Abstract
Hemiconvulsion-hemiplegia-epilepsy syndrome is a rare and severe neurological condition that results from prolonged status epilepticus in infancy and early childhood. This syndrome is characterized by unilateral prolonged seizures, primarily clonic in nature, which are followed by transient or permanent ipsilateral hemiplegia. In this report, we present the case of a 3-year-old girl who exhibited persistent left hemiparesis after experiencing an episode of prolonged focal seizures at the age of 2 years. Comprehensive neurological evaluation and brain MRI conducted in our department confirmed the diagnosis of hemiconvulsion-hemiplegia-epilepsy syndrome in its chronic phase.
Keywords: Hemiconvulsion, Hemiplegia, Epilepsy, Status epilepticus, MRI
Introduction
Hemiconvulsion-Hemiplegia-Epilepsy (HHE) syndrome is a distinct and rare epilepsy syndrome that predominantly affects children. It was first described by the French neurologist Henri Jean Pascal Gastaut et al. in 1960 [1]. HHE is characterized by a triad: prolonged unilateral convulsions, followed by transient or permanent hemiplegia of varying intensity, and the subsequent development of partial epilepsy. The etiology and underlying mechanisms of this condition remain to be fully understood. Radiological imaging plays a crucial role in the diagnosis and management of HHE syndrome, with Magnetic Resonance Imaging (MRI) being the preferred modality.
We describe the case of a 3-year-old child who was referred to our department for a brain MRI as part of the etiological work-up for epilepsy associated with left hemiparesis. Based on the clinical presentation and brain MRI findings, the diagnosis of HHE syndrome was made.
Case report
A 3-year-old girl, the second child of nonconsanguineous healthy parents with no significant antenatal issues and normal developmental milestone. At the age of 2 years, she experienced an episode of prolonged focal seizures affecting the left side of her body, which was managed with multiple antiepileptics at another hospital. Following these seizures, she developed weakness in her left upper and lower limbs, which persisted after discharge. She remained seizure-free on maintenance antiepileptic therapy (sodium valproate). She was referred to our department for evaluation of ongoing hemiparesis and psychomotor retardation.
On examination, her weight and height were within the normal range for her age. Neurological examination revealed spastic left hemiparesis and delayed motor milestones. Examination of other systems was unremarkable.
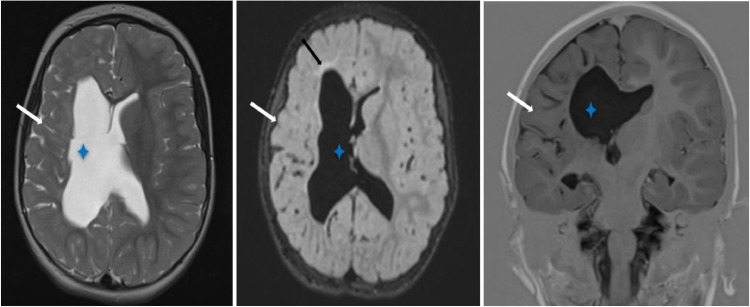
Magnetic resonance imaging of the brain (Fig. 1) showed generalized atrophy of the entire right cerebral hemisphere with homolateral ventricular dilatation and high signal hyperintensity of the subcortical white matter indicating gliosis.
Fig. 1.
T2-weighted, FLAIR, and TIR sequences (axial and coronal images) demonstrate generalized atrophy of the entire right cerebral hemisphere (white arrow), accompanied by ipsilateral ventricular ex vacuo dilatation (asterisk) and high signal hyperintensity of the subcortical white matter indicative of gliosis (black arrow).
Based on the clinical presentation, the patient's age, and the brain MRI findings the diagnosis of hemiconvulsion-hemiplegia-epilepsy syndrome was made.
Antiepileptic treatment with sodium valproate has been consistently maintained. Additionally, a comprehensive rehabilitation program was initiated shortly after the diagnosis, focusing on improving motor function and cognitive abilities with regular assessments planned every 3 months.
Discussion
HHE syndrome is a rare epileptic encephalopathy that follows prolonged status epilepticus in infancy and early childhood [2]. It is characterized by prolonged hemiclonic seizures, often occurring in the presence of fever. These seizures are followed by the development of transient or permanent hemiplegia. Subsequently, partial epilepsy commonly manifests [1].
HHE syndrome appears to be relatively uncommon, with precise prevalence and incidence rates remaining unknown. However, it has been reported to be declining in developed countries. This decline may be attributed to improved and quicker treatment of status epilepticus, especially the abortive treatments with benzodiazepines and increased rates of childhood immunizations, which reduce febrile status epilepticus [3].
The exact pathophysiology of HHE remains unclear. Several factors contribute to its pathogenesis [1]. Prolonged seizures can impair neuronal energy metabolism and cause excitotoxic cell injury. Inflammation and prolonged ictal activity affect blood-brain barrier permeability, exacerbating cell injury. Additionally, predisposing factors such as genetic influences and focal epileptogenic lesions have been suggested as potential underlying mechanisms.
Two primary forms of HHE syndrome have been recognized. Type I, the symptomatic form, often occurs after febrile seizures associated with acute cerebral disorders such as meningitis, encephalitis, head trauma, subdural hematoma, focal cortical dysplasia type IIID, and cerebral vascular disease [4]. This form typically presents with an earlier onset of epilepsy, which is of a symptomatic generalized type. Type II, the idiopathic form, is characterized by idiopathic status epilepticus, which subsequently leads to temporal lobe epilepsy [5].
Clinically, HHE syndrome typically presents in 3 stages:
-
1.
Hemiconvulsions: The initial stage involves prolonged (hours), unilateral clonic seizures. These convulsions often last for hours and may be resistant to conventional antiepileptic medications. The onset usually occurs in the first 2 years of life, often preceded by a febrile episode.
-
2.
Hemiplegia: Ipsilateral and occurring immediately following hemiconvulsions. The severity of hemiplegia can vary, often being profound. It may be transient, with full recovery within 1 to 12 months, or permanent.
-
3.
Epilepsy: The third stage is characterized by the onset of epilepsy, which typically develops months to years after the initial hemiconvulsions. The seizures are often complex and partial originating from the temporal lobe [1].
Radiological imaging plays a crucial role in the diagnosis and management of HHE syndrome. MRI is the preferred modality due to its superior ability to characterize brain parenchyma and detect subtle changes that occur in the course of the syndrome. In the early stages of HHE syndrome, MRI typically reveals T2 and DWI hyperintensity with a decreased apparent diffusion coefficient (ADC), predominantly affecting the subcortical white matter of the affected hemisphere with normal vascular imaging. These findings are indicative of cytotoxic edema [5]. Furthermore, some cases of HHE syndrome have reported additional involvement of the basal ganglia and hippocampus [6], suggesting that the pathophysiological impact of the syndrome can extend beyond the subcortical white matter. During the subacute phase which occurs 8-30 days post status epilepticus, progressive atrophy of the affected hemisphere is observed, accompanied by hyperintense signals on T2-weighted and FLAIR images due to gliosis. In the chronic phase, which extends beyond 3 months post status epilepticus, the MRI findings become more pronounced. There is marked atrophy affecting both the cortical and subcortical regions of the entire hemisphere, reflecting significant neuronal loss and brain volume reduction. This extensive atrophy is often accompanied by dilatation of the ventricular system.
EEG remains valuable in the diagnostic approach. During the critical phase, it typically shows asymmetric high-voltage, rhythmic slow waves (2-3 Hz), which are often bilateral but more pronounced in the hemisphere contralateral to the clinical crisis [7]. Following the prolonged seizure, there is a subsequent appearance of slow waves and spikes, followed by delta slowing with increased amplitude observed on the affected hemisphere [1].
In the early stages of HHE syndrome, the main differential diagnosis on imaging includes stroke, which can be distinguished by the presence of abnormalities that are not confined to a specific vascular territory and by normal findings on angio-MRI.
At the hemi-atrophy stage, differential diagnosis should consider other potential causes of cerebral hemi-atrophy, particularly:
-
•
Dyke-Davidoff-Masson Syndrome: characterized by cerebral hemi-atrophy along with ipsilateral calvarial thickening and hyper-pneumatization of paranasal air sinuses.
-
•
Sturge-Weber syndrome: involves cerebral hemi-atrophy typically localized to the parieto-occipital area, often accompanied by ipsilateral enlargement of the choroid plexus and prominent leptomeningeal enhancement.
-
•
Rasmussen encephalitis: initial atrophy is typically observed in the ipsilateral caudate nucleus, followed by more generalized hemisphere atrophy and signal changes.
The treatment of HHE syndrome primarily involves medical management aimed at controlling seizures, as there is no curative treatment for the condition. Carbamazepine and/or phenobarbitone have shown efficacy in seizure management [8]. For refractory cases, surgical interventions such as hemispherectomy and corpus callosotomy have been successful [9].
Conclusion
Hemiconvulsion-Hemiplegia-Epilepsy syndrome is a rare and severe neurological disorder that can greatly impact the quality of life for patients and their families. Radiological imaging, particularly MRI, is essential for diagnosis. Early recognition and aggressive seizure management are critical to reducing long-term neurological consequences. Further research is needed to enhance our understanding of HHE syndrome's pathophysiology and to develop more effective treatment strategies.
Patient consent
Written informed consent for the publication of this case report was obtained from the parents of the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Auvin S., Bellavoine V., Merdariu D., Delanoë C., Elmaleh-Bergés M., Gressens P., et al. Hemiconvulsion–hemiplegia–epilepsy syndrome: current understandings. Eur J Paediatr Neurol. 2012;16(5):413–421. doi: 10.1016/j.ejpn.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Sudan TS, Vinayan KP, Roy AG. Clinical, MRI and electrographic characteristics of three children with hemiconvulsion-hemiplegia/hemiconvulsion-hemiplegia-epilepsy (HH/HHE) syndrome - A rare childhood epileptic encephalopathy. Int J Epilepsy. 2017;4:79–86. doi: 10.1016/j.ijep.2016.12.004. [DOI] [Google Scholar]
- 3.Tenney JR, Schapiro MB. Child neurology: hemiconvulsion-hemiplegia-epilepsy syndrome. Neurology. 2012;79(1):e1–e4. doi: 10.1212/WNL.0b013e31825dce5f. [DOI] [PubMed] [Google Scholar]
- 4.Itamura S, Okanishi T, Arai Y, Nishimura M, Baba S, Ichikawa N, et al. Three cases of Hemiconvulsion-Hemiplegia-Epilepsy syndrome with focal cortical dysplasia type IIId. Front Neurol. 2019;10:1233. doi: 10.3389/fneur.2019.01233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toldo I, Calderone M, Boniver C, Dravet CH, Gerrini R, Laverda AM. Hemiconvulsion-hemiplej ia-epilepsiy syndrome: early magnetic resonance imaging inding and neuroradiological follow-up. Brain Dev. 2007;29:109–111. doi: 10.1016/j.braindev.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Barcia G, Desguerre I, Carmona O, Barnerias C, Chemaly N, Gitiaux C, et al. Hemiconvulsion-hemiplegia syndrome revisited: longitudinal MRI findings in 10 children. Dev Med Child Neurol. 2013;55(12):1150–1158. doi: 10.1111/dmcn.12233. [DOI] [PubMed] [Google Scholar]
- 7.Salafia S, Praticò AD, Pizzo E, Greco F, Di Bella D. Hemiconvulsion-hemiplegia-epilepsy syndrome. Magnetic resonance findings in a 3-year-old boy. Neurol Neurochir Pol. 2013;47(6):584–589. doi: 10.5114/ninp.2013.39076. [DOI] [PubMed] [Google Scholar]
- 8.Bhat RY, Kakkar S, Prakashini K. Hemiconvulsion-hemiplegia-epilepsy syndrome: clinical course and neuroradiological features in a 20-month-old girl. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-203482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holland KD, Buchhalter J. Hemiconvulsion-hemiplegia-epilepsy syndrome: another case for epilepsy surgery. Neurology. 2008;70(22 Pt 2):2097–2098. doi: 10.1212/01.wnl.0000313159.55530.e8. [DOI] [PubMed] [Google Scholar]