Abstract
The chimeric recombinant virus rHPIV3-NB, a version of human parainfluenza virus type 3 (HPIV3) that is attenuated due to the presence of the bovine PIV3 nucleocapsid (N) protein open reading frame (ORF) in place of the HPIV3 ORF, was modified to encode the measles virus hemagglutinin (HA) inserted as an additional, supernumerary gene between the HPIV3 P and M genes. This recombinant, designated rHPIV3-NBHA, replicated like its attenuated rHPIV3-NB parent virus in vitro and in the upper and lower respiratory tracts of rhesus monkeys, indicating that the insertion of the measles virus HA did not further attenuate rHPIV3-NB in vitro or in vivo. Monkeys immunized with rHPIV3-NBHA developed a vigorous immune response to both measles virus and HPIV3, with serum antibody titers to both measles virus (neutralizing antibody) and HPIV3 (hemagglutination inhibiting antibody) of over 1:500. An attenuated HPIV3 expressing a major protective antigen of measles virus provides a method for immunization against measles by the intranasal route, a route that has been shown with HPIV3 and respiratory syncytial virus vaccines to be relatively refractory to the neutralizing and immunosuppressive effects of maternally derived virus-specific serum antibodies. It should now be possible to induce a protective immune response against measles virus in 6-month-old infants, an age group that in developing areas of the world is not responsive to the current measles virus vaccine.
Measles virus is a member of the genus Morbillivirus of the Paramyxoviridae family of viruses (20). Measles virus infection causes the death of over 1 million children per year and remains among the most important causes of mortality due to infectious disease worldwide (27). A measles virus vaccine is available, but it is largely ineffective in infants under 9 to 15 months of age because maternally acquired measles virus-specific antibodies readily neutralize this parenterally administered attenuated vaccine virus (1). Since measles virus causes serious illness in infants 6 to 15 months of age (45), there is a need for a measles virus vaccine that can induce a protective immune response in infants possessing maternally acquired measles virus antibodies. Human parainfluenza virus type 3 (HPIV3) is another important human pathogen and is second only to respiratory syncytial virus as a cause of serious pediatric viral respiratory tract disease worldwide (7).
Several approaches to the development of vaccines to protect the very young infant against PIV3 or measles virus infection have been pursued (9, 14, 32, 42, 43, 54, 55). Virus vectors carrying a major antigenic determinant of HPIV3 (12, 53) or measles virus (11, 15, 36, 38, 44, 49, 50) have shown promise but are not always effective in the presence of serum antibodies to PIV3 (12) or measles virus (54), which are present in young infants as maternally derived serum immunoglobulin G. A live attenuated vaccine that is delivered directly into the respiratory tract, where it replicates and induces both a systemic and a mucosal antibody response, can effectively circumvent the neutralizing activity of serum antibody (12, 52).
Some of the most promising paramyxovirus vaccine candidates are live attenuated viruses, since these have been shown to be highly efficacious in nonhuman primates even in the presence of high levels of passively transferred antibodies, an experimental situation that simulates that of the very young infant with maternally acquired antibodies (8, 12). For HPIV3, two candidate vaccines have been shown in clinical trials to be well tolerated, safe, and immunogenic in infants and children, namely (i) the cold-passaged (cp) HPIV3 cp45 virus, which contains a number of attenuating point mutations, and (ii) the Kansas (Ka) strain of bovine PIV3 (BPIV3), which is attenuated by a host range restriction (see below) (22, 26). Because of these successful clinical experiences, we have been exploring the use of attenuated PIV3 as a vector to express antigens of additional pathogens for the purpose of designing bivalent or multivalent pediatric vaccines. We previously constructed a version of HPIV3, termed rcp45L (HA P-M) (14), that expressed measles virus hemagglutinin (HA) from an added gene and contained three cp45-derived attenuating point mutations in the L gene (39). rcp45L (HA P-M) was attenuated and immunogenic for both HPIV3 and measles virus in hamsters.
The strategy of using an animal virus that is attenuated in humans because of a host range restriction as a vaccine against a virulent antigenically related human virus represents the “Jennerian” approach to vaccine development (31). BPIV3 was found to be 100- to 1,000-fold restricted in replication in rhesus monkeys compared to wild-type (wt) HPIV3 (6). However, BPIV3 is only 25% antigenically related to HPIV3 in cross-neutralization assays (6) and is therefore not optimally immunogenic for HPIV3. We previously constructed a viable chimeric recombinant bovine-human PIV3 containing the nucleoprotein (N) open reading frame (ORF) from BPIV3 Ka in place of the HPIV3 N ORF, previously designated cKa-N (3) and referred to here as rHPIV3-NB. This virus was restricted in replication in rhesus monkeys to the same extent as its BPIV3 parent virus (3). Furthermore, this identified the BPIV3 N protein as a major determinant for the host range restriction of replication of BPIV3 in primates. rHPIV3-NB induced a high level of resistance in rhesus monkeys to challenge with the biologically derived wt JS strain of HPIV3. The rHPIV3-NB chimeric virus thus combines the antigenic determinants of wt HPIV3 with the host range restriction and attenuation phenotype of BPIV3. There are 79 differences out of a total of 515 amino acids between the N proteins of HPIV3 and BPIV3 (4). Many of these 79 amino acid differences likely contribute to the host range attenuation phenotype of rHPIV3-NB. Because the host range restriction of BPIV3 is expected to be based on numerous amino acid differences, it is anticipated that the attenuation phenotype of rHPIV3-NB will be stable even following prolonged replication in vivo. In the present study, we evaluated rHPIV3-NB as a vector for the expression of measles virus HA for the purpose of developing a bivalent vaccine for intranasal (IN) immunization of infants and young children.
Construction, recovery, and in vitro growth characteristics of rHPIV3-NBHA.
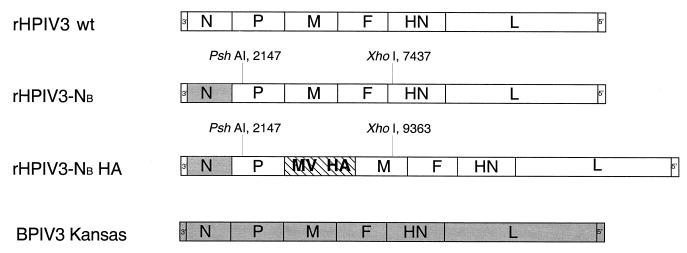
The antigenomic cDNA encoding rHPIV3-NB (3) was modified to contain the measles virus HA ORF inserted as an additional gene between the P and M genes (Fig. 1). The source of the HA gene was a previously constructed wt HPIV3 antigenomic cDNA, pFLC(HA P-M) (14), containing the HA ORF under the control of HPIV3 gene start and gene end transcription signals and inserted as a supernumerary gene into the wt rHPIV3 genome between the P and M genes. We replaced the PshAI-to-XhoI fragment of the rHPIV3-NB antigenomic cDNA with that of pFLC(HA P-M) bearing the HA gene. Recombinant virus, designated rHPIV3-NBHA, was readily recovered from HEp-2 cells transfected with the chimeric antigenomic cDNA and support plasmids and was biologically cloned and propagated on LLC-MK2 cells as described previously (42). Viral RNA was isolated from the recovered virus, and the added HA gene and flanking sequences were amplified by reverse transcription-PCR and were analyzed by restriction enzyme digestion and nucleotide sequencing. This confirmed that the genome structure of the recovered rHPIV3-NBHA virus was exactly as designed (data not shown).
FIG. 1.
Schematic diagram (not to scale) of the parent and chimeric PIV3s. The relative positions of the BPIV3 N ORF (░⃞; shaded regions consist of BPIV3 sequence) and measles virus HA ORF (▧) are indicated in biologically derived and recombinant PIV3s. The restriction sites used to transfer the HA gene into rHPIV3-NBHA are shown.
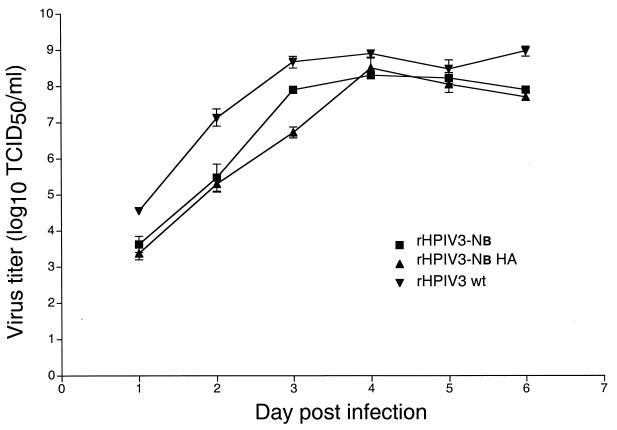
The kinetics of replication in vitro of rHPIV3-NBHA was compared to that of its rHPIV3-NB parent and wt rHPIV3 by infecting LLC-MK2 cells at a multiplicity of infection of 0.01 and measuring the virus yield at 24-h intervals, as described previously (42). rHPIV3-NBHA displayed a rate of growth similar to that of rHPIV3-NB and also grew to a peak titer on day 4 similar to that of each of its parent viruses (Fig. 2). This demonstrated that the insertion of an additional gene into the chimeric PIV3 genome did not attenuate this virus for replication in vitro.
FIG. 2.
Multistep growth curves of rHPIV3s. LLC-MK2 monolayers were infected in triplicate with the indicated rPIV3 at a multiplicity of infection of 0.01 at 32°C. Aliquots of the medium supernatants were harvested at 24-h intervals and were assayed at 32°C for virus titer. Virus titers are expressed as mean log10 TCID50 per milliliter ± SE.
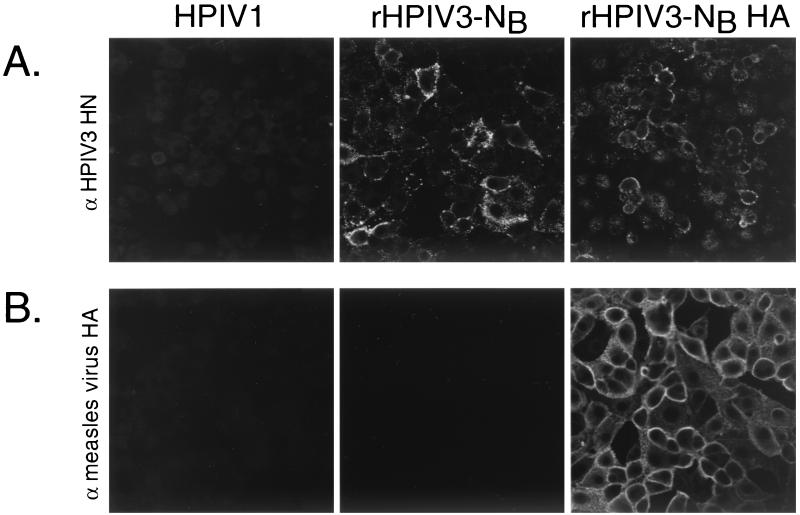
The expression of the measles virus HA was initially examined by immunostaining plaques formed on LLC-MK2 monolayer cultures infected with rHPIV3-NBHA with mouse monoclonal antibodies specific to the measles virus HA or with monoclonal antibodies specific for the HPIV3 hemagglutinin-neuraminidase (HN) protein as described previously (14). The viral titers determined by immunostaining rHPIV3-NBHA plaques on monolayer cultures with a mixture of measles HA- or HPIV3 HN-specific antibodies were essentially indistinguishable, indicating that the HA antigen was expressed by the majority of plaque-forming virions (data not shown). Expression of the measles virus gene was also confirmed by indirect immunofluorescence of LLC-MK2 cells infected with rHPIV3-NBHA (Fig. 3). LLC-MK2 cells grown on glass slides were infected with a recombinant HPIV3 or with wt HPIV1. Approximately 44 h postinfection, the cells were fixed and permeabilized as described previously (40). Mouse monoclonal anti-HPIV3 (101/1 and 454/11 [47]) (Fig. 3A) or anti-measles HA antibodies (79-XV-V17, 80-III-B2, and 81-1-366 [a gift of Stephen Jacobson, National Institutes of Health] [14]) (Fig. 3B) and fluorescein isothyocianate-conjugated anti-mouse immunoglobulin G antibodies (Jackson Immunochemicals, West Grove, Pa.) were used for detection of the HPIV3 HN or measles virus HA glycoprotein, respectively. The pattern of fluorescence in cells infected with rHPIV3-NBHA demonstrated that this recombinant expressed the major antigenic determinants of both HPIV3 and measles virus. Both viral glycoproteins localized to the cell membrane and to the cytoplasm. Efficient expression of the measles virus HA in vivo was confirmed as described below.
FIG. 3.
rHPIV3-NBHA expresses the major antigenic determinants of HPIV3 and measles virus. Mouse monoclonal anti-HPIV3 HN (101/1 and 454/11) (A) and mouse monoclonal anti-measles HA antibodies (79-XV-V17, 80-III-B2, and 81-1-366) (B) were used to detect the HN protein and HA in LLC-MK2 cells infected with the indicated virus.
rHPIV3-NBHA replicates to the same level as rHPIV3-NB in the respiratory tracts of rhesus monkeys.
Rhesus macaques are permissive for HPIV3 (13) and measles virus (34) replication and are, therefore, appropriate animal models for the study of PIV or measles virus infection and immunity. This nonhuman primate model has been used to screen PIV vaccine candidates before proceeding to clinical trials (23). We sought to determine if the presence of the measles virus HA significantly decreased the replication of rHPIV3-NB in the upper and lower respiratory tracts of immunized nonhuman primates, as had been previously observed in a rodent model when a supernumerary gene was inserted into an attenuated HPIV3 backbone (14, 41). We also sought to determine if rHPIV3-NBHA replicated sufficiently to induce a satisfactory immune response against both HPIV3 and measles virus in nonhuman primates, a more appropriate animal model than rodents for these human pathogens. The replication of rHPIV3-NBHA in the upper and lower respiratory tracts of rhesus monkeys was compared to that of its rHPIV3-NB parent as well as to that of wt rHPIV3 and wt BPIV3 (Table 1). Rhesus monkeys that were seronegative for both HPIV3 and measles virus were inoculated simultaneously by the IN and intratracheal (IT) routes with 1 ml of L15 medium per site containing 105 50% tissue culture infective doses (TCID50) of virus, as described previously (3, 37). Nasopharyngeal (NP) swab samples were collected on days 1 through 10 postinfection, and tracheal lavage (TL) samples were collected on days 2, 4, 6, 8, and 10 postinfection. Virus present in the NP and TL specimens was quantified by titration on LLC-MK2 cell monolayers at 32°C, as previously described (42), and the mean peak virus titer obtained was expressed as log10 TCID50 per milliliter (Table 1). Table 1 also includes data collected from similarly infected and sampled rhesus monkeys from two previous studies (3, 37).
TABLE 1.
rHPIV3-NBHA, a chimeric human-bovine PIV3 expressing the measles virus HA gene, is satisfactorily attenuated for replication in the upper and lower respiratory tracts of rhesus monkeys, induces antibodies to both HPIV3 and measles virus, and protects against HPIV3 wt virus challenge
| Group no. | Immunizing virusa | No. of animalsb | Response to
immunization
|
Response to challenge with HPIV3 wt on day
28 or 31d
|
Serum antibody response to administration of measles virus vaccine (Moraten) on day 59f (mean antibody titer to measles virus)f | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Virus
replication
|
Serum antibody response
|
Virus
replication
|
Serum antibody response
|
|||||||
| Mean
peak virus titerc
(log10TCID50/ml ± SE)
|
HAI antibody titer for HPIV3 on days 28 and 31de | Mean antibody titer to measles virusf | Mean peak HPIV3 virus
titerg
|
HAI antibody titer for HPIV3 on days 56 and 59e | ||||||
| NP swab | TL | NP swab | TL | |||||||
| 1 | rHPIV3 wt | 8 (2) | 4.7 ± 0.4 | 3.3 ± 0.4 | 8.4 ± 0.5 | <1.1 ± 0.0 (<6) | 1.4 ± 0.3 | 1.1 ± 0.2 | 11.5 ± 0.2 | 11.2 ± 1.7 (6,646) |
| 2 | rHPIV3-NB | 8 (2) | 2.6 ± 0.6 | 2.0 ± 0.4 | 7.5 ± 0.4 | <1.1 ± 0.0 (<6) | 2.1 ± 0.4 | 1.2 ± 0.2 | 11.1 ± 0.3 | 9.0 ± 0.2 (1,446) |
| 3 | rHPIV3-NB HA | 4 (4) | 2.2 ± 0.6 | 2.8 ± 0.6 | 7.0 ± 0.0 | 9.2 ± 0.3 (1,661) | 1.2 ± 0.7 | 2.3 ± 0.2 | 11.5 ± 0.3 | 9.7 ± 0.2 (2,347) |
| 4 | BPIV3 Ka | 8 (2) | 2.4 ± 0.3 | 1.9 ± 0.2 | 4.4 ± 0.5 | ND | 2.9 ± 0.2 | 2.0 ± 0.5 | 9.8 ± 0.6 | ND |
| 5 | Controlh | 10 (2) | ≤0.5 ± 0.0 | ≤0.5 ± 0.0 | <2.0 ± 0.0 | ND | 4.8 ± 0.2 | 4.3 ± 0.2 | 11.1 ± 0.4 | ND |
Monkeys were inoculated IN and IT with 105 TCID50 of virus in a 1-ml inoculum at each site.
With the exception of the group that received rHPIV3-NBHA (group 3), the data presented include historical data from studies reported previously (1, 33). The number of animals used in the current study is presented in parentheses. Groups 1, 2, 4, and 5 contain two new animals each from the present study.
NP swab samples were collected on days 1 to 10 postinfection. TL samples were collected on days 2, 4, 6, 8, and 10 postinfection. The mean of the peak virus titers for each animal in its group is given, irrespective of sampling day. Virus titrations were performed on LLC-MK2 cells at 32°C. The limit of detection of virus titer was 10 TCID50/ml.
In the present study, sera were collected from monkeys on day 31 postimmunization, and the animals were then challenged with HPIV3. In the two previous studies, monkeys were sampled and challenged on day 28 postimmunization. The antibody titers reported were performed in the same assay.
Serum HAI titer is expressed as the mean reciprocal log2 ± SE.
Neutralization values are those obtained for the eight new animals in the present study (groups 1, 2, and 3 [see the text]). Sixty percent plaque reduction neutralizing (PRN); mean reciprocal log2 ± SE on day 31 postimmunization or day 87 post-first immunization. The PRN assay was standardized with the second international standard antimeasles serum (National Institute for Biological Standards and Control, Potters Bar, Hertfordshire, United Kingdom; lot no. 66/202). Mean values in milli-international units are shown in parentheses. The eight animals from the present study (groups 1, 2, and 3) were immunized on day 59 with 105 PFU of the measles virus Moraten vaccine strain administered parenterally (intramuscularly). Serum was collected 28 days later (i.e., 87 days after the first immunization). ND, not done.
28 or 31 days after immunization, monkeys were inoculated IN and IT with 106 TCID50 of the biologically derived HPIV3 wt JS strain in a 1-ml inoculum at each site. NP and TL samples were collected on days 0, 2, 4, 6, and 8 postchallenge. The virus titers obtained for NP and TL samples on day 0 were ≤0.5 log10 TCID50/ml. Titers are expressed as log10 TCID50 per milliliter ± SE.
The control group consisted of animals which were not immunized or had received 105 PFU of respiratory syncytial virus (two new animals in the present study).
The rHPIV3-NBHA chimeric virus replicated in the upper and lower respiratory tracts of rhesus monkeys to a level comparable to that of its rHPIV3-NB parent virus. rHPIV3-NBHA was significantly restricted in replication in the upper respiratory tract compared to rHPIV3 wt (P < 0.05; Student's t test), but the level of replication of rHPIV3 wt in the lower respiratory tract is low, precluding meaningful statistical comparison. The level of replication of rHPIV3-NBHA was also comparable to that of the BPIV3 candidate vaccine, demonstrating that rHPIV3-NB HA retains the host range attenuation phenotype of rHPIV3-NB and BPIV3. This also indicated that, unexpectedly, the insertion of the measles virus HA gene into the rHPIV3-NB genome did not significantly further attenuate this virus for replication in the respiratory tracts of rhesus monkeys. This suggests that the attenuation conferred by inserting the HA ORF between the PIV3 P and M genes previously observed in hamsters (14) may be specific to that animal model or is largely masked in primates by the attenuation phenotype specified by the bovine N gene product.
Immunization of rhesus monkeys with rHPIV3-NBHA induced high titers of antibodies against both HPIV3 and measles virus and protected the monkeys from challenge with biologically derived HPIV3.
Although cell-mediated immunity likely plays a role in protection against PIV and measles virus disease, the sparing of severe measles virus infection in early infancy defines a major role for antibodies in resistance to disease caused by measles virus. Previously, it was found that hamsters immunized with a recombinant HPIV3 expressing the measles virus HA developed high serum neutralizing antibody titers to measles virus (14). However, it was not known if a strong immune response to a vectored antigen could be induced in primates, a more appropriate model for a human viral pathogen. As shown in Table 1, rhesus monkeys immunized with rHPIV3-NBHA developed a high level of serum antibodies against both HPIV3 and measles virus. Serum HPIV3 antibodies were quantified by hemagglutination inhibition (HAI) assay using guinea pig erythrocytes as described previously (48), and the titers are expressed as mean reciprocal log2 ± standard error (SE). A high level of serum HAI antibodies to HPIV3 was induced by both rHPIV3-NBHA (1:128) and rHPIV3-NB (1:181), demonstrating that these attenuated recombinants can induce a strong immune response against the backbone antigens of the HPIV3 vector. The serum neutralizing antibody titer against measles virus was quantified by plaque assay as described previously (14), and the titer is expressed as reciprocal mean log2 ± SE (Table 1). Rhesus monkeys immunized with rHPIV3-NBHA developed a high level of measles virus neutralizing antibodies of 1:588 (1,661 mIU) measured 31 days after immunization, a level that is in substantial excess of that needed to protect humans against infection with measles virus (5, 28).
To compare the efficacy of immunization with the live attenuated rHPIV3-NBHA and rHPIV3-NB virus vaccine candidates against wt HPIV3 infection, the monkeys were challenged IN and IT with 106 TCID50 of the biologically derived JS strain of wt HPIV3 31 days after immunization (Table 1). NP swab and TL samples were collected on days 2, 4, 6, and 8 postchallenge. Virus present in the specimens was quantified by serial dilution on LLC-MK2 monolayer cultures as described above. rHPIV3-NBHA and rHPIV3-NB induced comparable high levels of protection against challenge with wt HPIV3, as indicated by a 100- to 1,000-fold reduction in wt HPIV3 replication in the respiratory tract of immunized monkeys. This demonstrated that insertion of the measles virus HA gene into the chimeric bovine-human PIV3 did not diminish the level of protection induced by the HPIV3 glycoproteins present in the backbone of the attenuated vector.
We next sought to compare the immunogenicity of rHPIV3-NBHA with that of the live attenuated Moraten strain measles virus vaccine in rhesus monkeys. Rhesus monkeys previously infected with rHPIV3 (n = 2), rHPIV3-NB (n = 2), or rHPIV3-NBHA (n = 4) were immunized parenterally (intramuscularly) with 105 PFU of the Moraten virus on day 59, and serum samples were collected on day 87 and analyzed for neutralizing antibodies against measles virus (Table 1). In measles virus-naive animals (Table 1, groups 1 and 2), the titer of measles virus-specific antibodies induced by the Moraten vaccine virus was similar to that observed in rHPIV3-NBHA-immunized animals (Table 1, group 3). Thus, the immunogenicity of the rHPIV3-NBHA vector expressing the HA glycoprotein of measles virus was equivalent to that of the Moraten measles vaccine virus. This demonstrates that an attenuated PIV3 can be used as a vector to construct a multivalent vaccine to immunize primates against multiple human viral pathogens.
An important advantage of a PIV vector-based vaccine for measles virus over the licensed Moraten vaccine is that the PIV vector can be administered by the IN route, whereas live-attenuated measles virus vaccines are not consistently infectious by this route, probably as a consequence of their attenuation and adaptation to cell culture (10). This makes it possible to immunize with rHPIV3-NBHA in early infancy, an age group that cannot be immunized with a current live attenuated measles virus vaccine such as the Moraten strain because the vaccine virus is neutralized by passively acquired maternal antibodies (14). Replication of respiratory viruses in the upper respiratory tract is relatively refractory to an inhibitory effect of passively transferred serum antibodies (35). Therefore, it was not surprising to find that the HPIV3 and respiratory syncytial virus live attenuated vaccine candidates are infectious and immunogenic in experimental animals which have been administered physiologic amounts of virus-neutralizing antibodies as well as in infants and young children possessing maternally derived virus-specific serum antibodies (8, 12, 24, 25, 52). It is reasonable to expect that the same will be true of heterologous antigens borne by recombinant HPIV3. This will be investigated directly in future studies by examining the safety and protective efficacy of rHPIV3-NBHA in rhesus monkeys that have received passive infusion of physiologic amounts of antibodies specific to HPIV3, measles virus, or both. In addition, the local antibody response and the longevity of the serum immune response to the vectored measles antigen will be examined in future studies to determine if prior immunization with a PIV-measles recombinant interferes with subsequent immunization with the Moraten vaccine strain.
The lack of effective vaccination against measles virus infection results in the death of over 2,700 children every day worldwide (51). The rHPIV3-NBHA candidate vaccine offers a unique opportunity to immunize against two major causes of severe pediatric disease, namely, HPIV3 and measles virus. Unlike the currently licensed measles virus vaccines, we expect that chimeric rHPIV3-NBHA, expressing the major antigenic determinant of measles virus, can be used to induce a strong immune response to measles virus in infants about 6 months of age (14). Additional chimeric recombinant PIVs expressing the measles virus F glycoprotein with or without HA will also be generated, and their immunogenicity and efficacy will be examined in animal models. The need for a measles virus vaccine to protect children less than 15 months of age is greatest in the regions of the world where there also is a high prevalence of infection with human immunodeficiency virus (30, 33). The candidate measles vaccine described here should be phenotypically stable in vivo following prolonged replication in an immunocompromised host because the attenuation phenotype is likely specified by many of the 79 amino acid differences that differentiate the bovine and human N proteins, but this assumption requires experimental verification. We are further examining the basis of attenuation of the bovine N gene in rHPIV3-NB and its phenotypic stability following prolonged replication in a permissive host. An effective immunization strategy for infants and children will be required to meet the World Health Organization goal to eradicate measles by the year 2010. In particular, it would be advantageous in the final stage of measles eradication to employ a vaccine that does not involve infectious measles virus, thereby precluding possible persistence of the pathogen, as may occur in immunocompromised individuals, and reversion to the wt phenotype seen with other live attenuated virus vaccines (2, 16–19, 21, 29, 46).
Acknowledgments
We thank Robert Chanock, Jason Newman, and Lea Vogel for reviewing the manuscript. We also thank Judy Beeler for the standardized measles serum and Ernest Williams and Fatemeh Davoodi for technical assistance.
REFERENCES
- 1.Albrecht P, Ennis F A, Saltzman E J, Krugman S. Persistence of maternal antibody in infants beyond 12 months: mechanism of measles vaccine failure. J Pediatr. 1977;91:715–718. doi: 10.1016/s0022-3476(77)81021-4. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. Outbreak of poliomyelitis—Dominican Republic and Haiti, 2000. Morb Mortal Wkly Rep. 2000;49:1094–1103. [PubMed] [Google Scholar]
- 3.Bailly J E, McAuliffe J M, Durbin A P, Elkins W R, Collins P L, Murphy B R. A recombinant human parainfluenza virus type 3 (PIV3) in which the nucleocapsid N protein has been replaced by that of bovine PIV3 is attenuated in primates. J Virol. 2000;74:3188–3195. doi: 10.1128/jvi.74.7.3188-3195.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailly J E, McAuliffe J M, Skiadopoulos M H, Collins P L, Murphy B R. Sequence determination and molecular analysis of two strains of bovine parainfluenza virus type 3 that are attenuated for primates. Virus Genes. 2000;20:173–182. doi: 10.1023/a:1008130917204. [DOI] [PubMed] [Google Scholar]
- 5.Chen R T, Markowitz L E, Albrecht P, Stewart J A, Mofenson L M, Preblud S R, Orenstein W A. Measles antibody: reevaluation of protective titers. J Infect Dis. 1990;162:1036–1042. doi: 10.1093/infdis/162.5.1036. [DOI] [PubMed] [Google Scholar]
- 6.Coelingh K, Winter C C, Tierney E L, London W T, Murphy B R. Attenuation of bovine parainfluenza virus type 3 in nonhuman primates and its ability to confer immunity to human parainfluenza virus type 3 challenge. J Infect Dis. 1988;157:655–662. doi: 10.1093/infdis/157.4.655. [DOI] [PubMed] [Google Scholar]
- 7.Collins P L, Chanock R M, McIntosh K. Parainfluenza viruses. In: Fields B N, Knipe D M, Howley P M, Chanock R M, Melnick J L, Monath T P, Roizman B, Straus S E, editors. Fields virology. 3rd ed. Vol. 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1205–1243. [Google Scholar]
- 8.Crowe J E, Jr, Bui P T, Siber G R, Elkins W R, Chanock R M, Murphy B R. Cold-passaged, temperature-sensitive mutants of human respiratory syncytial virus (RSV) are highly attenuated, immunogenic, and protective in seronegative chimpanzees, even when RSV antibodies are infused shortly before immunization. Vaccine. 1995;13:847–855. doi: 10.1016/0264-410x(94)00074-w. [DOI] [PubMed] [Google Scholar]
- 9.Crowe J E, Jr, Collins P L, Chanock R M, Murphy B R. Vaccines against respiratory syncytial virus and parainfluenza virus type 3. In: Levine M M, Woodrow G C, Kaper J B, Cobon G S, editors. New generation vaccines. 2nd ed. New York, N.Y: Marcel Dekker, Inc; 1997. pp. 711–725. [Google Scholar]
- 10.Cutts F T, Clements C J, Bennett J V. Alternative routes of measles immunization: a review. Biologicals. 1997;25:323–338. doi: 10.1006/biol.1997.0103. [DOI] [PubMed] [Google Scholar]
- 11.Drillien R, Spehner D, Kirn A, Giraudon P, Buckland R, Wild F, Lecocq J P. Protection of mice from fatal measles encephalitis by vaccination with vaccinia virus recombinants encoding either the hemagglutinin or the fusion protein. Proc Natl Acad Sci USA. 1988;85:1252–1256. doi: 10.1073/pnas.85.4.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Durbin A P, Cho C J, Elkins W R, Wyatt L S, Moss B, Murphy B R. Comparison of the immunogenicity and efficacy of a replication-defective vaccinia virus expressing antigens of human parainfluenza virus type 3 (HPIV3) with those of a live attenuated HPIV3 vaccine candidate in rhesus monkeys passively immunized with PIV3 antibodies. J Infect Dis. 1999;179:1345–1351. doi: 10.1086/314769. [DOI] [PubMed] [Google Scholar]
- 13.Durbin A P, Elkins W R, Murphy B R. African green monkeys provide a useful nonhuman primate model for the study of human parainfluenza virus types-1, -2, and -3 infection. Vaccine. 2000;18:2462–2469. doi: 10.1016/s0264-410x(99)00575-7. [DOI] [PubMed] [Google Scholar]
- 14.Durbin A P, Skiadopoulos M H, McAuliffe J M, Riggs J M, Surman S R, Collins P L, Murphy B R. Human parainfluenza virus type 3 (PIV3) expressing the hemagglutinin protein of measles virus provides a potential method for immunization against measles virus and PIV3 in early infancy. J Virol. 2000;74:6821–6831. doi: 10.1128/jvi.74.15.6821-6831.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fooks A R, Schadeck E, Liebert U G, Dowsett A B, Rima B K, Steward M, Stephenson J R, Wilkinson G W. High-level expression of the measles virus nucleocapsid protein by using a replication-deficient adenovirus vector: induction of an MHC-1-restricted CTL response and protection in a murine model. Virology. 1995;210:456–465. doi: 10.1006/viro.1995.1362. [DOI] [PubMed] [Google Scholar]
- 16.Friedrich F. Molecular evolution of oral poliovirus vaccine strains during multiplication in humans and possible implications for global eradication of poliovirus. Acta Virol. 2000;44:109–117. [PubMed] [Google Scholar]
- 17.Furione M, Guillot S, Otelea D, Balanant J, Candrea A, Crainic R. Polioviruses with natural recombinant genomes isolated from vaccine-associated paralytic poliomyelitis. Virology. 1993;196:199–208. doi: 10.1006/viro.1993.1468. [DOI] [PubMed] [Google Scholar]
- 18.Georgescu M M, Balanant J, Macadam A, Otelea D, Combiescu M, Combiescu A A, Crainic R, Delpeyroux F. Evolution of the Sabin type 1 poliovirus in humans: characterization of strains isolated from patients with vaccine-associated paralytic poliomyelitis. J Virol. 1997;71:7758–7768. doi: 10.1128/jvi.71.10.7758-7768.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greensfelder L. Infectious diseases. Polio outbreak raises questions about vaccine. Science. 2000;290:1867–1869. [PubMed] [Google Scholar]
- 20.Griffin D E, Bellini W J. Measles virus. In: Fields B N, Knipe D M, Howley P M, Chanock R M, Melnick J L, Monath T P, Roizman B, Straus S E, editors. Fields virology. Vol. 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1267–1312. [Google Scholar]
- 21.Guillot S, Caro V, Cuervo N, Korotkova E, Combiescu M, Persu A, Aubert-Combiescu A, Delpeyroux F, Crainic R. Natural genetic exchanges between vaccine and wild poliovirus strains in humans. J Virol. 2000;74:8434–8443. doi: 10.1128/jvi.74.18.8434-8443.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall S L, Sarris C M, Tierney E L, London W T, Murphy B R. A cold-adapted mutant of parainfluenza virus type 3 is attenuated and protective in chimpanzees. J Infect Dis. 1993;167:958–962. doi: 10.1093/infdis/167.4.958. [DOI] [PubMed] [Google Scholar]
- 23.Hall S L, Stokes A, Tierney E L, London W T, Belshe R B, Newman F C, Murphy B R. Cold-passaged human parainfluenza type 3 viruses contain ts and non-ts mutations leading to attenuation in rhesus monkeys. Virus Res. 1992;22:173–184. doi: 10.1016/0168-1702(92)90049-f. [DOI] [PubMed] [Google Scholar]
- 24.Karron R A, Makhene M, Gay K, Wilson M H, Clements M L, Murphy B R. Evaluation of a live attenuated bovine parainfluenza type 3 vaccine in two- to six-month-old infants. Pediatr Infect Dis J. 1996;15:650–654. doi: 10.1097/00006454-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Karron R A, Wright P F, Hall S L, Makhene M, Thompson J, Burns B A, Tollefson S, Steinhoff M C, Wilson M H, Harris D O, et al. A live attenuated bovine parainfluenza virus type 3 vaccine is safe, infectious, immunogenic, and phenotypically stable in infants and children. J Infect Dis. 1995;171:1107–1114. doi: 10.1093/infdis/171.5.1107. [DOI] [PubMed] [Google Scholar]
- 26.Karron R A, Wright P F, Newman F K, Makhene M, Thompson J, Samorodin R, Wilson M H, Anderson E L, Clements M L, Murphy B R, Belshe R B. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J Infect Dis. 1995;172:1445–1450. doi: 10.1093/infdis/172.6.1445. [DOI] [PubMed] [Google Scholar]
- 27.Katz S L, Gellin B G. Measles vaccine: do we need new vaccines or new programs? Science. 1994;265:1391–1392. doi: 10.1126/science.8073281. [DOI] [PubMed] [Google Scholar]
- 28.Lee M S, Nokes D J, Hsu H M, Lu C F. Protective titres of measles neutralising antibody. J Med Virol. 2000;62:511–517. doi: 10.1002/1096-9071(200012)62:4<511::aid-jmv17>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 29.Martin J, Ferguson G L, Wood D J, Minor P D. The vaccine origin of the 1968 epidemic of type 3 poliomyelitis in Poland. Virology. 2000;278:42–49. doi: 10.1006/viro.2000.0614. [DOI] [PubMed] [Google Scholar]
- 30.Moss W J, Cutts F, Griffin D E. Implications of the human immunodeficiency virus epidemic for control and eradication of measles. Clin Infect Dis. 1999;29:106–112. doi: 10.1086/520136. [DOI] [PubMed] [Google Scholar]
- 31.Murphy B R, Chanock R M. Immunization against virus disease. In: Fields B N, Knipe D M, Howley P M, Chanock R M, Melnick J L, Monath T P, Roizman B, Straus S E, editors. Fields virology. 3rd ed. Vol. 1. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 467–498. [Google Scholar]
- 32.Osterhaus A, van Amerongen G, van Binnendijk R. Vaccine strategies to overcome maternal antibody mediated inhibition of measles vaccine. Vaccine. 1998;16:1479–1481. doi: 10.1016/s0264-410x(98)00112-1. [DOI] [PubMed] [Google Scholar]
- 33.Perry R T, Mmiro F, Ndugwa C, Semba R D. Measles infection in HIV-infected African infants. Ann N Y Acad Sci. 2000;918:377–380. doi: 10.1111/j.1749-6632.2000.tb05511.x. [DOI] [PubMed] [Google Scholar]
- 34.Polack F P, Auwaerter P G, Lee S H, Nousari H C, Valsamakis A, Leiferman K M, Diwan A, Adams R J, Griffin D E. Production of atypical measles in rhesus macaques: evidence for disease mediated by immune complex formation and eosinophils in the presence of fusion-inhibiting antibody. Nat Med. 1999;5:629–634. doi: 10.1038/9473. [DOI] [PubMed] [Google Scholar]
- 35.Prince G A, Horswood R L, Chanock R M. Quantitative aspects of passive immunity to respiratory syncytial virus infection in infant cotton rats. J Virol. 1985;55:517–520. doi: 10.1128/jvi.55.3.517-520.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schlereth B, Rose J K, Buonocore L, ter Meulen V, Niewiesk S. Successful vaccine-induced seroconversion by single-dose immunization in the presence of measles virus-specific maternal antibodies. J Virol. 2000;74:4652–4657. doi: 10.1128/jvi.74.10.4652-4657.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmidt A C, McAuliffe J M, Huang A, Surman S R, Bailly J E, Elkins W R, Collins P L, Murphy B R, Skiadopoulos M H. Bovine parainfluenza virus type 3 (BPIV3) fusion and hemagglutinin-neuraminidase glycoproteins make an important contribution to the restricted replication of BPIV3 in primates. J Virol. 2000;74:8922–8929. doi: 10.1128/jvi.74.19.8922-8929.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schnell M J, Buonocore L, Kretzschmar E, Johnson E, Rose J K. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc Natl Acad Sci USA. 1996;93:11359–11365. doi: 10.1073/pnas.93.21.11359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Skiadopoulos M H, Durbin A P, Tatem J M, Wu S L, Paschalis M, Tao T, Collins P L, Murphy B R. Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J Virol. 1998;72:1762–1768. doi: 10.1128/jvi.72.3.1762-1768.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Skiadopoulos M H, McBride A A. The bovine papillomavirus type 1 E2 transactivator and repressor proteins use different nuclear localization signals. J Virol. 1996;70:1117–1124. doi: 10.1128/jvi.70.2.1117-1124.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Skiadopoulos M H, Surman S R, Durbin A P, Collins P L, Murphy B R. Long nucleotide insertions between the HN and L protein coding regions of human parainfluenza virus type 3 yield viruses with temperature-sensitive and attenuation phenotypes. Virology. 2000;272:225–234. doi: 10.1006/viro.2000.0372. [DOI] [PubMed] [Google Scholar]
- 42.Skiadopoulos M H, Surman S R, St. Claire M, Elkins W R, Collins P L, Murphy B R. Attenuation of the recombinant human parainfluenza virus type 3 cp45 candidate vaccine virus is augmented by importation of the respiratory syncytial virus cpts530 L polymerase mutation. Virology. 1999;260:125–135. doi: 10.1006/viro.1999.9802. [DOI] [PubMed] [Google Scholar]
- 43.Stittelaar K J, Wyatt L S, de Swart R L, Vos H W, Groen J, van Amerongen G, van Binnendijk R S, Rozenblatt S, Moss B, Osterhaus A D. Protective immunity in macaques vaccinated with a modified vaccinia virus Ankara-based measles virus vaccine in the presence of passively acquired antibodies. J Virol. 2000;74:4236–4243. doi: 10.1128/jvi.74.9.4236-4243.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor J, Weinberg R, Tartaglia J, Richardson C, Alkhatib G, Briedis D, Appel M, Norton E, Paoletti E. Nonreplicating viral vectors as potential vaccines: recombinant canarypox virus expressing measles virus fusion (F) and hemagglutinin (HA) glycoproteins. Virology. 1992;187:321–328. doi: 10.1016/0042-6822(92)90321-f. [DOI] [PubMed] [Google Scholar]
- 45.Taylor W R, Mambu R K, ma-Disu M, Weinman J M. Measles control efforts in urban Africa complicated by high incidence of measles in the first year of life. Am J Epidemiol. 1988;127:788–794. doi: 10.1093/oxfordjournals.aje.a114860. [DOI] [PubMed] [Google Scholar]
- 46.Valsamakis A, Auwaerter P G, Rima B K, Kaneshima H, Griffin D E. Altered virulence of vaccine strains of measles virus after prolonged replication in human tissue. J Virol. 1999;73:8791–8797. doi: 10.1128/jvi.73.10.8791-8797.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Wyke Coelingh K L, Murphy B R, Collins P L, Lebacq-Verheyden A M, Battey J F. Expression of biologically active and antigenically authentic parainfluenza type 3 virus hemagglutinin-neuraminidase glycoprotein by a recombinant baculovirus. Virology. 1987;160:465–472. doi: 10.1016/0042-6822(87)90018-3. [DOI] [PubMed] [Google Scholar]
- 48.van Wyke Coelingh K L, Winter C, Murphy B R. Antigenic variation in the hemagglutinin-neuraminidase protein of human parainfluenza type 3 virus. Virology. 1985;143:569–582. doi: 10.1016/0042-6822(85)90395-2. [DOI] [PubMed] [Google Scholar]
- 49.Wild F, Giraudon P, Spehner D, Drillien R, Lecocq J P. Fowlpox virus recombinant encoding the measles virus fusion protein: protection of mice against fatal measles encephalitis. Vaccine. 1990;8:441–442. doi: 10.1016/0264-410x(90)90243-f. [DOI] [PubMed] [Google Scholar]
- 50.Wild T F, Bernard A, Spehner D, Drillien R. Construction of vaccinia virus recombinants expressing several measles virus proteins and analysis of their efficacy in vaccination of mice. J Gen Virol. 1992;73:359–367. doi: 10.1099/0022-1317-73-2-359. [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization. Expanded programme on immunization. Accelerated measles strategies. Wkly Epidemiol Rec. 1994;69:229–234. [PubMed] [Google Scholar]
- 52.Wright P F, Karron R A, Belshe R B, Thompson J, Crowe J E, Jr, Boyce T G, Halburnt L L, Reed G W, Whitehead S S, Anderson E L, Wittek A E, Casey R, Eichelberger M, Thumar B, Randolph V B, Udem S A, Chanock R M, Murphy B R. Evaluation of a live, cold passaged, temperature-sensitive, respiratory syncytial virus vaccine candidate in infancy. J Infect Dis. 2000;182:1331–1342. doi: 10.1086/315859. [DOI] [PubMed] [Google Scholar]
- 53.Wyatt L S, Shors S T, Murphy B R, Moss B. Development of a replication-deficient recombinant vaccinia virus vaccine effective against parainfluenza virus 3 infection in an animal model. Vaccine. 1996;14:1451–1458. doi: 10.1016/s0264-410x(96)00072-2. [DOI] [PubMed] [Google Scholar]
- 54.Zhu Y, Rota P, Wyatt L, Tamin A, Rozenblatt S, Lerche N, Moss B, Bellini W, McChesney M. Evaluation of recombinant vaccinia virus—measles vaccines in infant rhesus macaques with preexisting measles antibody. Virology. 2000;276:202–213. doi: 10.1006/viro.2000.0564. [DOI] [PubMed] [Google Scholar]
- 55.Zhu Y D, Fennelly G, Miller C, Tarara R, Saxe I, Bloom B, McChesney M. Recombinant bacille Calmette-Guerin expressing the measles virus nucleoprotein protects infant rhesus macaques from measles virus pneumonia. J Infect Dis. 1997;176:1445–1453. doi: 10.1086/514140. [DOI] [PubMed] [Google Scholar]