Abstract
Background
The Revised Body Awareness Rating Questionnaire (BARQ-R) is a self-report measure of body awareness. First aim: evaluate the structural validity of BARQ-R with Rasch analysis in community-dwelling Americans with and without musculoskeletal pain. Subaim: validate a Rasch analysis of BARQ-R done in Norwegian adults with musculoskeletal pain, through a secondary analysis in our sample of Americans with musculoskeletal pain.
Methods
BARQ-R has 12 items with scores ranging from 0 (completely disagree) to 3 (completely agree), with higher total scores reflecting lower degrees of body awareness. Through Rasch analysis, we evaluated unidimensionality, item hierarchy, and structural validity with item and person fit, targeting, person separation reliability (PSR), local item dependence (LID), differential item functioning (DIF), and principal components analysis of residuals (PCAR).
Results
We recruited 623 adults with and without musculoskeletal pain (average age = 50.27 ± 17.25 years). After rescoring 1 item and deleting 3 items, the 9-item Rasch-based BARQ-R had no misfitting items, the hierarchical ordering of the items followed clinical expectations, 3 (0.48%) misfitting persons, person mean location: -0.62 ± 1.03 logits (max -0.53, min 0.72 logits), minimal floor effect (1.93%) and ceiling effect (0.48%), no DIF, and PSR = 0.72. LID was found in 5 item pairs. The PCAR’s eigenvalue was 2.18. The secondary Rasch analysis in 152 adults with musculoskeletal pain (average age = 52.26 ± 16.13 years), demonstrated that, after rescoring 2 items, BARQ-R had no misfitting items and only 2 (1.32%) misfitting persons, good targeting (person mean location: -0.36 ± 0.88 logits), minimal floor effect (0.01%), no ceiling effect (0.00%), and PSR = 0.75. LID was found in 6 item pairs. The PCAR’s eigenvalue was 2.47.
Conclusions
BARQ-R had good item and person fit. PSR with items covering a limited logit range suggests that differing levels of body awareness are measured with only modest precision. Adding and revising items to cover a wider range of body awareness and to better address concepts of internal body awareness and body movements would improve BARQ-R’s utility. Further analyses are needed before BARQ-R’s use for research or in the clinic. In addition, future BARQ-R Rasch validation is needed in other populations with body awareness deficits, such as stroke or spinal cord injury.
Keywords: Validation study, Musculoskeletal pain, Healthy volunteers
Introduction
Body awareness has been defined as the ability to be consciously aware of (1) integrated multisensory body signals (such as visual, auditory, tactile, proprioceptive, and interoceptive signals); (2) body posture and body movements; (3) how body parts are situated in relation to other body parts; and (4) how the body is situated in space [1–10]. Roxendal (1985) adds two other aspects to the definition of body awareness, which are (5) feelings about one’s whole body, and (6) attitude to one’s physical capacity regarding movements and exercise [11, 12]. These two aspects also emerged during focus groups with participants with chronic musculoskeletal pain: “to be aware of one’s own body, associations about one’s own body, and feelings for one’s own body” [11]. Research has demonstrated that chronic pain is associated with decreased levels of body awareness [13–16]. Therefore, a body awareness scale can be useful in the clinic to assess those with chronic pain.
To measure body awareness, Dragesund et al. (2010) developed the Body Awareness Rating Questionnaire (BARQ), which is a 24-item patient-reported outcome measure with the following aspects of body awareness (and their reported internal consistency): Function (Cronbach’s α = 0.85), Mood (Cronbach’s α = 0.76), Feelings (Cronbach’s α = 0.79), and Awareness (Cronbach’s α = 0.69) [17]. The scale was designed for adults with chronic musculoskeletal pain and psychosomatic disorders [17]. The rationale behind the development of this scale was that if people are aware of their body posture and muscle tension, they will readjust their posture more quickly [17], thereby avoiding muscle tension and resulting pain. Dragesund et al. (2018) analyzed the structural validity of the 24-item BARQ with Rasch Measurement Theory [18] in Norwegian adults with musculoskeletal pain, which resulted in the Revised Body Awareness Rating Questionnaire (BARQ-R) with 12 items reflecting statements on body awareness, on a 4-point ordinal scale ranging from 0 (completely disagree) to 3 (completely agree), and with higher scores reflecting lower degrees of body awareness [18]. The 12 items had a person mean location of -0.04 ± 0.74 logits, person separation reliability (PSR) = 0.76, no disordered thresholds, good item fit, and unidimensionality. They found no differential item functioning (DIF) for sex (men: women), age (less than 43 years of age: 43 years or above), or duration of musculoskeletal pain (less than 5 years: 5 years or more).
A clinical use of the scale could be to measure changes in body awareness after treatments, e.g., to reduce pain [19] in adults with chronic musculoskeletal pain, but in that case, we would also need to ensure that the BARQ-R is structurally valid for adults with and without musculoskeletal pain. Additionally, it is important to note that BARQ-R has not yet been validated with Rasch analysis in other countries than Norway.
Therefore, in this study, our first aim was to evaluate the structural validity of the BARQ-R with Rasch analysis in community-dwelling adults with and without musculoskeletal pain in the United States (US). Our subaim was to validate Dragesund et al. (2018)’s Rasch analysis of the BARQ-R done in Norwegian adults with musculoskeletal pain, through a secondary analysis in our sample of adults with musculoskeletal pain in the US. In addition to the previously mentioned Rasch-based outputs that Dragesund et al. (2018) reported, we report mean error variance, floor and ceiling effects, and local item dependence (LID). For our two aims, we hypothesize that we will obtain good item and person fit, reflected by Chi-square fit residuals below 2.50 and non-significant Bonferroni corrected p-values, when the significance level is set at α = 0.05. Other outputs related to structural validity and unidimensionality are detailed in the statistical analysis section below.
Materials and methods
Participants
Participants were recruited from July 20th, 2019, through July 3rd, 2023. English-speaking community-dwelling adults (18 + years) with and without self-reported musculoskeletal pain were recruited through convenience sampling at the Minnesota State Fair and Highland Fest. Volunteer sampling was used for adults who were on a research volunteer contact list of the Brain Body Mind Lab at the University of Minnesota, because they had expressed a prior interest in being contacted for future research of the Brain Body Mind Lab, or they were part of a chronic low back pain study, for which the baseline assessment of BARQ-R was used here.
This study adhered to the principles of the Declaration of Helsinki (2013) and received approval from the Institutional Review Board of the University of Minnesota (IRB#s 00005656; 00005849). All participants provided informed consent. Adults with chronic low back pain signed consent on paper. At the Minnesota State Fair and Highland Fest, adults completed the BARQ-R as part of an anonymous survey on an iPad. Participants from the contact list completed the BARQ-R as part of an anonymous survey via email. Therefore, we did not collect any personal or identifiable information (including signatures) from those participants. After they read the consent form on an iPad/email and provided consent, those participants were quizzed on the comprehension of the content of the consent form through the University of California, San Diego Brief Assessment of Capacity to Consent (UBACC) [20]. All information was stored automatically on the secure University of Minnesota REDCap platform.
Main outcome measure
We used an observational study design to assess the structural validity of the BARQ-R. The BARQ-R is a reliable and valid patient-reported outcome measure of body awareness consisting of 12 items, scored on a 4-point ordinal scale, with score 0 representing “completely disagree”; score 1 “somewhat disagree”; score 2 “somewhat agree”; and score 3 “completely agree” [17]. Higher scores reflect lower degrees of body awareness [17].
Sample size calculation
We based our sample size on the Rasch Reporting Guideline for Rehabilitation Research (RULER) guideline’s recommendation that useful information can be obtained from sample sizes of n ≥ 100 if the mean error variance is ≤ 0.25 logits [21–23].
Statistical analysis
Descriptive statistics are reported for demographic, lifestyle, and general health information.
The Rasch model is a probabilistic model, which states that a person with a higher ability on a certain construct (i.e., body awareness ability) would have a higher probability of obtaining a better score on the scale (i.e., in this case a lower score) measuring that construct [24].
We assessed the BARQ-R with Rasch Measurement Theory using a Polytomous Partial Credit Model. We analyzed the data through the Rasch Unidimensional Measurement Model (RUMM2030) software (RUMM Laboratory, Perth, WA, Australia). Additional outputs were calculated with WINSTEPS 5.7.0.0. Output was reported following the RULER guidelines [21, 22]. We evaluated: (1) the presence of reversed thresholds, which can be solved by rescoring items (i.e., collapsing scoring categories); (2) item and person fit, with item and person misfit reflected by fit residuals above 2.50 with significant Bonferroni corrected p-values, when the significance level is set at α = 0.05. This is solved by deleting misfitting items one by one, and verifying the structural validity of the scale again without the presence of the misfitting item; [24]; We also investigate the hierarchy of the items; (3) targeting of the population, with good targeting reflected by the average person location being within 0.5 logits above or below the average item location (set by default at 0 logits ± 1 standard deviation) and less than 15% floor and ceiling effects [25]; and (4) PSR, which reflects how well we can distinguish groups of persons high versus low levels of body awareness [26], with PSR ≥ 0.70 sufficient for group decisions and PSR ≥ 0.90 sufficient for individual decisions [21, 22]. We also evaluated (5) Local item dependence (LID), measured through residual correlations, with those at least r = 0.20 above the average correlation, indicating pairs of items that are more correlated with each other, and thus sharing more content with this paired item than with other items in the scale; and (6) unidimensionality, in part tested through Principal Component Analysis of Residuals (PCAR) [21, 22] with suggestions of unidimensionality if the eigenvalue is < 2.00, and the percent variance on the first residual factor is < 10% [21, 22]. Furthermore, less than 5% of person logit locations are significantly different in a paired sample t-test, created by two subtests of the BARQ-R items, is suggestive of unidimensionality. The two subtests are created by items having negative (r<-0.3) vs. positive (r > 0.3) loadings with the first principal component. Of note, this test should not be viewed as a “definite” test for unidimensionality and does not replace an integrated interpretation based on context, purpose of measurement, and item fit, given that PCAR is dependent on sample size and the number of items selected in the paired t-test influences the interpretation of the results as well [27].
The Rasch analysis produces an item map, with items hierarchically ordered from hardest to easiest (top to bottom). For analyses revealing good structural validity, we provide a score-to-measure table relating the ordinal total score to the Rasch-based logit score and transformed logit score to 0-100%, for easier use in the clinic or research, as well as a scoring sheet with the new Rasch-based items. Of note, these score-to-measure tables can only be used for full datasets. (7) Lastly, we reported whether DIF is present for demographic or lifestyle outcomes whose samples are greater than 200 participants in each subgroup [21, 22]. In our case, DIF could be calculated in the whole group of community-dwelling adults with and without musculoskeletal pain for type of group (adults with pain; adults without pain), age (less than 65 years of age: 65 years or above), sex (men: women), past body awareness practice (yes; no) and current body awareness practice (yes: no). We did not calculate DIF for the secondary analysis of the subgroup of adults with musculoskeletal pain.
Results
Demographic data
There were 623 community-dwelling adults with and without self-reported musculoskeletal pain (mean age = 50.28 ± 17.25 years). In total, there were 72 participants (11.56%) of diverse racial backgrounds. Thirteen adults (2.09%) were Hispanic, i.e., 7 (1.12%) Hispanic-White and 6 (0.96%) Hispanic with diverse backgrounds.
Among this group,152 adults had musculoskeletal pain (mean age = 52.26 ± 16.13 years, 14.48% of diverse race). Table 1 displays the demographic, lifestyle, and general health information for the group with and without self-reported musculoskeletal pain, as well as for the subgroup with musculoskeletal pain separately.
Table 1.
Demographic, lifestyle, and general health data in community-dwelling adults with and without musculoskeletal pain
| Community-dwelling adults with and without musculoskeletal pain (n = 623) |
Subgroup of adults with musculoskeletal pain (n = 152) |
|
|---|---|---|
| Age (years, mean ± SD) | 50.27 ± 17.25 | 52.26 ± 16.13 |
| Sex (%) | ||
| Male | 33.87 | 23.03 |
| Female | 66.13 | 76.97 |
| Gender (%) | ||
| Male | 37.88 | 34.87 |
| Female | 61.48 | 64.47 |
| Non-binary | 0.32 | 0.00 |
| A-gender | 0.16 | 0.00 |
| Other | 0.16 | 0.66 |
| Racial background (%) | ||
| American Indian/Alaskan | 0.48 | 1.32 |
| Asian | 5.78 | 5.26 |
| Black/African American | 2.09 | 2.63 |
| Hawaiian/other Pacific Islander | 0.00 | 0.00 |
| Multiracial | 1.77 | 0.66 |
| Other | 1.44 | 4.61 |
| White | 88.44 | 85.52 |
| Ethnicity (%) | ||
| Hispanic | 2.09 | 3.29 |
| Non-Hispanic | 97.91 | 96.71 |
| Current Body Awareness Training (% yes) | 32.91 | 30.26 |
| Past Body Awareness Training (% yes) | 65.17 | 69.08 |
| Current Breathing Exercises (% yes) | 43.18 | 48.03 |
Rasch measurement theory
We first conducted a Rasch analysis of community-dwelling adults with and without musculoskeletal pain in the US. We then validated Dragesund et al. (2018)’s Rasch analysis, performed in adults in Norway, by performing a secondary Rasch subanalysis in our sample of adults with musculoskeletal pain. Below is the summary per target group. All iteration steps for each group are shown in Table 2.
Table 2.
Iteration table
| Analysis | Items | Rating scale cate- gories |
Person Mean (SD) logits | Mean error vari- ance |
Floor Effect n (%) | Ceiling Effect n (%) |
Overall Chi-square (DF) p-value |
PSR | Number of items with disordered thresholds | Number of misfitting Items | PCAR Eigenvalue (% variance) Paired sample t-test |
Number and % mis-fitting per-sons |
DIF |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OUR ANALYSIS | |||||||||||||
|
Community-dwelling adults with and without pain (n = 623) |
12 | 48 |
-0.40 (0.85) |
0.15 |
7 (1.12%) |
2 (0.32%) |
325.82 (108) p < 0.00001 |
0.74 |
2 (items 2,12) |
2 (item 11) Res = 3.73 p < 0.00001 (item 12) Res = 3.42 p = 0.002 |
2.33 (19.46%) |
10 (1.61%) |
|
|
Community-dwelling adults with and without pain (n = 623) rescored 2 (0012), 12 (0011) |
12 | 45 |
-0.48 (0.89) |
0.17 |
8 (1.28%) |
2 (0.32%) |
323.86 (108) p < 0.00001 |
0.74 | 0 |
1 (item 11) Res = 4.15 p < 0.00001 |
2.33 (19.41%) |
8 (1.28%) |
|
|
Community-dwelling adults with and without pain (n = 623) delete item 11 |
11 | 41 |
-0.49 (0.93) |
0.19 |
8 (1.28%) |
3 (0.48%) |
307.98 (99) p < 0.00001 |
0.73 | 0 |
3 (item 3) Res = 3.86 p = 0.00001 (item 4) Res = 3.37 p = 0.0002 (item 8) Res = 3.97 p = 0.00004 |
2.09 (19.01%) |
6 (0.96%) |
|
|
Community-dwelling adults with and without pain (n = 623) delete item 8 |
10 | 37 |
-0.55 (0.98) |
0.22 |
9 (1.44%) |
3 (0.48%) |
237.75 (90) p < 0.00001 |
0.73 | 0 |
2 (item 2) Res = 3.49 p = 0.005 (item 3) Res = 3.29 p = 0.003 |
2.17 (21.70%) |
4 (0.64%) |
|
|
Community-dwelling adults with and without pain (n = 623) delete item 2 |
9 | 34 |
-0.62 (1.03) |
0.25 |
12 (1.93%) |
3 (0.48%) |
205.75 (81) p < 0.00001 |
0.72 | 0 | 0 |
2.18 (24.23%) Paired t-test 7.22% |
3 (0.48%) |
No DIF |
|
Adults with musculo-skeletal pain (n = 152) |
12 | 48 |
-0.25 (0.83) |
0.15 | 2 (1.32%) | 0 |
149.20 (108) p = 0.005 |
0.75 |
2 (items 2,12) |
0 |
2.43 (20.21%) |
2 (1.32%) |
|
|
Adults with musculo-skeletal pain (n = 152) rescored items 2 (0012),12 (0011) |
12 | 45 |
-0.36 (0.88) |
0.17 | 2 (1.32%) | 0 | 149.91 (108) p = 0.005 | 0.75 | 0 | 0 |
2.47 (20.55%) Paired t-test 13.82% |
2 (1.32%) |
NA |
| ANALYSIS DRAGESUND et al. (2018) | |||||||||||||
|
Dragesund (n = 127) Adults with musculo-skeletal pain |
12 | 48 | -0.04 (0.74) | NA | NA | NA |
13.63, p = 0.95 |
0.76 | 0 | 0 |
NA Uni-dimensio-nal |
NA | No DIF |
Legend: DF = degrees of freedom; DIF = Differential Item Functioning; NA = not applicable, this analysis was not performed; No DIF = The DIF analysis was performed but no DIF was found; PCAR = Principal Components Analysis of Residuals; PSR = Person Separation Reliability; Res = Fit Residual; SD = standard deviation
Community-dwelling adults with and without self-reported musculoskeletal pain
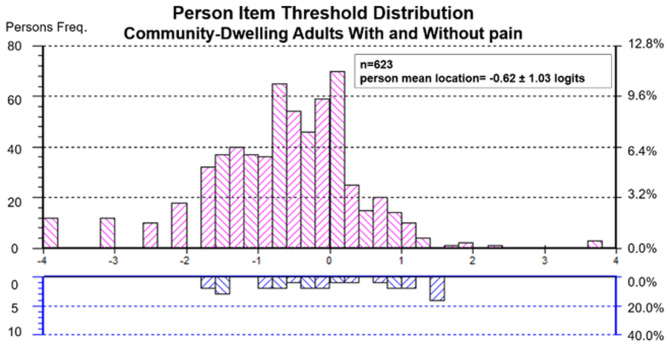
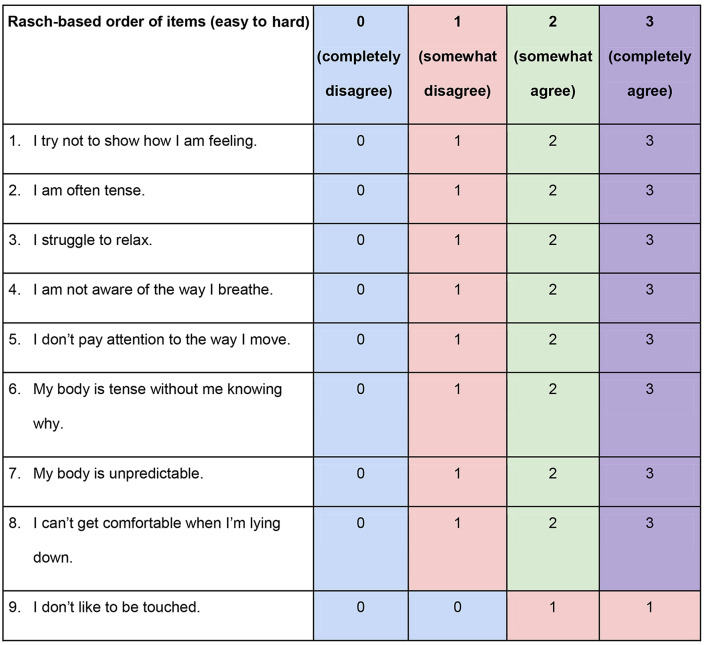
Initially, for community-dwelling adults with and without musculoskeletal pain (n = 623), two items presented misfit: item 11 “I avoid paying too much attention to my body” (Fit Residual = 3.73, p < 0.00001), and item 12 “I don’t like to be touched” (Fit Residual = 3.42, p = 0.000001). Additionally, two items (item 2 “My body is affected by how I feel”, and item 12) had disordered category thresholds. After rescoring item 2 to three categories [0-0-2-3] and item 12 to two categories [0-0-3-3], from the original scoring options [0-1-2-3], only item 11 was misfitting (Fit Residual = 3.73, p < 0.000014). After deleting item 11, three items displayed misfit: item 3 “I am not aware of the way I breathe” (Fit Residual = 3.86, p = 0.0001), item 4 “I don’t pay attention to the way I move” (Fit Residual = 3.37, p = 0.0002), and item 8 “My digestion is affected by how I feel” (Fit Residual = 3.37, p = 0.00004). After deleting item 8, there were two misfitting items, item 2 (Fit Residual = 3.49, p = 0.005), and item 3 (Fit Residual = 3.29, p = 0.003). After deleting item 2, the revised 9-item BARQ-R had no more items with disordered thresholds or misfitting items. There were only 3 (0.48%) misfitting persons. The person mean location was − 0.62 ± 1.03 logits (Fig. 1) which is close to being well-targeted. The mean standard error was 0.25 logits. The standard error of each of the 9 items ranged between 0.05 and 0.10 logits (Table 3). There were minimal floor (1.93%), and ceiling effects (0.48%). The scale showed sufficient reliability for group decision-making in this population (PSR = 0.72). The item fit statistics can be found in Table 3. Table 3 shows the hierarchy of the items, with “I try not to show how I am feeling” being the hardest item, and “I don’t like to be touched” being the easiest item for this group (Fig. 2). Consequential LID was found in 5 item pairs (Table 4A). PCAR had an eigenvalue of 2.18 (with percent variance of 24.23%). The paired t-test resulted in 7.22% of persons having a significantly different logit location on the two subtests, produced by respectively 2 and 3 items with positive vs negative loadings on the first principal component. There was no DIF for the type of group, age, sex, past body awareness practice, or current body awareness practice. The score-to-measure table is provided in Table 5 and the scoring sheet is provided in Table 6.
Fig. 1.
Person-item threshold distribution maps. Legend: The histogram shows the frequency of adults with and without musculoskeletal pain at their level of body awareness ability (pink histograms). Body awareness ability ranges from high (lowest logit value on the left side of the scale) to low (highest logit value on the right side of the scale). At the bottom of the figure, the blue histograms represent the frequency of item thresholds. Following the same logit scale, the hardest items are shown on the left, and the easiest items are shown on the right
Table 3.
Item fit statistics for the BARQ-R in community-dwelling adults with and without musculoskeletal pain
| Item | Location (logits) | Standard Error | Chi-Square | Fit Residuals | p-value |
|---|---|---|---|---|---|
| 7. I try not to show how I am feeling. | -0.53 | 0.05 | 21.91 | 3.20 | 0.01 |
| 1. I am often tense. | -0.47 | 0.05 | 28.44 | -2.20 | 0.0008 |
| 5. I struggle to relax. | -0.28 | 0.05 | 33.53 | -3.01 | 0.0001 |
| 3. I am not aware of the way I breathe. | -0.25 | 0.05 | 20.91 | 3.15 | 0.01 |
| 4. I don’t pay attention to the way I move. | 0.02 | 0.06 | 19.64 | 2.91 | 0.02 |
| 6. My body is tense without me knowing why. | 0.02 | 0.05 | 39.78 | -3.83 | 0.000008 |
| 9. I can’t get comfortable when I am lying down. | 0.40 | 0.05 | 10.45 | 0.29 | 0.32 |
| 10. My body is unpredictable. | 0.38 | 0.05 | 19.65 | 0.32 | 0.02 |
| 12. I don’t like to be touched. | 0.72 | 0.10 | 11.44 | 1.38 | 0.25 |
Legend: The Bonferroni adjusted p-value for 9 items = 0.006
Fig. 2.
Item threshold maps. Legend: The item threshold map shows the hardest items on the top to the easiest items on the bottom for adults with and without musculoskeletal pain
Table 4.
Local item dependence (LID) calculated with residual correlations for (A) community-dwelling adults with and without musculoskeletal pain and (B) adults with musculoskeletal pain
| Original numbering of BARQ-R items | Correlation | |
|---|---|---|
| A. Community-dwelling adults with and without pain r = -0.12 (LID ≥ 0.08) | ||
|
1. I am often tense. 5. I struggle to relax. |
0.20 | |
|
1. I am often tense. 6. My body is tense without me knowing why. |
0.17 | |
|
5. I struggle to relax. 6. My body is tense without me knowing why. |
0.19 | |
|
9. I can’t get comfortable when I am lying down. 10. I don’t like to be touched. |
0.13 | |
|
6. My body is tense without me knowing why. 9. I can’t get comfortable when I am lying down. |
0.15 | |
| B. Adults with musculoskeletal pain r = -0.09 (LID ≥ 0.11) | ||
|
1. I am often tense. 6. My body is tense without me knowing why. |
0.31 | |
|
3. I am not aware of the way I breathe. 4. I don’t pay attention to the way I move. |
0.55 | |
|
3. I am not aware of the way I breathe. 11. I avoid paying too much attention to my body. |
0.17 | |
|
4. I don’t pay attention to the way I move. 11. I avoid paying too much attention to my body. |
0.14 | |
|
5. I struggle to relax. 6. My body is tense without me knowing why. |
0.21 | |
|
7. I try not to show how I am feeling. 12. I don’t like to be touched. |
0.12 | |
Table 5.
Rasch-based score-to-measure table for community-dwelling adults with and without musculoskeletal pain
| Total BARQ-R Score | Logits RUMM |
Logits WINSTEPS |
Standard Error WINSTEPS |
Converted logits to 0-100 WINSTEPS |
|---|---|---|---|---|
| 0 | -3.81E | -3.86E | 1.14 | 0.00E |
| 1 | -3.01 | -3.62 | 1.03 | 19.93 |
| 2 | -2.45 | -2.87 | 0.75 | 26.30 |
| 3 | -2.06 | -2.40 | 0.63 | 30.29 |
| 4 | -1.76 | -2.04 | 0.57 | 33.34 |
| 5 | -1.50 | -1.74 | 0.53 | 35.88 |
| 6 | -1.27 | -1.48 | 0.50 | 38.11 |
| 7 | -1.07 | -1.24 | 0.48 | 40.15 |
| 8 | -0.87 | -1.02 | 0.47 | 42.04 |
| 9 | -0.69 | − 0.81 | 0.45 | 43.84 |
| 10 | -0.51 | − 0.60 | 0.45 | 45.56 |
| 11 | -0.34 | − 0.41 | 0.44 | 47.24 |
| 12 | -0.17 | − 0.21 | 0.44 | 48.88 |
| 13 | 0.00 | − 0.02 | 0.44 | 50.51 |
| 14 | 0.18 | 0.17 | 0.44 | 52.14 |
| 15 | 0.35 | 0.37 | 0.44 | 53.80 |
| 16 | 0.53 | 0.57 | 0.45 | 55.50 |
| 17 | 0.72 | 0.78 | 0.46 | 57.26 |
| 18 | 0.93 | 1.00 | 0.48 | 59.14 |
| 19 | 1.15 | 1.24 | 0.50 | 61.17 |
| 20 | 1.39 | 1.50 | 0.53 | 63.42 |
| 21 | 1.66 | 1.81 | 0.58 | 66.01 |
| 22 | 1.98 | 2.17 | 0.64 | 69.14 |
| 23 | 2.39 | 2.66 | 0.76 | 73.26 |
| 24 | 2.97 | 3.43 | 1.04 | 79.82 |
| 25 | 3.80E | 3.67E | 1.15 | 100.00E |
Table 6.
Scoring sheet of the BARQ-R for community-dwelling adults with and without pain
Secondary analysis: subgroup of adults with musculoskeletal pain
For the subgroup consisting of adults with musculoskeletal pain (n = 152), initially 2 items (items 2 “My body is affected by how I feel” and item 12 “I don’t like to be touched”) had disordered thresholds. Upon rescoring item 2 from scoring options [0-1-2-3] to scoring options [0-0-1-2] and item 12 to scoring options [0-0-1-1], there were no disordered items or misfitting items. There were only 2 (1.32%) misfitting persons. The 12-item BARQ-R showed good targeting for adults with musculoskeletal pain: person mean location: -0.36 ± 0.88 logits, minimal floor effect (0.01%), and no ceiling effect (0.00%). Reliability (PSR = 0.75) indicated sufficient reliability for group decision-making and distinguishing groups with high versus low body awareness ability. The hardest item was, “My body is affected by how I feel” and the easiest item was “I don’t like to be touched”. LID was found in 6 item pairs (Table 4B). PCAR had an eigenvalue of 2.47 (with percent variance of 20.55%). The paired t-test resulted in 13.82% of persons having a significantly different logit location on the two subtests, created by the positive (2 items) and negative principal component loadings (3 items). We did not calculate DIF because the sample size in the subgroups for demographic and lifestyle outcomes were too small.
Discussion
We analyzed the structural validity of the BARQ-R in community-dwelling adults with and without musculoskeletal pain with Rasch analysis (Aim 1). As a secondary analysis, we validated in a US sample, Dragesund et al. (2018)’s Rasch analysis results on the BARQ-R in adults with musculoskeletal pain (subaim). Overall, the BARQ-R has good structural validity in both the group of adults with and without musculoskeletal pain and the subgroup of adults with musculoskeletal pain, but measurement precision could be improved.
Community-dwelling adults with and without musculoskeletal pain
Structural validity of the BARQ-R was obtained after rescoring 1 item (i.e., item 12) and deleting 3 items (i.e., items 2, 8, and 11). The hierarchy of items indicates that “trying not to show how I feel” is the hardest item, whereas deciding whether we “like to be touched” is the easiest item.
Also given the high rate of people having low back pain, it may be easier to endorse that it is difficult to get comfortable lying down. Conversely, people do not always pay attention to their bodies and thus it may be harder to endorse an awareness that the body is tense, or that they are unable to relax. Further, depending on how someone is raised and what the belief system is about being allowed to express one’s feelings, “trying not to show how I am feeling” may be a difficult item to endorse.
Item 11, which was misfitting, seemed to cohere the deleted misfitting ‘attention items’ (items 2 and 8) to the rest of the scale. Those attention items (items 2, 8, 11) were negatively worded. Combining positively and negatively worded items in the same scale may result in measurement inaccuracies, which could have been why those items were misfitting [28, 29]. Relating emotions to feelings in the body may be an important aspect of body awareness. A solution for future Rasch analysis with BARQ-R may be to rephrase those items in a positive way and run the analysis again.
One reason why item 12 “I don’t like to be touched” needed to be rescored is that it could be related to personality or personal preference in being comfortable with being touched rather than whether one is aware of the body or not. Sometimes participants questioned whether this question referred to strangers or friends/close family.
With regards to the items used in the paired t-tests following the PCAR analysis, the coherence between the items is not as robust as we would like. Items 3 “I am not aware of the way I breathe” and 4 “I don’t pay attention to the way I move” had a positive loading on the first principal component. Items 1 “I am often tense”, 5 “I struggle to relax”, and 6 “My body is tense without me knowing why” had negative loading on the first principal component. The items with positive loadings could be related to “awareness of physical aspects of the body, requiring conscious or unconscious activation of muscles.” Breathing and moving can be easily perceived, also in adults who do not have pain. All items with negative loadings on the first component measured some aspects of “awareness of being tense,” which is a specific sensory awareness of the body related to the musculoskeletal system. Painful tension is often present in adults with musculoskeletal pain but adults without pain can perceive tension that is not (yet) painful. However, as mentioned in the methods, we want to point out that PCAR alone is not sufficient to declare that the scale is multidimensional, especially since in this particular case, the t-tests are only based on respectively 2 and 3 items [27]. Additionally, according to our additional Winstep analysis, there is not a lot of variance explained by residuals (15.6% explained by residuals) compared to 34.7% of variance explained by the measure.
Adults with musculoskeletal pain
Regarding the validation of the BARQ-R in adults with musculoskeletal pain, we found similar results as Dragesund et al. (2018) in terms of targeting (i.e., person mean location, floor and ceiling effect), PSR, and the fact that there were no reversed thresholds and that the BARQ-R had good item and person fit [18]. A minor difference was found in the hierarchy of item difficulty. The items were ordered the same way from negative logits to positive logits. Dragesund et al. (2018) reported “I am often tense” as the item at the top of the hierarchy whereas that item was reported as the third in our study. The item “My body is affected by how I feel” was reported as the first in our hierarchy, but was listed as second in Dragesund et al. (2018)’s study. Both Dragesund et al. (2018)’s and our analysis found “I don’t like to be touched” to be the last item. Dragesund et al. (2018) calculated DIF, but did not find DIF for sex, age, group, or duration of pain [18]. We did not report on DIF due to less than 200 participants in each subgroup, so we were unable to make a comparison, but we did not find DIF in the larger group.
Similar to the analysis in the larger group, the items that showed positive loadings with the first principal component were items 3, 4, and 11 “I avoid paying too much attention to my body”, and the items with negative loadings were items 1, 2 “My body is affected by how I feel”, 5, and 6, seeming to allude that the items do not cohere as strongly as we would expect. Item 11 “I avoid paying too much attention to my body”, would be a strategy one can employ to not feel pain. This item was removed in the larger group, because, content-wise, avoiding paying attention to the body may not be needed in persons who do not have pain, and it also garnered some confusion about what “too much” meant. Similarly, for the negatively loaded items, in the case of item 2 “My body is affected by how I feel”, pain is known to be associated with negative emotions or mood, so this item would make sense for people who have pain [30]. This item was also removed in the Rasch analysis of the larger group.
Hierarchy of items across both our analyses
The hierarchy of item difficulty is consistent across both our analyses (larger group with and without pain vs. adults with pain). The item “My body is affected by how I feel” was the hardest in the subgroup of adults with musculoskeletal pain. “I try not to show how I am feeling” was the second hardest item for adults with musculoskeletal pain. The item “My body is affected by how I feel” was deleted in the revised BARQ-R version for community-dwelling adults with and without musculoskeletal pain, and their hardest item was “I try not to show how I am feeling”. The item “I don’t like to be touched” was the easiest item across both analyses. Overall, the item logit locations are very similar for the whole group and the subanalysis of adults with musculoskeletal pain.
The main issue with BARQ-R is the modest measurement precision (PSR), which was apparent in both our Rasch analyses (PSR = 0.72 for the large group, PSR = 0.75 for the group with musculoskeletal pain) as well as in Dragesund et al. (2018)’s findings (PSR = 0.76). These results indicate that we cannot draw conclusions with regard to individual person’s body awareness levels. Moreover, the items do not cover a large logit range (only from − 0.47 to 0.72 logits). Items would need to cover a wider range of body awareness.
Limitations
We acknowledge that we have an underrepresentation of data from adults of diverse backgrounds across our groups. Our data was collected from adults in Minnesota, USA, where the majority of the population is non-Hispanic White (77.60%) [31]. Therefore, future studies should attempt to recruit data from different cultural and ethnic backgrounds, as well as investigate other types of diversity, such as sexual orientation, gender identification, Veteran status, adults living in rural, underserved areas, or adults experiencing socio-economic hardship. Moreover, it may be useful to test the structural validity of BARQ-R in adults with reported body awareness deficits, such as adults with spinal cord injury or stroke.
Conclusions
Overall, the BARQ-R has good structural validity regarding item and person fit, targeting, and reliability. The assessment had modest measurement precision, which hinders distinguishing body awareness ability among individual persons. Adding and revising items to cover a wider range of body awareness and to better address concepts of internal body awareness and body movements would further improve the utility of the BARQ. Further analyses need to be performed before using the BARQ-R scale for research or in the clinic. In addition, future Rasch analysis should include other populations that have reported body awareness deficits, such as adults with spinal cord injury or stroke.
Acknowledgements
We thank all participants; the Driven to Discover (D2D) Research Team; and the volunteers who helped at the D2D Facility at the Minnesota State Fair and at Highland Fest for providing us with the opportunity to carry out this study. We would like to thank Prof. Trudy Mallinson for her expert advice on data interpretion. We also would like to extend our deepest gratitude to Marc Noël for the critical review of the manuscript.
Abbreviations
- BARQ
Body Awareness Rating Questionnaire
- BARQ-R
Revised Body Awareness Rating Questionnaire
- DIF
Differential item functioning
- LID
Local item dependence
- PCAR
Principal Component Analysis of Residuals
- PSR
Personal Separation Reliability
- RULER
Rasch Reporting Guideline for Rehabilitation Research
- RUMM2030
Rasch Unidimensional Measurement Model
- US
United States
Author contributions
All authors contributed substantially to parts of the manuscript and critically revised it for content, approved the final version, and agreed to be accountable for the accuracy and integrity of this work. Specific contributions include: Conception or design of the work: AVDW; Acquisition and analysis of evidence: AVDW, SC, WD; Interpretation of the evidence: SC, AVDW, WD, JB; Writing - original draft; SC; Writing - review and editing: SC, AVDW, WD, JB.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health’s National Center for Advancing Translational Sciences. The funding agency had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Data availability
The dataset supporting the conclusions of this article is available in the Data Repository for the University of Minnesota (DRUM), 10.13020/qst8-dc65.
Declarations
Ethics approval and consent to participate
This study adhered to the principles of the most recent Declaration of Helsinki (2013) and received approval from the Institutional Review Board of the University of Minnesota (IRB#s 00005656; 00005849). All participants provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Garfinkel SN, Manassei MF, den Hamilton-Fletcher G. Bosch Y, Critchley HD, Engels M. Interoceptive dimensions across cardiac and respiratory axes. Philos Trans R Soc Lond B Biol Sci. 2016;371. [DOI] [PMC free article] [PubMed]
- 2.Park H-D, Blanke O. Coupling inner and outer body for self-consciousness. Trends Cogn Sci. 2019;23:377–88. [DOI] [PubMed] [Google Scholar]
- 3.Daprati E, Sirigu A, Nico D. Body and movement: consciousness in the parietal lobes. Neuropsychologia. 2010;48:756–62. [DOI] [PubMed] [Google Scholar]
- 4.Dijkerman HC, de Haan EH. Somatosensory processes subserving perception and action. Behav Brain Sci. 2007;30:189–201. discussion 201–39. [DOI] [PubMed] [Google Scholar]
- 5.Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, et al. Interoception and Mental Health: a Roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:501–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehling WE, Wrubel J, Daubenmier JJ, Price CJ, Kerr CE, Silow T, et al. Body awareness: a phenomenological inquiry into the common ground of mind-body therapies. Philos Ethics Humanit Med. 2011;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young KS, van der Velden AM, Craske MG, Pallesen KJ, Fjorback L, Roepstorff A, et al. The impact of mindfulness-based interventions on brain activity: a systematic review of functional magnetic resonance imaging studies. Neurosci Biobehav Rev. 2018;84:424–33. [DOI] [PubMed] [Google Scholar]
- 8.Gibson J. Mindfulness, Interoception, and the body: a contemporary perspective. Front Psychol. 2019;10:2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassanpour MS, Simmons WK, Feinstein JS, Luo Q, Lapidus RC, Bodurka J, et al. The Insular Cortex dynamically maps changes in Cardiorespiratory Interoception. Neuropsychopharmacology. 2018;43:426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gyllensten AL, Skär L, Miller M, Gard G. Embodied identity—A deeper understanding of body awareness. Physiother Theory Pract. 2010;26:439–46. [DOI] [PubMed] [Google Scholar]
- 11.Dragesund T, Råheim M. Norwegian psychomotor physiotherapy and patients with chronic pain: patients’ perspective on body awareness. Physiother Theory Pract. 2008;24:243–54. [DOI] [PubMed] [Google Scholar]
- 12.Roxendal G. Body awareness therapy and the body awareness scale: treatment and evaluation in psychiatric physiotherapy. 1985.
- 13.Mehling WE, Gopisetty V, Daubenmier J, Price CJ, Hecht FM, Stewart A. Body awareness: construct and self-report measures. PLoS ONE. 2009;4:e5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baskan E, Yagci N, Cavlak U. Factors affecting body awareness in older adults with chronic musculoskeletal pain. Arch Med Sci. 2021;17:934–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oliveira I, Garrido MV, Bernardes SF. On the body-mind nexus in chronic musculoskeletal pain: a scoping review. Eur J Pain. 2022;26:1186–202. [DOI] [PubMed] [Google Scholar]
- 16.Valenzuela-Moguillansky C, Reyes-Reyes A, Gaete MI. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front Hum Neurosci. 2017;11:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dragesund T, Ljunggren AE, Kvåle A, Strand LI. Body awareness rating questionnaire – development of a self-administered questionnaire for patients with long-lasting musculoskeletal and psychosomatic disorders. Adv Physiother. 2010;12:87–94. [Google Scholar]
- 18.Dragesund T, Strand LI, Grotle M. The revised body awareness rating questionnaire: Development into a Unidimensional Scale using Rasch Analysis. Phys Ther. 2018;98:122–32. [DOI] [PubMed] [Google Scholar]
- 19.Van de Winckel A, Zhang L, Hendrickson T, Lim KO, Mueller BA, Philippus A, et al. Identifying body awareness-related brain network changes after Spring Forest Qigong™ practice or P.Volve low-intensity exercise in adults with chronic low back pain: a feasibility phase I randomized clinical trial. medRxiv. 2023. 10.1101/2023.02.11.23285808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeste DV, Palmer BW, Appelbaum PS, Golshan S, Glorioso D, Dunn LB, et al. A new brief instrument for assessing decisional capacity for clinical research. Arch Gen Psychiatry. 2007;64:966–74. [DOI] [PubMed] [Google Scholar]
- 21.Van de Winckel A, Kozlowski AJ, Johnston MV, Weaver J, Grampurohit N, Terhorst L, et al. Reporting Guideline for RULER: Rasch Reporting Guideline for Rehabilitation Research: explanation and elaboration. Arch Phys Med Rehabil. 2022;103:1487–98. [DOI] [PubMed] [Google Scholar]
- 22.Mallinson T, Kozlowski AJ, Johnston MV, Weaver J, Terhorst L, Grampurohit N, et al. Rasch Reporting Guideline for Rehabilitation Research (RULER): the RULER Statement. Arch Phys Med Rehabil. 2022;103:1477–86. [DOI] [PubMed] [Google Scholar]
- 23.Wright BD. Misunderstanding the Rasch model. J Educ Meas. 2005;14:219–25. [Google Scholar]
- 24.Andrich D, Marais I. A course in Rasch Measurement Theory: measuring in the Educational, Social and Health Sciences. Springer; 2019.
- 25.McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4:293–307. [DOI] [PubMed] [Google Scholar]
- 26.Linacre JM. Reliability and separation of measures. https://www.winsteps.com/winman/reliability.htm. Accessed 3 Dec 2023.
- 27.Hagell P. Testing rating scale unidimensionality using the principal component analysis (PCA)/t-test protocol with the Rasch model: the primacy of theory over statistics. Open J Stat. 2014;04:456–65. [Google Scholar]
- 28.Van Sonderen E, Sanderman R, Coyne JC. Ineffectiveness of reverse wording of questionnaire items: let’s learn from cows in the rain. PLoS ONE. 2013;8:e68967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suárez-Álvarez J, Pedrosa I, Lozano LM, García-Cueto E, Cuesta M, Muñiz J. Using reversed items in Likert scales: a questionable practice. Psicothema. 2018;30:149–58. [DOI] [PubMed] [Google Scholar]
- 30.Saravanan A, Bajaj P, Matthews HL, Tell D, Starkweather A, Janusek L. Fatigue and depressive mood in chronic low back pain. Pain Manag Nurs. 2024;25:225–30. [DOI] [PubMed] [Google Scholar]
- 31.Minnesota P. 2023. https://worldpopulationreview.com/states/minnesota-population. Accessed 28 Feb 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available in the Data Repository for the University of Minnesota (DRUM), 10.13020/qst8-dc65.