risk exposure level (TMREL).17 TMREL represents the level of risk exposure that minimizes the risk at the population level, effectively capturing the maximum attributable burden if the exposure were reduced to this ideal level.17 To estimate the burden of high BMI, we calculated DALYs by multiplying DALYs for the health outcomes related to high BMI by the population attributable fraction (PAF) for high BMI. This approach is also used to estimate high BMI-attributable deaths. Risks are categorized based on how BMI exposure is measured: dichotomous, polytomous, or continuous. The PAF indicates the proportion of risk that would be reduced if BMI was reduced to TMREL. The socio-demographic index (SDI) is introduced as a composite measure reflecting the development status of various geographic locales. This index is derived from three indicators: the total fertility rate among women under 25, educational attainment for individuals aged 15 and above, and per capita income adjusted for time lag. The SDI scale, ranging from a value close to zero (indicating low development) to a maximum value (indicating high development), categorizes countries and territories into five quintiles, from low to high developmental status, providing a nuanced understanding of the interplay between socioeconomic factors and health outcomes.
Statistical analysis
We analyzed the disease burden attributable to high BMI, considering metrics such as the total number and rate of deaths or DALYs, age-standardized rates, and percent changes. The age-standardized rates were calculated by adjusting to the global age structure, which is essential for comparing different populations or changes over time. The 95% uncertainty intervals (UIs) were delineated by the 2.5th and 97.5th percentiles, representing the 25th and 975th values, respectively, from the ordered set of 1000 estimates. Population-attributable fractions were used to measure the proportion of age-standardized DALYs that could have been prevented with reduced exposure to high BMI. Furthermore, we explored the relationship between the SDI and the disease burden attributable to high BMI across different locations and years. A 95% UI excluding zero was considered statistically significant. The mapping figures were created using mapchart.net.
Ethics
The institutional review board granted an exemption for this study, as it utilized publicly accessible data that contained no confidential or personally identifiable patient information.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
The overall impact and temporal trend of high BMI
In 2021, there was an estimated incidence of 3.7 million deaths and an estimated prevalence of 128.5 million cases of DALYs (Tables 1 and 2). Globally, there has been a significant increase in global deaths and DALYs attributable to high BMI for both males and females (number of deaths: from 1.5 million to 3.7 million; DALYs: from 48.0 million to 128.5 million), corresponding to a nearly 2.5-fold increase (Fig. 1A and B). Specifically, the global deaths attributable to high BMI have risen from 0.8 million (95% UI 0.4 million, 1.3 million) in 1990 to 2.0 million (95% UI 0.9 million, 3.2 million) in 2021 for females, and from 0.6 million (95% UI 0.3 million, 1.0 million) in 1990 to 1.7 million (95% UI 0.9 million, 2.6 million) in 2021 for males.
Table 1.
Deaths and age-standardized death rates of high BMI in 1990 and 2021 and the temporal trend of age-standardized death rates from 1990 to 2021.
| 1990 |
2021 |
Relative change in age-standardized death rate, 1990–2021 (95% CI) | |||
|---|---|---|---|---|---|
| No. death cases (95% UI) | Age-standardized death rates per 100,000 (95% UI) | No. death cases (95% UI) | Age-standardized death rates per 100,000 (95% UI) | ||
| Global | 1,459,533 (723,043–2,287,052) | 40.90 (19.87–64.16) | 3,709,063 (1,847,840–5,658,334) | 44.23 (22.01–67.64) | 0.08 (0.01–0.15) |
| Sex | |||||
| Female | 828,147 (407,103–1,302,480) | 41.57 (20.18–65.25) | 2,013,089 (979,000–3,076,045) | 43.26 (21.08–66.05) | 0.04 (−0.03 to 0.12) |
| Male | 631,386 (315,453–988,214) | 39.03 (19.35–60.80) | 1,695,974 (861,972–2,635,343) | 44.90 (23.01–70.17) | 0.15 (0.06–0.23) |
| SDI | |||||
| Low SDI | 70,040 (42,195–110,220) | 32.89 (20.11–51.01) | 204,362 (114,078–318,520) | 43.22 (24.93–66.40) | 0.31 (0.14–0.50) |
| Low-middle SDI | 177,919 (100,108–281,095) | 31.91 (18.22–49.61) | 671,617 (349,426–1,011,204) | 49.59 (26.29–74.99) | 0.55 (0.35–0.74) |
| Middle SDI | 306,277 (185,062–452,734) | 33.78 (20.37–50.30) | 1,126,388 (581,131–1,700,642) | 44.80 (23.60–67.57) | 0.33 (0.10–0.46) |
| High-middle SDI | 430,095 (194,645–685,431) | 48.62 (22.28–77.66) | 904,396 (417,515–1,428,690) | 46.71 (21.70–73.63) | −0.04 (−0.12 to 0.05) |
| High SDI | 472,370 (199,898–767,235) | 43.07 (18.21–69.90) | 797,416 (368,146–1,253,107) | 35.13 (16.59–54.47) | −0.18 (−0.24 to −0.07) |
| Causes | |||||
| Cardiovascular diseases | 863,066 (477,898–1,316,551) | 37.30 (0.36–13.63) | 1,904,239 (1,072,732–2,864,242) | 34.24 (7.36–12.87) | −0.07 (−0.14 to 0.02) |
| Chronic respiratory diseases | 38,041 (16,523–59,933) | 1.58 (1.36–0.43) | 62,363 (26,317–100,543) | 1.19 (8.36–0.31) | −0.26 (−0.35 to −0.14) |
| Diabetes and kidney diseases | 330,122 (170,826–489,762) | 13.57 (2.36–4.53) | 1,142,121 (602,169–1,666,047) | 19.81 (9.36–7.14) | 0.50 (0.39–0.64) |
| Digestive diseases | 21,103 (4725–35,436) | 1.06 (3.36–0.14) | 46,716 (10,268–79,844) | 0.98 (10.36–0.13) | −0.09 (−0.19 to 0.12) |
| Musculoskeletal disorders | 137,353 (57,450–225,297) | 6.03 (4.36–1.51) | 356,738 (146,116–581,012) | 6.80 (11.36–1.71) | 0.14 (0.07–0.20) |
| Neoplasms | 31,577 (−1617–142,814) | 5.43 (5.36 to −0.07) | 139,439 (−21,838–580,290) | 7.44 (12.36 to −0.27) | 0.47 (−0.47 to 2.67) |
| Neurological disorders | 38,272 (8106–107,542) | 2.62 (6.36–0.20) | 57,447 (12,864–150,517) | 1.75 (13.36–0.15) | −0.29 (−0.40 to −0.08) |
| Respiratory infections and tuberculosis | 863,066 (477,898–1,316,551) | 37.30 (0.36–13.63) | 1,904,239 (1,072,732–2,864,242) | 34.24 (7.36–12.87) | −0.07 (−0.14 to 0.02) |
| Sense organ diseases | 38,041 (16,523–59,933) | 1.58 (1.36–0.43) | 62,363 (26,317–100,543) | 1.19 (8.36–0.31) | −0.26 (−0.35 to −0.14) |
| Regions | |||||
| Southeast Asia, East Asia, and Oceania | 209,280 (133,212–314,962) | 21.31 (13.51–31.76) | 843,126 (434,145–1,321,468) | 32.18 (16.72–50.06) | 0.51 (0.03–0.87) |
| Central Europe, Eastern Europe, and Central Asia | 313,169 (127,541–516,522) | 70.50 (28.19–116.6) | 482,197 (206,766 - 766,422) | 73.46 (31.57–116.87) | 0.04 (−0.06 to 0.18) |
| High-income | 495,925 (211,655–800,301) | 41.52 (17.71–67.04) | 815,587 (370,336–1,288,209) | 33.19 (15.69–51.55) | −0.20 (−0.25 to −0.09) |
| Latin America and Caribbean | 121,529 (62,408–183,615) | 58.07 (30.04–87.81) | 390,581 (200,873–593,116) | 63.83 (32.60–97.11) | 0.10 (0.01–0.19) |
| North Africa and Middle East | 139,628 (80,646–204,715) | 94.42 (54.85–138.13) | 444,512 (248,383–651,458) | 111.09 (62.99–165.05) | 0.18 (0.05–0.30) |
| South Asia | 91,954 (46,062–155,163) | 16.58 (8.74–27.79) | 448,678 (214,705–698,248) | 31.70 (15.44–49.7) | 0.91 (0.56–1.33) |
| Sub-Saharan Africa | 88,048 (53,414–136,421) | 45.76 (27.18–70.37) | 284,382 (160,256–427,513) | 67.34 (38.78–102.13) | 0.47 (0.29–0.66) |
| World Bank regions | 825,830 (405,994–1,298,931) | 24.19 (11.59–37.98) | 3,701,337 (1,843,736–5,646,169) | 44.19 (21.98–67.58) | 0.83 (0.72–0.97) |
| WHO region | 1,448,757 (717,769–2,270,841) | 40.84 (19.84–64.08) | 3,684,012 (1,835,234–5,618,806) | 44.25 (22.01–67.65) | 0.08 (0.01–0.15) |
| European union | 300,328 (130,095–482,020) | 50.23 (21.68–80.72) | 419,910 (198,142–672,566) | 37.28 (17.88–59.34) | −0.26 (−0.32 to −0.15) |
| League of Arab States | 93,700 (54,474–138,019) | 101.80 (58.54–149.61) | 314,703 (177,705–467,749) | 130.76 (75.14–195.39) | 0.28 (0.11–0.45) |
| Commonwealth | 221,787 (107,464–356,741) | 28.87 (14.05–46.35) | 741,090 (356,775–1,136,519) | 38.31 (18.41–59.14) | 0.33 (0.20–0.48) |
| OECD Countries | 608,719 (263,354–978,455) | 45.88 (19.90–73.72) | 1,077,196 (511,582–1,688,391) | 39.26 (19.08–60.51) | −0.14 (−0.20 to −0.02) |
| G20 | 1,045,845 (498,668–1,651,416) | 38.33 (17.91–60.41) | 2,508,139 (1,216,695–3,877,430) | 38.98 (18.96–60.30) | 0.02 (−0.05 to 0.09) |
| African union | 151,517 (90,193–228,330) | 60.15 (35.72–89.11) | 491,144 (275,282–731,417) | 86.48 (49.45–129.8) | 0.44 (0.26–0.60) |
| Four World regions | 1,453,713 (720,260–2,278,004) | 40.82 (19.84–64.04) | 3,698,546 (1,842,234–5,642,121) | 44.19 (21.98–67.58) | 0.08 (0.01–0.15) |
| World bank income levels | 1,456,672 (721,695–2,282,563) | 40.86 (19.86–64.11) | 3,704,134 (1,845,217–5,650,715) | 44.21 (21.99–67.61) | 0.08 (0.01–0.15) |
| Nordic region | 14,360 (5312–23,981) | 37.09 (13.88–61.66) | 16,769 (7097–27,654) | 25.05 (10.77–41.28) | −0.32 (−0.39 to −0.16) |
| Organization of Islamic Cooperation | 244,516 (137,488–372,008) | 52.41 (29.85–78.55) | 806,667 (439,001–1,198,877) | 71.57 (39.42–107.21) | 0.37 (0.24–0.49) |
| Association of Southeast Asian Nations | 53,733 (32,894–83,980) | 21.96 (13.48–33.99) | 222,760 (118,705–342,708) | 35.86 (19.44–55.15) | 0.63 (0.37–0.88) |
| Gulf Cooperation Council | 7520 (3992–11,670) | 105.29 (56.86–163.13) | 35,910 (20,177–51,894) | 137.46 (76.71–201.14) | 0.31 (0.07–0.63) |
| Sahel region | 28,578 (16,831–44,670) | 48.03 (28.28–74.92) | 80,107 (44,088–123,263) | 62.89 (34.89–96.41) | 0.31 (0.10–0.56) |
| Health system grouping levels | 1,456,701 (721,713–2,282,604) | 40.86 (19.86–64.11) | 3,704,180 (1,845,244–5,650,779) | 44.21 (22–67.61) | 0.08 (0.01–0.15) |
Abbreviations: BMI, high body mass index; CI, confidence interval; SDI, Socio-demographic Index; UI, uncertainty intervals.
Table 2.
DALYs and age-standardized DALYs rates of high BMI in 1990 and 2021 and the temporal trend of age-standardized DALYs rates from 1990 to 2021.
| 1990 |
2021 |
Relative change in age-standardized DALYs rate, 1990–2021 (95% CI) | |||
|---|---|---|---|---|---|
| No. DALYs cases (95% UI) | Age-standardized DALYs rates per 100,000 (95% UI) | No. DALYs cases (95% UI) | Age-standardized DALYs rates per 100,000 (95% UI) | ||
| Global | 48,042,109 (21,178,404–77,317,173) | 1189.69 (522.74–1915.93) | 128,520,083 (55,989,249–202,388,462) | 1493.24 (648.20–2350.72) | 0.26 (0.17–0.34) |
| Sex | |||||
| Female | 26,097,463 (11,042,501–42,206,794) | 1219.65 (517.22–1973.78) | 67,213,786 (28,417,735–105,552,569) | 1483.07 (629.86–2327.33) | 0.22 (0.13–0.30) |
| Male | 21,944,646 (10,106,039–35,110,379) | 1141.04 (531.56–1819.10) | 61,306,297 (27,566,755–94,931,875) | 1497.29 (673.38–2322.15) | 0.31 (0.21–0.40) |
| SDI | |||||
| Low SDI | 2,468,140 (1,381,991–4,049,774) | 969.81 (540.86–1583.95) | 7,889,939 (3,922,665–12,376,646) | 1346.99 (674.20–2106.27) | 0.39 (0.21–0.57) |
| Low-middle SDI | 6,286,643 (3,073,215–10,180,681) | 938.73 (471.39–1504.69) | 24,642,855 (11,581,774–38,153,751) | 1598.37 (751.34–2480.38) | 0.70 (0.50–0.87) |
| Middle SDI | 11,315,469 (5,727,436–17,561,040) | 1014.16 (526.82–1571.85) | 40,789,161 (18,222,014–62,362,498) | 1488.92 (668.95–2281.19) | 0.47 (0.26–0.58) |
| High-middle SDI | 13,456,764 (5,557,920–21,736,296) | 1361.36 (558.23–2199.25) | 28,327,365 (11,609,614–45,257,815) | 1482.16 (608.58–2355.15) | 0.09 (0.01–0.17) |
| High SDI | 14,426,131 (5,751,872–23,595,458) | 1349.13 (539.85–2203.07) | 26,714,020 (10,995,809–41,789,440) | 1457.17 (627.77–2256.99) | 0.08 (−0.01 to 0.19) |
| Causes | |||||
| Cardiovascular diseases | 21,082,657 (11,331,044–32,461,613) | 535.01 (291.22–821.15) | 45,426,879 (23,767,187–69,603,288) | 529.00 (277.28–808.64) | −0.01 (−0.09 to 0.06) |
| Chronic respiratory diseases | 2,253,937 (1,125,455–3,432,736) | 50.53 (24.72–78.10) | 3,283,296 (1,620,702–5,034,164) | 39.42 (19.62–60.16) | −0.22 (−0.29 to −0.13) |
| Diabetes and kidney diseases | 13,104,970 (6,710,991–18,815,930) | 320.65 (162.23–465.23) | 49,731,775 (27,183,231–69,950,744) | 574.62 (314.16–807.45) | 0.79 (0.67–0.94) |
| Digestive diseases | 1,324,282 (287,806–2,380,137) | 32.27 (6.95–57.57) | 2,802,393 (641,037–4,835,769) | 32.89 (7.50–56.74) | 0.02 (−0.06 to 0.12) |
| Musculoskeletal disorders | 4,717,812 (371,436–10,245,415) | 110.57 (8.37–240.46) | 13,400,010 (1,048,084–28,718,885) | 155.33 (12.24–332.41) | 0.40 (0.34–0.47) |
| Neoplasms | 3,549,049 (1,548,429–5,731,481) | 87.53 (37.43–141.83) | 8,894,525 (3,751,953–14,385,271) | 102.17 (43.24–165.02) | 0.17 (0.08–0.23) |
| Neurological disorders | 644,750 (−42,107–2,422,441) | 21.39 (−1.39–80.20) | 2,665,746 (−494,345–9,332,493) | 32.86 (−5.97–115.18) | 0.54 (0.10–2.94) |
| Respiratory infections and tuberculosis | 1,296,112 (256,345–3,776,109) | 29.91 (6.01–86.03) | 2,066,810 (446,316–5,536,306) | 24.05 (5.18–64.58) | −0.20 (−0.31 to 0.03) |
| Sense organ diseases | 68,540 (−1906–165,947) | 1.84 (−0.05–4.48) | 248,650 (−13,061–579,751) | 2.91 (−0.15–6.79) | 0.59 (0.36–1.62) |
| Regions | |||||
| Southeast Asia, East Asia, and Oceania | 7,972,187 (4,497,186–12,493,796) | 659.23 (379.70–1031.99) | 31,031,603 (13,226,316–49,136,271) | 1100.63 (478.05–1746.16) | 0.67 (0.24–0.93) |
| Central Europe, Eastern Europe, and Central Asia | 9,418,518 (3,651,238–15,443,012) | 2008.27 (780.70–3287.69) | 13,789,576 (5,658,981–22,092,071) | 2189.72 (898.17–3505.03) | 0.09 (0.00–0.20) |
| High-income | 14,936,271 (5,897,635–24,372,439) | 1299.67 (515.44–2118.25) | 26,139,558 (10,499,378–41,015,537) | 1371.22 (579.46–2121.93) | 0.06 (−0.04 to 0.16) |
| Latin America and Caribbean | 4,550,785 (2,085,209–7,043,071) | 1881.69 (865.03–2905.67) | 14,073,821 (6,522,934–21,037,056) | 2227.31 (1031.03–3335.41) | 0.18 (0.10–0.27) |
| North Africa and Middle East | 4,542,622 (2,313,706–6,876,469) | 2526.69 (1321.48–3786.86) | 15,774,861 (7,841,442–23,600,021) | 3247.44 (1609.13–4855.73) | 0.29 (0.16–0.41) |
| South Asia | 3,612,123 (1,610,431–6,096,514) | 543.83 (252.26–913.62) | 17,553,020 (7,566,331–27,474,915) | 1098.12 (475.32–1719.6) | 1.02 (0.70–1.36) |
| Sub-Saharan Africa | 3,009,604 (1,650,519–4,816,184) | 1288.99 (708.52–2050.68) | 10,157,644 (5,017,330–15,818,678) | 1898.45 (945.08–2932.51) | 0.47 (0.31–0.63) |
| World Bank Regions | 47,906,166 (21,121,531–77,097,280) | 1188.20 (522.09–1913.51) | 128,277,498 (55,876,040–202,010,595) | 1492.27 (647.69–2349.24) | 0.26 (0.17–0.34) |
| WHO region | 47,688,874 (21,020,965–76,788,067) | 1188.19 (522.04–1914.43) | 127,682,162 (55,639,354–201,113,478) | 1492.98 (648.19–2350.74) | 0.26 (0.17–0.34) |
| European Union | 8,428,331 (3,406,036–13,723,281) | 1461.20 (589.22–2373.18) | 11,106,470 (4,310,550–17,860,250) | 1267.93 (506.44–2022.55) | −0.13 (−0.19 to −0.07) |
| League of Arab States | 3,056,198 (1,602,889–4,593,954) | 2708.37 (1461.43–4053.07) | 11,408,470 (5,753,042–16,990,011) | 3713.32 (1893.44–5560.98) | 0.37 (0.22–0.53) |
| Commonwealth | 7,732,670 (3,348,346–12,866,477) | 846.76 (366.51–1409.62) | 27,868,080 (12,140,569–43,551,500) | 1283.19 (559.36–2009.60) | 0.52 (0.36–0.68) |
| OECD Countries | 18,642,094 (7,576,845–30,190,134) | 1434.51 (584.48–2319.57) | 34,746,848 (14,372,327–53,679,642) | 1554.11 (670.37–2366.55) | 0.08 (0.00–0.19) |
| G20 | 34,214,590 (14,641,752–55,454,396) | 1115.25 (477.73–1807.32) | 85,493,105 (35,825,698–134,094,642) | 1346.35 (565.80–2114.31) | 0.21 (0.12–0.29) |
| African Union | 5,037,264 (2,618,826–7,851,120) | 1639.26 (874.05–2528.10) | 17,235,050 (8,674,459–26,019,866) | 2415.7 (1222.07–3635.08) | 0.47 (0.31–0.63) |
| Four World Regions | 47,855,321 (21,095,443–77,027,750) | 1187.53 (521.73–1912.67) | 128,185,788 (55,838,414–201,884,619) | 1491.84 (647.51–2348.75) | 0.26 (0.17–0.34) |
| World Bank Income Levels | 47,952,176 (21,140,154–77,173,043) | 1188.79 (522.33–1914.48) | 128,361,805 (55,916,035–202,142,032) | 1492.69 (647.91–2349.89) | 0.26 (0.17–0.34) |
| Nordic Region | 399,165 (146,287–664,556) | 1154.19 (426.71–1916.65) | 479,516 (175,707–787,612) | 949.22 (360.87–1546.95) | −0.18 (−0.25 to −0.10) |
| Organization of Islamic Cooperation | 8,246,518 (4,084,511–12,898,204) | 1479.44 (744.85–2301.14) | 29,894,508 (14,423,277–45,038,509) | 2157.72 (1040.46–3257.70) | 0.46 (0.33–0.58) |
| Association of Southeast Asian Nations | 2,065,164 (1,101,511–3,295,373) | 728.50 (394.16–1167.96) | 8,601,899 (3,947,409–13,389,979) | 1247.70 (578.04–1955.85) | 0.71 (0.47–0.94) |
| Gulf Cooperation Council | 275,454 (136,331–424,694) | 2904.59 (1450.77–4483.04) | 1,694,469 (881,404–2,462,284) | 4012.53 (2092.75–5867.85) | 0.38 (0.13–0.72) |
| Sahel region | 960,105 (514,358–1,532,975) | 1365.44 (732.51–2172.67) | 3,050,986 (1,537,485–4,728,889) | 1841.60 (918.23–2842.58) | 0.35 (0.16–0.56) |
| Health system grouping levels | 47,953,147 (21,140,711–77,174,479) | 1188.81 (522.34–1914.51) | 128,363,341 (55,916,850–202,144,164) | 1492.71 (647.92–2349.91) | 0.26 (0.17–0.34) |
Abbreviations: BMI, high body mass index; CI, confidence interval; DALYs, deaths and disability-adjusted life years; SDI, Socio-demographic Index; UI, uncertainty intervals.
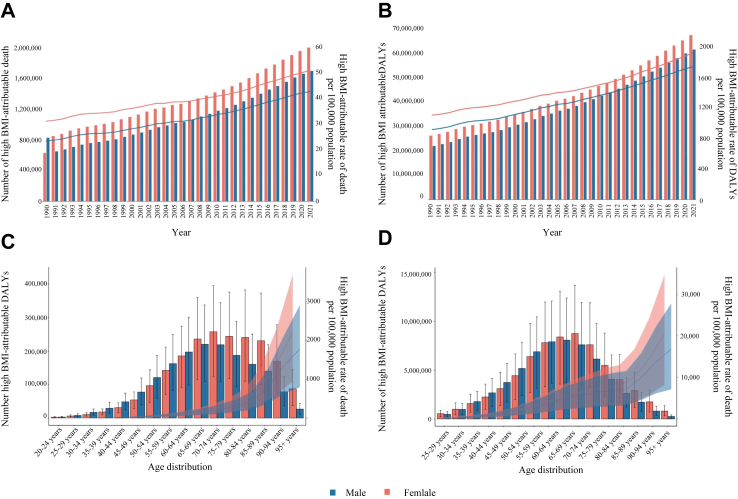
Fig. 1.
(A) Temporal trend of death numbers and rates attributable to high BMI by females and males from 1990 to 2021; (B) Temporal trend of DALYs numbers and rates attributable to high BMI by females and males from 1990 to 2021; (C) Death numbers and rates attributable to high BMI by sex and age distribution; (D) DALYs numbers and rates attributable to high BMI by sex and age distribution. Abbreviations: DALYs, deaths and disability-adjusted life years.
From 2019 to 2020, the age-standardized death rates increased slightly from 44.1 to 44.13 per 100,000 population, and the age-standardized DALY rates rose from 1464.6 to 1477.85 per 100,000 population. During the COVID-19 pandemic (2020–2021), the death rates slightly increased from 44.13 to 44.23 per 100,000 population, while the DALY rates further rose from 1477.85 to 1493.24 per 100,000 population. These increases during the COVID-19 pandemic were more pronounced than in previous periods. Furthermore, the global DALYs attributable to high BMI have increased from 26.1 million (95% UI 11.0 million, 42.2 million) in 1990 to 67.2 million (95% UI 28.4 million, 105.6 million) in 2021 for females, and from 21.9 million (95% UI 10.1 million, 35.1 million) in 1990 to 61.3 million (95% UI 94.9 million, 27.6 million) in 2021 for males. Despite these increases, the age-standardized rates of high BMI-attributable deaths remained stable for females and increased by 15.0% for males between 1990 and 2021. Similarly, the age-standardized rates of high BMI-attributable DALYs only increased by 21.7% for females and 31.2% for males during the same period.
The rates of high BMI-attributable deaths and DALYs increased with age, and this pattern was consistent for both females and males (Fig. 1C and D). In age groups younger than 75 years, high BMI-attributable death and DALYs rates were lower in females than males, but in age groups 65 years and older, these rates were higher in females than in males. The number of high BMI-attributable deaths peaked in the 70–74 age group for females, while for males, the peak was observed in the 65–69 age group. The number of high BMI-attributable DALYs peaked in the 65–59 and 60–64 age groups for females and males. Additionally, the numbers of high BMI-attributable deaths and DALYs were lower in females than in males in age groups under 60 years, while the numbers were higher in females than males in age groups 60 years and older.
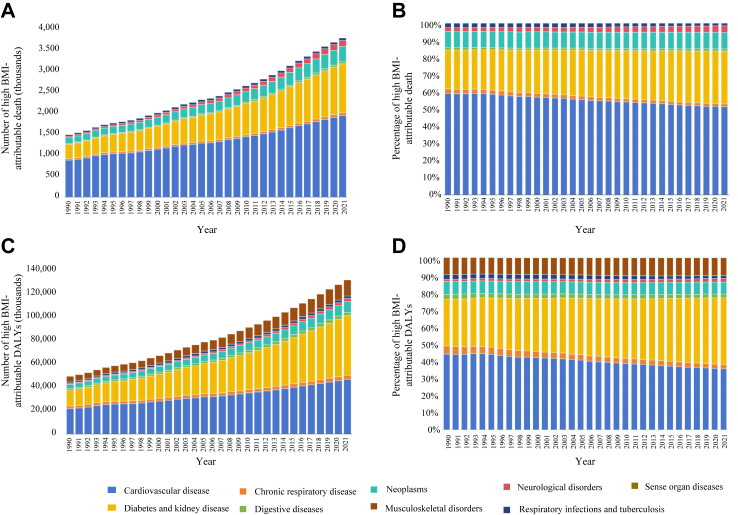
Impact of high BMI on GBD level 2 and 3 causes
In 2021, across GBD level-2 causes, cardiovascular disease and the composite of diabetes and kidney diseases were the two primary contributors to high BMI-attributable DALYs. The absolute number of DALYs for cardiovascular disease and the composite of diabetes and kidney diseases was 1.9 million and 1.1 million, respectively. The age-standardized DALY rates were 497.3 (95% UI 271.8, 699.5) per 100,000 people for cardiovascular disease and 496.7 (95% UI 347.2, 679.6) per 100,000 people for the composite of diabetes and kidney diseases (Fig. 2). This was followed by musculoskeletal disorders, with a DALY rate of 134.0 (95% UI 104.8, 287.2) per 100,000 people, and neoplasms, with a DALY rate of 88.9 (95% UI 37.5, 143.9) per 100,000 people. Together, these accounted for 91.4% of all high BMI-attributable DALYs. Additionally, 39.6% (95% UI 21.3%, 54.6%) of all diabetes and kidney diseases age-standardized DALYs worldwide were attributable to high BMI. In comparison, the corresponding proportions were 38.3% (95% UI 28.4%, 48.7%) for cardiovascular disease and 4.6% (95% UI 2.7%, 7.1%) for musculoskeletal disorders. Similar patterns were observed for deaths. GBD level 2 causes of high BMI-attributable DALYs and deaths with age distribution are shown in Supplement Figure S1. From 1990 to 2010, age-standardized death and DALYs rates of diabetes significantly increased and became comparable to those of CVD (Supplement Figure S2A and C). High BMI contributes significantly to the burden of several GBD level-3 causes (Supplement Tables S1 and S2). Specifically, for every 100,000 people, the attributable DALYs due to high BMI were highest for diabetes mellitus, ischemic heart disease, hypertensive heart disease, chronic kidney disease, low back pain, and stroke. The absolute numbers of DALYs for these conditions were 39.3 million for diabetes mellitus, 23.9 million for ischemic heart disease, 12.6 million for hypertensive heart disease, 10.4 million for chronic kidney disease, 8.3 million for low back pain, and 7.6 million for stroke. For every 100,000 people, the absolute number of deaths due to high BMI was highest for ischemic heart disease, diabetes mellitus, hypertensive heart disease, chronic kidney disease, stroke, and Alzheimer's and other dementias. The absolute numbers of deaths for these conditions were, respectively, 1.0 million for ischemic heart disease, 0.7 million for diabetes mellitus, 0.6 million for hypertensive heart disease, 0.4 million for chronic kidney disease, 0.3 million for stroke, and 0.1 million for Alzheimer's and other dementias.
Fig. 2.
(A) Temporal trend of the number of deaths by GBD level 2 causes attributable to high BMI from 1990 to 2021; (B) Temporal trend of the contribution of GBD level 2 causes for deaths attributable to high BMI from 1990 to 2021; (C) Temporal trend of the number of DALYs attributable to high BMI by GBD level 2 causes from 1990 to 2021; (D) Temporal trend of the contribution of GBD level 2 causes for DALYs attributable to high BMI from 1990 to 2021. Abbreviations: DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study.
Impact of high BMI on GBD super-region
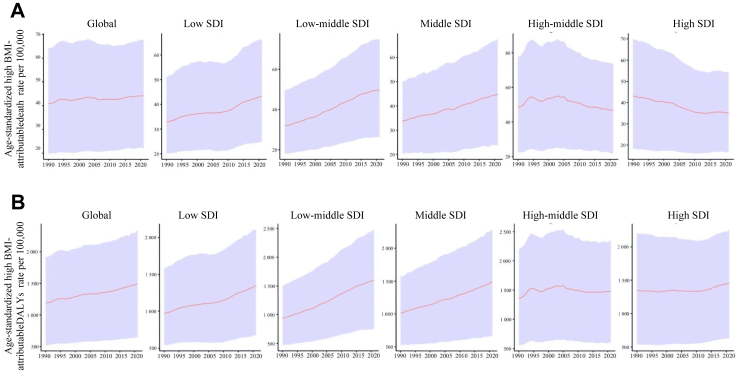
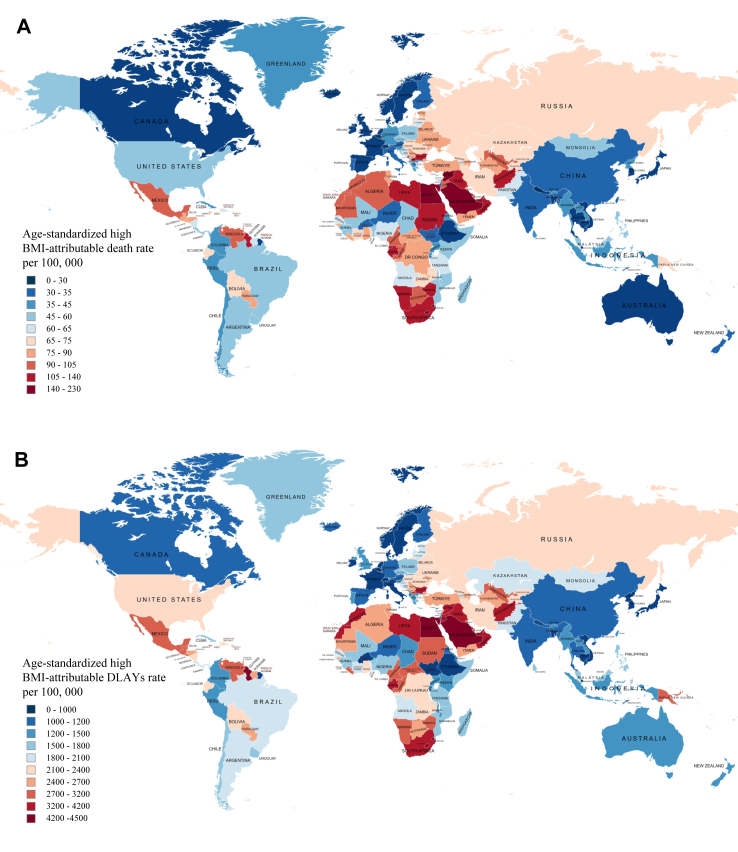
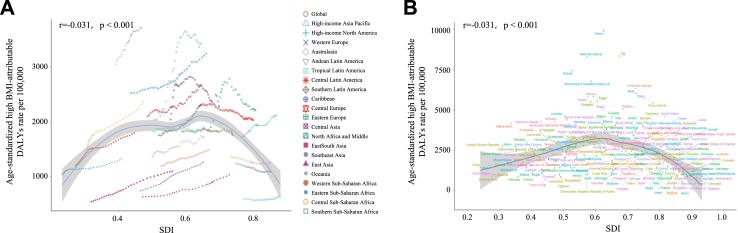
Temporal trends of age-standardized death and DALY rates in each region from 1990 to 2021 are shown in Fig. 3. The burden of high BMI increased worldwide between 1990 and 2021, especially in the Middle East, and it remains a significant challenge in those regions and others (Fig. 4). The countries with the highest age-standardized rates of high BMI-attributable deaths and DALYs are those in the high-SDI quintile, with 44.9 (95% UI 29.3, 62.2) deaths per 100,000 people and 1462.3 (95% UI 1007.4, 1963.7) DALYs per 100,000 people, as well as the low SDI quintile with 38.8 (95% UI 19.8, 63.1) deaths per 100,000 people and 1240.2 (95% UI 672.0, 1912.3) DALYs per 100,000 people. Conversely, the countries with high SDI had the lowest age-standardized DALY rates, and those with low-middle SDI had the highest. Fig. 5 shows the association between DALY rates and SDI across countries. As SDI increases, the age-standardized DALY rates initially rise until SDI reaches approximately 0.50, which begins to decrease with higher SDI values exceeding 0.65. The age-standardized death and DALY rates attributable to high BMI in 2021 by 204 countries and territories were shown in Supplement Tables S3 and S4. Across countries, six countries (Nauru, Fiji, Marshall Islands, Kiribati, Egypt, and Eswatini) had the highest mortality rates. The DALYs and age-standardized DALYs rates were the highest in Nauru, Fiji and the Marshall Islands. From 1990 to 2021, most GBD super regions experienced an increase in age-standardized rates of high BMI-attributable deaths and DALYs. Only the Nordic region and European Union experienced a decline in the age-standardized rate of high BMI-attributable deaths during the study period. Across all countries and territories, six countries (Zimbabwe, Lesotho, Pakistan, India, Indonesia, and Libya) experienced the highest increase in the age-standardized rates of high BMI-attributable deaths and DALYs. Six countries (Ethiopia, Norway, Greenland, Czechia, Ireland, and Germany) experienced the highest decline in the age-standardized rate of high BMI-attributable DALYs during the study period. Age-standardized deaths and DALYs rates by GBD level-2 causes and GBD super-region in 2021 were shown in Supplement Figure S2B and D.
Fig. 3.
(A) Temporal trend of age-standardized death rates attributable to high BMI from 1990 to 2021 globally and regionally; (B) Temporal trend of age-standardized DALYs rates attributable to high BMI from 1990 to 2021 globally and regionally. Abbreviations: DALYs, deaths and disability-adjusted life years; SDI, Socio-demographic Index.
Fig. 4.
(A) Age-standardized DALY rates attributable to high BMI in 2021; (B) Age-standardized DALYs rates attributable to high BMI in 2021. Abbreviations: BMI, high body mass index; DALYs, deaths and disability-adjusted life years.
Fig. 5.
(A) Age-standardized DALYs rates attributable to high BMI across GBD super-region by SDI from 1990 to 2021; (B) Age-standardized DALYs rates attributable to high BMI across 204 countries and territories by SDI in 2021 Abbreviations: DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study; SDI, Socio-demographic Index.
Discussion
Our systematic analysis of the recent and publicly available GBD 2021 database on the disease burden and trends attributable to high BMI indicates a significant and constant increase in the global rates of high BMI over the past 30 years among individuals aged ≥20 years. There are significant differences between countries and diseases in the levels and changes in high BMI, with specific regional trends.
The analysis shows that from 1990 to 2021, high BMI-attributable deaths and DALYs have increased significantly for both males and females, but with notable differences. Females experienced a substantial rise in the absolute numbers of deaths and DALYs, while males showed a more significant increase in age-standardized rates of these metrics. For females, age-standardized rates remained substantially stable, indicating a growing burden without a change in relative risk, whereas males experienced a 15.0% rise in death rates and a 31.2% rise in DALYs. These differences highlight the need for gender-specific public health strategies to address the rising global impact of high BMI. Despite the widespread recognition of the obesity epidemic, there is a significant gap in effectively applying interventions for the prevention and management of obesity.25 Efforts to explain the significant increase in the global rates of high BMI over the past three decades have focused on various factors, including lifestyle changes, reduced physical activity, and dietary changes.26,27 First, the rise in global high BMI rates directly results from lifestyle changes accompanying social and demographic transitions that started several decades ago.28,29 The world is facing similar challenges due to swift economic, demographic, and lifestyle changes, such as changes in food consumption, decreased physical activity, and increased sedentary behavior.28,30 Second, the reduced energy expenditure among adults because of changes in work and transportation methods may also play a role in the increasing global rates of high BMI. During the COVID-19 pandemic (2020–2021), the increases in age-standardized death and DALY rates were more pronounced compared to the pre-pandemic period (2019–2020). This worsening may be likely due to increased sedentary behaviors, healthcare disruptions, and heightened stress, which likely exacerbate existing health issues.31,32 Additionally, the prevalence of high BMI is rising globally due to changes in global food systems and consumption patterns driven by economic and technological influences.33,34 High levels of ultra-processed food (UPF), hyper-palatable foods (HPF), and high energy density (HED) are contributing to this trend.35,36 These foods are affordable and convenient, leading to increased consumption and coinciding with rising obesity rates. In contrast, fiber-rich foods like whole grains and fruits make up a smaller portion of the food supply and are less consumed, resulting in the intake of higher calories and subsequent weight gain.37
Our findings indicate that CVD and the composite of diabetes and kidney diseases were the two leading causes of death and disability-adjusted life-years attributable to high BMI. The DALYs for diabetes and kidney diseases have increased significantly with an annual percentage change in age-standardized DALYs rates of 0.79 (0.67–0.94). Conversely, the DALYs for CVD have remained stable with an annual percentage change in age-standardized DALY rates of −0.01 (−0.09 to 0.06). At the GBD level 3, diabetes mellitus has surpassed ischemic heart disease and hypertensive heart disease, becoming the leading cause attributable to high BMI. The updated study on the global burden of diabetes also reported that a high BMI is the primary risk factor for type 2 diabetes, contributing to more than 50% of global DALYs in 2021.38 In recent decades, there has been a growing correlation between high BMI and type 2 diabetes, with exposure increased considerably between 2000 and 2021.6 Childhood obesity is a growing global concern, with increasing prevalence in both high- and low-income countries.39,40 This condition poses significant health risks, including type 2 diabetes and cardiovascular disease, and can lead to long-term chronic issues if not addressed.41 Additionally, childhood obesity has psychosocial effects, such as stigma and lower self-esteem, which may further complicate management and treatment.42 However, the management of high BMI seems to be a more significant challenge than glycemic control, primarily because patients often find it difficult to use effective and inexpensive drugs and adhere to exercise programs consistently.43 Medical professionals may use obesity medications or bariatric surgery as alternative treatments.15,44 Despite their effectiveness in reducing weight, these interventions have drawbacks such as high costs and adverse effects like nausea, vomiting, diarrhea, and neuropathy.15,25 Although pharmaceutical interventions aimed at controlling hypertension and reducing plasma low-density lipoprotein cholesterol levels may provide partial benefit, they are insufficient in significantly decreasing the majority of metabolic disease risks attributable to high BMI.45
We analyzed the impact of metabolic risks and found significant regional disparities. In May 2022, the World Health Organization (WHO) reported that ∼60% of European citizens are overweight or obese.46 Nearly one-third of the global population could be classified as overweight or obese, with a prevalence exceptionally high in developed countries in the future.46 Our research findings indicate that high BMI-attributable DALYs have increased in almost every region over the past 30 years, except for high SDI regions, where they remain stable. We would like to be optimistic that the obesity epidemic has peaked in the developed world. The burden and increase in deaths and DALYs attributable to high BMI were more significant for countries with low-middle SDI but not low SDI. In low-income regions, most of the population lacks access to high-protein dietary options. Instead, their diet predominantly includes carbohydrates sourced from rice and other readily available food items. This nutritional pattern is also marked by a higher intake of calories, animal products, and sugars.47 These factors may lead to a transition to less healthy food choices, which may worsen issues related to high BMI. However, our analysis of the GBD 2021 database does not explain why the low SDI region has experienced slower rates of increase in high BMI. Thus, the complexity of the relationship between high BMI and SDI reasonably suggests that changes in the burden attributable to high BMI cannot be fully explained by analyzing income levels or SDI levels. Although high BMI-attributable death rates and DALY rates have declined in some regions, such as Ireland, this trend contrasts with broader data indicating that CVD deaths have plateaued and obesity rates continue to rise. Despite improvements in some health metrics, many high-income nations, such as Ireland, are experiencing stagnation in life expectancy, suggesting that other factors may offset gains in high BMI-related outcomes. This discrepancy underscores the need for a nuanced analysis of regional health trends, considering factors such as healthcare advancements, public health policies, and socioeconomic changes.
The increase in obesity has significant implications for the disease burden worldwide, yet the current approach to addressing obesity is often disjointed and fragmented. There is a pressing global need to prevent obesity (starting from childhood and adolescence), promote weight loss, and reduce the risk of disease in individuals struggling with high BMI.48 High BMI is a whole-of-society and system-level problem requiring multi-stakeholder actions.49 Governments and communities must vigorously implement evidence-based policies to achieve global targets for controlling high BMI.50 Researchers should work on understanding how high BMI is changing globally and develop strategies to encourage behavioral changes.51 However, the effectiveness of ‘behavioral’ changes in tackling the obesity epidemic is debatable vis-a-vis structural population-level interventions.52 The debate between behavioral changes and structural population-level interventions in tackling obesity focuses on their respective impacts and effectiveness.52 Behavioral changes focus on individual habits and can yield short-term results, but they often fail to produce long-lasting effects without ongoing support.53 In contrast, structural interventions address broader environmental and systemic factors, potentially leading to widespread public health improvements.54 While behavioral strategies are helpful, they are usually limited in scope compared to structural changes that reshape the environment to support healthier choices on a larger scale.55 It is reasonable that a combined approach might offer the most comprehensive solution to the obesity epidemic.52 Public health policymakers should allocate funding and prioritize this important issue on their agendas.56 Early intervention is crucial, and efforts should begin with parents and families to develop education and awareness, starting with the youngest members of society.57 This can be achieved through targeted funding, food aid such as healthy food subsidies or coupons, free healthy school meals, and primary care-based nutrition interventions.58
This study has significant limitations that should be discussed. General limitations of the GBD methodology are described in more detail elsewhere.6,16 First, the methodology adopted for the GBD study involves the inclusion of surveys based on self-reported data regarding body weight and height. To mitigate this issue, the GBD study incorporates a correction method for the self-reported data, employing observed relationships from datasets that include self-reported and directly measured weights and heights. Second, while BMI is a convenient measure of body fat, it does not fully consider the differences in body composition and regional fat distribution between different ethnic groups. Specifically, BMI cannot distinguish between lean and fat mass, as it does not consider bone density and body composition. Additionally, the GBD 2021 database does not address disability weights or the life expectancy methods used. Third, using a universal cutoff point for BMI may underestimate the rates of high BMI in some countries. However, BMI is based on measures easily collected at the population level. Fourth, the analyses employed in this manuscript are downloaded from the GBD Compare/GHDx database, which is in public domain and we have included updated analyses to 2021. Fifth, the GBD study does not provide data on the prevalence of high BMI. Consequently, we are unable to include this information in our analysis. Sixth, childhood obesity was not a focus of the present analysis despite its increasing global prevalence and significance.
In conclusion, this study provides a comprehensive update on the global trends and burden of high BMI to 2021 using the recent and publicly available GBD 2021 database. The prevalence of high BMI has increased globally over the past 30 years (from 2019 to 2021) and is a significant factor in the global burden of disease. The increasing global rates of high BMI and the associated disease burden highlight the urgent and continuing need for regular surveillance and monitoring of BMI, as well as the analysis and identification of the main risk factors that may be different across regions and countries.
Contributors
All authors approve the final version of the manuscript, including the authorship list and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have read and approved the final version of the manuscript for submission. Conceptualization: X-D Zhou and M-H Zheng; Data curation and formal analysis: X-D Zhou, Q-F Chen and M-H Zheng; Accessed and verified the data: X-D Zhou and Q-F Chen; Writing, review, and editing: X-D Zhou, Q-F Chen, W Yang, M Zuluaga, G Targher, CD. Byrne, L Valenti, F Luo, CS. Katsouras, O Thaher, A Misra, K Ataya, RJ. Oviedo, AP Kong, K Alswat, A Lonardo, YJ Wong, A Abu-Abeid, HA Momani, A Ali, GA Molina, O Szepietowski, N Adxamovich Jumaev, MC Kızılkaya, O Viveiros, CJ Toro-Huamanchumo, KYY Kok, O Ospanov, SI Abbas, AG Robertson, Y Fouad, CS. Mantzoros, HJ Zhang, N Méndez-Sánchez, S Sookoian, W-K Chan, S Treeprasertsuk, L Adams, P Ocama, JD. Ryan, N Perera, AI. Sharara, SA. Al-Busafi, CK Opio, M Garcia, MC Lim-Loo, E Ruiz-Úcar, A Prasad, A Casajoana, TN. Abdelbaki, and M-H Zheng.
Data sharing statement
GBD study 2021 data resources were available online from the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool).
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
Christopher D. Byrne has received grant support from Echosens. Ming-Hua Zheng has received honoraria for lectures from AstraZeneca, Hisky Medical Technologies and Novo Nordisk, consulting fees from Boehringer Ingelheim. Anoop Misra has received honoraria from Novo Nordisk, AstraZendeca, Janssen, and Boehringer Ingelheim. Wah-Kheong Chan is a consultant or advisory board member for Abbott, Roche, Abbvie, Boehringer Ingelheim and Novo Nordisk; and a speaker for Abbott, Novo Nordisk, Echosens, Viatris and Hisky Medical. No other disclosures were reported; John D. Ryan received consultancy fees from Falk, Gilead, Pfizer and a speaker honorarium from Takeda. Christos S. Mantzoros reports grants through his institution from Merck, Massachusetts Life Sciences Center and Boehringer Ingelheim, has received grants through his Institution and personal consulting fees from Coherus Inc. and AltrixBio, he reports personal consulting fees and support with research reagents from Ansh Inc., collaborative research support from LabCorp Inc., reports personal consulting fees from Olympus, Genfit, Lumos, Novo Nordisk, Amgen, Biodexa, Laekna, Corcept, Intercept, 89 Bio, Madrigal, Aligos, Esperion and Regeneron, travel support and fees from UptoDate, TMIOA, Elsevier, and the Cardio Metabolic Health Conference. The other authors report no disclosure.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (82070588, 82370577), the National Key R&D Program of China (2023YFA1800801).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102848.
Appendix A. Supplementary data
(A) Number of deaths by GBD level 2 causes and age distribution; (B) Contribution of GBD level 2 causes for deaths by age distribution; (C) Number of DALYs by GBD level 2 causes and age distribution; (D) Contribution of GBD level 2 causes for DALYs by age distribution. Abbreviations: BMI, high body mass index; DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study.
(A) Temporal trend of age-standardized death rate by GBD level 2 causes; (B) Age-standardized death rate by GBD level 2 causes and GBD super-region in 2021; (C) Age-standardized DALYs rate by GBD level 2 causes and GBD super-region in 2021. Abbreviations: BMI, high body mass index; DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study.
References
- 1.Singh-Manoux A., Fayosse A., Sabia S., et al. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: a cohort study. PLoS Med. 2018;15(5) doi: 10.1371/journal.pmed.1002571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freisling H., Viallon V., Lennon H., et al. Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: a multinational cohort study. BMC Med. 2020;18(1):5. doi: 10.1186/s12916-019-1474-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou X.D., Targher G., Byrne C.D., et al. An international multidisciplinary consensus statement on MAFLD and the risk of CVD. Hepatol Int. 2023;17(4):773–791. doi: 10.1007/s12072-023-10543-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10352):563–591. doi: 10.1016/s0140-6736(22)01438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yates T., Summerfield A., Razieh C., et al. A population-based cohort study of obesity, ethnicity and COVID-19 mortality in 12.6 million adults in England. Nat Commun. 2022;13(1):624. doi: 10.1038/s41467-022-28248-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2162–2203. doi: 10.1016/s0140-6736(24)00933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X., Ma N., Lin Q., et al. Body roundness index and all-cause mortality among US adults. JAMA Netw Open. 2024;7(6) doi: 10.1001/jamanetworkopen.2024.15051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hutten C.G., Padalia K., Vasbinder A., et al. Obesity, inflammation, and clinical outcomes in COVID-19: a multicenter prospective cohort study. J Clin Endocrinol Metab. 2024 doi: 10.1210/clinem/dgae273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hendren N.S., de Lemos J.A., Ayers C., et al. Association of body mass index and age with morbidity and mortality in patients hospitalized with COVID-19: results from the American heart association COVID-19 cardiovascular disease registry. Circulation. 2021;143(2):135–144. doi: 10.1161/circulationaha.120.051936. [DOI] [PubMed] [Google Scholar]
- 10.Ioannou G.N., Weiss N.S., Kowdley K.V., Dominitz J.A. Is obesity a risk factor for cirrhosis-related death or hospitalization? A population-based cohort study. Gastroenterology. 2003;125(4):1053–1059. doi: 10.1016/s0016-5085(03)01200-9. [DOI] [PubMed] [Google Scholar]
- 11.Almeda-Valdes P., Aguilar-Salinas C.A., Uribe M., Canizales-Quinteros S., Méndez-Sánchez N. Impact of anthropometric cut-off values in determining the prevalence of metabolic alterations. Eur J Clin Invest. 2016;46(11):940–946. doi: 10.1111/eci.12672. [DOI] [PubMed] [Google Scholar]
- 12.Zhang H., Zhou X.D., Shapiro M.D., et al. Global burden of metabolic diseases, 1990-2021. Metabolism. 2024;160 doi: 10.1016/j.metabol.2024.155999. [DOI] [PubMed] [Google Scholar]
- 13.Tsai A.G., Williamson D.F., Glick H.A. Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes Rev. 2011;12(1):50–61. doi: 10.1111/j.1467-789X.2009.00708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahase E. Global cost of overweight and obesity will hit $4.32tn a year by 2035, report warns. BMJ. 2023;380:523. doi: 10.1136/bmj.p523. [DOI] [PubMed] [Google Scholar]
- 15.Alsaqaaby M.S., Cooney S., le Roux C.W., Pournaras D.J. Sex, race, and BMI in clinical trials of medications for obesity over the past three decades: a systematic review. Lancet Diabetes Endocrinol. 2024;12(6):414–421. doi: 10.1016/s2213-8587(24)00098-6. [DOI] [PubMed] [Google Scholar]
- 16.Dai H., Alsalhe T.A., Chalghaf N., Riccò M., Bragazzi N.L., Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: an analysis of the Global Burden of Disease Study. PLoS Med. 2020;17(7) doi: 10.1371/journal.pmed.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–2161. doi: 10.1016/s0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drucker D.J. Diabetes, obesity, metabolism, and SARS-CoV-2 infection: the end of the beginning. Cell Metab. 2021;33(3):479–498. doi: 10.1016/j.cmet.2021.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chong B., Jayabaskaran J., Kong G., et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. eClinicalMedicine. 2023;57 doi: 10.1016/j.eclinm.2023.101850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fäldt A., Nejat S., Durbeej N., Holmgren A. Childhood overweight and obesity during and after the COVID-19 pandemic. JAMA Pediatr. 2024;178(5):498–500. doi: 10.1001/jamapediatrics.2024.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M.L., Gago C.M. Shifts in child health behaviors and obesity after COVID-19. JAMA Pediatr. 2024;178(5):427–428. doi: 10.1001/jamapediatrics.2024.0027. [DOI] [PubMed] [Google Scholar]
- 22.Le L.T.H., Hoang T.N.A., Nguyen T.T., et al. Sex differences in clustering unhealthy lifestyles among survivors of COVID-19: latent class analysis. JMIR Public Health Surveill. 2024;10 doi: 10.2196/50189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray C.J.L. Findings from the global burden of disease study 2021. Lancet. 2024;403(10440):2259–2262. doi: 10.1016/s0140-6736(24)00769-4. [DOI] [PubMed] [Google Scholar]
- 24.Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2100–2132. doi: 10.1016/s0140-6736(24)00367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laddu D., Neeland I.J., Carnethon M., et al. Implementation of obesity science into clinical practice: a scientific statement from the American heart association. Circulation. 2024;150(1):e7–e19. doi: 10.1161/cir.0000000000001221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seage C.H. A systematic review of the effectiveness of attentional bias modification to support weight management in individuals who are overweight or obese. Obes Rev. 2024;25(7) doi: 10.1111/obr.13745. [DOI] [PubMed] [Google Scholar]
- 27.Khorrami Chokami K., Khorrami Chokami A., Cammarata G., et al. Current perspectives in obesity management: unraveling the impact of different therapy approach in real life obesity care. J Transl Med. 2024;22(1):536. doi: 10.1186/s12967-024-05322-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zink J., Booker R., Wolff-Hughes D.L., et al. Longitudinal associations of screen time, physical activity, and sleep duration with body mass index in U.S. youth. Int J Behav Nutr Phys Act. 2024;21(1):35. doi: 10.1186/s12966-024-01587-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J., Fong D.Y.T., Lok K.Y.W., et al. Key lifestyles and health outcomes across 16 prevalent chronic diseases: a network analysis of an international observational study. J Glob Health. 2024;14 doi: 10.7189/jogh-14-04068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker P., Friel S. Food systems transformations, ultra-processed food markets and the nutrition transition in Asia. Global Health. 2016;12(1):80. doi: 10.1186/s12992-016-0223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gebeyehu D.T., East L., Wark S., Islam M.S. Disability-adjusted life years (DALYs) based COVID-19 health impact assessment: a systematic review. BMC Public Health. 2023;23(1):334. doi: 10.1186/s12889-023-15239-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Global age-sex-specific mortality Life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):1989–2056. doi: 10.1016/s0140-6736(24)00476-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):2793–2807. doi: 10.1098/rstb.2010.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mason-D'Croz D., Bogard J.R., Sulser T.B., et al. Gaps between fruit and vegetable production, demand, and recommended consumption at global and national levels: an integrated modelling study. Lancet Planet Health. 2019;3(7):e318–e329. doi: 10.1016/s2542-5196(19)30095-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hall K.D., Ayuketah A., Brychta R., et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019;30(1):67–77.e3. doi: 10.1016/j.cmet.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sutton C.A., Stratton M., L'Insalata A.M., Fazzino T.L. Ultraprocessed, hyper-palatable, and high energy density foods: prevalence and distinction across 30 years in the United States. Obesity (Silver Spring) 2024;32(1):166–175. doi: 10.1002/oby.23897. [DOI] [PubMed] [Google Scholar]
- 37.Marrón-Ponce J.A., Flores M., Cediel G., Monteiro C.A., Batis C. Associations between consumption of ultra-processed foods and intake of nutrients related to chronic non-communicable diseases in Mexico. J Acad Nutr Diet. 2019;119(11):1852–1865. doi: 10.1016/j.jand.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 38.Global, regional, and National burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023;402(10397):203–234. doi: 10.1016/s0140-6736(23)01301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horesh A., Tsur A.M., Bardugo A., Twig G. Adolescent and childhood obesity and excess morbidity and mortality in young adulthood-a systematic review. Curr Obes Rep. 2021;10(3):301–310. doi: 10.1007/s13679-021-00439-9. [DOI] [PubMed] [Google Scholar]
- 40.Ogden C.L., Fryar C.D., Martin C.B., et al. Trends in obesity prevalence by race and hispanic origin-1999-2000 to 2017-2018. JAMA. 2020;324(12):1208–1210. doi: 10.1001/jama.2020.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishtar S., Gluckman P., Armstrong T. Ending childhood obesity: a time for action. Lancet. 2016;387(10021):825–827. doi: 10.1016/s0140-6736(16)00140-9. [DOI] [PubMed] [Google Scholar]
- 42.Nafiu O.O., Chimbira W.T., Tait A.R. Pediatric preoperative assessment: six million missed opportunities for childhood obesity education. Anesth Analg. 2018;126(1):343–345. doi: 10.1213/ane.0000000000001990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Afshin A., Forouzanfar M.H., Reitsma M.B., et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gilden A.H., Catenacci V.A., Taormina J.M. Obesity. Ann Intern Med. 2024;177(5):itc65–itc80. doi: 10.7326/aitc202405210. [DOI] [PubMed] [Google Scholar]
- 45.Kopp K.O., Glotfelty E.J., Li Y., Lahiri D.K., Greig N.H. Type 2 diabetes mellitus/obesity drugs: a neurodegenerative disorders savior or a bridge too far? Ageing Res Rev. 2024;98 doi: 10.1016/j.arr.2024.102343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chooi Y.C., Ding C., Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. doi: 10.1016/j.metabol.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 47.Springmann M., Clark M.A., Rayner M., Scarborough P., Webb P. The global and regional costs of healthy and sustainable dietary patterns: a modelling study. Lancet Planet Health. 2021;5(11):e797–e807. doi: 10.1016/s2542-5196(21)00251-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187–225. doi: 10.1161/circulationaha.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friel S., Collin J., Daube M., et al. Commercial determinants of health: future directions. Lancet. 2023;401(10383):1229–1240. doi: 10.1016/s0140-6736(23)00011-9. [DOI] [PubMed] [Google Scholar]
- 50.Chiolero A. Why causality, and not prediction, should guide obesity prevention policy. Lancet Public Health. 2018;3(10):e461–e462. doi: 10.1016/s2468-2667(18)30158-0. [DOI] [PubMed] [Google Scholar]
- 51.Spring B., Pfammatter A.F., Scanlan L., et al. An adaptive behavioral intervention for weight loss management: a randomized clinical trial. JAMA. 2024;332(1):21–30. doi: 10.1001/jama.2024.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wolfenden L., Wiggers J. Strengthening the rigour of population-wide, community-based obesity prevention evaluations. Public Health Nutr. 2014;17(2):407–421. doi: 10.1017/s1368980012004958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hall K.D., Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin North Am. 2018;102(1):183–197. doi: 10.1016/j.mcna.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Swinburn B.A., Sacks G., Hall K.D., et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/s0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 55.Roberto C.A., Swinburn B., Hawkes C., et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985):2400–2409. doi: 10.1016/s0140-6736(14)61744-x. [DOI] [PubMed] [Google Scholar]
- 56.Spiga F., Tomlinson E., Davies A.L., et al. Interventions to prevent obesity in children aged 12 to 18 years old. Cochrane Database Syst Rev. 2024;5(5) doi: 10.1002/14651858.CD015330.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Oliveira Otto M.C., Anderson C.A.M., Dearborn J.L., et al. Dietary diversity: implications for obesity prevention in adult populations: a science advisory from the American heart association. Circulation. 2018;138(11):e160–e168. doi: 10.1161/cir.0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hashem K.M., Burt H.E., Brown M.K., MacGregor G.A. Outcomes of sugar reduction policies, United Kingdom of great Britain and northern Ireland. Bull World Health Organ. 2024;102(6):432–439. doi: 10.2471/blt.23.291013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Number of deaths by GBD level 2 causes and age distribution; (B) Contribution of GBD level 2 causes for deaths by age distribution; (C) Number of DALYs by GBD level 2 causes and age distribution; (D) Contribution of GBD level 2 causes for DALYs by age distribution. Abbreviations: BMI, high body mass index; DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study.
(A) Temporal trend of age-standardized death rate by GBD level 2 causes; (B) Age-standardized death rate by GBD level 2 causes and GBD super-region in 2021; (C) Age-standardized DALYs rate by GBD level 2 causes and GBD super-region in 2021. Abbreviations: BMI, high body mass index; DALYs, deaths and disability-adjusted life years; GBD, global burden of disease study.