Abstract
Objective
This study aims to analyze the distribution of otolaryngologists between urban and rural counties in Pennsylvania.
Study Design
Retrospective database.
Setting
American Academy of Otolaryngology–Head and Neck Surgery (AAO‐HNS) database and Centers for Medicare and Medicaid Services (CMS) Database.
Methods
The AAO‐HNS database (Entnet.org) and the CMS Database were used to identify otolaryngologists, their primary location, and their state of training. The 2023 Rural‐Urban Continuum Codes were used to classify metropolitan (codes 1‐3) and nonmetropolitan counties (codes 4‐9) and determine county populations.
Results
A total of 388 otolaryngologists were identified across 67 Pennsylvania counties (33 metropolitan, 34 nonmetropolitan), 80% of which were male. There were 354 otolaryngologists in metropolitan counties serving 11.2 million people, with an average of 2.4 otolaryngologists per 100,000 people (/100 k). The majority of otolaryngologists (n = 235, 60.6%) are located in counties designated by code 1. There were 34 otolaryngologists in nonmetropolitan counties serving 1.8 million people, with an average of 2.4 otolaryngologists/100 k. Montour County (code 6) is home to a large academic center and accounts for 14/34 otolaryngologists in the nonmetropolitan counties. With the exception of Montour County, the remaining nonmetropolitan counties averaged 1.0 otolaryngologist/100 k. Only 3 metropolitan counties did not have otolaryngologists compared to 19 nonmetropolitan counties without otolaryngologists. Most otolaryngologists received their residency training in Pennsylvania (n = 177). New York (n = 35) and Maryland (n = 24) were the second most common states for training.
Conclusion
There is a lack of otolaryngologists in rural counties of Pennsylvania, except in counties home to large academic centers.
Keywords: geospatial analysis, health care disparities, otolaryngology workforce, rural health
Otolaryngology problems are some of the most common conditions encountered in primary and urgent care, affecting nearly 20% of adults and up to 50% of children. 1 , 2 The population aged 65 and older is the fastest‐growing population in the United State. The prevalence of conditions associated with older age, such as head and neck cancer and hearing loss, significantly increases the demand for otolaryngologists. 3 This highlights the importance of access to adequate otolaryngology care to diagnose and manage patients with otolaryngology conditions effectively.
Patients in rural areas are less likely to have access to subspecialty care compared to those in urban areas. 4 As a result, there has been interest in assessing the impact of rurality on health outcomes. 5 Compared to urban populations, those living in rural areas have higher rates of smoking and decreased awareness of the effects of human papillomavirus, 2 major risk factors for head and neck cancers. 6 , 7 Patients living in rural areas have also been reported to present with more advanced disease and higher mortality rates from head and neck cancer compared to their urban counterparts. 8 , 9
A database study of over 9000 otolaryngologists conducted in 2016 reported that otolaryngologists were overrepresented in large metropolitan cities in the United States. 10 Pennsylvania is the fifth most populous state and contains the third largest rural population in the United States. 11 , 12 This study aims to analyze the distribution of otolaryngologists in urban and rural counties in Pennsylvania.
Methods
The American Academy of Otolaryngology–Head and Neck Surgery (AAO‐HNS) database (www.enthealth.org/find-ent/) and the Centers for Medicare and Medicaid Services (CMS) database Medicare Physician and Other Practitioners database were used to identify otolaryngologists in Pennsylvania. Information on the surgeon's primary work location and state of residency training were collected.
The AAO‐HNS database lists all current board‐certified otolaryngologists who are members of the AAO‐HNS and their primary work locations. The latest version (2021) of the CMS data set was used to identify and cross‐reference additional otolaryngologists who may not be listed in the AAO‐HNS database. The CMS data set lists all otolaryngology physicians and provides a summary of information on the services and procedures provided to Medicare (fee‐for‐service) Part B (Medical Insurance) beneficiaries by physicians and other health care professionals. These data sets contain information on use, payments, and submitted charges organized by the National Provider Identifier, Healthcare Common Procedure Coding System code, and geography. 13 Residents and fellows in training were excluded. To ensure that our information was up to date, we searched each physician's name and excluded them if their current practice location was outside of Pennsylvania.
The 2023 Rural‐Urban Continuum Codes were used to classify metropolitan and nonmetropolitan counties and determine county populations. These codes distinguish US metropolitan (metro) counties by the population size of their metro area and nonmetropolitan (nonmetro) counties by their degree of urbanization and adjacency to a metro area. The division of counties, metro and nonmetro, is subdivided into 3 metro and 6 nonmetro categories. Each county and census‐designated county‐equivalent in the United States, including those in outlying territories, is assigned one of these 9 codes. The metro codes are divided into (1) counties in metro areas of 1 million population or more, (2) counties in metro areas of 250,000 to 1 million population, and (3) counties in metro areas of fewer than 250,000 population. The nonmetro areas are as follows: (4) an urban population of 20,000 or more, adjacent to a metro area, (5) an urban population of 20,000 or more not adjacent to a metro area, (6) an urban population of 5000 to 20,000 adjacent to a metro area, (7) an urban population of 50,000 to 20,000, not adjacent to a metro area, (8) an urban population of fewer than 5000 adjacent to a metro area, and (9) an urban population of fewer than 5000, not adjacent to a metro area. The average number of otolaryngologists per 100,000 residents (/100 k) was calculated for each county classification. The US Census was queried to determine the size of each county to calculate the average number of otolaryngologists per 100 square miles for each rural‐urban continuum code county classification.
The websites used for this study are publicly available, and no protected health information was accessed. The Penn State University institutional review board (IRB) determined that IRB review and approval is not required (STUDY00025118).
Results
A total of 388 otolaryngologists were identified, of which 83% were male. Pennsylvania's total population was 13,002,700. Of 67 counties, 33 were considered metropolitan, and 34 were nonmetropolitan. There were 354 otolaryngologists in metropolitan counties serving 11.2 million people, with an average of 2.4 otolaryngologists/100 k. Across the 3 metropolitan counties, the median number of otolaryngologists/100 k was 2.3. The majority of otolaryngologists (n = 235, 60.6%) are located in counties designated by code 1.
There were 34 otolaryngologists in nonmetropolitan counties serving 1.8 million people, with an average of 2.4 otolaryngologists/100 k. Of the 34 nonmetropolitan counties, 19 counties had 0 practicing otolaryngologists. Meanwhile, Montour County (code 6) is home to a large academic center, accounting for 14 of the 34 otolaryngologists in the nonmetropolitan counties. Due to the presence of this academic medical center, this small county averaged 77.19 otolaryngologists/100 k. With the exception of Montour County, the remaining nonmetropolitan counties averaged 1.0 otolaryngologists/100 k. Pennsylvania's total population is distributed across approximately 44,729.9 square miles. In counties designated by code 1, there was an average of 7.49 otolaryngologists/100 square miles. Nonmetropolitan counties had fewer than 1 otolaryngologist/100 square miles, except those designated by code 6, which had an average of 1.05 otolaryngologists/100 square miles. Table 1 summarizes the otolaryngology workforce categorized by the rural‐urban continuum codes.
Table 1.
Distribution of the Otolaryngologists in Pennsylvania by Rural‐Urban Classification
| Rural‐urban classification code | Total population | Total number of otolaryngologists | Average number of otolaryngologists per 100,000 people | Average number of otolaryngologists per 100 square miles |
|---|---|---|---|---|
| 1 | 6,675,131 | 235 | 2.23 | 7.49 |
| 2 | 3,620,675 | 97 | 2.63 | 1.36 |
| 3 | 931,695 | 22 | 2.30 | 0.47 |
| 4 | ‐ | ‐ | ‐ | ‐ |
| 5 | 922,745 | 13 | 1.33 | 0.19 |
| 6 | 497,927 | 19 | 8.09 | 1.05 |
| 7 | 155,650 | 1 | 0.56 | 0.04 |
| 8 | 170,961 | 0 | 0.00 | 0.00 |
| 9 | 27,916 | 1 | 2.03 | 0.03 |
Only 3 metropolitan counties did not have otolaryngologists compared to 19 nonmetropolitan counties without otolaryngologists. Most otolaryngologists completed their residency training in Pennsylvania (n = 177, 45.6%). New York (n = 35, 9.0%) and Maryland (n = 24, 6.2%) were the second and third most common states for training. Nineteen surgeons (4.8%) graduated from a non‐US residency program. A geospatial analysis of the distribution of otolaryngologists across Pennsylvania can be seen in Figure 1.
Figure 1.
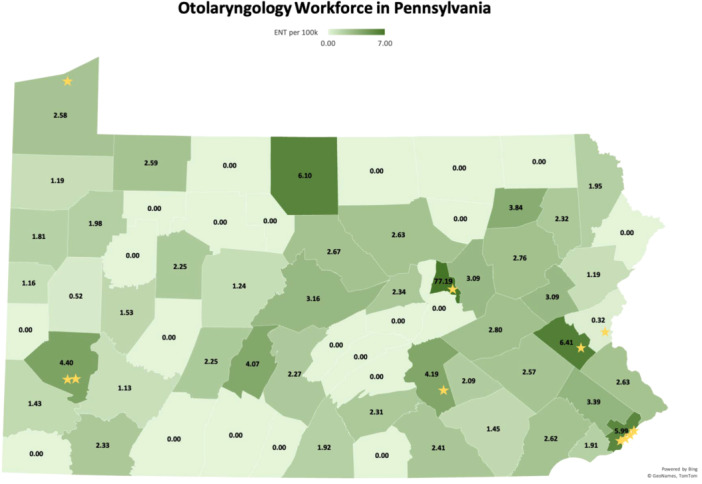
Analysis of the otolaryngology workforce as represented by the number of otolaryngologists per 100,000 people. ENT, ear, nose, and throat. Each star represents the location of an academic residency training program.
Discussion
Otolaryngology–head and neck surgery is a relatively small subspecialty with physicians providing a wide range of expertise in conditions affecting activities of daily living and people of all ages. These conditions are increasingly common, largely due to the growing geriatric population. 3 While primary care physicians often treat uncomplicated medical conditions related to the ear, nose, and throat, specialist and expert surgical care is often needed for many patients. People living in rural areas may have limited access to subspecialty care compared to those living in urban areas. Understanding the current distribution of otolaryngologists is critical to workforce planning and resource allocation. Our study found that Pennsylvania's otolaryngology workforce is not evenly distributed across state counties. The density of otolaryngologists was inversely correlated with rurality, except in nonmetropolitan counties with large academic centers.
Most otolaryngologists were male, which is consistent with other surgical subspecialties. However, with the increasing number of female trainees graduating each year, the gender gap is slowly closing. 14 Most otolaryngologists practice in metropolitan areas, consistent with previous studies. 10 Among the metropolitan counties, Lehigh, Philadelphia, and Allegheny counties had the highest number of otolaryngologists/100 k. Allegheny and Philadelphia are the most populated counties in Pennsylvania, home to multiple academic medical centers and residency training programs. While Lehigh County is categorized as a smaller metropolitan area, it also houses an academic medical center. Since tertiary care centers represent a concentration of resources, patients in more rural areas without readily available access to larger medical centers may need to be referred to these facilities for more complicated otolaryngology conditions, which can be costly and time‐consuming.
The lack of otolaryngologists in nonmetropolitan counties is a concern. When Montour County was excluded from the nonmetropolitan counties, there was an average of 1 otolaryngologist per 100 k patients. In 19 rural counties, there are 0 reported otolaryngologists. Similarly, an average of 7.49 otolaryngologists/100 square miles were seen in counties designated by code 1. This is in stark contrast even to the other 2 metro areas, which averaged 1.36 and 0.47 otolaryngologists/100 square miles in metropolitan counties (codes 2 and 3). When excluding Montour County, nonmetropolitan counties averaged fewer than 0.2 otolaryngologists/100 square miles. This was not surprising, as most physicians practice in places with high populations, incomes, and education. 15 Similar disparities in the otolaryngology landscape have been reported in Illinois and Nebraska. 16 , 17 There is a greater density of otolaryngologists in Pennsylvania's metro areas, with our study reporting an average of 2.4 otolaryngologists/100 k people compared to an average of 1.32 otolaryngologists/100 k people in urban areas of Illinois. 16 Both prior studies categorized counties based on the 2013 National Center of Health Sciences Urban‐Rural Classification Scheme for Counties. In contrast, our study utilized the 2023 Rural‐Urban Continuum Codes, which has a more up‐to‐date population census. 18 In addition to population size, this classification for nonmetropolitan areas takes into account their degree of urbanization and proximity to metro areas.
Studies have reported head and neck cancer survival differences by race and socioeconomic status, with some reporting differences by rural‐urban status. 8 , 19 Another study suggested that rural head and neck cancer survivors may be more likely to report a decreased quality of life. 20 Interestingly, some suggest that living at shorter distances to one's cancer treatment facility is associated with lower overall survival. 21 , 22 Timely access to care is critical, particularly, with the rapidly growing aging population. 3 Older patients are susceptible to conditions such as age‐related hearing loss or loss of balance, and those living in rural areas may be at a higher risk for delayed hearing aid acquisition compared to those in urban areas. 23
There is a significant need to improve access to adequate otolaryngology care. A national study showed that 61.8% of otolaryngologists practiced in metropolitan areas, areas that represent 55.3% of the population. 10 Rural areas are often underrepresented, particularly, in isolated areas removed from large medical centers. This geospatial analysis of the otolaryngology landscape in Pennsylvania can help inform policymakers to develop strategies for delivering care to underserved rural counties. While more resident trainees are graduating each year, otolaryngology residency remains competitive, with only about 370 surgeons graduating each year. 24 Other health care team members, such as advanced practice providers, help meet growing demands for care, but physician oversight is still required. Telemedicine is another avenue to improve access to otolaryngology care and has demonstrated some success during the COVID‐19 pandemic. 25 However, in some instances, telemedicine cannot replace the value of in‐person physical exams and assessments. While increasing the number of graduating otolaryngologists or providing incentives for rural practice may help mitigate this, more solutions are needed to help close the gaps in rural health care.
Our study was not without limitations. Subspecialty otolaryngology coverage by county was not known. While many physicians complete a fellowship, it is not necessary for an otolaryngologist to perform specialized surgeries. The full scope of one's otolaryngology practice is not always clearly listed and defined online. Our study also did not include advanced practice providers, speech‐language pathologists, audiologists, and other critical members of the health care team that help improve access to care. The surgeon's associated county was recorded based on what was listed as their primary location on the AAO‐HNS website. However, it is also not uncommon for otolaryngologists to work at multiple sites nearby. While 2 databases were used to collect names of otolaryngologists, there are likely non‐Medicare surgeons or those not registered with the AAO‐HNS that are not listed.
Conclusions
There is a shortage of otolaryngologists in rural Pennsylvania counties, with the exception of counties home to large academic centers. The current infrastructure of the otolaryngology workforce in Pennsylvania is aggregated in larger metropolitan areas. Understanding the current distribution of the otolaryngology workforce may aid policymakers in developing strategies to mitigate the gap in specialty care in rural communities.
Author Contributions
Bao Y. Sciscent, concept design, acquisition, analysis, and interpretation of data, writing the manuscript, presentation; Kimberly Chan, concept design, acquisition, analysis, and interpretation of data, critical editing of the manuscript; Hänel W. Eberly, interpretation of data, critical editing of the manuscript; David Goldenberg, interpretation of data, critical editing of the manuscript; Neerav Goyal, supervision, concept design, interpretation of data, critical editing of the manuscript, final approval.
Disclosures
Competing interests
None.
Funding source
No funding was received for this article.
Acknowledgments
The authors thank Caia Hypatia for their assistance with manuscript preparation and submission.
References
- 1. Sorichetti B, Pauwels J, Jacobs T, Chadha N, Kozak E, Kozak F. High frequency of otolaryngology/ENT encounters in Canadian primary care despite low medical undergraduate. Can Med Educ J. 2019;13(1):86‐89. 10.36834/cmej.72328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahboubi H, Lin HW, Bhattacharyya N. Prevalence, characteristics, and treatment patterns of hearing difficulty in the United States. JAMA Otolaryngol Head Neck Surg. 2017;144(1):65‐70. 10.1001/jamaoto.2017.2223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chiu BL, Pinto JM. Aging in the United States. Otolaryngol Clin North Am. 2018;51(4):697‐704. 10.1016/j.otc.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barreto T, Jetty A, Eden AR, Petterson S, Bazemore A, Peterson LE. Distribution of physician specialties by rurality. J Rural Health. 2021;37(4):714‐722. 10.1111/jrh.12548 [DOI] [PubMed] [Google Scholar]
- 5. Urban MJ, Shimomura A, Shah S, Losenegger T, Westrick J, Jagasia AA. Rural otolaryngology care disparities: a scoping review. Otolaryngol Head Neck Surg. 2022;166(6):1219‐1227. 10.1177/01945998211068822 [DOI] [PubMed] [Google Scholar]
- 6. Parker MA, Weinberger AH, Eggers EM, Parker ES, Villanti AC. Trends in rural and urban cigarette smoking quit ratios in the US from 2010 to 2020. JAMA Netw Open. 2022;5(8):e2225326. 10.1001/jamanetworkopen.2022.25326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mohammed KA, Subramaniam DS, Geneus CJ, et al. Rural‐urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39‐43. 10.1016/j.ypmed.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 8. Clarke JA, Despotis AM, Ramirez RJ, Zevallos JP, Mazul AL. Head and neck cancer survival disparities by race and rural–urban context. Cancer Epidemiol Biomarkers Prevent. 2020;29(10):1955‐1961. 10.1158/1055-9965.epi-20-0376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lawrence LA, Heuermann ML, Javadi P, Sharma A. Socioeconomic status and rurality among patients with head and neck cancer. Otolaryngol Head Neck Surg. 2022;166(6):1028‐1037. 10.1177/01945998211019278 [DOI] [PubMed] [Google Scholar]
- 10. Vickery TW, Weterings R, Cabrera‐Muffly C. Geographic distribution of otolaryngologists in the United States. Ear Nose Throat J. 2016;95(6):218‐223. [PubMed] [Google Scholar]
- 11. United States Census Bureau . Nation's urban and rural populations shift following 2020 census. 2022. Accessed May 31, 2024. https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html
- 12. United States Census Bureau . Census population clock. Accessed May 31, 2024. https://www.census.gov/popclock/embed.php?component=populous
- 13. Centers for Medicare & Medicaid Services . Medicare physician & other practitioners—by Provider. 2022. Accessed May 13, 2024. https://data.cms.gov/provider-summary-by-type-of-service/medicare-physician-other-practitioners/medicare-physician-other-practitioners-by-provider/data
- 14. Quereshy HA, Quinton BA, Mowry SE. Otolaryngology workforce trends by gender—when and where is the gap narrowing. Am J Otolaryngol. 2022;43(3):103427. 10.1016/j.amjoto.2022.103427 [DOI] [PubMed] [Google Scholar]
- 15. Gadkaree SK, McCarty JC, Siu J, et al. Variation in the geographic distribution of the otolaryngology workforce: a national geospatial analysis. Otolaryngol Head Neck Surg. 2020;162(5):649‐657. 10.1177/0194599820908860 [DOI] [PubMed] [Google Scholar]
- 16. Urban MJ, Wojcik C, Eggerstedt M, Jagasia AJ. Rural‐urban disparities in otolaryngology: the state of Illinois. Laryngoscope. 2021;131(1):E70‐E75. 10.1002/lary.28652 [DOI] [PubMed] [Google Scholar]
- 17. LaCrete F, Ratnapradipa KL, Carlson K, Lyden E, Dowdall JR. Rural‐urban otolaryngologic observational workforce analysis: the state of Nebraska. Laryngoscope Investig Otolaryngol. 2023;8(6):1602‐1606. 10.1002/lio2.1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. USDA Economic Research Service. U.S. Department of Agriculture . Rural‐urban continuum codes. 2024. Accessed April 3, 2024. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- 19. Pagedar NA, Davis AB, Sperry SM, Charlton ME, Lynch CF. Population analysis of socioeconomic status and otolaryngologist distribution on head and neck cancer outcomes. Head Neck. 2019;41(4):1046‐1052. 10.1002/hed.25521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adamowicz JL, Christensen A, Howren MB, et al. Health‐related quality of life in head and neck cancer survivors: evaluating the rural disadvantage. J Rural Health. 2022;38(1):54‐62. 10.1111/jrh.12571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bird CE, Traylor JI, Youssef M, Abdullah KG. Distance traveled to glioblastoma treatment: a measure of the impact of socioeconomic status on survival. Clin Neurol Neurosurg. 2021;209:106909. 10.1016/j.clineuro.2021.106909 [DOI] [PubMed] [Google Scholar]
- 22. Massa ST, Liebendorfer AP, Zevallos JP, Mazul AL. Distance traveled to head and neck cancer provider: a measure of socioeconomic status and access. Otolaryngol Head Neck Surg. 2020;162(2):193‐203. 10.1177/0194599819892015 [DOI] [PubMed] [Google Scholar]
- 23. Chan S, Hixon B, Adkins M, Shinn JB, Bush ML. Rurality and determinants of hearing healthcare in adult hearing aid recipients. Laryngoscope. 2017;127(10):2362‐2367. 10.1002/lary.26490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. NRMP . Main residency match data and reports. 2023. Accessed May 31, 2024. https://www.nrmp.org/match-data-analytics/residency-data-reports/
- 25. Lorenz FJ, Heikel T, Tucker J, Lin A, Gniady JP, Goldenberg D. Telemedicine in otolaryngology in the context of the end of the COVID‐19 public health emergency. Otolaryngol Head Neck Surg. 2024;170(2):624‐626. 10.1002/ohn.550 [DOI] [PubMed] [Google Scholar]


