Abstract
Purpose of Review
To provide an overview of the current evidence of the timing of surgery and rehabilitation after multiligamentous knee injuries (MLKIs) and offer insights into the ongoing multi-center randomized controlled study, the ‘STaR trial’.
Recent Findings
Due to the complexity of the MKLIs, they are usually treated surgically with the goal of either repairing or reconstructing the injured ligaments. Although the current literature on MLKIs is relatively extensive, the consensus on the timing of surgery or rehabilitation following surgery for MLKIs is still lacking. While current literature mostly suggests early treatment, there is also evidence preferring delayed treatment. Furthermore, evidence on the timing of postoperative rehabilitation is limited. Thus, the current multi-center randomized controlled study, the ‘STaR trial’, is expected to respond to these questions by adding new high-level evidence.
Summary
The MLKIs are often associated with knee dislocation and constitute a highly complex entity, including concomitant injuries, such as neurovascular, meniscal, and cartilaginous injuries. The treatment of MLKIs usually aims to either repair or reconstruct the injured ligaments, however, there is no general consensus on the timing of surgery or rehabilitation following an MLKI surgery. This current review stresses the need for more high-level research to address the paucity of evidence-based treatment guidelines for the treatment of complex MLKIs.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12178-024-09923-w.
Keywords: Multiligamentous knee injury, MLKI, Timing, Surgery, Rehabilitation, Complications, Outcomes
Introduction
Multiligamentous knee injuries (MLKIs) are severe, limb-threatening injuries that can occur either in conjunction with tibiofemoral dislocation or independently. The definition of MLKI requires the injury of at least two of the four knee ligaments, including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MLC) lateral collateral ligament (LCL) and posterolateral corner (PLC) (Fig. 1). These injuries are usually associated with sporting activities, such as skiing and American football, or high-velocity events like motor vehicle accidents [1]. In some cases, MLKIs may also be linked to low-velocity injuries, particularly in patients with high body mass index [2].
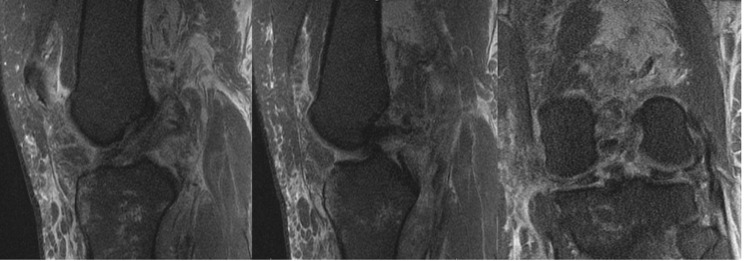
Fig. 1.
MRI of MLKI involving ACL, PCL, and PLC. ACL = anterior cruciate ligament; MLKI = multiligamentous knee injury; MRI = magnetic resonance imaging; PCL = posterior cruciate ligament; PLC = posterolateral corner
MLKIs have traditionally been classified using the Schenck classification system, which categorized the injured ligaments, the number of injured structures, and the eventual presence of concomitant periarticular fractures, [3] or by the Moore classification system in cases of fracture-dislocations [4]. However, a new classification system, focusing on the pathoanatomy of MLKIs has recently been developed as a part of a large multi-center randomized controlled study called ‘the Surgical Timing and Rehabilitation (STaR) trial’ (Table 1) [5]. Due to the complexity of the MKLIs, they are usually treated surgically with the aim of either repairing or reconstructing the injured ligaments [6, 7]. Although the current literature on MLKIs is relatively extensive, there is still no consensus on the timing of surgery or rehabilitation following surgery for MLKIs. Thus, the goal of this review is to provide an overview of the current evidence of the timing of surgery and rehabilitation after MLKIs and offer insights into the ongoing multi-center randomized controlled study, the ‘STaR trial’.
Table 1.
Anatomic classification of knee dislocation according to Poploski et al. [5].
| MLK 1-AM | Complete tear of the ACL with complete tear of the sMCL and/or PMC |
|---|---|
| MLK 1-AL | Complete tear of the ACL with complete tear of the LCL and/or PLC |
| MLK 1-AML | Complete tear of the ACL with complete tear of the sMCL and/or PMC and the LCL and/or PLC |
| MLK 1-PM | Complete tear of the PCL with complete tear of the sMCL and/or PMC |
| MLK 1-PL | Complete tear of the PCL with complete tear of the LCL and/or PLC |
| MLK 1-PML | Complete tear of the PCL with complete tear of the sMCL and/or PMC and the LCL and/or PLC |
| MLK 2 | Complete tears of the ACL and PCL without injury to the sMCL, PMC, LCL, or PLC |
| MLK 3-M | Complete tears of the ACL and PCL with complete tear of the sMCL and/or PMC |
| MLK 3-L | Complete tears of the ACL and PCL with complete tear of the LCL and/or PLC |
| MLK 4 | Complete tears of the ACL, PCL, sMCL and/orPMC, and LCL and/or PLC |
ACL: Anterior cruciate ligament; LCL: Lateral collateral ligament; MLK: Multiligamentous knee injury, PCL: Posterior cruciate ligament; PLC: Posterolateral corner; PMC: Posteromedial corner; sMCL: Superficial medial collateral ligament
Associated Injuries
MLKIs are commonly associated with other concomitant injuries, such as neurovascular, meniscal, and cartilaginous injuries, as well as intra-articular fractures. While peroneal nerve injuries have been reported to occur in approximately 19% of MLKI cases, vascular injuries have been shown to present in 18% of MLKI injuries, depending on the nature of the injury [8]. Neurovascular injuries have shown to occur most commonly along with MLKI injuries involving structures such as PCL, LCL, and/or PLC [5]. Concomitant meniscal injuries have been shown to exist in approximately 56% of MLKI injuries, most commonly occurring along with MLKIs involving ACL [5]. Cartilaginous injuries have been associated with approximately 28% of MLKI cases [8], with an incidence of 40% in combined ACL and PCL reconstruction cases [9]. Finally, the incidence of intra-articular fractures, involving the femoral condyle or tibial plateau, is not fully understood as many current studies have excluded concomitant fractures [10–12]. Nevertheless, a recent study, aiming to report characteristics of MLKIs using a pathoanatomic MLKI classification system, demonstrated the incidence of intra-articular fractures in combination with MLKIs varying between 2% and 25% [5]. Notably, these intra-articular fractures were most commonly observed in knees with injuries to the MCL and/or PMC, coupled with injuries to the LCL and/or PLC, in combination with either ACL or PCL injury.
Treatment
Immediate Management
Early management principles of MLKI are relatively well established. Generally, Adult Trauma Life Support (ATLS) principles should be applied for all high-energy MLKIs when presenting in the acute setting. A thorough neurovascular examination has to be performed, including distal pulses and sensitivity, capillary refill time, motor function of all limb compartments and further examination such as the ankle brachial pressure index (ABPI). Any pathological finding mandates immediate exploration by a vascular surgeon. In the presence of a knee dislocation, primary management is the immediate reduction of the knee joint (Fig. 2). Restoring anatomical alignment is supposed to prevent further damage to intra- and extraarticular tissues and neurovascular structures. To ensure adequately maintained reduction, the knee joint should be immobilized in a splint and radiographs should be obtained. If surgical intervention is required for a vascular injury, an external fixator can be applied concomitantly. This may also be indicated in the presence of fractures, open injuries or in cases where concentric alignment of the knee joint cannot be achieved or maintained by closed reduction and splinting [13]. Generally, all acute MLKI should be considered and treated as a knee dislocation whether witnessed or not, considering potential spontaneous or pre-hospital reduction [14]. Accurate and vigilant treatment is required to avoid oversights or misdiagnoses, which might endanger limb preservation and might cause devastating short- and long-term outcomes [15].
Fig. 2.

X-ray of Posterior Tibiofemoral Dislocation and Reduced Tibiofemoral Joint
Surgical vs. Non-Surgical Treatment
Due to a paucity of high-level evidence on which to base treatment decisions, controversy regarding optimal management remains, as there is currently no comprehensive consensus approach to the treatment of MLKI [16]. The heterogeneous nature of these injuries and advances in surgical techniques must be considered when comparing operative versus non-operative approaches of MLKI. However, the vast majority of current literature suggests that operative treatment is superior in improving functional and clinical outcomes [11, 12, 17–20], as well as associated with higher rates of return to work and activity [17, 19–21] when compared to nonoperative management. Non-operative treatment may be considered in exceptional cases, i.e. comorbidities, concomitant traumatic injuries, or immobility contraindicate knee surgery. In summary, surgical stabilization can be considered the current standard for management in medically appropriate patients with MLKI.
Timing of Surgery (Acute vs. Delayed)
Although there is now general consensus on operative treatment providing better outcomes for most patients, there is ongoing debate on the optimal timing of surgery for MLKI.
Supporters of early surgery argue for operating within the acute phase after injury, within which identification of injured structures and neurovascular anatomy is not significantly impaired by scar formation. Avoiding substantial scarring or degeneration of damaged tissue in an early approach is particularly important in the case of bony avulsions and when considering ligament repair techniques [22]. Furthermore, many authors advocate for early surgery to enable the earlier beginning of rehabilitation with restored joint mechanics, ultimately yielding better functional outcomes [7, 10, 11, 23] and reduced risk of subsequent chondral or meniscal damage. However, there is currently no consensus on the critical time frame for early surgery, with many authors suggesting two or three weeks within injury. [10, 11, 14, 24]
Other authors have reported favorable outcomes of a staged approach [25]. Delayed operative management has been associated with advantages, such as reduced swelling, improved preoperative range of motion, and initiation of rehabilitation before surgery. Early surgery in the presence of capsular injury may lead to fluid extravasation and increased risk of compartment syndrome [13]. Delaying surgery may further avoid unnecessary operative treatment by enabling the healing of structures with intrinsic healing potential, such as the MCL before then surgically targeting those structures that have not healed. Supporters of delayed surgery further argue that acute surgical management of cruciate ligaments has been associated with a higher incidence of arthrofibrosis [26].
Beyond these arguments it is important to note, that surgical timing may be dictated by external factors. Early, non-ligamentous surgical intervention may be necessary under certain circumstances including neurovascular injury and open or non-reducible knee dislocation. Likewise, concomitant life-threatening injuries may preclude early ligament reconstruction. Studies investigating optimal surgical time management are complicated by a large number of confounding factors. Most of the currently available knowledge is based on retrospective studies and randomized controlled trials are scarce.
One-Stage vs. Two-Stage
In addition to deciding whether to pursue acute or delayed treatment of a MLKI, these procedures can also be done in a staged fashion. While less common, a recent analysis of the treatment of patients with MLKI reported that staged procedures were used for 5.8% of cases, particularly in injuries that involved both medial and lateral-sided injuries. Most commonly, surgical treatment of the peripheral structures was performed during the initial surgery followed by the central structures later [5]. This is often seen in patients with acute bony injuries in which treatment of the medial or lateral-sided injury is performed acutely to ensure the ability to repair fracture fragments or in the setting of acute meniscal injuries that require reduction. Furthermore, this two-stage technique may be chosen in patients who may not be stable or medially cleared to undergo an MLKI reconstruction procedure. A recent study compared matched patients who underwent one-stage and two-stage surgical procedure in the treatment of MLKI involving the posterolateral corner found no difference in patient reported outcome scores (Lysholm or the International Knee Documentation Committee (IKDC)). However, there was an increase in patients who developed stiffness requiring manipulation under anesthesia in the group of patients that had a one-stage procedure [27]. Given that staging can occur for multiple reasons including injury characteristics such as concomitant injuries or severity of injury, it is difficult to generalize these findings to all patients with MLKIs.
Surgical Technique
Repair vs. Reconstruction
The decision to repair versus reconstruct (or augment with reconstruction and repair) in the context of MLKI is unique to the specific injury pattern and often timing between injury and presentation for evaluation. In general, cruciate ligament injuries are typically treated with reconstruction and acute bony avulsions should be repaired acutely if possible. With respect to medial-sided injuries, MCL and PMC injuries have shown good outcomes with both repair and reconstruction with no overwhelming evidence suggesting the superiority of one technique over the other [28]. A recent review of 24 patients with KDIII-M injuries with a follow-up of over 6 years found that repair of medial-sided structures was a negative predictor for IKDC or Lysholm scores post-operatively [29]. However, other studies have demonstrated that having an MCL reconstruction compared to a repair was a significant risk factor for both IKDC and Lysholm scores being less than or equal to 75 [30]. This lack of consensus suggests that decision-making should be individualized for each patient and specific injury. It is the author’s preference to repair the MCL when able and to restore the native anatomy. If the remaining tissue is of poor quality or too encased in scar tissue to repair, then augmentation or reconstruction is performed. If in addition to valgus instability, the patient has anteromedial rotatory instability, the MCL in addition to the PMC structures should also be repaired or reconstructed with several techniques described [7, 14].
With respect to lateral-sided injuries of the LCL and PLC, literature has supported reconstruction over repair in the context of MLKIs. In a consensus statement of international PLC experts published in 2019, anatomic posterolateral corner reconstruction was the preferred technique with repair of the primary PLC structures (LCL/popliteus tendon) being recommended in the context of bony avulsion injuries [31]. In a recent systematic review of 12 studies and 288 patients, an overall failure rate of 12.4% was observed with surgical failure significantly higher in patients undergoing repair (21.9%) compared to reconstruction (7.1%) [32]. There are several described reconstruction options for PLC injuries with the two most common variations being fibular based reconstruction with a single graft and a two-tailed reconstruction with one limb recreating the function of the LCL and the other the popliteus. There is no evidence of one technique being superior [33, 34].
Postoperative Rehabilitation
The current evidence on postoperative rehabilitation is inconclusive, as the literature is divided between early and delayed rehabilitation without clear recommendations favoring one over the other. However, the ongoing ‘STaR trial’ seeks to address this question. The study includes two arms, with one specifically designed to provide evidence on the timing of postoperative rehabilitation. The postoperative rehabilitation includes general brace use, at least during the first six weeks following the surgery. No hyperextension is allowed until six weeks postoperatively. Furthermore, no active hamstring contraction is allowed until eight weeks postoperatively if either the PCL or posterior capsule is injured.
Early rehabilitation is initiated after the first postoperative visit, with weight bearing as tolerated and unrestricted range of motion in a brace. However, it is important to be aware that this protocol is not an ‘accelerated protocol’ as no overpressure, end-rage stretching/mobilization, or painful weight bearing is allowed. During the first postoperative week, patients are advised to wear a brace locked in extension with a non-weight bearing gait and crutches. Seven to ten days postoperative, flexion range of motion and weight bearing are allowed to tolerance depending on the type of injury (Table 2.) Toward the four weeks postoperatively, the knee range of motion is allowed to be between 0 and 45 degrees. If more than ten degrees of flexion contracture remains at the six-week postoperative mark, patients are advised to contact their surgeon. In contrast, delayed rehabilitation is initiated four weeks after surgery, thus, patients are advised to wear a brace locked in extension with a non-weight-bearing gait without any joint motion during the first four postoperative weeks.
Table 2.
Tissue-specific Rehabilitation modifications (STaR trial)
| Tissue | Rehabilitation Modifications |
|---|---|
| ACL | • No modifications |
| PCL |
• Protect posterior translation of the tibia for 6 weeks • No active hamstring contraction for 8 weeks |
| PLC |
• Follow PCL rehab modifications • Avoid rotation and varus stress for 6 weeks (minimum) • Avoid passive hyperextension beyond 0 degrees of extension (8 weeks) |
| MCL |
• Perform ROM exercises with foot internally rotated • Avoid excessive valgus forces (8 weeks) • Protect hyperextension if the capsule is involved (8 weeks) |
| Meniscus Root/Body Repair |
• Brace locked in extension for 4 weeks, WBAT • Avoid WB flexion for 4 weeks • Limit NWB flexion ROM to 90 degrees for 4 weeks • No active hamstring contraction for 8 weeks for meniscus repairs |
ACL: Anterior cruciate ligament; MCL: Medial collateral ligament; PCL: Posterior cruciate ligament; PLC: Posterolateral corner; NWB: Non-weight bearing; ROM: Range of motion; WB: Weight bearing; WBAT: Weight bearing as tolerated
Post-Operative Outcomes
Previous literature has reported a higher percentage of excellent or good IKDC scores in surgically treated patients compared to those undergoing nonsurgical treatment (58% vs. 20%) [7]. Furthermore, higher rates of return to work and sport have been associated with surgical treatment [21]. Thus, 72% and 29% of patients undergoing surgical treatment for their MLKI have been reported to return to work and sports, respectively, while only 52% and 10% of patients treated with nonsurgical treatment are able to return to work and sports, respectively [7]. Similar to nonsurgical treatment, repair has been associated with inferior postoperative outcomes compared to reconstruction, as decreased stability, range of motion and lower rates of return to play following repair compared to reconstruction have been demonstrated (0% vs. 33%) [7]. Furthermore, a higher failure rate following PLC surgery was reported in those undergoing repair vs. reconstruction (37% vs. 9%).
The concomitant injuries along with MLKIs have also been shown to correlate with inferior postoperative outcomes. While overall return to any work rates after surgical treatment of MLKI vary widely and are patient- and injury-specific, some research has reported rates as high as 80%. [21] It is also important to note that while some individuals may return to work, they may not reengage in the same level of functional demand or duty. Finally, 23% of patients treated for combined ACL, PCL, medial and/or lateral injuries have been demonstrated to sustain generative joint disease [35] impacting their later knee function and subsequent quality of life.
Complications
The MLKIs can have limb-threatening complications even prior to any surgical intervention, such as nerve or vascular injuries with an incidence of up to 40% [36]. Surgery is typically indicated for MLKIs, and there are multiple potential postoperative complications that occur more frequently after MLKI reconstruction or repair compared to when a single ligament is fixed. Common postoperative complications after multiligament knee reconstruction include wound infection requiring irrigation and debridement, arthrofibrosis requiring manipulation under anesthesia and/or lysis of adhesions, deep vein thrombosis (DVT), need for removal of hardware, and revision ligament surgery for graft failure [37].
A retrospective case-control study of 108 patients with MLKI who underwent reconstruction found that 29.6% of patients had at least one postoperative complication. In the group of patients sustaining complications, the rates for each complication were: 16.7% for arthrofibrosis, 6.5% for wound infection, 5.6% for revision ligament surgery, 4.6% requiring removal of hardware, and 1.8% for DVT [37]. In contrast, the overall postoperative risk of arthrofibrosis and wound infection requiring intervention for isolated ACL reconstruction is reported to be 2% and 1%, respectively [38, 39]. The authors also found that smoking and planned staged surgery significantly increased the overall complication risk, while increased length of time from injury to surgery significantly decreased this risk [37].
A systematic review examining 36 studies with 4,159 patients who underwent MLKI surgery identified a postoperative stiffness rate of 9.8%. The authors found that the risk of postoperative stiffness was significantly lower for patients with 2 injured ligaments compared to ≥3 ligaments, and early surgery (< 3 weeks) had significantly increased odds of postoperative stiffness compared to delayed surgery (≥3 weeks) [40]. Regarding the timing of surgery, there are many confounding factors that may contribute to the incidence of stiffness with early or delayed surgery. To better answer the question of ideal surgical timing for MLKIs without retrospective bias, a multicenter randomized clinical trial is currently underway comparing early versus delayed surgery and postoperative rehabilitation after MLKI [41].
Conclusion
The MLKIs are often associated with knee dislocation and constitute a highly complex entity. Common concomitant neurovascular, meniscal, and cartilaginous injuries necessitate comprehensive and vigilant management. Usual treatment aims to either repair or reconstruct the injured ligaments, however, there is no general consensus on the timing of surgery or rehabilitation following surgery for MLKIs. Our review stresses the need for more high-level research to address the paucity of evidence-based treatment guidelines for these complex injuries to ultimately improve outcomes for patients.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Author Contributions
All listed authors have contributed substantially to this work: literature search and initial manuscript preparation were performed by ZJH, JK, AMW, and AL. NAA, BPL, JJI, and VM assisted with editing and finalizing the manuscript. All authors have read and approved the final manuscript to be submitted and published.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing Interests
The authors declare the following potential conflicts of interest or sources of funding: BPL received payment from Mid-Atlantic Surgical Systems, LLC for education. JJI is President of the Board of Directors for the Journal of Orthopaedic and Sports Physical Therapy (JOSPT). VM received consulting fees from Smith & Nephew and Newclip, educational fees from Arthrex, DePuy Synthesis, and Conmed, and is a board member of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS), and the Assistant editor-in-chief of Knee Surgery, Sports Traumatology, Arthroscopy (KSSTA). Also, VM has a patent, U.S. Patent No. 9,949,684, issued on April 24, 2018, to the University of Pittsburgh.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neri T, Myat D, Beach A, Parker DA. Multiligament knee Injury: Injury patterns, outcomes, and Gait Analysis. Clin Sports Med. 2019;38(2):235–46. [DOI] [PubMed] [Google Scholar]
- 2.Werner BC, Gwathmey FW Jr., Higgins ST, Hart JM, Miller MD. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med. 2014;42(2):358–63. [DOI] [PubMed] [Google Scholar]
- 3.Schenck R. Classification of knee dislocations. In: The multiple ligament injured knee: a practical guide to management edn. Edited by Fanelli G. New York, NY: Springer; 2004: 37–49.
- 4.Moore TM. Fracture–dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–40. [PubMed] [Google Scholar]
- 5.**Poploski KM, Lynch AD, Burns TC, Harner CD, Levy BA, Owens BD, Richter DL, Schenck RC Jr., Musahl V, Irrgang JJ. Presentation and Surgical Management of Multiple Ligament Knee Injuries: A Multicenter Study from the Surgical Timing and Rehabilitation (STaR) Trial for MLKIs Network. J Bone Joint Surg Am 2023, 105(8):607–613.: Multi-center study with a total of 773 individuals from 14 centers who underwent surgery for MLKI reporting on clinical characteristics, injury patterns, concomitant injuries and method of surgical intervention. [DOI] [PubMed]
- 6.**Boos AM, Wang AS, Hevesi M, Krych AJ, Stuart MJ, Levy BA. Long-term Outcomes After Surgical Reconstruction of Multiligamentous Knee Injuries: Results at Minimum 10-Year Follow-up. Orthop J Sports Med 2024, 12(1):23259671231223188. Case series including 55 knees who underwent surgical reconstruction for MLKI at a mean follow-up of 15 ± 5 years with overall satisfactory mean PRO scores. [DOI] [PMC free article] [PubMed]
- 7.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–8. [DOI] [PubMed] [Google Scholar]
- 8.Kim SH, Park YB, Kim BS, Lee DH, Pujol N. Incidence of Associated Lesions of Multiligament Knee Injuries: a systematic review and Meta-analysis. Orthop J Sports Med. 2021;9(6):23259671211010409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zsidai B, Horvath A, Winkler PW, Narup E, Kaarre J, Svantesson E, Musahl V, Hamrin Senorski E, Samuelsson K. Different injury patterns exist among patients undergoing operative treatment of isolated PCL, combined PCL/ACL, and isolated ACL injuries: a study from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2022;30(10):3451–60. Cohort study based on Swedish registry data comprising a total of 45,564 individuals who underwent either isolated reconstruction of PCL or ACL, or both. The level III study reports on injury mechanism and concomittant injuries. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2–8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):739–49. [DOI] [PubMed] [Google Scholar]
- 11.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical Management of knee dislocations. JBJS 2004, 86(2). [DOI] [PubMed]
- 12.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy: J Arthroscopic Relat Surg. 2009;25(4):430–8. [DOI] [PubMed] [Google Scholar]
- 13.Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2011;42(11):1198–204. [DOI] [PubMed] [Google Scholar]
- 14.Ng JWG, Myint Y, Ali FM. Management of multiligament knee injuries. EFORT Open Rev. 2020;5(3):145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seroyer ST, Musahl V, Harner CD. Management of the acute knee dislocation: the Pittsburgh experience. Injury. 2008;39(7):710–8. [DOI] [PubMed] [Google Scholar]
- 16.*Makaram NS, Murray IR, Geeslin AG, Chahla J, Moatshe G, LaPrade RF. Diagnosis and treatment strategies of the multiligament injured knee: a scoping review. Br J Sports Med 2023, 57(9):543–550. Scoping review including 417 studies on diagnosis and treatment of multiligament knee injuries, showing insufficient high-level evidence to support definitive management strategies for MLKI. [DOI] [PubMed]
- 17.Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations: a meta-analysis. Am J Knee Surg. 2001;14(1):33–8. [PubMed] [Google Scholar]
- 18.Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev. 2011;19(2):167–73. [DOI] [PubMed] [Google Scholar]
- 19.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30(5):718–27. [DOI] [PubMed] [Google Scholar]
- 20.Wong CH, Tan JL, Chang HC, Khin LW, Low CO. Knee dislocations-a retrospective study comparing operative versus closed immobilization treatment outcomes. Knee Surg Sports Traumatol Arthrosc. 2004;12(6):540–4. [DOI] [PubMed] [Google Scholar]
- 21.Everhart JS, Du A, Chalasani R, Kirven JC, Magnussen RA, Flanigan DC. Return to work or Sport after Multiligament knee Injury: a systematic review of 21 studies and 524 patients. Arthroscopy. 2018;34(5):1708–16. [DOI] [PubMed] [Google Scholar]
- 22.Moatshe G, Chahla J, LaPrade RF, Engebretsen L. Diagnosis and treatment of multiligament knee injury: state of the art. J ISAKOS. 2017;2(3):152–61. [Google Scholar]
- 23.Hohmann E, Glatt V, Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: a systematic review and meta-analysis. Knee. 2017;24(5):909–16. [DOI] [PubMed] [Google Scholar]
- 24.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2–9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1013–26. [DOI] [PubMed] [Google Scholar]
- 25.Ohkoshi Y, Nagasaki S, Shibata N, Yamamoto K, Hashimoto T, Yamane S. Two-stage reconstruction with autografts for knee dislocations. Clin Orthop Relat Res. 2002;398:169–75. [DOI] [PubMed] [Google Scholar]
- 26.Harner CD, Irrgang JJ, Paul J, Dearwater S, Fu FH. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20(5):499–506. [DOI] [PubMed] [Google Scholar]
- 27.Freychet B, Kennedy NI, Sanders TL, Levy NM, Leland DP, Krych AJ, Stuart MJ, Levy BA. No difference between single and staged posterolateral corner surgical procedures in the multiligament injured/dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2170–6. [DOI] [PubMed] [Google Scholar]
- 28.Kovachevich R, Shah JP, Arens AM, Stuart MJ, Dahm DL, Levy BA. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):823–9. [DOI] [PubMed] [Google Scholar]
- 29.King AH, Krych AJ, Prince MR, Pareek A, Stuart MJ, Levy BA. Surgical outcomes of Medial Versus lateral Multiligament-Injured, dislocated knees. Arthroscopy. 2016;32(9):1814–9. [DOI] [PubMed] [Google Scholar]
- 30.Hanley JM, Anthony CA, DeMik D, Glass N, Amendola A, Wolf BR, Bollier M. Patient-reported outcomes after multiligament knee Injury: MCL repair Versus Reconstruction. Orthop J Sports Med. 2017;5(3):2325967117694818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chahla J, Murray IR, Robinson J, Lagae K, Margheritini F, Fritsch B, Leyes M, Barenius B, Pujol N, Engebretsen L, et al. Posterolateral corner of the knee: an expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2520–9. [DOI] [PubMed] [Google Scholar]
- 32.Fortier LM, Knapik DM, Condon JJ, DeWald D, Khan Z, Kerzner B, Matava MJ, LaPrade R, Chahla J. Higher success rate observed in reconstruction techniques of acute posterolateral corner knee injuries as compared to repair: an updated systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5565–78. [DOI] [PubMed] [Google Scholar]
- 33.LaPrade RF, Johansen S, Agel J, Risberg MA, Moksnes H, Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92(1):16–22. [DOI] [PubMed] [Google Scholar]
- 34.LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32(6):1405–14. [DOI] [PubMed] [Google Scholar]
- 35.Fanelli GC, Sousa PL, Edson CJ. Long-term followup of surgically treated knee dislocations: stability restored, but arthritis is common. Clin Orthop Relat Res. 2014;472(9):2712–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.*Constantinescu D, Luxenburg D, Syros A, Bondar KJ, Barnhill S, Vanden Berge D, Vilella-Hernandez F. Vascular Injury After Knee Dislocation: A Meta-Analysis Update. J Am Acad Orthop Surg 2023, 31(4):e198-e206. A meta-analysis update on the clinical implications of knee dislocations including frequency of vascular injury, amputation, and nerve injuries; reporting an increased prevalence of KD1 and lateral KDs to previous literature and a rate of 62.2% of surgical repair in those patients with concomitant vascular injuries. [DOI] [PubMed]
- 37.Patel NK, Lian J, Nickoli M, Vaswani R, Irrgang JJ, Lesniak BP, Musahl V. Risk factors Associated with complications after Operative Treatment of Multiligament knee Injury. Orthop J Sports Med. 2021;9(3):2325967121994203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ. Procedural intervention for arthrofibrosis after ACL reconstruction: trends over two decades. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):532–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao D, Liang GH, Pan JK, Zeng LF, Luo MH, Huang HT, Han YH, Lin FZ, Xu NJ, Yang WY, et al. Risk factors for postoperative surgical site infections after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2023;57(2):118–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ozbek EA, Dadoo S, Grandberg C, Runer A, Cong T, Hughes JD, Irrgang JJ, Musahl V. Early surgery and number of injured ligaments are associated with postoperative stiffness following multi-ligament knee injury surgery: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023;31(10):4448–57. A systematic review and meta-analysis of 36 studies, reporting 9.8% of stiffness after multi-ligament knee injury surgery with early surgery (< 3 weeks) resulting in significantly increased odds of postoperative stiffness compared with delayed surgery (>= 3 weeks). [DOI] [PubMed] [Google Scholar]
- 41.Poploski KM, Lynch AD, Burns TC, Harner CD, Levy BA, Owens BD, Richter DL, Schenck RC Jr., Musahl V, Irrgang JJ, et al. Presentation and Surgical Management of multiple ligament knee injuries: a Multicenter Study from the Surgical timing and Rehabilitation (STaR) trial for MLKIs Network. J Bone Joint Surg Am. 2023;105(8):607–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.