Summary:
Vulvoperineal defects mount significant functional and aesthetic challenges for reconstructive surgeons, often followed by postoperative complications. Ideal flap creation and perforator selection is vital for proper healing, especially in those with comorbid health concerns. This report details an innovative approach to vulvar reconstruction using a freestyle perforator flap from the medial thigh, identified by color flow Doppler ultrasound (CDU). This noninvasive imaging technique made possible the exact identification and confirmation of a well-vascularized pedicle, giving rise to a tailored flap for enhanced postoperative recovery and healing. The flap was designed based on real-time vascular mapping by CDU and validated through indocyanine green angiography, ensuring robust perfusion. The case of this patient demonstrated the successful application of portable CDU to navigate the intricate vessel network of the medial thigh, which would not have been possible with traditional imaging modalities such as computed tomography alone. The lack of postoperative complications following reconstruction demonstrates how this strategy for addressing vulvoperineal defects is advantageous due to meticulous perforator selection based on the patient’s unique anatomy. CDU is therefore an important tool for achieving optimal outcomes related to form and function, all while reducing the risks of donor site morbidity.
Vulvoperineal defects may result from a broad spectrum of conditions, from congenital abnormalities and cancer to infection or trauma.1 Flap reconstruction is commonly advised for such defects, depending on profile of the affected area, defect size and shape, and the patient’s functional and aesthetic goals.2–5 These procedures pose unique reconstructive challenges due to notoriously high infection rates and poor healing given regional kinesthetic complexity.2,4
Ideal donor flaps possess sufficient blood supply, yet flaps with robust vasculature may also have a tendency for size-mismatch with the affected area.2 Although local flaps may be adequately pliable, they frequently lack reliable blood supply.1,2,6 Additional considerations include donor site morbidities, such as pain, scarring, or discoloration of the skin.2,4 Notably, freestyle fasciocutaneous thigh flaps offer singular step execution for ample soft tissue coverage.1,2,6 As outlined in this case report, integrating advanced imaging modalities with this approach provides a less morbid way to restore form and function.
CASE PRESENTATION
A 55-year-old woman presented to the emergency department with a 5-cm necrotic, erythematous vulvoperineal lesion extending 2–3 cm beyond the borders of the affected site. She was diagnosed with necrotizing soft tissue infection, visualized by contrast computed tomography (CT) of the abdomen and pelvis at admission. The patient’s medical history included poorly controlled type 2 diabetes mellitus (most recent hemoglobin A1C > 14).
METHODS
The patient underwent serial debridement with gynecology and general surgery, followed by negative pressure wound therapy (Fig. 1). She was treated with broad-spectrum antibiotics and insulin drip for diabetic ketoacidosis until glucose levels were regulated. Then, plastic surgery was consulted for wound coverage. A fasciocutaneous flap was preferred due to like-for-like reconstruction, robust blood supply, and avoidance of scarring resulting in stricture or exposure of sensitive structures.
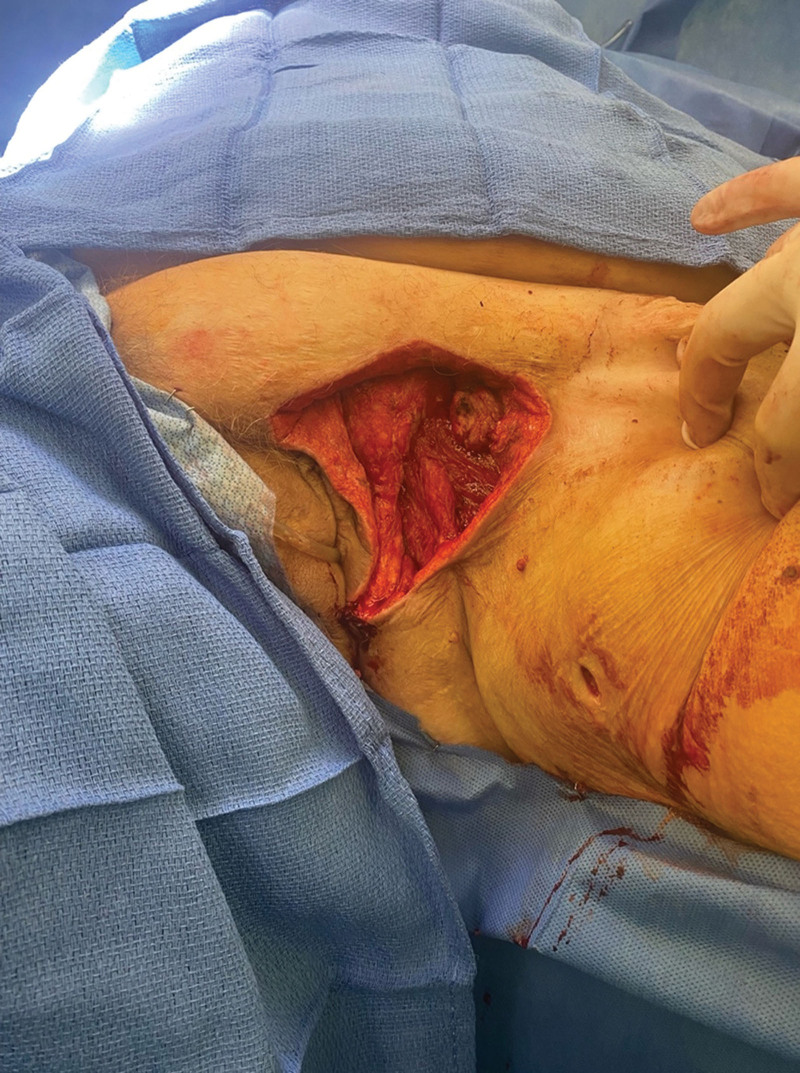
Fig. 1.
Wound after serial debridement and negative pressure wound therapy.
Using a Clarius 15-MHz portable color flow Doppler ultrasound (Clarius Vancouver, BC, Canada), a septocutaneous anterolateral thigh perforator was detected in addition to a dominant medial thigh perforator with a long course that connected to vessels in the groin preoperatively. The Misonix ultrasonic device was used to debride the wound. An incision was made where the medial thigh and anterolateral thigh flaps joined, dissecting medially in the suprafascial plane until a small perforator was encountered, which penetrated the deep fascia.
Exploring further medially, a larger perforator vessel running axially down the leg was discovered and identified as the more desirable vessel producing a stronger signal on Doppler exam (Fig. 2). An incision around the elliptical skin paddle was made and dissection continued down to the fascia circumferentially. (See figure, Supplemental Digital Content 1, which displays the flap isolated on the perforator with tunneling toward the vulvar defect. http://links.lww.com/PRSGO/D559.)
Fig. 2.
Proposed two flap options based on medial and lateral thigh perforators.
As this vessel approached the medial border of the rectus femoris, the vessel became subfascial. The deep fascia was entered, tracing toward the groin. The incision was then extended superiorly for better visualization. A 10-cm pedicle was dissected with the perforator flap. (See figure, Supplemental Digital Content 2, which displays the medial thigh after pedicled perforator flap dissection. http://links.lww.com/PRSGO/D560.) At the endpoint of the pedicle dissection, the vein diverged medially to the confluence of the grater saphenous vein and the artery coursed towards the common femoral artery.
Indocyanine green (ICG) angiography was used to assess flap perfusion, examined via the SPY PHI system (Stryker Portage, Mich.), which detected adequate perfusion. A subcutaneous tunnel was created toward the superolateral portion of the wound. The distal end of the flap was thinned and contoured for symmetry with the labia majora (Figs. 3, 4). The most prominent Doppler signal was marked with a polypropylene suture. The patient did well postoperatively and was discharged three days later with a 2-week course of intravenous antibiotics.
Fig. 3.
Flap after the final inset to vulvar defect.
Fig. 4.
Vulvoperineal region 4-months postoperatively.
DISCUSSION
Compared with myocutaneous flaps, perforator flaps can provide thinner fasciocutaneous coverage with like-for-like reconstruction, improving the quality of wound healing and reducing donor site morbidities.2,6,7 In this case, the selected vessel was found bilaterally with a deep and long axial course. The parent vessels supplying this flap, observed on initial CT with contrast, traced back to the external iliac artery and the greater saphenous vein, perhaps representing an anomalous axial flap. Freestyle perforator flaps described previously, such as by Huang et al2 were local VY advancements, differing from the regional anterior thigh perforator used in this case of vulvar reconstruction.
For complex anatomical regions coupled with subtle anatomical variation, color Doppler ultrasonography (CDU) allows comprehensive exploration of perforator options, resulting in a novel flap design. The use of CDU with pedicled freestyle perforator flap design has been associated with less morbidity compared with traditional anterolateral thigh flaps,2 favoring the use of high-resolution assistive technologies to guide flap planning. In this patient, high-resolution vascular structures were detected via CDU, validated, and confirmed by way of ICG angiography. The advantages of handheld CDU include tailoring and adjusting flap design in the operating room, providing a real-time understanding of three-dimensional anatomy. CDU can clearly show where a perforator exits the deep fascia and its course through subcutaneous fat, which aids skin paddle design and identifying suitably thin perforators or flap elevation.
CT produces a minimum of 0.5-mm slices, much larger than newer ultrasonography techniques which can locate vessels 0.2 mm in diameter.8 With improved sensitivity and precision, as well as decreased cost and need for contrast administration, this imaging modality served as an optimal guide for detecting microvasculature.8 CDU can be especially useful for visualization of superficial perforators by determining velocity of blood flow and vascular resistance to further inform on perforator selection based on the quality of perfusion.8 Successfully using CDU and ICG angiography to strategically detect viable perforators and then design a pedicled freestyle fasciocutaneous flap illustrates a promising tool for vulvar reconstruction. CDU is routinely done at our institution for perforator identification and is often the only form of imaging done for anterolateral thigh, superficial circumflex iliac artery perforator, thoracodorsal artery perforator, posterior tibial artery, peroneal artery, and other perforator flaps.
CONCLUSIONS
This treatment regimen for a vulvoperineal defect highlights how perforator selection and flap creation remain pertinent. Freestyle flap design allows for versatile reconstruction and lower risks of donor site morbidity. The CDU-mapped trajectory of a vessel reduces the risk of postoperative complications and increases the efficiency of viable perforator identification and ideal flap design. This tool has an expanding role for reconstructive surgeons, providing security in flap viability and successful reconstruction.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ETHICAL APPROVAL
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
DECLARATION OF HELSINKI
This study was conducted according to the principles expressed in the Declaration of Helsinki.
Supplementary Material
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Yang J, Ko SH, Oh SJ, et al. Reconstruction of a perineoscrotal defect using bilateral medial thigh fasciocutaneous flaps. Arch Plast Surg. 2013;40:72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang JJ, Wu CW, Tsao CK, et al. Pedicled perforator flaps for vulvar reconstruction—a versatile, less invasive and simple way with favorable results. Plast Reconstr Surg. 2014;134:148–149. [Google Scholar]
- 3.Ahmad I, Maurya RK, Mahmud AA, et al. Medial thigh flap: an eminent method of reconstruction of scrotal defect following Fournier’s gangrene. Turk J Plast Surg. 2018;26:116–121. [Google Scholar]
- 4.Caretto AA, Servillo M, Tagliaferri L, et al. Secondary post-oncologic vulvar reconstruction—a simplified algorithm. Front Oncol. 2023;13:1195580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muneuchi G, Ohno M, Shiota A, et al. Deep inferior epigastric perforator (DIEP) flap for vulvar reconstruction after radical vulvectomy: a less invasive and simple procedure utilizing an abdominal incision wound. Ann Plast Surg. 2005;55:427–429. [DOI] [PubMed] [Google Scholar]
- 6.Persichetti P, Simone P, Berloco M, et al. Vulvo-perineal reconstruction: medial thigh septo-fascio-cutaneous island flap. Ann Plast Surg. 2003;50:85–89. [DOI] [PubMed] [Google Scholar]
- 7.Hand LC, Maas TM, Baka N, et al. Utilizing V-Y fasciocutaneous advancement flaps for vulvar reconstruction. Gynecol Oncol Rep. 2018;26:24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chim H, Nichols DS, Chopan M. Ultrasound for perforator mapping and flap design in the hand and upper extremity. J Hand Surg Am. 2023;48:595–601. [DOI] [PubMed] [Google Scholar]