Abstract
Background
This study aimed to clarify the feasibility of cardiovascular physical therapy assessment and intervention in older patients with heart failure (HF) in Japan.
Methods and Results
We performed a secondary analysis of data from a nationwide multicenter registry (the J-Proof HF), and enrolled consecutive HF patients aged ≥65 years who were prescribed cardiovascular physical therapy during hospitalization from December 2020 to March 2022. Of the 9,650 enrolled patients (median age 83.0 years; 49.8% male), the availability rate of comorbidities and assessments was >95%. In the activities of daily living (ADL) assessment, the Barthel Index (BI) and Functional Independence Measure were 97.6% and 60.4%, respectively. The results of the physical therapy assessment indicated completion rates of ≥80%, with lower rates of <60% for gait speed and short-performance physical battery in the group with a BI of <85 points. In physiotherapy intervention, gait training and muscle strength training were performed by >80% of patients, whereas aerobic exercise and resistance training were performed by 35.4% and 2.6% patients, respectively.
Conclusions
Our results in this study indicated that medical findings, such as comorbidities, echocardiography, and laboratory findings, were considered a feasible assessment that could be confirmed at all hospitals. Gait training, ADL training, and muscle strength training are much more common than exercise training in older patients with HF.
Key Words: Feasible assessment and intervention, Older heart failure, Physical therapy
The number of patients with heart failure (HF), especially older patients, has increased exponentially over the past decade and is expected to increase continuously throughout the next decade in Japanese society.1 HF in the elderly is often difficult to treat due to multimorbidity, low physical function, and difficulty in continuing treatment, including taking medications, self-management, and participating in an outpatient cardiac rehabilitation program.2 Therefore, there is a need to develop effective intervention strategies for older patients with HF.
Standard assessment and treatment for patients with HF are provided by the Heart Failure Treatment Guidelines of the Japanese Society of Cardiology and the Standard Program of the Japanese Society of Cardiac Rehabilitation.2,3 Despite the guidelines that summarize scientific evidence and standard programs that guide clinical practice, it is unclear whether the assessments and treatments recommended in the guidelines and standard programs are implemented in a clinical setting. Furthermore, while guidelines and standard programs cover a broad population of patients with HF, they are limited with respect to content specific to older patients with HF and physical therapy.
The Japanese Society of Cardiovascular Physical Therapy is conducting the Japanese Physical Therapy Multicenter Registry of Older Frail patients with Heart Failure (J-Proof HF), a nationwide registry of physical therapy in older HF patients. We have reported that 37.1% of patients had hospitalization-associated disability, which is a decline in the capacity for activities of daily living (ADL) during hospitalization.4 Demonstrating real-world data on assessments and interventions related to cardiovascular physical therapy in Japan will enable us to provide useful information for the standardization of assessment and intervention strategies.
Therefore, the purpose of the present study was to clarify the availability and feasibility of the assessment and intervention of cardiovascular physical therapy for older patients with HF in Japan using data from the J-Proof HF.
Methods
Participants
The J-Proof HF is a prospective nationwide multicenter registry of patients with acute HF in Japan. A total of 96 institutions throughout Japan that employ members of the Japanese Society of Cardiovascular Physical Therapy participated in the registry. From December 2020 to March 2022, consecutive patients aged ≥65 years who were prescribed physical therapy by their physicians during hospitalization after admission for worsening HF were enrolled in the J-Proof HF. The exclusion criteria were death during hospitalization, invasive treatment (transcatheter aortic valve implantation, MitraClip, or surgery) during hospitalization, acute coronary syndrome, and inability to walk before admission. Patients who were discharged within 3 days or transferred to another department or hospital due to the onset of a new disease during hospitalization were also excluded.
Basic information on the J-Proof HF, study description, and primary and secondary endpoints can be found in the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (ID UMIN000047893). The research protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Juntendo University School of Health Sciences, Tokyo, Japan (Reference no. 19-005). The study was approved by the ethics committees of all 96 participating institutions.4 Patient consent was obtained using either the opt-out or informed consent method, depending on the judgment of the ethics committees of the participating institutions.
Data Collection
We collected patient demographic data, diagnoses, comorbidities (including diabetes [DM], hypertension [HT], hyperlipidemia [HL], chronic kidney disease [CKD], hemodialysis [HD], myocardial infarction [MI], chronic obstructive pulmonary disease [COPD], musculoskeletal disease, cerebrovascular disease [CVD], cancer, and peripheral artery disease [PAD]), cardiac function based on echocardiography (including left ventricular ejection fraction [LVEF], left atrial dimension [LAD], and ratio of the early transmitral flow velocity to the early diastolic mitral annular velocity [E/e′]), and laboratory data at admission (creatinine [Cre], albumin [Alb], blood urea nitrogen [BUN], estimated glomerular filtration rate [eGFR], C reactive protein [CRP], hemoglobin [Hb], sodium [Na], B-type natriuretic peptide [BNP], and N terminal proBNP [NT-proBNP]) from the medical charts. HT was determined as currently treating or blood pressure of 140/80 mmHg or higher. Diabetes was determined as currently treating, HbA1c >6.5%, fasting blood glucose >126 mg/dL or occasional blood glucose >200 mg/dL. HL was determined as currently treating or LDL >140 mg/dL, HDL <40 mg/dL, and triglycerides >150 mg/dL.
To evaluate the prehospital ADL status, the Barthel Index (BI)5 and Kihon checklist (KCL) score6 were also recorded, and the Functional Independence Measure (FIM)7 was also evaluated at discharge wherever possible. The Short Physical Performance Battery (SPPB),8 grip strength, walking speed, upper arm and lower leg circumferences, and Japanese Cardiovascular Health Study Index9 scores were assessed at hospital discharge. We also collected data on physical therapy during hospitalization, including the length of hospital stay, duration of physical therapy, number of physical therapy units (20 min/unit), and physical therapy intervention programs as follows: ADL training, gait training, muscle strength training, aerobic exercise, and resistance training. In this study, we defined exercise therapy performed with specific exercise equipment as aerobic exercise or resistance training, and other types as gait training and muscle strength training.
At the data center, omissions, input errors, and out-of-range values were checked by a person not involved in the study on a computer with restricted access that was not connected to the Internet, and each institution was asked to correct the data if necessary. The data were then re-entered and double-checked by 2 physical therapists for additional verification.
Data Analysis
Continuous variables are presented as medians and interquartile ranges (IQR), while categorical variables are presented as numbers and percentages. In this study, the input rate was calculated as the availability rate. We also calculated the availability rate of physical therapy assessments and intervention programs by dividing the patients into 2 groups according to the presence or absence of disuse syndrome (BI <85 points at discharge). We compared the groups using either the chi-square test or Fisher’s exact test, as appropriate.
All analyses were performed using the SPSS 26.0 software package (SPSS Inc., Tokyo, Japan), with a P value of <0.05 considered statistically significant.
Results
Between December 2020 and March 2022, 10,062 patients were enrolled; 412 patients met the exclusion criteria and were excluded, leaving 9,650 patients included in the present study (Figure 1). The median age of patients was 83.0 years (IQR 77–88 years), and 49.8% of patients were male. Table 1 shows the demographic and clinical characteristics of patients. The median length of hospital stay was 16 days, and the median pre-admission BI and KCL scores were 100 and 11 points, respectively. The median value of the LVEF was 47%, whereas for BNP and NT-proBNP, it was 556.7 pg/mL and 4,798.0 pg/mL, respectively. The median duration of physical therapy during hospitalization was 7 days, while the median number of physical therapy units was 15.0 units. A total of 3,245 (33.6%) patients was diagnosed with disuse syndrome (BI <85 points) at discharge.
Figure 1.
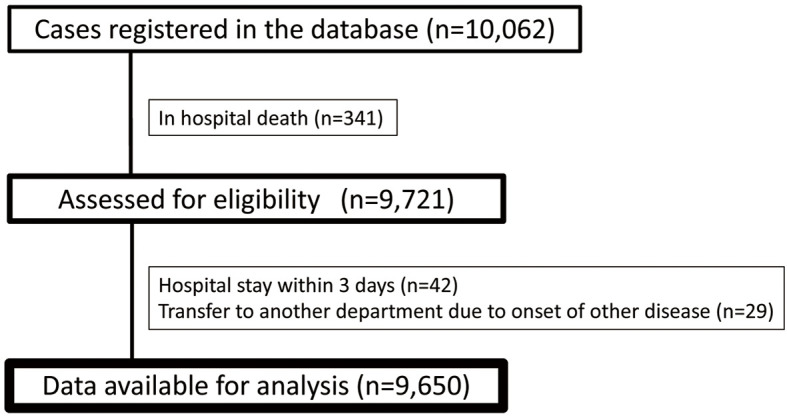
Flowchart of patient selection.
Table 1.
Demographic and Clinical Characteristics of Patients
| Total (n=9,650) |
Missing data, n (%) |
|
|---|---|---|
| Age (years) | 83 [77–88] | 0 (0) |
| Male sex | 49.8 | 0 (0) |
| BMI (kg/m2) | 22.5 [20.1–25.2] | 314 (3.2) |
| Hospital stay (days) | 16 [11–23] | 0 (0) |
| HT | 68.1 | 0 (0) |
| Ischemic heart disease | 15.5 | 0 (0) |
| Diabetes | 34.6 | 0 (0) |
| HL | 31.2 | 0 (0) |
| CKD | 39.3 | 1 (0) |
| HD | 1.9 | 1 (0) |
| COPD | 7.3 | 0 (0) |
| MSD | 26.0 | 0 (0) |
| CVD | 15.6 | 0 (0) |
| NYHA | 23 (0.2) | |
| I | 3.6 | |
| II | 19.0 | |
| III | 40.5 | |
| IV | 36.7 | |
| LVEF | 47.4 [34.0–61.0] | 583 (6) |
| HFrEF/HFmrEF/HFpEF | 34.0/17.1/48.9 | |
| LAD (mm) | 44.3 [39.0–49.0] | 999 (10) |
| E/e′ | 16.9 [12.2–23.0] | 2,646 (26.5) |
| Hb (g/dL) | 11.4 [10.0–13.0] | 24 (0.2) |
| Alb (g/dL) | 3.5 [3.2–3.8] | 250 (2) |
| Na (mEq/L) | 140 [138–142] | 25 (0.2) |
| eGFR (mL/min/1.73 m2) | 41.0 [28.0–55.7] | 107 (1) |
| BNP (pg/dL) | 556.7 [308.6–991.9] | 100 (1) |
| NT-proBNP (pg/dL) | 4,798.0 [2,247–10,398] | 100 (1) |
| Prehospital Kihon checklist (points) | 11 [7–14] | 1,136 (12) |
| Prehospital Barthel index (points) | 100 [85–100] | 196 (2) |
| FIM at discharge (points) | 111 [90–123] | 3,825 (39.6) |
| Medication | ||
| ACE/ARB/ARNi | 57.5 | 10 (0.1) |
| β-blockers | 65.8 | 10 (0.1) |
| MRA | 31.2 | 10 (0.1) |
| SGLT-2 inhibitor | 15.9 | 23 (0.2) |
| Diuretics | 84.7 | 10 (0.1) |
| Anticoagulant agent | 49.5 | 9 (0.1) |
Unless indicated otherwise, data are presented as %, or median [IQR]. ACE, angiotensin-converting enzyme; Alb, albumin; ARB, angiotensin II receptor blocker; ARNi, angiotensin receptor neprilysin inhibitor; BMI, body mass index; BNP, B-type natriuretic peptide; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disease; eGFR, estimated glomerular filtration rate; FIM, functional independence measure; Hb, hemoglobin; HD, hemodialysis; HFmrEF, heart failure with mildly reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HL, hyperlipidemia; HT, hypertension; LAD, left atrial dimension; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonists; MSD, musculoskeletal disease; Na, sodium; NT-proBNP, N-terminal pro B-type natriuretic peptide; NYHA, New York Heart Association; SGLT2, sodium-glucose cotransporter 2.
The comorbidities, cardiac function, and laboratory data are shown in Table 1. Almost all assessments had an availability rate of above 95%, with LAD and E/e′ being available in 89.6% and 72.5% of patients, respectively. In the ADL assessment, the BI and FIM data were available in 97.6% and 60.4% of patients, respectively.
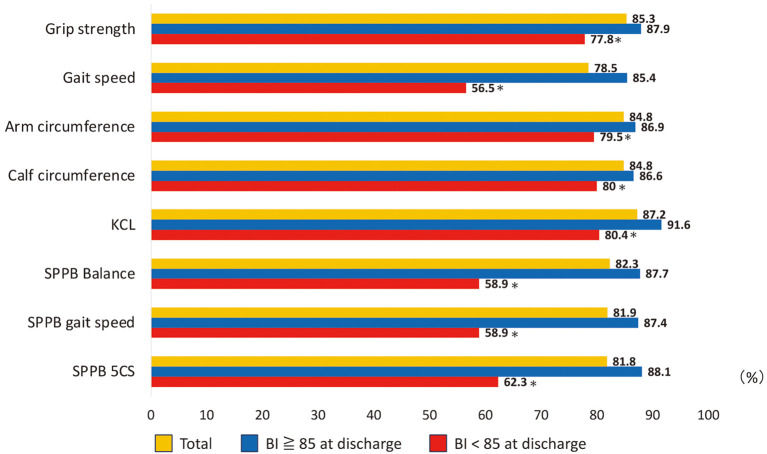
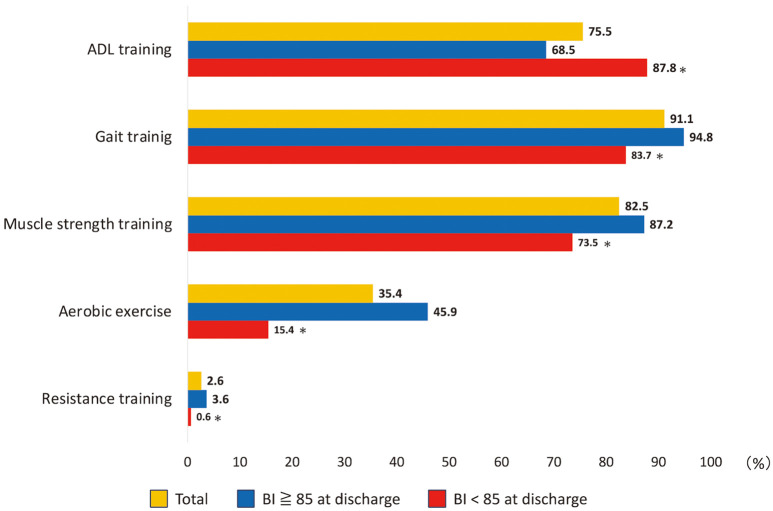
The results of the physical therapy assessments are shown in Figure 2. The physical functional assessments had an availability rate of approximately 80% or higher, with lower rates of <60% for gait speed and SPPB in the group with a BI <85 points (P<0.001). Details of the physical therapy interventions are presented in Table 2 and Figure 3. The total number of units during hospitalization averaged 19.9 units, with an average of 1.7 units per day. Gait and muscle strength training was performed in >80% of patients, whereas aerobic exercise and resistance training was performed in 3,414 (35.4%) and 241 (2.6%) patients, respectively.
Figure 2.
Availability rates of assessment of physical function and performance. *P<0.001 vs. BI ≥85 group. 5CS, 5 chair stand; BI, Barthel Index; KCL, Kihon checklist; SPPB, short physical performance battery.
Table 2.
Distribution of Hospital Stay and Amount of PT Intervention
| Length of hospital stay (days) |
Initiation days of PT (days) |
No. total PT (units) |
Duration of PT (days) |
Daily dose of PT (unit/day) |
|
|---|---|---|---|---|---|
| Mean | 19.0 | 3.8 | 19.9 | 11 | 1.7 |
| 25% tile | 11 | 2 | 10 | 6 | 1.2 |
| Median | 16 | 3 | 15 | 9 | 1.6 |
| 75% tile | 23 | 4 | 24 | 13 | 2 |
| Minimum | 4 | 1 | 1 | 1 | 0.4 |
| Maximum | 317 | 110 | 236 | 137 | 3 |
PT, physical therapy.
Figure 3.
Availability rates of physical therapy intervention. *P<0.001 vs. BI ≥85 group. ADL, activities of daily living; BI, Barthel Index.
Discussion
The present study used nationwide registry data to examine the feasibility of cardiovascular physical therapy assessments and interventions. In summary, comorbidities, cardiac function, and laboratory data were available for more than 90% of patients, and the availability rates of ADL assessment were 97% for BI and 60% for FIM. Approximately 80% underwent physical function assessment; more than 70% underwent ADL, gait, and muscle strength training; 35% underwent aerobic exercise; and 2.6% underwent resistance training. To the best of our knowledge, this study is the first to clarify the feasibility rate of the assessments and interventions recommended by the guidelines and standard programs.
Japanese Large-Scale Registry Study on HF
A previous large-scale registry study of acute HF patients with AHF in Japan included the JCARE-CARD (2013)10 and ATTEND registry (2011).11 The JCARE-CARD enrolled 2,675 patients with acute and chronic HF at 164 hospitals, while the ATTEND registry enrolled 1,110 patients with acute heart failure at 32 hospitals. The J-Proof HF enrolled 10,620 patients with acute HF at 96 hospitals and is considered one of the largest registries among previous studies in Japan. In addition, the median age of the study population was 83 years, which is approximately 10 years older than in previous studies; this may be related to the inclusion criteria of J-Proof HF, which included patients aged ≥65 years and those prescribed physical therapy as an inpatient. The inclusion criteria of this study differs from the JCARE-CARD and ATTEND registry, reflecting the current state of cardiovascular physiotherapy for older HF patients.
The J-Proof HF subjects had an average hospital stay of 16.0 days, LVEF of 47.4%, BNP of 556.7 pg/dL, and NT-proBNP of 4,798.0 pg/dL. In contrast, the aforementioned studies reported average hospitalization durations of 15 days10 and 21 days,11 LVEF of 42%,10 and BNP levels of 878 pg/dL10 and 1,063 pg/dL.11 The present study demonstrates a patient background similar in size to previous study reports and is considered to reflect the real-world data of HF patients in Japan. Therefore, as the J-Proof HF reflects the true characteristics of HF patients receiving physiotherapy during hospitalization, it is likely that the results can be generalized to real-world cardiovascular physiotherapy practices in Japan.
Patient Characteristics on the Medical Chart
The availability rate of the comorbidities, cardiac function, and laboratory findings investigated in this study was almost 100%, indicating that these findings can be confirmed at any hospital. In this study, we investigated the comorbidities DM, HT, HL, CKD, HD, MI, COPD, MSD, CVA, malignancy, and PAD. DM, HT, HL, MI, and PAD are the coronary risk factors associated with ischemic heart disease. Although not direct outcome measures for physical therapy, these findings are crucial for understanding patient health and should be routinely assessed using the Japanese Cardiac Rehabilitation Standard Program.3 Additionally, CKD and HD have been reported as prognostic factors for HF, whereas COPD, musculoskeletal disease, and CVA have been reported to affect physical therapy intervention programs. These findings highlight the importance of a comprehensive approach to cardiovascular physical therapy. The laboratory findings investigated in this study, including creatinine (eGFR), Alb, CRP, Hb, Na, and BNP/NT-proBNP, have been reported as prognostic factors in patients with HF,12 and are important for understanding HF severity and conditions. Moreover, LVEF is frequently used in clinical settings, including HF classification13 and risk stratification during cardiac rehabilitation.3 Although the findings collected in this study were not directly measured by the physical therapist and were extracted from the medical chart, the availability rate was more than 90%, which can be confirmed at any hospital, suggesting that these findings should be a feasible assessment in cardiovascular physical therapy.
Assessment of Physical Function, ADL, and Frailty
The results of this study showed an availability rate of approximately 80% for the assessment of physical function and was higher for those with BI scores >85 points at approximately 90%. Arm circumference, grip strength, gait speed, and SPPB scores investigated in this study were used as prognostic factors in a previous study on patients with HF. Additionally, the BI and CHS criteria have been reported to be associated with prognosis in previous studies on patients with HF.14,15 These findings are also important as treatment outcome measures for physical therapy,2 and are recommended in guidelines and standard programs as they are easy to perform in a clinical setting.2,3 Based on the availability rate of >80% in this study, these findings suggest it is feasible to incorporate these assessments into cardiovascular physical therapy practice.
The results of this study showed that the availability rate of the FIM was 60.4%. The FIM assesses independence in ADL and is mainly used in the field of stroke rehabilitation. It was rarely performed in the cardiovascular field previously because most patients requiring cardiac rehabilitation were younger and independent in ADL. According to the Japanese health care insurance system, an FIM score of <115 points is the criterion for disuse syndrome, and previous findings of the J-Proof HF reported that 55.5% of older patients with HF had a discharge FIM score of <115 points.4 This study used the FIM assessment as a measurement outcome whenever possible, with an availability rate of 60.4%; however, it is expected that this rate is likely to be even lower in clinical settings. As the number of older HF patients with low ADL is expected to increase in the future, the number of patients who need transfer to recovery phase rehabilitation hospitals is expected to also increase. While Japanese guidelines recommend cardiac rehabilitation programs in the recovery phase setting, the guidelines and standard programs lack specific guidance on ADL assessment. Therefore, to ensure seamless continuation of cardiovascular physiotherapy in recovery phase rehabilitation hospitals, increasing the use of the FIM assessment in the cardiovascular physiotherapy field is crucial.
Physical Therapy Program
The results of this study showed that gait training and muscle strength training were performed in 90% of patients, and this high rate was also maintained in the group with a BI of <85 points. Previous J-Proof HF have reported that approximately 40% of older patients with HF develop hospital-associated disabilities.4 Therefore, maintaining physical function and activity during the acute phase is important. Early mobilization programs are recommended for patients with acute HF,2,3 which may be a reason for the high rates of gait and muscle strength training. In addition, no special equipment or machine is required for gait and muscle strength training, making them feasible at any hospital. The results of the present study suggest that gait and muscle strength training are frequently performed physical therapy interventions in older patients with HF.
In contrast, the rates of exercise therapy, such as aerobic exercise and resistance training, were low at 35.4% and 2.6%, respectively. These rates were further reduced in patients with a BI score of <85 points. Although guidelines recommend that exercise therapy should be performed in older patients with HF,2 it was observed that there is a lower prevalence of aerobic exercise and resistance training performed in the clinical setting of older HF patients. Approximately 60% of the J-Proof HF participants had physical frailty at discharge, which could be the reason for the lower rate of exercise therapy. Furthermore, the median value of in-hospital physical therapy was 9 days, which suggests that there may not have been enough days to perform exercise therapy during the acute phase hospital setting. Based on the results of present study, further research is needed to identify factors influencing exercise therapy and to develop standard physical therapy interventions for older patients with HF.
Study Limitations
The present study has several limitations. First, although the J-Proof HF was established with the cooperation of 96 institutions throughout Japan, it did not cover all regions of Japan or all hospitals offering cardiac rehabilitation. Second, this study only included patients who were prescribed physical therapy after hospitalization in an acute hospital; we could not include all patients who did not undergo physical therapy. Approximately 40% of all HF patients received physical therapy during hospitalization in a previous nationwide survey;16 therefore, our findings may be somewhat influenced by selection bias. Future research with a larger, more representative sample could provide more definitive insights. Third, we have not collected the findings that are considerably well known for exercise testing, including the 6-min walking distance and cardiopulmonary exercise testing. Last, the data collection period for this study was during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. A previous study reported that the SARS-CoV-2 pandemic has affected cardiac rehabilitation programs;17 consequently, the low rate of exercise training in our study may have been affected by the SARS-CoV-2 pandemic. Nevertheless, this study is the first to demonstrate real-world Japanese data on cardiovascular physical therapy, and the results of this study will be useful for validating the quality of clinical practice.
Conclusions
The main findings of this study were that medical findings, including comorbidities, echocardiography, and laboratory findings, of the J-Proof HF were considered feasible measurements that could be confirmed at all hospitals. Furthermore, the assessments of physical function from the J-Proof HF were shown to be highly feasible for patients who are independent in their ADL. Basic training, which includes ADL, gait, and muscle strength training, is much more common than exercise training in older patients with HF.
Sources of Funding
This work was supported by research funding from the Japanese Society of Cardiovascular Physical Therapy.
Disclosures
K.K. and T.T. are members of Circulation Reports’ Editorial Team.
IRB Information
The research protocol was approved by the Ethics Committee of Juntendo University School of Health Sciences, Tokyo, Japan (Reference no. 19-005).
Acknowledgments
The authors are grateful to Kaori Taniguchi (Faculty of Health Science, Juntendo University) for technical assistance. During the preparation of this manuscript, the authors used DeepL to verify their written English.
References
- 1. Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, Ito M, et al.. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ J 2008; 72: 489–491. [DOI] [PubMed] [Google Scholar]
- 2. Makita S, Yasu T, Akashi YJ, Adachi H, Izawa H, Ishihara S, et al.. JCS/JACR 2021 guideline on rehabilitation in patients with cardiovascular disease. Circ J 2022; 87: 155–235. [DOI] [PubMed] [Google Scholar]
- 3. Izawa H, Yoshida T, Ikegame T, Izawa KP, Ito Y, Okamura H, et al.. Standard cardiac rehabilitation program for heart failure. Circ J 2019; 83: 2394–2398. [DOI] [PubMed] [Google Scholar]
- 4. Takahashi T, Iwata K, Morisawa T, Kato M, Kono Y, Taya M, et al.. Incidence of hospitalization-associated disability in older patients with heart failure. Circ J 2024; 88: 672–679. [DOI] [PubMed] [Google Scholar]
- 5. Mahoney FI, Barthel DW.. Functional evaluation: The Barthel Index. Md State Med J 1965; 14: 61–65. [PubMed] [Google Scholar]
- 6. Arai H, Satake S.. English translation of the Kihon Checklist. Geriatr Gerontol Int 2015; 15: 518–519. [DOI] [PubMed] [Google Scholar]
- 7. Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD.. Performance profiles of the functional independence measure. Am J Phys Med Rehabil 1993; 72: 84–89. [DOI] [PubMed] [Google Scholar]
- 8. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al.. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–M94. [DOI] [PubMed] [Google Scholar]
- 9. Satake S, Arai H.. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr Gerontol Int 2020; 20: 992–993. [DOI] [PubMed] [Google Scholar]
- 10. Hamaguchi S, Yokoshiki H, Kinugawa S, Tsuchihashi-Makaya M, Yokota T, Takeshita A, et al.. Effects of atrial fibrillation on long-term outcomes in patients hospitalized for heart failure in Japan: A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2009; 73: 2084–2090. [DOI] [PubMed] [Google Scholar]
- 11. Sato N, Kajimoto K, Asai K, Mizuno M, Minami Y, Nagashima M, et al.. Acute decompensated heart failure syndromes (ATTEND) registry. A prospective observational multicenter cohort study: Rationale, design, and preliminary data. Am Heart J 2010; 159: 949–955. [DOI] [PubMed] [Google Scholar]
- 12. Tsutsui H, Isobe M, Ito H, Ito H, Okumura K, Ono M, et al.. JCS 2017/JHFS 2017 guideline on diagnosis and treatment of acute and chronic heart failure. Circ J 2019; 83: 2084–2184. [DOI] [PubMed] [Google Scholar]
- 13. Tsutsui H, Ide T, Ito H, Kihara Y, Kinugawa K, Kinugawa S, et al.. JCS/JHFS 2021 guideline focused update on diagnosis and treatment of acute and chronic heart failure. Circ J 2021; 85: 2252–2291. [DOI] [PubMed] [Google Scholar]
- 14. Motoki H, Nishimura M, Kanai M, Kimura K, Minamisawa M, Yamamoto S, et al.. Impact of inpatient cardiac rehabilitation on Barthel Index score and prognosis in patients with acute decompensated heart failure. Int J Cardiol 2019; 293: 125–130. [DOI] [PubMed] [Google Scholar]
- 15. Hamada T, Kubo T, Kawai K, Nakaoka Y, Yabe T, Furuno T, et al.. Clinical characteristics and frailty status in heart failure with preserved vs. reduced ejection fraction. ESC Heart Fail 2022; 9: 1853–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kamiya K, Yamamoto T, Tsuchihashi-Makaya M, Ikegame T, Takahashi T, Sato Y, et al.. Nationwide survey of multidisciplinary care and cardiac rehabilitation for patients with heart failure in Japan: An analysis of the AMED-CHF Study. Circ J 2019; 83: 1546–1552. [DOI] [PubMed] [Google Scholar]
- 17. Kida K, Nishitani-Yokoyama M, Kono Y, Kamiya K, Kishi T, Node K, et al.. Second nationwide survey of Japanese cardiac rehabilitation training facilities during the coronavirus disease 2019 (COVID-19) outbreak. Circ Rep 2022; 4: 469–473. [DOI] [PMC free article] [PubMed] [Google Scholar]