Abstract
Background
We considered the suggestion that mental health is the product of two intersecting continua: psychological distress and mental wellbeing.
Objectives
To understand prevalences of low mental wellbeing, depression and anxiety, and examine associations between them and with sociodemographic variables.
Methods
In a cross-sectional survey in informal settlements, 4906 women aged 18–49 years answered questions on mental wellbeing (Short Warwick-Edinburgh Mental Wellbeing Scale: SWEMWBS) and symptoms of depression (Patient Health Questionnaire: PHQ-9) and anxiety (Generalised Anxiety Disorder: GAD-7). We used regression models to examine associations of lower mental wellbeing with symptoms suggesting moderate-to-severe depression and anxiety, and with sociodemographic characteristics.
Results
About 15% of women reported symptoms of low wellbeing, 9% symptoms of moderate-to-severe depression, and 6% symptoms of moderate-to-severe anxiety. Women with low wellbeing did not necessarily report symptoms suggesting anxiety or depression, and women with anxiety or depression did not necessarily report low wellbeing. In adjusted models, poorer and less educated women were more likely to report low wellbeing. Symptoms of anxiety or depression were more likely to be reported by widowed, separated, or divorced women, women who were in paid employment, and women who used drugs or alcohol themselves or whose partners did. Women with low wellbeing had at least double the odds of reporting symptoms of moderate-to-severe depression or anxiety than women who reported greater wellbeing.
Conclusion
The findings support the idea of two continua of mental health. How individual women cope with mental illness and nevertheless enjoy a state of wellbeing deserves more study.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12905-024-03389-1.
Keywords: Mental Health, Psychological well-being, Depression, Anxiety, Poverty areas, India.
| Text box 1. Summary box | |
|---|---|
| What is already known on this topic? | |
| • It has been suggested that mental health has two dimensions: psychological distress (corresponding with mental illness) and mental wellbeing (corresponding with feeling good and functioning well). There is some supportive evidence for this idea, although little from the global South. | |
| What this study adds | |
| • The study is the first to use question scales to ask women in informal settlements in India about their mental wellbeing, depression and anxiety. Almost a quarter of women reported symptoms suggesting low mental wellbeing, depression or anxiety. Substantial numbers reported low mental wellbeing in the absence of psychological distress, and some felt good and functioned well in the presence of psychological distress. | |
| How this study might affect research, practice or policy | |
| • Understanding of the dimensions of mental health in informal settlements in which people are exposed to multiple stressors is limited. The idea of two continua of mental health merits study, particularly in terms of its implications for services. The finding that some women are able to maintain a sense of mental wellbeing despite psychological distress has implications for research on coping abilities. |
Background
Recent estimates put the global burden of mental illness at around 420 million disability-adjusted life years, accounting for one in every six years lived with disability and an economic cost of USD 5 trillion [1, 2]. Before the Covid-19 pandemic began, an estimated 970 million people were living with a mental disorder. More than half were women (508 million), around one-third had an anxiety disorder (301 million) [2], and 82% of them lived in a low- or middle-income country [2]. Stark though these figures are, they focus on mental illness rather than mental health. The World Health Organization (WHO) defines mental health as “a state of well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community” [2]. This is in keeping with the idea of health as more than the absence of disease, a holistic framing that predates its articulation by philosophers such as Aristotle and position statements such as the Alma Ata Declaration of 1978 [3].
Although a focus on mental illness characterizes much of the discussion among policymakers, clinicians and researchers, it has been suggested that mental health has two dimensions: psychological distress and mental wellbeing. The idea is implicit in the WHO characterization of mental health as a continuum state with experiences ranging from an optimal state of wellbeing to debilitating states of great suffering and emotional pain [2, 3]. Linked most with the work of Keyes, the two continua model suggests that mental health is located in a field defined by intersecting axes: a continuum of mental wellbeing and a continuum of mental illness [4, 5].
Mental wellbeing is a combination of optimal functioning and subjective emotional experiences [3, 6, 7]. Its components include individual potential, meaningfulness, good relationships, sense of purpose and the value of one’s life [6, 8]. Wellbeing has itself been theoretically divided into feeling good and functioning well [9]: hedonic wellbeing (pleasure, happiness, life satisfaction) [10], and eudemonic wellbeing (good relationships, fulfilment, self-realisation) [4, 6, 9, 11]. A person can be thought of as flourishing when they both feel good and function well. Wellbeing is linked with achievement in personal, interpersonal and professional spheres and is important for creating and maintaining healthy societies [12]. It is linked with better physical health and longevity [13], work performance, life satisfaction, and economic and social development [14–17]. People with greater wellbeing tend to be more productive at work, learn better and be creative and more engaged in prosocial behaviour and favourable interpersonal connection [18]. People with lower wellbeing use mental health services more frequently [19], are more likely to report symptoms of depression [20, 21], suffer depression of greater severity, and are more likely to self-harm [22, 23]. These associations may be stronger than those described for social determinants of mental health such as socioeconomic status, human capital, working conditions, or family background [24].
In India, estimates of the prevalence of mental illness range from 2 to 57% in the general population [25–27] and 8–61% in urban informal settlements [28–30]. Analogous estimates are not available for wellbeing, although subjective wellbeing on a five-question scale was associated with neighbourhood cohesion in two informal settlements in Delhi [31]. Despite progress in physical healthcare infrastructure, the Indian mental healthcare system faces numerous challenges: shortages of clinicians at all levels, fragmented services, insufficient financial support and resources, social stigma and discrimination, perceived coercion, and limited awareness [3, 26, 32–35]. Mental health receives 0.16% of the national healthcare budget, itself 3.2% of public sector expenditure. India’s 2017 Mental Healthcare Act (MHCA, 2017) represents a significant advance in establishing a legal framework for mental health and the decriminalization of self-harming behaviors, including suicide. It provides direction for services for people living with mental illness and aims to protect, promote and fulfil their rights to convenient, quality, affordable and accessible mental healthcare [36]. It does not explicitly address wellbeing.
Objective
The non-government organization SNEHA (Society for Nutrition, Education and Health Action) has been implementing a programme on prevention of violence against women in Mumbai’s informal settlements for the past two decades. This group of socioeconomically and environmentally disadvantaged women in urban India are under considerable pressure and their concerns may be rather different from those of the Western, Educated, Industrialized, Rich, and Democratic (WEIRD) participants who characterize the literature [37]. Central to our activities is the need to integrate support for women’s mental health in the response to violence, and this has led us to consider the use of assessment tools for common mental disorders such as depression and anxiety.
The importance of social determinants as causes and triggers for both violence and common mental disorders is manifest daily in the accounts of our clients and participants. Structural conditions such as income and socioeconomic position, education, employment, housing and neighbourhood conditions, food security, childhood adversity, discrimination, and access to affordable healthcare all have the potential to affect mental health outcomes, contribute to mental health disparities, and promote positive mental health [35, 38, 39]. The intersection of poverty, inequalities, distress and struggle—of the psychological with the sociostructural—supports a composite view of mental health in terms of psychological distress and mental wellbeing. It also speaks to contemporary discussions in global mental health [40], and particularly the issue of intersection between multiple dimensions of experience and need [41, 42]. For this reason, we included measures of both psychological distress and mental wellbeing in our assessment tools. Our objectives were (1) to compare the findings of scales for symptoms of depression and anxiety with a scale for mental wellbeing, and (2) to examine associations with sociodemographic characteristics.
Methods
Setting, design, and participants
Residents of informal settlements face more challenges to their mental health than non-slum and rural residents [43–46]. High population density, poor housing and substandard living conditions exacerbate risks of injury and infectious diseases and probably increase the risk of common mental disorders [43–45, 47]. The study used data collected before the SNEHA TARA (Taking Action Reaching All) cluster randomized controlled trial in Mumbai, India [48]. In a cross-sectional systematic random sample survey, we interviewed around 100 women in each of 50 clusters of approximately 500 households. Between 5th December 2017 and March 2019, 5277 households were approached for the survey. A sample of 4900 from an approximate population of 125,000 would have a precision of approximately 1%, and would have 80% power to detect a difference of 6% in prevalence estimates for domestic violence of 10–20%. The survey respondents were women aged 18 to 49 years.
Data collection
After a three-month training program, a group of 16 women interviewers mapped study areas and residences and developed a list of homes with potential respondents. Starting at a random point in each cluster, interviewers approached one woman aged 18–49 years in every second home on the list. Each cluster yielded data from 100 women. Interviews were prearranged to ensure confidentiality and privacy. Following the provision of information regarding the aim of the interview and their right to withdraw, participants provided signed consent. Interviewers used Android tablets to input data into a database within the CommCare platform (www.dimagi.com/commcare/). Details are available elsewhere [49]. Data were collected in accordance with the General Data Protection Regulation 2018 and stored in a MySQL database overseen by SNEHA information managers.
We had a duty of care if respondents disclosed violence or mental health concerns. We established a network with local police stations and social services in advance of the survey to facilitate referral and service linkages for women who needed them. Interviewers followed support protocols which included safety assessment, crisis intervention, home visits, counselling, liaison with healthcare, police, and legal services, and developing safety and follow-up plans for the survivor and her family. Three field supervisors supported interviewers by providing a direct connection to counselling services by phone at any time. Investigators also received automated notification of the need for referral if a respondent’s score on mental health screens was suggestive of concern. Participants were given a visiting card that was easy to hide and contained addresses and phone numbers of essential services, along with a toll-free helpline number. SNEHA counselors and community networks ensured follow-up [48].
Outcome variables: wellbeing and symptoms of anxiety and depression
To examine associations with variables such as spousal characteristics, we limited the dataset to ever-married women. We examined self-reported mental wellbeing and mental illness. The Short Warwick-Edinburgh Mental Wellbeing Scale-7 (SWEMWBS) assessed participants’ mental wellbeing in the past two weeks. The SWEMWBS is psychometrically robust, is suited for population use with individuals aged 13 years or older, and has been used to evaluate wellbeing interventions in demographic research worldwide, including the general population, older people, stigmatised minorities, people living with schizophrenia, and service users with mental health concerns [50–52]. The Hindi version has been validated [53–55]. The Patient Health Questionnaire (PHQ-9) was administered to screen for depression [56] and the Generalized Anxiety Disorder scale (GAD-7) for anxiety in the last two weeks [57]. Both have been validated in India and, in both cases, a score of > = 10 suggests clinically significant problems requiring further examination [58].
Exposure variables: demographic and socioeconomic characteristics
We included marital status, age, education, employment, substance use, faith, caste and socioeconomic position as potential risk factors for low wellbeing, depression and anxiety based on prior research in India [59–64]. Socioeconomic position was derived from standardized weights for the first component of a principal components analysis of household assets [65, 66].
Statistical analysis
We checked the reliability of the SWEMWBS, PHQ-9, and GAD-7 with Cronbach’s alpha. We used a score of > = 10 on the PHQ-9 and GAD-7 to indicate moderate-to-severe symptoms of depression or anxiety [58]. With a mean SWEMWBS score of 24.07 and a standard deviation of 5.63, 15% of the sample would be predicted to have a score of > = 29.70 (= 24.07 + 5.63) or < = 18.44 (= 24.07–5.63). We established a cut-off score of < = 18.44 as an indication of low mental wellbeing [67]. We tabulated frequencies and proportions of women who screened positive for low mental wellbeing, and positive for moderate-to severe depression on the PHQ-9 and moderate-to-severe anxiety on the GAD-7. We developed unadjusted and adjusted logistic regression models for low wellbeing, moderate-to-severe depressive symptoms, and moderate-to-severe anxiety symptoms to investigate their association with the following exposure variables: marital status, age, education, faith, caste, socioeconomic asset quintile, employment of women and their husbands, and alcohol or drug use by women or their husbands, suggested as potential variables affecting wellbeing and mental health [68]. We examined the association between low wellbeing as an independent variable and moderate-to-severe depression and anxiety as dependent variables in unadjusted and adjusted logistic regression models. Models were adjusted for background characteristics as described above. We also computed unadjusted and adjusted linear regression models for wellbeing, depression, and anxiety scores. We used survey commands in STATA 15.0 (StataCorp LLC) for all analyses.
Results
Participant characteristics
Table 1 summarises the characteristics of 4906 women aged 18 to 49 years who had been married at least once and were interviewed between December 2017 and March 2019. 42% had secondary or higher education, while only a quarter were engaged in paid work, mostly in the informal sector or as domestic workers, and earned a mean USD 163 a year. Most households were of substantial construction, but did not have their own toilets.
Table 1.
Characteristics of 4906 ever-married women respondents in informal settlements in Mumbai, India
| Characteristic | n | (%) |
|---|---|---|
| Marital status | ||
| Currently married | 4694 | (96.0) |
| Widowed, separated or divorced | 212 | (4.0) |
| Age in completed years | ||
| 18–19 y | 57 | (1.2) |
| 20–29 y | 1911 | (39.0) |
| 30–39 y | 2031 | (41.4) |
| 40–49 y | 907 | (18.5) |
| Education in completed years | ||
| No formal education | 938 | (19.0) |
| Primary 1–5 y | 846 | (17.0) |
| Middle 6–8 y | 1099 | (22.0) |
| Secondary 9–10 y | 1105 | (23.0) |
| Higher secondary 11–12 y | 533 | (11.0) |
| Higher 12 y or more | 385 | (8.0) |
| Respondent employed | 1182 | (24.0) |
| Respondent monthly income, INR | ||
| < 1000 | 233 | (20.0) |
| 1000–2999 | 303 | (27.0) |
| 3000–5999 | 279 | (25.0) |
| 6000+ | 322 | (28.0) |
| Respondent uses alcohol or drugs | 612 | (12.0) |
| Husband age in completed years | ||
| 18–19 y | 14 | (< 1) |
| 20–29 y | 917 | (19.0) |
| 30–39 y | 2102 | (44.0) |
| 40–49 y | 1370 | (29.0) |
| 50 + y | 391 | (8.0) |
| Husband employed | 4686 | (98.0) |
| Husband monthly income, INR | ||
| < 10,000 | 1095 | (23.0) |
| 10,000–11,999 | 997 | (21.0) |
| 12,000–14,999 | 652 | (14.0) |
| 15,000+ | 1942 | (41.0) |
| Husband uses alcohol or drugs | 2100 | (44.0) |
| Housing fabric | ||
| Insubstantial | 336 | (7.0) |
| Mixed | 2052 | (42.0) |
| Robust | 2518 | (51.0) |
| Toilet facility type | ||
| Private | 836 | (17.0) |
| Public | 4368 | (82.0) |
| No facility | 2 | (< 1) |
| Faith | ||
| Hindu | 1826 | (37.0) |
| Muslim | 2882 | (59.0) |
| Other | 198 | (4.0) |
| Caste | ||
| General | 2854 | (58.0) |
| Other Backward Caste | 1180 | (24.0) |
| Scheduled Tribe or Caste | 872 | (18.0) |
| Socioeconomic quintile | ||
| 1 poorest | 969 | (21.0) |
| 2 | 936 | (20.0) |
| 3 | 934 | (20.0) |
| 4 | 933 | (20.0) |
| 5 least poor | 935 | (20.0) |
Characteristics of 4906 ever-married women respondents in informal settlements in reported wellbeing and symptoms of anxiety and depression
Cronbach’s alpha indicated acceptable internal consistency for the SWEMWBS (α 0.737), PHQ-9 (α 0.860), and GAD-7 (α 0.843). SWEMWBS scores correlated negatively with PHQ-9 (r -0.206; p < 0.001) and GAD-7 scores (r -0.199; <0.001). There was a positive correlation between PHQ-9 and GAD-7 scores (r 0.789; p < 0.001). On self-report, 15% of women had symptoms suggesting low wellbeing, 9% symptoms suggestive of moderate-to-severe depression, and 6% symptoms suggestive of moderate-to-severe anxiety. Almost 23% reported either low wellbeing or symptoms suggesting moderate-to-severe depression or anxiety.
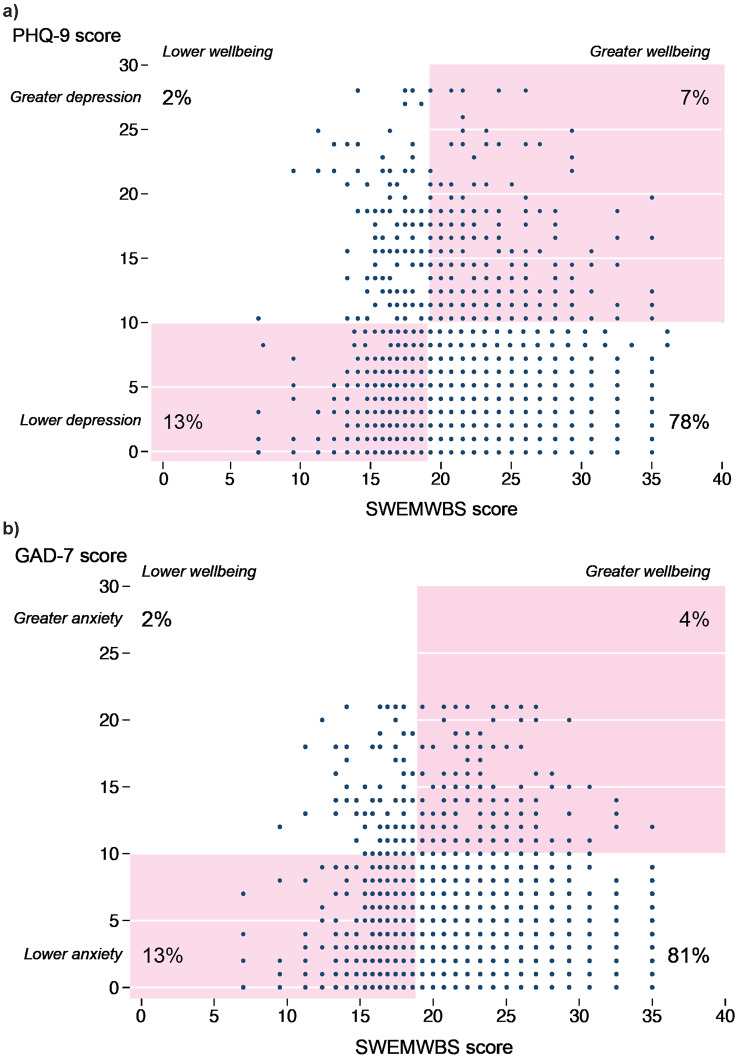
Figure 1 plots PHQ-9 scores and GAD-7 scores against SWEMWBS scores. The plots are divided into quadrants by lines corresponding with cut-offs suggesting clinical concern. The largest numbers of individuals fell into the quadrant corresponding to acceptable wellbeing and no concern about anxiety or depression. Although 2% of women reported symptoms suggesting depression and 2% anxiety in the presence of low wellbeing, there were two mismatched quadrants. 13% reported symptoms of low wellbeing without depression or anxiety, 7% reported symptoms of depression, and 4% reported symptoms suggestive of anxiety, without obviously low wellbeing.
Fig. 1.
Self-reported symptoms suggesting common mental disorder, by symptoms suggesting lower or greater wellbeing on Short Warwick-Edinburgh Mental Wellbeing Scale (SWEMWBS): (a) Patient Health Questionnaire 9 (PHQ-9); (b) Generalised Anxiety Disorder 7 (GAD-7)
Table 2 summarises the prevalence of low wellbeing and moderate-to-severe depression and anxiety, categorised by women’s background characteristics.
Table 2.
Screens for low wellbeing and symptoms of moderate-to-severe depression and anxiety, by characteristics of 4906 ever-married women in urban informal settlements, Mumbai, India
| Low wellbeing on SWEMWBS | Moderate-to-severe depression symptoms on PHQ-9 | Moderate-to-severe anxiety symptoms on GAD-7 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | No | Yes | No | Yes | No | Yes | ||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Marital status | ||||||||||||
| Currently married | 3999 | (85.2) | 695 | (14.8) | 371 | (92.1) | 4694 | (7.9) | 4443 | (94.7) | 251 | (5.4) |
| Widowed, separated, divorced | 175 | (82.6) | 37 | (17.5) | 140 | (66.0) | 72 | (34.0) | 164 | (77.4) | 48 | (22.6) |
| Age (years) | ||||||||||||
| 18–19 | 48 | (84.2) | 9 | (15.8) | 52 | (91.2) | 5 | (8.8) | 53 | (93.0) | 4 | (7.0) |
| 20–29 | 1605 | (84.0) | 306 | (16.0) | 1757 | (91.9) | 154 | (8.1) | 1813 | (94.9) | 98 | (5.1) |
| 30–39 | 1732 | (85.3) | 299 | (14.7) | 1863 | (91.7) | 168 | (8.3) | 1919 | (94.5) | 112 | (5.5) |
| 40–49 | 789 | (87.0) | 118 | (13.0) | 791 | (87.2) | 116 | (12.8) | 822 | (90.6) | 85 | (9.4) |
| Schooling | ||||||||||||
| No schooling | 763 | (81.3) | 175 | (18.7) | 109 | (88.4) | 938 | (11.6) | 865 | (92.2) | 73 | (7.8) |
| Primary, class 1–5 | 687 | (81.2) | 159 | (18.8) | 760 | (89.8) | 86 | (10.2) | 789 | (93.3) | 57 | (6.7) |
| Middle, class 6–8 | 933 | (84.9) | 166 | (15.1) | 981 | (89.3) | 118 | (10.7) | 1015 | (92.4) | 84 | (7.6) |
| Secondary, class 9–10 | 970 | (87.8) | 135 | (12.2) | 1027 | (92.9) | 78 | (7.1) | 1055 | (95.5) | 50 | (4.5) |
| Higher secondary, class 11–12 | 475 | (89.1) | 58 | (10.9) | 499 | (93.6) | 34 | (6.4) | 510 | (95.7) | 23 | (4.3) |
| Higher education | 346 | (89.9) | 39 | (10.1) | 367 | (95.3) | 18 | (4.7) | 373 | (96.9) | 12 | (3.1) |
| Employment of respondent | ||||||||||||
| No remunerated employment | 3153 | (84.7) | 571 | (15.3) | 3445 | (92.5) | 279 | (7.5) | 3536 | (95.0) | 188 | (5.1) |
| In remunerated employment | 1021 | (86.4) | 161 | (13.6) | 1018 | (86.1) | 164 | (13.9) | 1071 | (90.6) | 111 | (9.4) |
| Employment of husband | ||||||||||||
| No remunerated employment | 79 | (79.8) | 20 | (20.2) | 74 | (74.8) | 25 | (25.3) | 85 | (85.9) | 14 | (14.1) |
| In remunerated employment | 3993 | (85.2) | 693 | (14.8) | 4305 | (91.9) | 381 | (8.1) | 4426 | (94.5) | 260 | (5.6) |
| Alcohol or drug use by respondent | ||||||||||||
| No | 3647 | (84.9) | 647 | (15.1) | 3950 | (92.0) | 344 | (8.0) | 4064 | (94.6) | 230 | (5.4) |
| Yes | 527 | (86.1) | 85 | (13.9) | 513 | (83.8) | 99 | (16.2) | 543 | (88.7) | 69 | (11.3) |
| Alcohol or drug use by husband | ||||||||||||
| No | 2333 | (86.8) | 355 | (13.2) | 2548 | (94.8) | 140 | (5.2) | 2592 | (96.4) | 96 | (3.6) |
| Yes | 1742 | (83.0) | 358 | (17.1) | 1832 | (87.2) | 268 | (12.8) | 1919 | (91.4) | 181 | (8.6) |
| Caste | ||||||||||||
| General caste | 2441 | (85.5) | 413 | (14.5) | 2587 | (90.6) | 267 | (9.4) | 2676 | (93.8) | 178 | (6.2) |
| Other backward caste | 1026 | (87.0) | 154 | (13.1) | 1087 | (92.1) | 93 | (7.9) | 1115 | (94.5) | 65 | (5.5) |
| Scheduled tribe or caste | 707 | (81.1) | 165 | (18.9) | 789 | (90.5) | 83 | (9.5) | 816 | (93.6) | 56 | (6.4) |
| Faith | ||||||||||||
| Muslim | 1544 | (84.6) | 282 | (15.4) | 1631 | (89.3) | 195 | (10.7) | 1687 | (92.4) | 139 | (7.6) |
| Hindu | 2465 | (85.5) | 417 | (14.5) | 2659 | (92.3) | 223 | (7.7) | 2742 | (95.1) | 140 | (4.9) |
| Other | 165 | (83.3) | 33 | (16.7) | 173 | (87.4) | 25 | (12.6) | 178 | (89.9) | 20 | (10.1) |
| Household socioeconomic quintile | ||||||||||||
| 1 Poorest | 755 | (77.9) | 214 | (22.1) | 854 | (88.1) | 115 | (11.9) | 895 | (92.4) | 74 | (7.6) |
| 2 | 777 | (83.0) | 159 | (17.0) | 854 | (91.2) | 82 | (8.8) | 878 | (93.8) | 58 | (6.2) |
| 3 | 808 | (86.5) | 126 | (13.5) | 843 | (90.3) | 91 | (9.7) | 879 | (94.1) | 55 | (5.9) |
| 4 | 832 | (89.2) | 101 | (10.8) | 862 | (92.4) | 71 | (7.6) | 879 | (94.2) | 54 | (5.8) |
| 5 Least poor | 833 | (89.1) | 102 | (10.9) | 869 | (92.9) | 66 | (7.1) | 890 | (95.2) | 45 | (4.8) |
| All (N) | 4906 | (100.0) | 4906 | (100.0) | 4906 | (100.0) | ||||||
Footnote
SWEMWBS: Short Warwick-Edinburgh Mental Wellbeing Scale-7. PHQ-9: Patient Health Questionnaire-9. GAD-7: Generalised Anxiety Disorder-7
Association between low wellbeing and symptoms of moderate-to-severe depression and anxiety
Table 3 shows outputs of logistic regression models for low wellbeing and reported symptoms of moderate-to-severe depression and moderate-to-severe anxiety, unadjusted and adjusted with socioeconomic and sociodemographic covariates. In the adjusted model, poorer and less educated women were more likely to report low wellbeing. Symptoms of anxiety or depression were more likely to be reported by widowed, separated or divorced women, women who were in paid employment and women who used drugs or alcohol themselves or whose husbands did. The findings were consistent with linear regression models using SWEMWBS, PHQ-9 and GAD-7 scores (Supplementary Table 1).
Table 3.
Univariable and multivariable logistic regression models for low wellbeing and symptoms of moderate-to-severe depression and anxiety, by characteristics of 4906 ever-married women in urban informal settlements, Mumbai, India
| Characteristic | Low mental wellbeing on SWEMWBS | Moderate-to-severe depression symptoms on PHQ-9 | Moderate-to-severe anxiety symptoms on GAD-7 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | [95% CI] | aOR | [95% CI] | OR | [95% CI] | aOR | [95% CI] | OR | [95% CI] | aOR | [95% CI] | |
| Marital status | ||||||||||||
| Currently married | 1 | 1 | 1 | 1 | 1 | |||||||
| Widowed, separated, divorced | 1.2 | [0.7, 2.0] | 1.3 | [0.6, 2.6] | 6.0 | [4.2, 8.6] | 4.6 | [2.6, 8.0] | 5.2 | [3.9, 7.0] | 3.4 | [1.8, 6.4] |
| Age (years) | ||||||||||||
| 18–19 | 1 | 1 | 1 | 1 | 1 | |||||||
| 20–29 | 1.0 | [0.4, 2.9] | 1.0 | [0.4, 3.0] | 0.9 | [0.4, 2.2] | 1.1 | [0.4, 3.1] | 0.7 | [0.3, 1.9] | 0.9 | [0.3, 2.7] |
| 30–39 | 0.9 | [0.3, 2.8] | 0.9 | [0.3, 2.8] | 0.9 | [0.4, 2.3] | 0.9 | [0.3, 2.8] | 0.8 | [0.3, 2.1] | 0.9 | [0.3, 2.7] |
| 40–49 | 0.8 | [0.3, 2.4] | 0.7 | [0.2, 2.3] | 1.5 | [0.6, 3.9] | 1.4 | [0.5, 4.1] | 1.4 | [0.5, 3.7] | 1.5 | [0.5, 4.4] |
| Schooling | ||||||||||||
| No schooling | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Primary class 1–5 | 1.0 | [0.8, 1.3] | 1.1 | [0.8, 1.4] | 0.9 | [0.6, 1.2] | 0.9 | [0.6, 1.2] | 0.9 | [0.6, 1.3] | 0.8 | [0.5, 1.2] |
| Middle 6–8 | 0.8 | [0.6, 1.0] | 0.8 | [0.6, 1.0] | 0.9 | [0.7, 1.2] | 0.9 | [0.7, 1.3] | 1.0 | [0.7, 1.4] | 1.0 | [0.7, 1.4] |
| High 9–10 | 0.6 | [0.5, 0.8] | 0.7 | [0.5, 0.8] | 0.6 | [0.4, 0.8] | 0.7 | [0.5, 1.0] | 0.6 | [0.4, 0.7] | 0.7 | [0.5, 0.9] |
| Higher 11–12 | 0.5 | [0.4, 0.8] | 0.5 | [0.4, 0.8] | 0.5 | [0.3, 0.8] | 0.8 | [0.5, 1.3] | 0.5 | [0.3, 0.9] | 0.7 | [0.4, 1.3] |
| Above 12 | 0.5 | [0.3, 0.7] | 0.5 | [0.4, 0.8] | 0.4 | [0.2, 0.6] | 0.6 | [0.3, 1.0] | 0.4 | [0.2, 0.7] | 0.6 | [0.3, 1.2] |
| Employment of respondent | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 0.9 | [0.7, 1.1] | 0.9 | [0.7, 1.1] | 2.0 | [1.6, 2.5] | 1.5 | [1.2, 2.0] | 2.0 | [1.5, 2.5] | 1.5 | [1.1, 2.1] |
| Employment of husband | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 0.7 | [0.4, 1.2] | 0.8 | [0.4, 1.5] | 0.3 | [0.2, 0.4] | 0.7 | [0.4, 1.3] | 0.4 | [0.2, 0.6] | 1.0 | [0.5, 2.0] |
| Alcohol or drug use by respondent | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 0.9 | [0.7, 1.2] | 0.7 | [0.5, 1.0] | 2.2 | [1.7, 2.9] | 1.4 | [1.0, 1.9] | 2.3 | [1.6, 3.1] | 1.4 | [1.1, 1.9] |
| Alcohol or drug use by husband | ||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.4 | [1.2, 1.6] | 1.3 | [1.1, 1.5] | 2.7 | [2.2, 3.3] | 2.2 | [1.8, 2.8] | 2.6 | [1.8, 3.6] | 2.1 | [1.4, 3.0] |
| Caste | ||||||||||||
| General caste | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| OBC (Other backward caste) | 0.9 | [0.7, 1.1] | 0.9 | [0.7, 1.1] | 0.8 | [0.7, 1.1] | 0.9 | [0.7, 1.1] | 0.9 | [0.7, 1.2] | 0.9 | [0.7, 1.3] |
| ST/SC (Scheduled tribe or caste) | 1.4 | [1.1, 1.8] | 1.5 | [1.1, 1.9] | 1.0 | [0.8, 1.4] | 0.9 | [0.7, 1.3] | 1.0 | [0.7, 1.5] | 1.0 | [0.7, 1.4] |
| Faith | ||||||||||||
| Muslim | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Hindu | 0.9 | [0.7, 1.2] | 1.0 | [0.8, 1.3] | 0.7 | [0.6, 0.9] | 0.8 | [0.6, 1.0] | 0.6 | [0.5, 0.9] | 0.6 | [0.4, 0.9] |
| Other | 1.1 | [0.6, 1.8] | 1.1 | [0.6, 2.0] | 1.2 | [0.8, 1.9] | 1.1 | [0.6, 2.1] | 1.4 | [0.8, 2.2] | 1.3 | [0.7, 2.2] |
| Household socioeconomic quintile | ||||||||||||
| 1 Poorest | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 2 | 0.7 | [0.6, 0.9] | 0.7 | [0.6, 0.9] | 0.7 | [0.5, 1.0] | 0.7 | [0.5, 1.0] | 0.8 | [0.6, 1.1] | 0.8 | [0.5, 1.2] |
| 3 | 0.6 | [0.4, 0.7] | 0.6 | [0.4, 0.8] | 0.8 | [0.6, 1.1] | 0.8 | [0.6, 1.1] | 0.8 | [0.5, 1.2] | 0.8 | [0.5, 1.2] |
| 4 | 0.4 | [0.3, 0.6] | 0.5 | [0.3, 0.6] | 0.6 | [0.5, 0.8] | 0.6 | [0.4, 0.8] | 0.7 | [0.5, 1.1] | 0.7 | [0.4, 1.0] |
| 5 Least poor | 0.4 | [0.3, 0.6] | 0.5 | [0.4, 0.7] | 0.6 | [0.4, 0.8] | 0.7 | [0.4, 1.0] | 0.6 | [0.4, 0.9] | 0.7 | [0.4, 1.1] |
| All (N) | 4906 | (100.0) | 4906 | (100.0) | 4906 | (100.0) | ||||||
Footnote
SWEMWBS: Short Warwick-Edinburgh Mental Wellbeing Scale-7. PHQ-9: Patient Health Questionnaire-9. GAD-7: Generalised Anxiety Disorder-7. CI: confidence interval. OR: odds ratio. aOR: odds ratio adjusted with covariates for marital status, age, schooling, employment of respondent and husband, alcohol or drug use by respondent of husband, caste, faith and socioeconomic score
The findings from both unadjusted and adjusted logistic regression models for symptoms of moderate-to-severe depression or anxiety are summarized in Supplementary Table 2. Adjusting for background characteristics, the model suggested that women with low wellbeing had 2-fold and 2.2-fold greater odds of reporting symptoms of moderate-to-severe depression or moderate-to-severe anxiety than women with greater wellbeing.
Discussion
In a survey of the mental health of almost 5000 women in urban informal settlements in Mumbai, 9% reported PHQ-9 scores suggesting depression, 6% GAD-7 scores suggesting anxiety and 15% SWEMWBS scores suggesting low wellbeing. The three sets of scores were mutually correlated. The number of women who reported low wellbeing exceeded the number who reported symptoms of anxiety or depression.
Prevalences of symptoms of moderate-to-severe depression and anxiety were lower in our study than reported in others in informal settlements in Mumbai or elsewhere in India. However, they were higher than the national average and higher than those reported by residents of non-slum areas [25, 26, 28–30, 69, 70]. Our findings may reflect population reality. It is conceivable that lower prevalence of anxiety and depression might reflect a greater sense of self-determination combined with improvements in environment, livelihoods and lifestyle in urban informal settlements. Migration, particularly from rural to urban centres, has been described as affecting the self-esteem of migrants positively as a result of economic opportunities and better livelihoods. One study found that rural migrants settled in urban regions have better later-life mental health [71]. Alternatively, the differences could be the result of methodological variation between studies in terms of sampling, scales or cut-offs for mental health conditions. It is possible that the stigma that accompanies mental health concerns led to underreporting of symptoms, although we presume that this would be a feature of all studies and our team of interviewers were well trained and supervised. With respect to mental wellbeing, the mean score (24.07) was actually higher than the mean score for women (23.59) in a national study in England [72].
Symptoms of anxiety, depression and low wellbeing were more likely to be reported by older women. Although we found a positive association between age and mental health concerns, our sample only included women under the age of 50. This means that we were unable to extend the analysis into older age, which is often characterized by a gradual decline in physical and mental health and an increased risk of disease [73]. It would be interesting to examine interaction between age and exposure to violence. Symptoms of anxiety or depression were more likely to be reported by widowed, separated or divorced women, women who were in remunerated occupations, and women who used drugs or alcohol themselves or whose husbands did. These findings are in line with the literature [2, 28, 59, 61, 64, 74–77]. Low wellbeing was more likely to be reported by older, poorer, and less educated women. A study from China suggested that the reductive effect of mental wellbeing in terms of happiness increased with age [21].
Paradoxically, use of alcohol or drugs was associated with fewer reports of low wellbeing. It is possible that this reflects their positive effects on tension and self-efficacy, in at least the short term [78], but we are wary of commenting on a single finding. Our analysis did not include exposure to intimate partner violence as an exposure covariate. However, it is well documented that women survivors are more likely to access mental healthcare services, and women with mental health conditions are more likely to experience intimate partner violence victimization [79].
Framing mental health along two continua corresponding with wellbeing and mental illness, we found some correspondence between low reported wellbeing and symptoms of anxiety and depression, and likewise between satisfactory wellbeing and absence of anxiety and depression. A range of studies have found similar associations [21, 80–83]. Our findings are in line with the WHO position on mental health [2], and with the idea of mental health as (at least) two continua. Perhaps the most interesting finding is the disjunction between the mental wellbeing and mental illness constructs. Women with low wellbeing did not necessarily report symptoms suggesting anxiety or depression, and women with anxiety or depression did not necessarily have low wellbeing. It seems feasible that individuals with mental health conditions can still enjoy mental wellbeing (or resist lower wellbeing) by having a support system, resilience, and style of coping [2, 84]. We have no studies in India with which to compare these findings because studies of anxiety and depression have not examined wellbeing, and vice versa, but the findings are in line with other studies suggesting that the possibility of mental wellbeing persists even when experiencing mental health conditions [85].
Our findings raise a number of questions for further exploration. Is it true that women are able to maintain a sense of wellbeing in the presence of potentially debilitating symptoms of anxiety or depression? If so, what is it that helps women exposed to multiple social determinants cope with mental illness to a degree to which their wellbeing is maintained? Will the findings differ for women in less challenging environments who are not exposed to poverty, insecurity of tenure and environmental degradation? Is it something to do with social and family support or cultural attitudes to the kinds of questions used in assessment scales? Would the findings be different for men? For example, in a study that administered the Positive and Negative Affect Schedule (PANAS)—Revised [86, 87] and the Satisfaction with Life Scale (SWLS) [88] to around 1000 adults in urban Bengaluru, subjective wellbeing was generally greater in men than in women [89].
Limitations
The usual inferential limitations apply to our cross-sectional study. External validity is limited by the focus on a sample of ever-married women aged 18–49 years and their residence in urban informal settlements in India. The findings were based on self-reported answers to question scales which, though validated, may not be measuring quite what they seek to. We have no clinical diagnosis for constellations of symptoms suggestive of anxiety and depression. There is some concern that diagnostic categories and classification of mental disorders need revisiting in the context of global mental health [39]. Screening tools such as the PHQ-9 do not address cultural concepts of distress [90, 91]: ways in which cultural groups experience, understand, and communicate suffering, behavioural problems, or troubling thoughts and emotions [92]. Cultural concepts of distress now feature in the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 and could be included in approaches to screening [90].
Clinical implications
Our study is the first in India to examine mental health along two continua and provides some support for the idea of doing so. It contributes to a growing body of work on wellbeing in South Asia and raises questions about the maintenance of wellbeing in the face of mental illness. That individuals experiencing mental illness can enjoy a state of wellbeing, lead meaningful lives and contribute to society is important and in agreement with India’s Mental Healthcare Act [36]. Conversely, that individuals with low wellbeing may not receive appropriate social and psychological support in the absence of diagnosable clinical conditions is of concern.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our gratitude to the women and community guardians who volunteered to participate in the study. We are grateful to SNEHA colleagues Miheeka Vast and Manju Singh, Apoorva Gupta, Unnati Machchhar and Shilpa Adelkar, Bhaskar Kakad and Gauri Savkur, Archana Bagra for financial and human resource management, and Vanessa D’Souza and Shanti Pantvaidya for their leadership.
Abbreviations
- CI
Confidence Interval
- DSM-5
The Diagnostic and Statistical Manual of Mental Disorders-5
- GAD-7
Generalised Anxiety Disorder-7
- IEC
Institutional Ethics Committee
- MHCA, 2017
Mental Healthcare Act, 2017
- OR/aOR
Odds Ratio/ Adjusted Odds Ratio
- PANAS-R
Positive and Negative Affect Schedule—Revised
- PHQ-9
Patient Health Questionnaire-9
- PUKAR
Partners for Urban Knowledge, Action, and Research
- SNEHA
Society for Nutrition, Education and Health Action
- SWEMWBS
Short Warwick-Edinburgh Mental Wellbeing Scale
- SWLS
The Satisfaction with Life Scale
- USD
United States dollar
- TARA
Taking Action Reaching All
- WEIRD
Western, Educated, Industrialized, Rich, and Democratic
- WHO
The World Health Organization
Author contributions
ND and DO acquired funding and ND was responsible for managing the project. SK, ND, and DO conceived and designed the work. SK designed the data collection materials and managed the acquisition of data with guidance from ND and DO. SK conceptualised the manuscript concept, analysed and interpreted the data and wrote the first draft. DO contributed to subsequent drafts and conceptualization of the analysis. All authors revised the draft critically for intellectual content and approved the final version. The authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of it are appropriately investigated and resolved.
Funding
This work was funded by the Wellcome Trust [206417/Z/17/Z]. For the purpose of Open Access, the authors have applied a CC BY public copyright licence to any author accepted manuscript version arising from this submission. The funder had no role in study design, data collection and analysis, publishing decisions, or manuscript preparation.
Open access funding provided by SRM Institute of Science and Technology for SRMIST – Medical & Health Sciences.
Data availability
Data can be accessed with permission at https://osf.io/szmup DOI 10.17605/OSF.IO/U3RGS.
Declarations
Ethical approval and consent to participate
The survey followed WHO guidelines for researching domestic and sexual violence against women [93]. Interviewers were trained in ethical procedures and WHO ethical and safety guidelines were followed [94]. Informed consent was obtained from participants. Participants received information about counselling and crisis support services available locally and referrals for support were made based on a response protocol. Ethical approval was granted by the University College London Research Ethics Committee (3546/003, 27/09/2017) and by PUKAR (Partners for Urban Knowledge, Action, and Research) Institutional Ethics Committee (25/12/2017).
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine 2022, 54. [DOI] [PMC free article] [PubMed]
- 2.WHO: World mental health report: transforming mental health for all. Geneva: World Health Organization. 2022. In.; 2022.
- 3.Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–98. [DOI] [PubMed] [Google Scholar]
- 4.Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539–48. [DOI] [PubMed] [Google Scholar]
- 5.Headey B, Kelley J, Wearing A. Dimensions of mental health: Life satisfaction, positive affect, anxiety and depression. Soc Indic Res. 1993;29:63–82. [Google Scholar]
- 6.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Personal Soc Psychol. 1989;57(6):1069. [Google Scholar]
- 7.Henderson L, Knight T. Integrating the hedonic and eudaimonic perspectives to more comprehensively understand wellbeing and pathways to wellbeing. 2012.
- 8.Stone AA, Mackie CE. Subjective well-being: Measuring happiness, suffering, and other dimensions of experience. National Academies; 2013. [PubMed]
- 9.Ryan RM, Deci EL. On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52(1):141–66. [DOI] [PubMed] [Google Scholar]
- 10.Diener E. Subjective well-being. Psychol Bull. 1984;95(3):542–75. [PubMed] [Google Scholar]
- 11.Keyes CLM. Social well-being. Social Psychol Q 1998:121–40.
- 12.Durand M. The OECD better life initiative: How’s life? And the measurement of well-being. Rev Income Wealth. 2015;61(1):4–17. [Google Scholar]
- 13.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richards M, Huppert FA. Do positive children become positive adults? Evidence from a longitudinal birth cohort study. J Posit Psychol. 2011;6(1):75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diener E, Pressman SD, Hunter J, Delgadillo-Chase D. If, why, and when subjective well-being influences health, and future needed research. Appl Psychol Health Well Being. 2017;9(2):133–67. [DOI] [PubMed] [Google Scholar]
- 16.Knapp M, McDaid D, Parsonage M. Mental health promotion and mental illness prevention: The economic case. 2011.
- 17.Deaton A. Income, health, and well-being around the world: Evidence from the Gallup world poll. J Econ Perspect. 2008;22(2):53–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diener E. New findings and future directions for subjective well-being research. Am Psychol. 2012;67(8):590–7. [DOI] [PubMed] [Google Scholar]
- 19.Michalski CA, Diemert LM, Hurst M, Goel V, Rosella LC. Is life satisfaction associated with future mental health service use? An observational population-based cohort study. BMJ open. 2022;12(4):e050057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cummins RA. Subjective well-being, homeostatically protected mood and depression: A synthesis. Explor Happiness: Present Future Perspect 2013:77–95.
- 21.Li C, Xia Y, Zhang Y. Relationship between subjective well-being and depressive disorders: Novel findings of cohort variations and demographic heterogeneities. Front Psychol. 2023;13:1022643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant JB, Batterham PJ, McCallum SM, Werner-Seidler A, Calear AL. Specific anxiety and depression symptoms are risk factors for the onset of suicidal ideation and suicide attempts in youth. J Affect Disord. 2023;327:299–305. [DOI] [PubMed] [Google Scholar]
- 23.Liu H, Yu Z, Ye B, Yang Q. Grit and life satisfaction among college students during the recurrent outbreak of COVID-19 in China: The mediating role of depression and the moderating role of stressful life events. Front Public Health. 2022;10:895510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lombardo P, Jones W, Wang L, Shen X, Goldner EM. The fundamental association between mental health and life satisfaction: Results from successive waves of a Canadian national survey. BMC Public Health. 2018;18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel V. The epidemiology of common mental disorders in South Asia. Nimhans J. 1999;17:307–28. [Google Scholar]
- 26.Gautham MS, Gururaj G, Varghese M, Benegal V, Rao GN, Kokane A, Chavan BS, Dalal PK, Ram D, Pathak K et al. The National Mental Health Survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry 2020, 66(4):361–372. [DOI] [PubMed]
- 27.Mathias K, Goicolea I, Kermode M, Singh L, Shidhaye R, Sebastian MS. Cross-sectional study of depression and help-seeking in Uttarakhand, North India. BMJ Open. 2015;5(11):e008992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panigrahi A, Panigrahi M, Padhy AP, Das SC. Common mental disorder and its socio-demographic correlates among married women residing in slum areas of Bhubaneswar, India. Women Health. 2017;57(5):521–33. [DOI] [PubMed] [Google Scholar]
- 29.Gawde N, Nasirabadi M, Shah N, Nagaonkar S. Psychiatric morbidity in an urban slum of Mumbai: Cross sectional study. Asian J Psychiatr. 2013;6(6):478–82. [DOI] [PubMed] [Google Scholar]
- 30.Silvanus V, Subramanian P. Epidemiological study of mental morbidity in an urban slum community in India for the development of a community mental health programme. Nepal Med Coll J. 2012;14(1):13–7. [PubMed] [Google Scholar]
- 31.Humble S, Sharma A, Rangaraju B, Dixon P, Pennington M. Associations between neighbourhood social cohesion and subjective well-being in two different informal settlement types in Delhi, India: A quantitative cross-sectional study. BMJ open. 2023;13(4):e067680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel V, Xiao S, Chen H, Hanna F, Jotheeswaran AT, Luo D, Parikh R, Sharma E, Usmani S, Yu Y, et al. The magnitude of and health system responses to the mental health treatment gap in adults in India and China. Lancet. 2016;388(10063):3074–84. [DOI] [PubMed] [Google Scholar]
- 33.Grover S, Avasthi A, Singh A, Dan A, Neogi R, Kaur D, Lakdawala B, Rozatkar AR, Nebhinani N, Patra S, et al. Stigma experienced by caregivers of patients with severe mental disorders: A nationwide multicentric study. Int J Soc Psychiatry. 2017;63(5):407–17. [DOI] [PubMed] [Google Scholar]
- 34.Raveesh B, Singh SP, Pathare S. Coercion and mental health services in the Indian subcontinent and the Middle East. Coercion Community Mental Health Care: Int Perspect 2016:79.
- 35.Patel V, Pereira J, Coutinho L, Fernandes R, Fernandes J, Mann A. Poverty, psychological disorder and disability in primary care attenders in Goa, India. Br J Psychiatry. 1998;172(6):533–6. [DOI] [PubMed] [Google Scholar]
- 36.Mental HA. 2017: Ministry of Law and Justice, New Delhi, India. In. Edited by India Go. India: The Controller of Publications, Delhi-110054, India; 2017.
- 37.Henrich J, Heine SJ, Norenzayan A. The weirdest people in the world? Behav Brain Sci. 2010;33(2–3):61–83. discussion 83–135. [DOI] [PubMed] [Google Scholar]
- 38.Kirkbride JB, Anglin DM, Colman I, Dykxhoorn J, Jones PB, Patalay P, Pitman A, Soneson E, Steare T, Wright T, et al. The social determinants of mental health and disorder: Evidence, prevention and recommendations. World Psychiatry. 2024;23(1):58–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacob KS, Patel V. Classification of mental disorders: A global mental health perspective. Lancet. 2014;383(9926):1433–5. [DOI] [PubMed] [Google Scholar]
- 40.Kirmayer LJ. Rethinking cultural competence. In., vol. 49: Sage Publications Sage UK: London, England; 2012: 149–164. [DOI] [PubMed]
- 41.Burgess RA. The struggle for the social: Rejecting the false separation of ‘social’ worlds in mental health spaces. Soc Psychiatry Psychiatr Epidemiol. 2024;59(3):409–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burgess RA, Jain S, Petersen I, Lund C. Social interventions: A new era for global mental health? Lancet Psychiatry. 2020;7(2):118–9. [DOI] [PubMed] [Google Scholar]
- 43.Jungari S, Chauhan BG, Bomble P, Pardhi A. Violence against women in urban slums of India: A review of two decades of research. Glob Public Health. 2022;17(1):115–33. [DOI] [PubMed] [Google Scholar]
- 44.Sambisa W, Angeles G, Lance PM, Naved RT, Thornton J. Prevalence and correlates of physical spousal violence against women in slum and nonslum areas of urban Bangladesh. J Interpers Violence. 2011;26(13):2592–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.IIPS. ICF: National family health survey (NFHS-4), 2015-16: India. Mumbai: IIPS. Mumbai: International Institute for Population Sciences 2017.
- 46.Atal S, Foster J. A woman’s life is tension: A gendered analysis of women’s distress in poor urban India. Transcult Psychiatry. 2021;58(3):404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.IIPS. National family health survey (NFHS-3), 2005-06: India. Volume 1. International Institute for Population Sciences; 2007.
- 48.Daruwalla N, Machchhar U, Pantvaidya S, D’Souza V, Gram L, Copas A, Osrin D. Community interventions to prevent violence against women and girls in informal settlements in Mumbai: The SNEHA-TARA pragmatic cluster randomised controlled trial. Trials. 2019;20(1):743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Daruwalla N, Kanougiya S, Gupta A, Gram L, Osrin D. Prevalence of domestic violence against women in informal settlements in Mumbai, India: A cross-sectional survey. BMJ Open. 2020;10(12):e042444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lyons A, Pitts M, Grierson J. Factors related to positive mental health in a stigmatized minority: An investigation of older gay men. J Aging Health. 2013;25(7):1159–81. [DOI] [PubMed] [Google Scholar]
- 51.Hughes K, Lowey H, Quigg Z, Bellis MA. Relationships between adverse childhood experiences and adult mental well-being: Results from an English national household survey. BMC Public Health. 2016;16:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vaingankar JA, Abdin E, Chong SA, Sambasivam R, Jeyagurunathan A, Seow E, Picco L, Pang S, Lim S, Subramaniam M. Psychometric properties of the positive mental health instrument among people with mental disorders: A cross-sectional study. Health Qual Life Outcomes. 2016;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vaingankar JA, Abdin E, Chong SA, Sambasivam R, Seow E, Jeyagurunathan A, Picco L, Stewart-Brown S, Subramaniam M. Psychometric properties of the short Warwick Edinburgh mental well-being scale (SWEMWBS) in service users with schizophrenia, depression and anxiety spectrum disorders. Health Qual Life Outcomes. 2017;15(1):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Brach M, Schmicker M, Bentlage E, et al. Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PLoS ONE. 2020;15(11):e0240204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stewart-Brown S. The Warwick-Edinburgh mental well-being scale (WEMWBS): Performance in different cultural and geographical groups. Mental well-being. edn.: Springer; 2013. pp. 133–50.
- 56.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 58.Kroenke KaS RL. Instruction manual: Instructions for patient health questionnaire (PHQ) and GAD-7 measures 2010.
- 59.Shidhaye R, Gangale S, Patel V. Prevalence and treatment coverage for depression: A population-based survey in Vidarbha, India. Soc Psychiatry Psychiatr Epidemiol. 2016;51(7):993–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban south Indian population–the Chennai urban rural epidemiology study (CURES-70). PLoS ONE. 2009;4(9):e7185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shidhaye R, Patel V. Association of socio-economic, gender and health factors with common mental disorders in women: A population-based study of 5703 married rural women in India. Int J Epidemiol. 2010;39(6):1510–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nandi DN, Banerjee G, Boral GC, Ganguli H, Ajmany S, Ghosh A, Sarkar S. Socio-economic status and prevalence of mental disorders in certain rural communities in India. Acta Psychiatr Scand. 1979;59(3):276–93. [DOI] [PubMed] [Google Scholar]
- 63.Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women. Population-based longitudinal study. Br J Psychiatry. 2006;189(6):547–55. [DOI] [PubMed] [Google Scholar]
- 64.Patel V, Kirkwood BR, Pednekar S, Pereira B, Barros P, Fernandes J, Datta J, Pai R, Weiss H, Mabey D. Gender disadvantage and reproductive health risk factors for common mental disorders in women: A community survey in India. Arch Gen Psychiatry. 2006;63(4):404–13. [DOI] [PubMed] [Google Scholar]
- 65.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography. 2001;38(1):115–32. [DOI] [PubMed] [Google Scholar]
- 66.Vyas S, Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plann. 2006;21(6):459–68. [DOI] [PubMed] [Google Scholar]
- 67.Shah N, Cader M, Andrews B, McCabe R, Stewart-Brown SL. Short Warwick-Edinburgh mental well-being scale (SWEMWBS): Performance in a clinical sample in relation to PHQ-9 and GAD-7. Health Qual Life Outcomes. 2021;19(1):260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392–407. [DOI] [PubMed] [Google Scholar]
- 69.Bentley AB. Beyond black and blue intimate partner violence as a form of family violence against women and common mental disorders in Mumbai informal settlements. UCL (University College London); 2020.
- 70.Subbaraman R, Nolan L, Shitole T, Sawant K, Shitole S, Sood K, Nanarkar M, Ghannam J, Betancourt TS, Bloom DE, et al. The psychological toll of slum living in Mumbai, India: A mixed methods study. Soc Sci Med. 2014;119:155–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang J, Nazroo J, Zhang N. Gender differences in rural-urban migration and its impact on depression in later life. Health Place. 2022;77:102890. [DOI] [PubMed] [Google Scholar]
- 72.Ng Fat L, Scholes S, Boniface S, Mindell J, Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short Warwick-Edinburgh mental well-being scale (SWEMWBS): Findings from the health survey for England. Qual Life Res. 2017;26(5):1129–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.WHO Aging and Health, Geneva WH, Organization. 2022. [https://www.who.int/news-room/fact-sheets/detail/ageing-and-health ].
- 74.Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Soc Sci Med. 2008;66(8):1733–49. [DOI] [PubMed] [Google Scholar]
- 75.Gururaj G, Varghese M, Benegal V, Rao GN, Pathak K, Singh L, Mehta R, Ram D, Shibukumar T, Kokane A. National mental health survey of India, 2015-16: prevalence, patterns and outcomes. Bengaluru: Natl Inst Mental Health Neuro Sci NIMHANS Publication 2016, 129.
- 76.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systematic review. BMJ. 2004;328(7443):794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bhattacharya A, Camacho D, Kimberly LL, Lukens EP. Women’s experiences and perceptions of depression in India: A metaethnography. Qual Health Res. 2019;29(1):80–95. [DOI] [PubMed] [Google Scholar]
- 78.Addicott MA, Marsh-Richard DM, Mathias CW, Dougherty DM. The biphasic effects of alcohol: Comparisons of subjective and objective measures of stimulation, sedation, and physical activity. Alcohol Clin Exp Res. 2007;31(11):1883–90. [DOI] [PubMed] [Google Scholar]
- 79.WHO: WHO multi-country study on women’s health and domestic violence against women: Summary report of initial results on prevalence, health outcomes and women’s responses. Geneva, World Health Organization. 2005. In.; 2005.
- 80.Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–27. [DOI] [PubMed] [Google Scholar]
- 81.Dyrbye LN, Harper W, Moutier C, Durning SJ, Power DV, Massie FS, Eacker A, Thomas MR, Satele D, Sloan JA, et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad Med. 2012;87(8):1024–31. [DOI] [PubMed] [Google Scholar]
- 82.Grant F, Guille C, Sen S. Well-being and the risk of depression under stress. PLoS One. 2013;8(7):e67395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Park SJ, Wasil AR, Gillespie S, Shingleton RM, Weisz JR, DeRubeis RJ. Depression and anxiety symptoms, subjective well-being, and happiness among Indian high school students. Indian J Psychiatry. 2023;65(6):655–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gautam S, Jain A, Chaudhary J, Gautam M, Gaur M, Grover S. Concept of mental health and mental well-being, it’s determinants and coping strategies. Indian J Psychiatry. 2024;66(Suppl 2):S231–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Weich S, Brugha T, King M, McManus S, Bebbington P, Jenkins R, Cooper C, McBride O, Stewart-Brown S. Mental well-being and mental illness: Findings from the adult psychiatric morbidity survey for England 2007. Br J Psychiatry. 2011;199(1):23–8. [DOI] [PubMed] [Google Scholar]
- 86.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–70. [DOI] [PubMed] [Google Scholar]
- 87.Feldman Barrett L, Russell JA. Independence and bipolarity in the structure of current affect. J Personal Soc Psychol. 1998;74(4):967. [Google Scholar]
- 88.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–5. [DOI] [PubMed] [Google Scholar]
- 89.Agrawal J, Murthy P, Philip M, Mehrotra S, Thennarasu K, John JP, Girish N, Thippeswamy V, Isaac M. Socio-demographic correlates of subjective well-being in urban India. Soc Indic Res. 2011;101:419–34. [Google Scholar]
- 90.Kohrt BA, Rasmussen A, Kaiser BN, Haroz EE, Maharjan SM, Mutamba BB, de Jong JT, Hinton DE. Cultural concepts of distress and psychiatric disorders: Literature review and research recommendations for global mental health epidemiology. Int J Epidemiol. 2014;43(2):365–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Caplan S, Alvidrez J, Paris M, Escobar JI, Dixon JK, Desai MM, Whittemore R, Scahill LD. Subjective versus objective: an exploratory analysis of latino primary care patients with self-perceived depression who do not fulfill primary care evaluation of mental disorders patient health questionnaire criteria for depression. Prim Care Companion CNS Disorders. 2010;12(5):26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.American Psychiatric Association D. Diagnostic and statistical manual of mental disorders: DSM-5. Volume 5. American psychiatric association Washington, DC; 2013.
- 93.Jewkes R, Dartnall E, Sikweyiya Y. Ethical and safety recommendations for research on perpetration of sexual violence. Pretoria: Sexual violence research initiative, medical research council; 2012. [Google Scholar]
- 94.WHO. Putting Women First: Ethical and safety recommendations for research on domestic violence against women. Department of gender and Women’s health, family and community health; 2001.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data can be accessed with permission at https://osf.io/szmup DOI 10.17605/OSF.IO/U3RGS.