Abstract
Introduction:
Down syndrome, or trisomy 21, is the most diagnosed chromosomal abnormality and is associated with multiple orthopedic concerns, including scoliosis. We sought to examine the surgical treatment of scoliosis associated with Down syndrome with an emphasis on specific complications in this population.
Methods:
A retrospective review of 13 patients with Down syndrome who underwent surgical intervention for spinal deformity between 2000 and 2018 were identified. Postoperative complications were classified using the modified Clavien-Dindo-Sink system. Perioperative and final follow-up radiographic data were analyzed.
Results:
The mean age at surgery was 14.2 years (11–19) with a mean follow-up of 3.6 years (0.4–6.2) at the time of data collection. Seven (54%) patients had postoperative complications, all related to wound healing. Three patients (23%) had major complications (Clavien-Dindo-Sink grade ≥3). These included one deep surgical site infection, one hematoma, and one seroma, all requiring surgical drainage. Four additional patients (31%) had minor complications (Clavien-Dindo-Sink grade ≤2).
Discussion:
Surgical intervention for scoliosis in patients with Down syndrome is associated with high complication rates despite the use of more modern surgical techniques and implant types. Complications in this cohort primarily involved wound healing, whereas previous studies described high rates of postoperative implant failure, pseudoarthrosis, and significant curve progression, which were not experienced by the patients in this study. Although the etiology of wound-related complications is unknown, awareness of this risk may help surgeons optimize surgical technique, postoperative monitoring, and preoperative counseling of families.
Level of Evidence:
IV—single-institution retrospective case series.
Keywords: Scoliosis, trisomy 21, Down syndrome, syndromic scoliosis, spinal fusion, spinal deformity, spinal surgery, complications
Introduction
Down syndrome (DS), or Trisomy 21, is one of the most common chromosomal abnormalities, occurring in approximately 1 in 700–800 live births.1,2 Meiotic disjunction resulting in three copies of chromosome 21 accounts for 96% of DS cases 2 and the risk increases with maternal age. 3 DS has been associated with a variety of orthopedic conditions, including scoliosis as well as occipito-atlanto-axial instability, 4 hip dysplasia, slipped capital femoral epiphysis, patellar instability, pes planus, and hallux valgus. 5
The incidence of scoliosis associated with DS is not well established. Milbrandt et al. reported an overall incidence of 9% over 50 years at one institution. 6 Two previously published studies note complication rates as high as 57%–71% in a total of 14 patients with DS undergoing spinal fusion for scoliosis.6,7 These complications included implant failure, infection, junctional kyphosis, pseudarthrosis, and wound healing problems. Both reported a similar postoperative acute infection rate of 14%. These studies described spinal fusions performed between 1954 and 2004 utilizing older implant types and instrumentation constructs. A recently published multicenter study reviewing procedures performed between 2009 and 2019 found that patients with DS continue to have high rates of postoperative complications following posterior spinal fusion for scoliosis despite the use of more modern implant types and surgical techniques. 8 The overall complication rate in this cohort was 52%, with a 17% reoperation rate. The complications reported in this study were similar to those reported in the two previously published studies.
In this study, we sought to describe the postoperative complications associated with the surgical treatment of scoliosis in patients with DS using the modified Clavien-Dindo-Sink (CDS) classification system. We hypothesized that there would be a lower overall complication rate after spine fusion for scoliosis in patients with DS with the use of more modern implants and surgical techniques.
Methods
Institutional review board approval was obtained a waiver of consent was applied. Patients with a diagnosis of DS or mosaic trisomy 21 who underwent surgical treatment for spinal deformity at a single institution between January 1, 2000 and December 31, 2018, were included. All surgeries were performed by one of eight board-certified and fellowship-trained pediatric orthopedic surgeons. Patients without a diagnosis of DS or those undergoing revision surgery were excluded. No patients in this cohort underwent growth-friendly constructs.
A retrospective chart review was used to gather demographic, radiographic, and surgical data. Body mass index (BMI) z-scores were calculated using age, sex, height, and weight at the time of surgery. Radiographic parameters including major coronal and sagittal curve magnitudes were collected preoperatively, immediately postop, and at final follow-up.
Patients’ complications were categorized and compared using the modified CDS classification system. The modified CDS is reliable and valid for classifying surgical complications in pediatric orthopedic patients. 9 The system consists of seven grades (I, II, IIIa, IIIb, Iva, IVb, and V) and ranks complications from minor to major events. During the study time period, standardized surgical protocols for patients with neuromuscular and syndromic scoliosis evolved to include the use of incisional negative pressure dressings to decrease the incidence of wound complications and infection. Reoperation was defined as any unplanned repeat surgical interventions required after the initial procedure. Surgical site Infection was defined as any patient with a positive wound culture.
Statistical analysis was performed using SPSS software (Version 24; IBM; Armonk, NY) 10 to assess mean, range, and standard deviation for demographic, radiographic, and surgical data. We analyzed the major curve Cobb and overall kyphosis preoperatively, immediately postop, and at final follow-up.
Results
In all, 13 patients (seven females and six males) with a diagnosis of DS (12 trisomy 21, 1 with mosaic trisomy 21) underwent surgical treatment for spinal deformity (Tables 1 and 2). All patients had genetic diagnoses established prenatally or in early childhood. Six patients (46%) had a history of bracing. The mean age at surgery was 14.2 years ± 2.6 (range: 11.8–19.3). Seven patients (54%) had a history of congenital cardiac anomalies; four patients (31%) had a history of cardiac surgery. 61.5% of patients had double major curves while 38.5% of patients had thoracic curve types. The mean age-adjusted BMI z-score was 0.68 ± 0.92 (−0.56–2.05). One patient had cervical vertebral anomalies with equivocal instability and the remaining 12 patients had no cervical spine pathology.
Table 1.
Patient demographics.
| Variable types | N | Variables | Total (percent total) |
|---|---|---|---|
| Sex | 13 | Male | 6 (46) |
| Female | 7 (54) | ||
| History of cardiac defects | 13 | Yes | 7 (54) |
| No | 6 (46) | ||
| History of cardiac surgery | 13 | Yes | 4 (31) |
| No | 9 (69) | ||
| Cervical vertebral anomaly | 13 | Yes | 1 (8) |
| No | 12 (92) | ||
| History of bracing | 13 | Yes | 6 (46) |
| No | 7 (54) | ||
| Curve type | 13 | Thoracic | 5 (38.5) |
| Double major | 8 (61.5) | ||
| Initial surgery type | 13 | Definitive posterior fusion | 13 (100) |
| Construct used | 13 | Pedicle screws | 9 (69) |
| Hybrid | 4 (30.8) |
Table 2.
Index procedural information.
| Variables | N | Mean ± Std (Min–Max) |
|---|---|---|
| Age at surgery (years) | 13 | 14.2 ± 2.6 (11.8–19.3) |
| BMI | 13 | 22.4 ± 4.5 (16.9–33.1) |
| BMI z-score | 13 | 0.68 ± 0.92 (−0.56–2.05) |
| Total levels | 13 | 12.8 ± 1.54 (10–15) |
| Implant density | 13 | 1.35 ± 0.25 (1.00–1.82) |
| Total blood loss (mL) | 13 | 590 ± 203 (100–1000) |
| Surgical time (min) | 13 | 299 ± 64 (210–435) |
| Length of stay (days) | 13 | 5 ± 3.2 (3–15) |
| Follow-up (years) | 13 | 3.6 ± 2.0 (0.42–6.2) |
| Major Cobb at Preop | 13 | 67° ± 10° (57°–92°) |
| Major Cobb at immediate postoperative | 13 | 27° ± 10° (13°–46°) |
| Major Cobb at FFU | 13 | 31° ± 11° (18°–49°) |
| % Correction of the major curve at immediate postoperative | 13 | 60% ± 12% (37%–80%) |
| % Correction of major curve at FFU | 13 | 56% ± 13% (33%–71%) |
| T5–T12 Kyphosis at Preop | 13 | 20° ± 8.7° (0°–37°) |
| T5–T12 Kyphosis at immediate postoperative | 11 | 22° ± 6.5° (11°–31°) |
| T5–T12 Kyphosis at FFU | 13 | 21° ± 6.7° (12°–38°) |
| T2–T12 Kyphosis at Preop | 13 | 28° ± 11° (0°–45°) |
| T2–T12 Kyphosis at immediate postoperative | 13 | 31.2° ± 8.3° (14°–41°) |
| T2–T12 Kyphosis at FFU | 13 | 27° ± 10° (16°–46°) |
BMI: body mass index; FFU: final follow-up; Std: standard deviation.
All patients underwent posterior spinal fusion with segmental pedicle-screw constructs (Figures 1 and 2). The average number of levels fused was 12.8 ± 1.5 (range: 10–15). Four patients (30.8%) were instrumented with a hybrid construct using a combination of segmental pedicle screws and >2 hooks/wires. Ponte osteotomies were performed on one patient for correction of focal kyphosis in the thoracolumbar spine. All 13 patients were fused into the lumbar spine. Donated allograft and local autograft were used in 12 (92%) cases with 1 case using iliac crest autograft. The mean implant density was 1.35 ± 0.25 (1.00–1.82). Intraoperative neuromonitoring was performed on all patients; none had intraoperative neuromonitoring changes or postoperative neurologic complications. Absorbable suture material was used for deep dermal closure in all cases. Nonabsorbable suture material was used for skin closure in four (30.7%) cases and absorbable material in nine (69.2%) cases (Table 3). As a result of institutional practices, four patients in this cohort received a negative pressure dressing while the rest did not. For the overall cohort, the mean length of hospital stay after the initial procedure was 5 ± 3.2 days (range: 3–15). Preoperatively, the average major curve Cobb was 67° ± 10° (range: 57°–92°), 27° ± 10° (range: 13°–46°) immediately postop, and 31° ± 11° (range: 18°–49°) at final follow-up. Preoperatively, the T5–T12 Kyphosis was 20° ± 8.7° (range: 0°–37°), 22° ± 6.5° (range: 11°–31°) immediately postop, and 21° ± 6.7° (12°–38°) at final follow-up. Of the 10 patients with minimum 2-year follow-up, the mean amount of follow-up was 4.52 ± 1.2 years (2.3–6.2 years, the average major cob at final follow-up was 27.9° ± 10.6° (range: 18°–49° with a mean correction of 59.9% ± 10.4% (range: 47%–71%), and the T5–T12 Kyphosis was 21° ± 7.5° (range: 13°–38°). Lastly, of the 10 patients with minimum 2-year follow-up, 3 (30%) had curve progression greater than 5°.
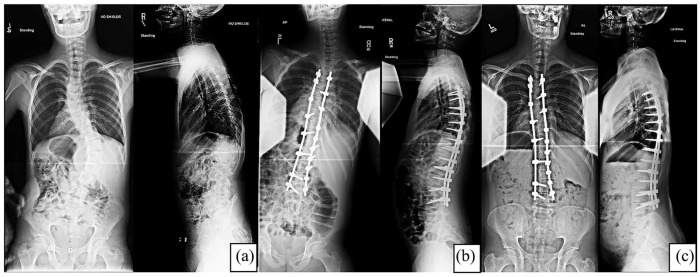
Figure 1.
Standing radiographs of a 12-year-old with DS and scoliosis were obtained preoperatively, immediately postoperative, and 5 years after the index procedure. Bracing was attempted but was not tolerated. He had no apparent back pain before surgery. He had a routine post-op course and was able to perform all his normal activities at subsequent follow-up visits. (a) Preoperative posteroanterior (PA)/lateral radiographs. (b) Immediate postoperative PA/lateral radiographs. (c) Final follow-up PA/lateral radiographs demonstrate maintained hardware fixation.
Figure 2.
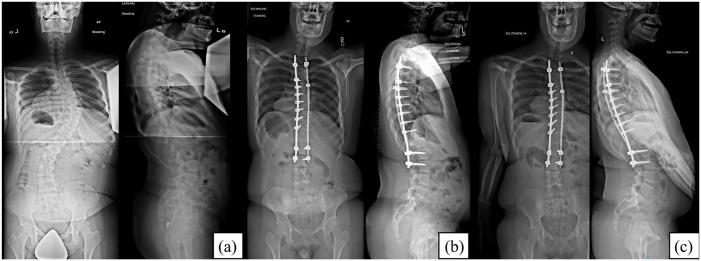
Standing radiographs of a 19-year-old with DS and scoliosis were obtained preoperatively, immediately postoperative, and at the most recent follow-up of 3 years after the index procedure. He had no clinical symptoms before surgery. He had a routine post-op course and had no limitations to his activities at his most recent clinic visit. (a) Preoperative posteroanterior (PA)/lateral radiographs. (b) Immediate postoperative PA/lateral radiographs. (c) Most recent follow-up PA/lateral radiographs demonstrate maintained hardware fixation.
Table 3.
Cohort demographics and modified CDS classification for postoperative complications.
| Overall grade | Case | Suture type at skin closure | Postoperative complication | Age at treatment | Sex | BMI | Pre-op Cobb (°) | Final follow-up Cobb (°) | Surgical time (min) | EBL (mL) | Follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Grade 1 | 1 | Absorbable | Wound dehiscence; bilateral popliteal fossa wounds | 16 + 6 | F | 21.6 | 92 | 49 | 390 | 700 | 3.4 |
| 2 | Absorbable | Excess drainage | 11 + 10 | F | 27.9 | 60 | 40 | 327 | 450 | 0.4 | |
| Grade 2 | 3 | Absorbable | Excess drainage; pleural effusion and post-op fever treated with antibiotics | 13 + 4 | M | 25.8 | 61 | 23 | 270 | 500 | 3.8 |
| 4 | Absorbable | Purulent drainage treated with antibiotics | 16 + 4 | F | 21.0 | 57 | 26 | 225 | 100 | 1.0 | |
| Grade 3 | 5 | Absorbable | Culture-negative hematoma undergoing I&D | 12 + 1 | F | 21.4 | 64 | 32 | 435 | 850 | 5.3 |
| 6 | Absorbable | Deep SSI undergoing I&D ×2 with fluid culture positive for Enterobacter | 12 + 2 | F | 21.8 | 59 | 19 | 210 | 550 | 5.2 | |
| 7 | Nonabsorbable | Stitch abscess, scar widening, and culture-negative seroma undergoing I&D | 12 + 6 | M | 16.9 | 76 | 40 | 255 | 785 | 2.3 | |
| Grade 4 | No patient experienced a grade 4 postoperative complication | ||||||||||
| Grade 5 | No patient experienced a grade 5 postoperative complication | ||||||||||
| No postoperative complications | 8 | Absorbable | — | 12 + 6 | M | 17.1 | 58 | 21 | 333 | 500 | 5.3 |
| 9 | Absorbable | — | 13 + 4 | M | 18.1 | 66 | 20 | 312 | 1000 | 5.3 | |
| 10 | Nonabsorbable | — | 18 + 10 | F | 21.1 | 73 | 45 | 300 | 350 | 0.5 | |
| 11 | Nonabsorbable | — | 13 + 11 | F | 21.8 | 76 | 29 | 315 | 400 | 5.0 | |
| 12 | Nonabsorbable | — | 19 + 4 | M | 33.1 | 62 | 18 | 270 | 400 | 3.3 | |
| 13 | Absorbable | — | 12 + 8 | M | 23.3 | 63 | 33 | 243 | 600 | 6.2 | |
BMI: body mass index; EBL: estimated blood loss; I&D: incision & drainage; SSI: surgical site infection.
Seven of 13 patients (54%) had postoperative complications, with four (31%) having minor complications (CDS 1 or 2) and three patients (23%) having major complications (CDS ≥3) (Table 3). Minor complications included one patient with prolonged serosanguinous wound drainage for 3 months postoperatively. One patient had a superficial wound dehiscence that was observed and healed 2 weeks postoperatively. A third patient had a postoperative fever and was found to have a pleural effusion on a chest X-ray that resolved with antibiotics. Concurrently, the patient was noted to have wound drainage which was monitored and resolved without treatment. The last patient was noted to have wound drainage postoperatively and was treated with oral antibiotics.
Major complications included one patient with wound drainage on a post-op day (POD) 5 who underwent I&D on POD 9 due to continued drainage. Cultures were performed during the I&D; however, these were negative. A second patient developed a stitch abscess, scar widening, and seroma at the distal incision several weeks following discharge. Scar revision with I&D of the seroma was performed on POD 23. Cultures were performed during the I&D but were found to be negative. A third patient underwent I&D for persistent fevers on POD 8 and was noted to have a closed dermal layer with underlying fascial dehiscence. Deep wound cultures grew Enterobacter and the patient underwent a second I&D on POD 11 with wound closure. The patient was treated postoperatively with 4 days of IV antibiotics, followed by 3 months of oral antibiotics with resolution of the infection.
At the most recent follow-up, all patients had returned to their baseline level of ambulation. Two patients complained of occasional back pain that did not cause functional limitations.
Discussion
The purpose of this study was to review our institution’s experience with spinal fusion for scoliosis in DS patients with the hypothesis that the use of more modern surgical techniques and implants would lead to a lower overall complication rate. While the patients in this case series experienced a similar overall complication rate (54%) compared to previously published studies, they had a significantly lower rate of infection (8%). The predominant type of postoperative complication found in this cohort of patients was wound related—four patients with prolonged wound drainage after surgery, one wound dehiscence, and one seroma. Only one patient was noted to have a deep surgical site infection (SSI). This patient was also noted to have a dehiscence of their fascial closure.
There have been three previously published studies reviewing outcomes after spine fusion for DS patients with scoliosis with a total of 37 patients. These studies report complication rates between 52% and 71%, which is similar to the complication rate found in this cohort. The most common complications reported in these patients were pseudoarthrosis, infection, and implant failure. In the series reported here, the predominant type of complication encountered was wound related with no findings of pseudoarthrosis or implant failure. Patients with DS are known to have immunodeficiency, increased tissue elasticity, and differences in pain signaling, which may in part lead to an increased incidence of wound healing problems as noted in this series of patients.
Immunodeficiency and dysregulation are common manifestations of DS and cause increased susceptibility to infections. 11 Surgical implant systems have evolved over time with more recent implant systems offering lower profile implants, which may decrease local soft tissue irritation and infection. 12 We report an 8% infection rate in this study, which is slightly lower than that reported previously in patients with DS undergoing spinal fusion for scoliosis (14%).6,7 For further comparison with a similar procedure, rates of infection in patients with DS who underwent posterior fusion for atlantoaxial instability have been reported at 5%–20%.13,14 In the current series, a single patient with an SSI developed fevers and increased drainage on POD3. Shortly thereafter the wound began draining and an I&D performed on POD8 revealed fascial dehiscence.
Previous studies have shown a 52%–71% complication rate following spinal fusion for scoliosis in patients with DS6–8 which is comparable to the 54% complication rate found in this cohort. Interestingly, all seven patients with postoperative complications had issues related to wound healing. To our knowledge, significant wound healing problems after orthopedic surgery have not been previously reported in this patient population; however, other surgical specialties have reported similar postoperative wound complications. 15 We posit that this is related to structural differences in collagen and altered tissue elasticity seen in this population although further study is needed.16,17 Differences in pain perception in DS patients compared to the general population, which may permit early and excessive wound stress or trauma, have also been proposed as an explanation for wound healing complications. McGuire et al. 18 in 2015 reported a delay in the conduction of acute pain signals and increased inter-hemispheric transmission time in the DS population, suggesting an altered ability to respond to acute noxious stimuli. 19 Despite delayed somatosensory processing, tissue damage in response to noxious stimuli is not delayed and may even be enhanced.18,20 These differences in acute pain signals may increase a DS patient’s ability to tolerate certain activities or movements in the immediate postoperative period that could lead to self-inflicted tissue damage and subsequent wound healing problems.
Surgical approach and instrumentation have evolved over time with the anticipation that more rigid spinal fixation and the use of all pedicle screw constructs may reduce certain complications such as implant dislodgement and pseudarthrosis. 12 Milbrandt et al. surmised in 2005 that the use of pedicle screws for distal fixation would markedly enhance fixation; this was a concern from their study population in which six of seven procedures used hooks for distal fixation and four of seven patients developed implant failure, three of which also had pseudarthrosis. Recently, Fraser et al. 8 reported returns to the OR due to instrumentation complications despite the use of more modern instrumentation and all with the majority of pedicle screw constructs. In our current study, all patients received pedicle screw constructs in the lumbar spine and no patients developed implant failure postoperatively. Although not eliminated, we see a decrease in complications when utilizing modern instrumentation methods. This highlights the benefit of advancements in surgical implants and techniques to decrease postoperative complications after spine fusion, especially in this patient population.
The limitations of this study include the relatively small number of patients. This study, however, significantly contributes to the number of patients with DS surgically treated for scoliosis at a single center compared to what is previously reported in the literature. Larger numbers may allow for statistically significant associations to be made between specific complications and varying aspects of treatment, to identify risk factors for the increased complication rates experienced in patients with DS. Three of the cases included in the current study lacked a 2-year follow-up, which may fail to capture late complications, such as hardware failure and pseudarthrosis. Ideally, these patients would be excluded; however, considering the small sample size, the authors concluded that it was important to retain the three patients who did not meet a 2-year follow-up to highlight the number of postoperative wound complications, which is a novel finding in this population. All reports of wound complications happened within 90 days of the surgery and each patient included had a minimum of 6 months of follow-up. This study is the largest single-center review of patients with DS surgically treated for scoliosis which may highlight a more uniform way of treatment for the population compared to previous multicenter reviews.
While this study demonstrates more wound complications than previously reported, it is difficult to determine the etiology of these problems or to identify measures that can be undertaken to prevent these problems. To date, there are no evidence-based strategies known to reduce complications related to wound healing in this patient population. Postoperatively at our institution, we began utilizing incisional negative pressure dressings in 2017 for neuromuscular and syndromic patients. It is the author’s impression that the use of negative pressure dressings postoperatively could be beneficial in lowering infection rates. Based on this, the authors recommend that surgeons treating scoliosis in patients with DS be aware of the high wound complication rate and take measures to avoid them such as meticulous wound closure, the use of incisional negative pressure dressings, fastidious post-op wound care, and education of families about activity levels post-op to try and prevent such complications.
In conclusion, the overall complication rate after spinal fusion for scoliosis in patients with DS remains high despite improvements in surgical techniques and spine implant systems. Previously reported high rates of implant failure, pseudoarthrosis and curve progression did not occur in our patient population. The main complications observed in this cohort were related to wound healing with a slightly lower infection rate than previously reported. Although the specific etiology of wound-healing complications is unknown, it may be associated with differences in tissue elasticity and acute pain perception, which is often seen in the DS population. Therefore, awareness of this significant risk may help surgeons optimize surgical technique, influence postoperative care and activity restrictions, and provide appropriate preoperative counseling to families.
Supplemental Material
Supplemental material, sj-pdf-1-cho-10.1177_18632521241277031 for Acute postoperative complications after spine deformity correction in patients with Down syndrome by Claire W Bonnyman, Lydia N Klinkerman, Brandon A Ramo and Megan E Johnson in Journal of Children’s Orthopaedics
Footnotes
Author contributions: The authors listed meet each of the four authorship criteria as stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Compliance with ethical standards: Institutional review board approval was obtained from a waiver of consent was applied for the study.
Anonymized/Removed from Manuscript: University of Texas Southwestern Medical Center STU: 092016-091.
ORCID iD: Megan E Johnson  https://orcid.org/0000-0002-5968-9469
https://orcid.org/0000-0002-5968-9469
Supplemental material: Supplemental material for this article is available online.
References
- 1. Parker SE, Mai CT, Canfield MA, et al. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol 2010; 88(12): 1008–1016. [DOI] [PubMed] [Google Scholar]
- 2. Bull MJ. Down syndrome. N Engl J Med 2020; 382(24): 2344–2352. [DOI] [PubMed] [Google Scholar]
- 3. Hassold T, Chiu D. Maternal age-specific rates of numerical chromosome abnormalities with special reference to trisomy. Hum Genet 1985; 70(1): 11–17. [DOI] [PubMed] [Google Scholar]
- 4. Levy BJ, Schulz JF, Fornari ED, et al. Complications associated with surgical repair of syndromic scoliosis. Scoliosis 2015; 10: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Diamond LS, Lynne D, Sigman B. Orthopedic disorders in patients with Down’s syndrome. Orthop Clin North Am 1981; 12(1): 57–71. [PubMed] [Google Scholar]
- 6. Milbrandt TA, Johnston CE, 2nd. Down syndrome and scoliosis: a review of a 50-year experience at one institution. Spine (Phila Pa 1976) 2005; 30(18): 2051–2055. [DOI] [PubMed] [Google Scholar]
- 7. Lerman JA, Emans JB, Hall JE, et al. Spinal arthrodesis for scoliosis in Down syndrome. J Pediatr Orthop 2003; 23(2): 159–161. [PubMed] [Google Scholar]
- 8. Fraser HG, Krakow A, Lin A, et al. Outcomes of posterior spinal fusion in pediatric patients with down syndrome. J Bone Joint Surg Am 2022; 104(23): 2068–2073. [DOI] [PubMed] [Google Scholar]
- 9. Dodwell ER, Pathy R, Widmann RF, et al. Reliability of the modified Clavien-Dindo-Sink complication classification system in pediatric orthopaedic surgery. JB JS Open Access 2018; 3(4): e0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. [Google Scholar]
- 11. Verstegen RHJ, Kusters MAA. Inborn errors of adaptive immunity in down syndrome. J Clin Immunol 2020; 40(6): 791–806. [DOI] [PubMed] [Google Scholar]
- 12. Mignemi M, Tran D, Ramo B, et al. Repeat surgical interventions following “Definitive” instrumentation and fusion for idiopathic scoliosis: 25-year update. Spine Deform 2018; 6(4): 409–416. [DOI] [PubMed] [Google Scholar]
- 13. Takeoka Y, Kakutani K, Miyamoto H, et al. Complications of posterior fusion for atlantoaxial instability in children with down syndrome. Neurospine 2021; 18(4): 778–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hofler RC, Pecoraro N, Jones GA. Outcomes of surgical correction of atlantoaxial instability in patients with down syndrome: systematic review and meta-analysis. World Neurosurg 2019; 126: e125–e135. [DOI] [PubMed] [Google Scholar]
- 15. Cairo SB, Zeinali LI, Berkelhamer SK, et al. Down syndrome and postoperative complications in children undergoing intestinal operations. J Pediatr Surg 2019; 54(9): 1832–1837. [DOI] [PubMed] [Google Scholar]
- 16. Marentette JO, Anderson CC, Prutton KM, et al. Trisomy 21 impairs PGE2 production in dermal fibroblasts. Prostaglandins Other Lipid Mediat 2021; 153: 106524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Iwamoto T, Yamada A, Yuasa K, et al. Influences of interferon-gamma on cell proliferation and interleukin-6 production in Down syndrome derived fibroblasts. Arch Oral Biol 2009; 54(10): 963–969. [DOI] [PubMed] [Google Scholar]
- 18. McGuire BE, Defrin R. Pain perception in people with Down syndrome: a synthesis of clinical and experimental research. Front Behav Neurosci 2015; 9: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Heath M, Grierson L, Binsted G, et al. Interhemispheric transmission time in persons with Down syndrome. J Intellect Disabil Res 2007; 51(Pt 12): 972–981. [DOI] [PubMed] [Google Scholar]
- 20. Kotulska K, Larysz-Brysz M, LePecheur M, et al. APP/SOD1 overexpressing mice present reduced neuropathic pain sensitivity. Brain Res Bull 2011; 85(6): 321–328. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cho-10.1177_18632521241277031 for Acute postoperative complications after spine deformity correction in patients with Down syndrome by Claire W Bonnyman, Lydia N Klinkerman, Brandon A Ramo and Megan E Johnson in Journal of Children’s Orthopaedics