Summary
Bangladesh reduced malaria incidence by 93% from 2008 to 2020 through the action of governmental and non-governmental organizations. The Bangladesh context is unique to South Asia because its successful public sector malaria control programs have historically not engaged corporate partners (as undertaken in Sri Lanka and proposed in India). However, ∼18 million people continue to live at risk of infection in Bangladesh and for-profit private healthcare providers, catalytic for malaria elimination in many countries, are expected to benefit the national program. We distilled (from a large and complex literature) nine distinct strategies important in other developing settings and weighed them in the context of Bangladesh's flourishing private health care sector, driven by patient demand, self-interest and aspirations for public good, as well as heterogeneity in providers and malaria-prevalence. We propose a new model dependent on five strategies and its immediate deployment considerations in high endemic areas, to empower Bangladesh's phased agenda of eliminating indigenous malaria transmission by 2030.
Keywords: Malaria elimination, Bangladesh, Chittagong hill tracts, Malaria, Private sector engagement, Public health, Health policy
Introduction
Among the remaining malaria-endemic countries, Bangladesh has experienced remarkable recent success in the control of malaria. In 2008, the National Malaria Elimination Program (NMEP) and a consortium of NGOs headed by the Bangladesh Rural Advancement Committee (BRAC) redoubled malaria control efforts within the country, combining the mass distribution of long-lasting insecticide nets (LLINs) to reduce bites from malaria-transmitting mosquitos, in–home review of appropriate net use, rapid point-of-care diagnosis, and prompt treatment with frontline artemisinin-based combination treatments (ACTs; Fig. 1).1 This strategy has allowed the country to achieve near-elimination status in 8 of its 13 malaria-endemic regions (Fig. 2a and b)1; likewise, malaria case and death rates within the country decreased up to 2020 (Fig. 2c).1 This rapid progress prompted Bangladesh to set the ambitious target date of 2030 for the scaled elimination of malaria from the country.
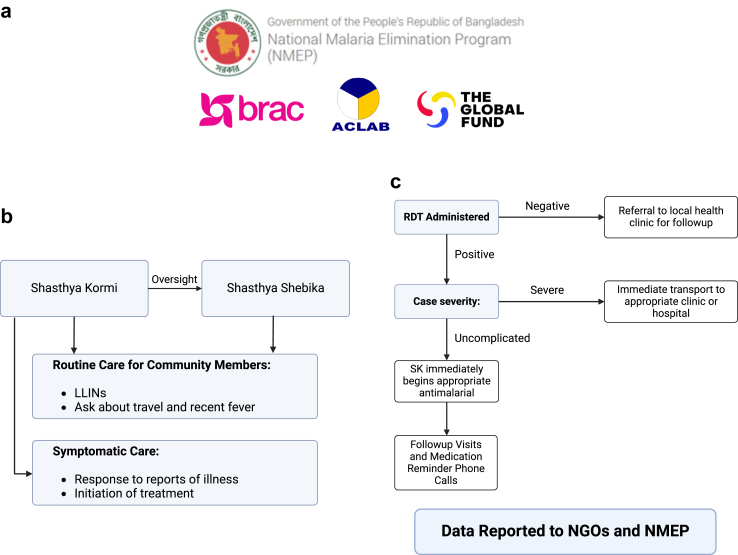
Fig. 1.
Malaria Elimination in Bangladesh. a) Supported by the Global Fund, the Govt of Bangladesh's National Malaria Elimination Program (NMEP) works in conjunction with the NGO BRAC as well as others such as ACLAB (Alliance for Cooperation and Legal Aid Bangladesh). b) Most elimination interventions are carried out at the community members by Shastya Kormi (SK) and Shasthya Shebika (SS). Shasthya Kormi are paid, trained, high-school graduate, female health care community supervisors, who both directly visit community members and oversee multiple SS. Shasthya Shebika have less training and provide only routine care, such as counseling on the use and maintenance of long-lasting insecticide nets (LLINs) and querying about recent travel or fever. LLINs are widely issued to prevent mosquito biting at night or rest periods. Proper numbers and usage are also gauged during routine visits. c) Reports of fever over the prior 24–48 h are rapidly followed up by an in–home RDT. If negative, affected individuals are given a written referral to a local health clinic for further follow up. Severe patients are immediately sent to a suitable clinic or hospital. Patients positive for P. falciparum or P. vivax with uncomplicated malaria are directly started on appropriate antimalarial drug treatment by the SK. The SK keeps contact via cell phone at the times of all subsequent doses (∼8 h apart) to check on the patient and compliance. In addition, she visits in-person each day that the patient continues to be febrile. Conversely, febrile or otherwise-ill patients also directly call their SK for an immediate home visit, RDT, drug treatment and collection of clinical history and travel data. All this information as well as the spent RDTs are transferred to the NGO and NMEP. 80% of all malaria infections in Bangladesh are identified by SK's or Sasthya Sebikas (who report to SK's and do not administer antimalarial drugs unsupervised). The result is high-quality, accountable, patient-centered care, with collation of rich natural history data at a national scale to inform the malaria elimination agenda, as well as empowerment of community health workers who are aware of the central role they play in Bangladesh's success in diminishing malaria as well as supporting the general health of their communities. Created in BioRender. Mcardle, R. (2022) BioRender.com/m21q149.
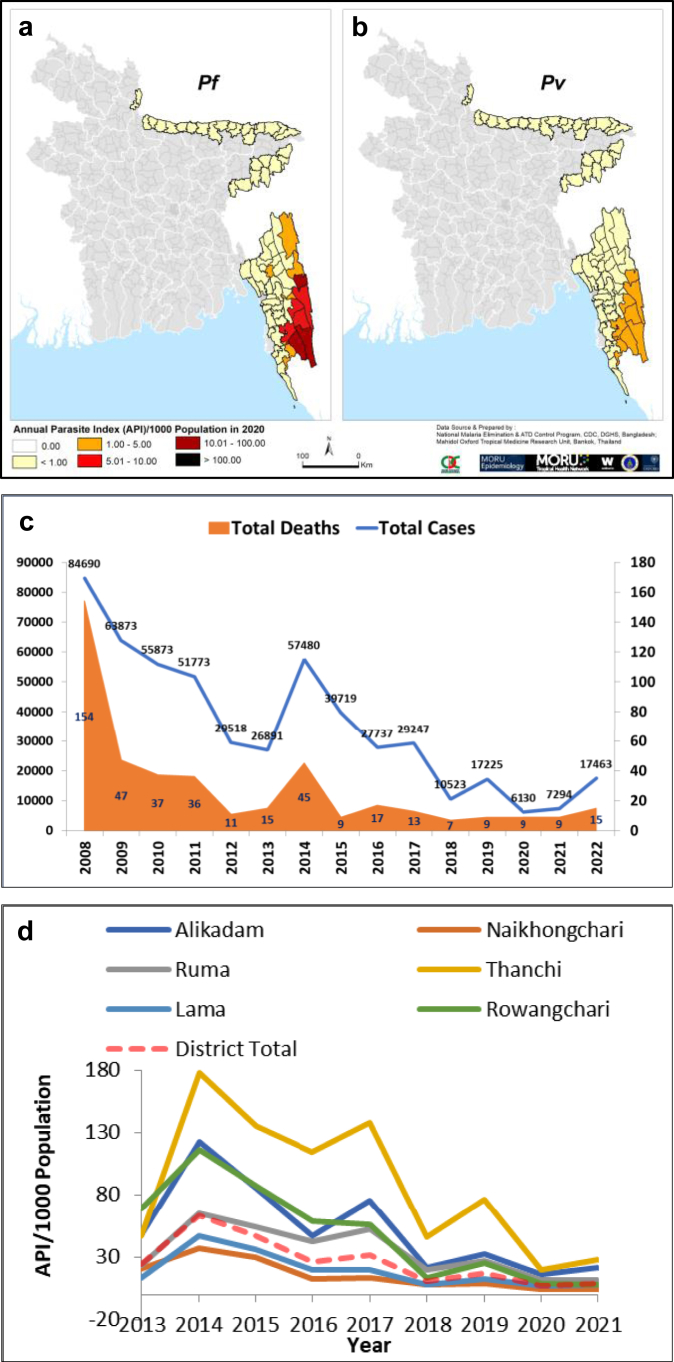
Fig. 2.
Dynamics of malaria control in Bangladesh. a-b, Map for phased malaria elimination by 2030 in Bangladesh for P. falciparum (Pf) and P. vivax (Pv). Regions marked in (i) red show high malaria levels seen in the CHT in the southeast, targeted for elimination by 2030; (ii) orange with intermediate levels are targeted for 2027; (iii) yellow with low levels are targeted for 2025; c, Malaria cases and deaths in Bangladesh 2008–2022; d, Annual Parasitological Index (API) 2013–2021 in sub-districts of Bandarban district which has the highest levels of malaria in the CHT. (All data are courtesy of the National Malaria Elimination Program, Govt of Bangladesh). From Haldar et al., 2023 Trends in Parasitol. 10.1016/j.pt.2023.06.009 using Creative Commons License.
However, several challenges persist. Transmission remains high in three districts (Bandarban, Rangamati, and Khagrachari) in the Chittagong Hill Tracts (CHTs; Fig. 2a and b), a region which in 2021 and 2022 showed increases in malaria incidence (Fig. 2c and d), posing significant challenges for continued elimination efforts.1 Care in the CHT districts is complicated by remote settlements of Indigenous (non-Bengali) peoples which are poorly served by roads and transportation.2 In contrast, two low-endemic districts, Cox's Bazar and Chittagong, are more accessible to present control efforts but continue to face the prospect of imported malaria from the neighboring high-transmission CHT districts.3 Eight northeastern districts at near-elimination present only a few cases of malaria annually.
One important task for the malaria elimination program in Bangladesh is to better involve the for-profit private healthcare sector into malaria elimination efforts. Data suggests that the private sector represents over 97% of all healthcare available in some endemic areas, and NMEP estimates show that around 20% of malaria patients still utilize the private sector (see Fig. 1). While malaria is a notifiable disease in Bangladesh, many PHPs (particularly in the high-endemic districts) are unaware of this fact, resulting in serious underreporting. This poses a barrier to WHO certification of malaria elimination, which requires proof of a comprehensive surveillance system. In addition, untrained private providers, who often prove difficult to regulate, have been shown to provide ineffective management of malaria cases in other developing settings,4 threatening to increase both malaria deaths and antimalarial resistance. Thus, in order to meet the 2030 target date for malaria elimination, malaria control efforts in Bangladesh will require robust private sector engagement (PSE), incorporating PHPs into existing surveillance networks, granting them the ability to aid in case detection, and requiring them to refer confirmed-positive cases to public treatment frameworks. This viewpoint collates and analyzes the strategies used for PSE elsewhere in the literature, weighing them in the context of challenges facing malaria elimination to develop a multi-modal plan to suggest the most promising path for PSE in Bangladesh.
The Bangladeshi private healthcare sector is large and heterogenous, comprising of both formal and informal providers. Formal providers (trained and registered through official government channels) include private hospitals, clinics and pharmacies. Informal providers, include untrained drug vendors, traditional healers such as religious, ayurvedic, and homeopathic therapists, and even formally-trained physicians who have unregistered clinics in addition to their public practice.5
PHPs in Bangladesh also face unique incentives which drive their behavior.6 They must compete with cheaper but often overcrowded public healthcare options. The for-profit private sector has competitive advantages in its high responsiveness to patient demand and strong personal relationships with patients. It also features a rich referral network, both from the public and private sectors. Referral fees are common practice. In summary, PHPs in Bangladesh are driven by a combination of internal and external factors including self-interest, patient demand, and, in some cases, concern for the public good.7
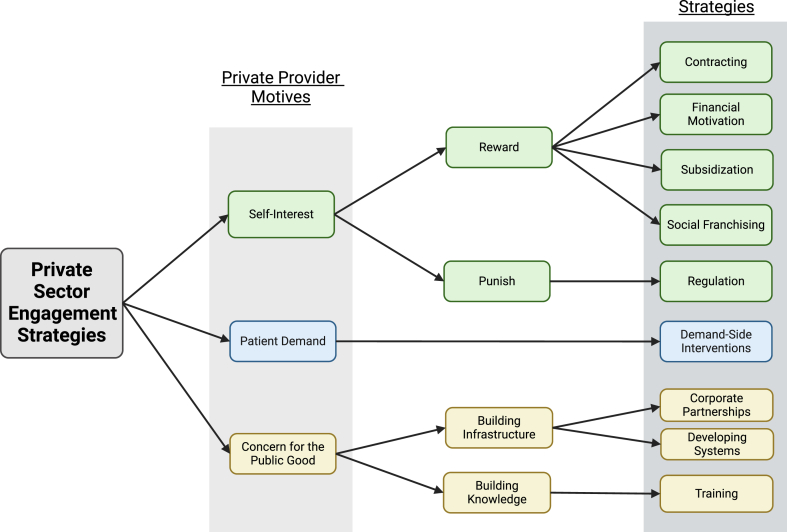
We have identified nine distinct strategies, connected by three primary motivators of Bangladeshi PHP behavior (Fig. 3).
-
1.
Contracting: Contracting represents the full employment of PHPs to perform certain duties. Bangladesh already features a comprehensive public system for malaria treatment except for in the CHTs (where no organizations which could be contracted exist), and thus contracting does not represent a promising strategy in its context.
-
2.
Financial motivation. Incentive payments (synonymous with “pay-for-performance”; P4P) are targeted financial rewards for specific activities and may increase the reporting of disease cases to centralized surveillance networks by as much as 84%.8, 9, 10, 11 Given the existing practice of referral fees, rewards may ensure compliance in Bangladesh.
-
3.
Regulation. Regulation functions by imposing legal punishments for noncompliance12 but regulatory strategies in developing settings face much weaker enforcement support.12, 13, 14 Although malaria is a public health notifiable disease in Bangladesh, regulation is undercut by poor enforcement networks, particularly in geographically remote malaria hotspots.
-
4.
Subsidization. Subsidization (i.e. provision to PHPs below market cost) of direct treatments (i.e. artemisinin combination therapies, or ACTs) has largely proven successful at increasing access to and use of ACTs.15 Rapid Diagnostic Test (RDT) subsidization has been less studied, although it does show some promise as a mechanism to reduce counterfeit tests.16
-
5.
Social franchising. Social franchising strategies offer PHPs both financial and other benefits (like increasing patient volume), but they increase prices and decrease access, and thus are unsuitable for rural settings.17,18 However, certification (by which PHPs gain endorsement for meeting standards)17 may be valuable in Bangladesh (as has been found elsewhere).14
-
6.
Demand-side interventions. Demand-side interventions, which seek to modify the healthcare-seeking behavior of patients, represent a promising solution to change the incentives, and thus the behavior, of PHPs.7,11,13 In aggregate they improve demand for health services, particularly when used in combination with other provider-facing strategies.9,17,19, 20, 21
-
7.
Corporate partnerships. Large corporations have inherent motivation to engage in healthcare programs: they benefit both directly from a healthier workforce and indirectly from the increased “social license” that arises from helping to tackle health issues in local communities.22 However the absence of large industry in the CHTs and low malaria burden elsewhere likely make corporate partnerships more challenging in Bangladesh.
-
8.
Developing systems. Beyond forging partnerships with large employers, efforts to strengthen material and social infrastructure must be considered foundational for all other PSE efforts. In Bangladesh, PSE programs require supply chain integration and the construction of novel data platforms for case reporting, and organizational support, such as forging strong connections with local leadership.8,21,23
-
9.
Training. PHPs oftentimes lack the skills and knowledge needed to successfully comply with public health mandates24: this also holds true in Bangladesh. Training seeks to fill these gaps, providing PHPs with the technical tools needed to aid in disease control efforts. Almost all commentators agree that training initiatives work best in combination with other strategies.5,11,13,24, 25, 26
Fig. 3.
Potential PSE Strategies for PHPs in Bangladesh. Based on a review of private sector engagement (PSE) in the literature (see Methods and Fig. 3), 9 potential strategies for PSE in the context of malaria elimination were revealed: contracting, financial motivation, subsidization, social franchising, regulation, demand-side interventions, corporate partnerships, developing systems, and training. A review of the Bangladeshi private healthcare sector revealed three primary motivators for private healthcare providers: provider self-interest, patient demand, and altruism (concern for patient good). Four mechanisms (reward, punish, building infrastructure, building knowledge) that connect strategies to motivation are also shown. Created in BioRender. Mcardle, R. (2023) BioRender.com/e78q521.
A full literature review and description of methods and results are provided in the Appendix in the Supplementary file.
Discussion
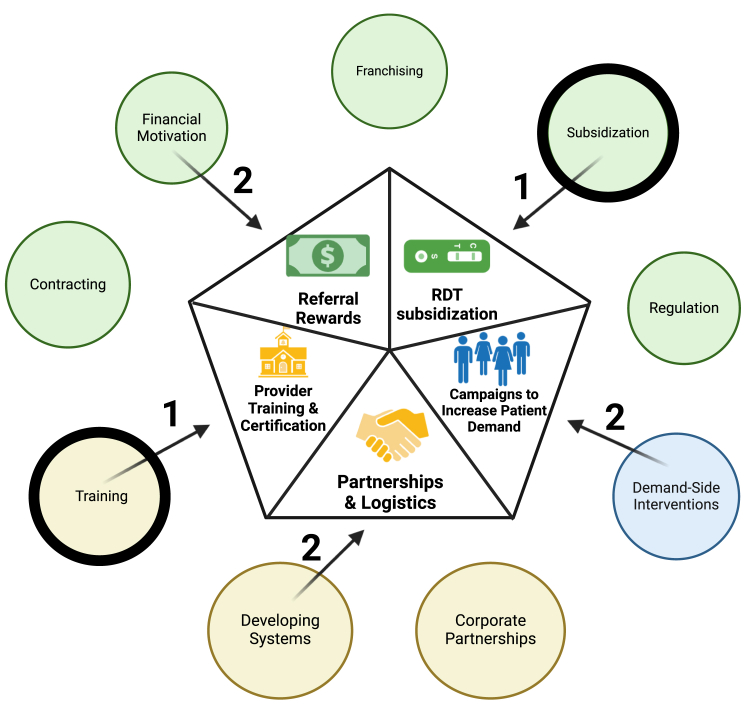
We recommend a two-step, multimodal model to optimize for-profit private sector engagement in Bangladesh (Fig. 4). As phase one of our intervention, we recommend the provision of free or subsidized RDTs to PHPs to ensure adequate testing and the in-person, monthly training of providers on both proper RDT usage and case reporting (preferably through electronic reporting methods such as DHIS2 or other electronic reporting apps).27 Successful completion of both by PHPs and continued usage at follow-up spot checks 3–6 months later may be accompanied by the provision of an official certification. As a second phase, and pursuant to the outcomes of the first, we recommend broadening campaigns to increase patient demand for providers with a government-sponsored certification, the provision of cash rewards to PHPs upon the referral of a confirmed positive case, and a continuing strengthening of the partnerships and logistics required to ensure program success. A multimodal model is also necessitated by the heterogeneity of motivation amongst PHPs in Bangladesh, all of which are targeted under our model.
Fig. 4.
Model for PSE in Bangladesh. Matching the analysis of the success levels of individual strategies in the literature with the context of malaria elimination in Bangladesh, we created a stepped, multi-modal recommendation model for Bangladesh. This model targeted all three modes of provider motivation, including referral rewards incentive payments and RDT subsidization for providers motivated by self-interest, namely campaigns to increase patient demand for providers motivated by patient demand, training and the formation of partnerships and logistics for providers motivated by concern for the public good. The stepped feature accommodates phased elimination strategy of the National Malaria Elimination Program and conditions in high endemic districts of the CHTs, where there is urgent need to decrease malaria levels but the number of private providers maybe lower and a significant fraction may be informal providers. Here close attention should be paid to the first steps of training of providers to conduct diagnosis with subsidized RDT and rapid, secure entry of data into electronic formats needed by the national program as well as subsidization of RDTs (1, encircled in bold). Success in utilization of RDT could be followed by step (2) of developing systems to support networks that emerge between the patient community, private provider and NMEP, as well as by demand-side interventions and incentive payments for referrals. Created in BioRender. Mcardle, R. (2022) BioRender.com/s84a20.
For-profit private sector healthcare providers have not been well incorporated into Bangladesh's public-sector malaria elimination efforts and in this regard its successes have been unique (in the South Asian context). Corporate partners have played a large role in Sri Lanka and the same has been proposed in India.28,29 Our findings and analyses show that PSE with informal and formal providers, will be an important tool for strengthening malaria surveillance and treatment networks as the country works towards elimination. We recognize that there is heterogeneity in the private sector as well as paucity of information on the numbers of PHPs and the extent to which they engage in the diagnosis of malaria across CHT districts. But given the immediate need to initiate PSE, we suggest that sub-districts with the highest annual parasitological index (API; # of infected individuals per 1000) be prioritized through pilot studies and we therefore discuss in greater detail the application of the model to these regions, below.
At the outset, we suggest engagement of consultancies and diagnostic centers, private clinics (with trained doctors), drug stores with malaria diagnostic facilities as well as established NGO clinics (that are not yet partners with the government). Five to ten of the indicated provider types are expected to be found in different rural high-endemic sub-districts. We propose training that is in-person and on a monthly basis, with spot checks for quality control to maintain high standards and keep up with turnover. We also propose that RDTs be provided without cost or at very low cost. In most settings this is done to flood the market with cheap high-quality tests in order to push poorer quality or counterfeit tests out of the market. This should also hold true in Bangladesh. A number of RDTs could also be given for free as a reward if a positive case is reported. They will be provided by government-NGO partners (who are provided with RDT's from the Global Fund). Again, surprise spot checks may need to be conducted and patients should be asked in exit surveys if they paid for RDTs. But we also think that the program could be successful if PHPs charged a small fee for the test (to make a little profit because otherwise they won't carry them).
Another important consideration is electronic data entry. There is access to mobile networks and PHPs have smart phones and access to the internet. In particular, DHIS2, a nationwide health information network already used by multiple government health programs in Bangladesh rural areas.30 It has been utilized in malaria elimination in multiple settings in Southeast Asia25 and Africa.27 Thus it is well understood for use in malaria elimination and likely to present an informed framework that may be suitably modified to meet malaria case reporting needs in Bangladesh.
On behaviour and demand side interventions, patients often do not know that they have malaria, so they visit private providers to obtain a diagnosis. In addition, demand-side interventions would be designed to increase the proportion of patients visiting private providers who prefer certified clinics and to increase the proportion of patients seeking high-quality, certified RDTs. Further, to be treated patients need not visit another clinic, but rather can be treated under the BRAC-NGO Shasthya Kormi system via in–home visits. As indicated earlier, we propose minimum standards, such that PSE initially begin with consultancy and diagnostic centers, private clinics (with trained doctors), drug stores, with malaria diagnostic facilities as well as established NGO clinics (that are not yet partners with the government). We also propose outcomes evaluation over 3–6 months and thereby develop validated training protocols that provide basis for accreditation/certification across high endemic areas (since there are registered diagnostic centers that perform malaria RDTs across these areas). These validated training protocols may subsequently be used with PHP who operate informally, as long as they can meet the standards and can achieve accreditation/certification. With respect to regulation of blood draws, in Bangladesh, registered diagnostic centers that perform blood tests such as malaria RDTs exist across the endemic areas. Moreover, trained health care workers (Shasthya Kormi) in BRAC-NGO consortia who partner with government are approved for point-of-care (at home) diagnosis and treatment of P. falciparum and P. vivax malaria. Sharps and contaminated waste will be turned over to government facilities and their partner NGOs, who already do this for Shasthya Kormi.
Presently the government program provides malaria treatment free of costs at listed hospitals and through Shasthya Kormi (associated with partner NGOs). PSE will have to show robust performance in diagnosis, before PHPs can be included in dispensing treatments.
On cost projections, the RDTs are provided by The Global Fund and therefore free. Hence the principal cost lies in training existing staff at the PHP, carrying out spot checks, as well as developing data tool kits/apps that need to be developed for electronic transfer of data that is compatible with government platforms. The Bangladeshi context is unique to South Asia because its successful public sector malaria control programs have not needed to engage corporate partners (as undertaken in Sri Lanka and proposed in India).28,29 We propose that cost estimates be reached through undertaking pilot projects that will also yield data on efficacy (i.e. the extent to which detection is increased), which in turn will yield projections on improved health (which will provide a positive impact on the economy). Cost toward “developing systems” of communication, transportation, and infrastructure in the CHTs would likely require significant resources. However, these goals align with the government's broader aim of becoming a middle-income country by 2035, and so funding would not need to originate from malaria control programs but rather from broader, better-funded national development programs. All levels of the Govt of Bangladesh are committed to the elimination of malaria by 20301 and it is reasonable to expect they will make necessary allocations appropriate for a country that aspires to be a middle-income country by 2035.
Contributors
Ryan McArdle: Conceptualization, Investigation, Methodology, Visualization, Writing—Original Draft, Writing—Review and Editing.
Ching Swe Phru: Project Administration, Supervision, Writing—Review and Editing.
Mohammad Sharif Hossain: Project Administration, Supervision, Writing—Review and Editing.
Mohammad Shafiul Alam: Conceptualization, Project Administration, Supervision, Writing—review and editing.
Kasturi Haldar: Conceptualization, Funding Acquisition, Supervision, Project Administration, Visualization, Writing—Original Draft, Writing—Review and Editing.
Data sharing statement
This study aims to provide full data transparency. A full list of search terms and sources included in the literature review can be found in the supplemental materials. All other inquiries for data sharing can be directed to the corresponding author.
Declaration of interests
No funding was received for the formulation of this manuscript. The authors declare no competing interests.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2024.100487.
Appendix A. Supplementary data
References
- 1.Program NME . Directorate general of health services, Ministry of Health and Family Welfare; Dhaka, Bangladesh: 2021. National strategic plan for malaria elimination 2021-2025. directorate general of health services MoHaFW.https://apmen.org/sites/default/files/all_resources/National%20Strategic%20Plan_Malaria%20Elimination_Bangladesh_2021-2025.pdf [Google Scholar]
- 2.Matin M.A., Sarkar N.D.P., Phru C.S., et al. Precarity at the margins of malaria control in the Chittagong Hill Tracts in Bangladesh: a mixed-methods study. Pathogens. 2020;9(10):840. doi: 10.3390/pathogens9100840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinha I., Sayeed A.A., Uddin D., et al. Mapping the travel patterns of people with malaria in Bangladesh. BMC Med. 2020;18(1):45. doi: 10.1186/s12916-020-1512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Onoka C.A., Onwujekwe O.E., Hanson K., Uzochukwu B.S. Sub-optimal delivery of intermittent preventive treatment for malaria in pregnancy in Nigeria: influence of provider factors. Malar J. 2012;11(1):317. doi: 10.1186/1475-2875-11-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennett A., Avanceña A.L.V., Wegbreit J., Cotter C., Roberts K., Gosling R. Engaging the private sector in malaria surveillance: a review of strategies and recommendations for elimination settings. Malar J. 2017;16(1):252. doi: 10.1186/s12936-017-1901-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown M., Bouanchaud P., Tesfazghi K., et al. Motivation to test, treat, and report malaria cases: a quantitative assessment among private sector providers in the Greater Mekong Subregion. Malar J. 2022;21(1):82. doi: 10.1186/s12936-022-04108-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams A.M., Ahmed R., Shuvo T.A., Yusuf S.S., Akhter S., Anwar I. Exploratory qualitative study to understand the underlying motivations and strategies of the private for-profit healthcare sector in urban Bangladesh. BMJ Open. 2019;9(7) doi: 10.1136/bmjopen-2018-026586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eijkenaar F., Emmert M., Scheppach M., Schöffski O. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Pol. 2013;110(2–3):115–130. doi: 10.1016/j.healthpol.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Diaconu K., Witter S., Binyaruka P., et al. Appraising pay-for-performance in healthcare in low- and middle-income countries through systematic reviews: reflections from two teams. Cochrane Database Syst Rev. 2022;5(5) doi: 10.1002/14651858.Ed000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondo K.K., Damberg C.L., Mendelson A., et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med. 2016;31 Suppl 1(Suppl 1):61–69. doi: 10.1007/s11606-015-3567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah N.M., Brieger W.R., Peters D.H. Can interventions improve health services from informal private providers in low and middle-income countries?: a comprehensive review of the literature. Health Pol Plann. 2011;26(4):275–287. doi: 10.1093/heapol/czq074. [DOI] [PubMed] [Google Scholar]
- 12.Chakravarthi I. Regulation of private health care providers in India: current status, future directions. Indian J Publ Adm. 2018;64(4):587–598. doi: 10.1177/0019556118780093. [DOI] [Google Scholar]
- 13.Montagu D., Goodman C. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? Lancet (London, England) 2016;388(10044):613–621. doi: 10.1016/s0140-6736(16)30242-2. [DOI] [PubMed] [Google Scholar]
- 14.Morgan R., Ensor T., Waters H. Performance of private sector health care: implications for universal health coverage. Lancet (London, England) 2016;388(10044):606–612. doi: 10.1016/s0140-6736(16)00343-3. [DOI] [PubMed] [Google Scholar]
- 15.Hanson K., Goodman C., Tougher S. Multicountry independent evaluation. Final Report; 2012. Independent evaluation of the phase 1 of the affordable medicines facility–malaria (AFMm)http://unitaidorg/assets/Midterm evaluation-Affordable-medicines-for-malaria-facility-AFMm-Phase=1pdf [Google Scholar]
- 16.Visser T., Bruxvoort K., Maloney K., et al. Introducing malaria rapid diagnostic tests in private medicine retail outlets: a systematic literature review. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montagu D., Goodman C., Berman P., Penn A., Visconti A. Recent trends in working with the private sector to improve basic healthcare: a review of evidence and interventions. Health Pol Plann. 2016;31(8):1117–1132. doi: 10.1093/heapol/czw018. [DOI] [PubMed] [Google Scholar]
- 18.Beyeler N., York De La Cruz A., Montagu D. The impact of clinical social franchising on health services in low- and middle-income countries: a systematic review. PLoS One. 2013;8(4) doi: 10.1371/journal.pone.0060669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiragu M., Fonner V.A., Munyuwiny S., et al. Does capacity development increase demand for health services and rights among key populations affected by HIV? A systematic review of evidence from low and middle-income countries. AIDS Behav. 2020;24(8):2268–2281. doi: 10.1007/s10461-020-02936-9. [DOI] [PubMed] [Google Scholar]
- 20.Naugle D.A., Hornik R.C. Systematic review of the effectiveness of mass media interventions for child survival in low- and middle-income countries. J Health Commun. 2014;19 Suppl 1(sup1):190–215. doi: 10.1080/10810730.2014.918217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beck D.C., Munro-Kramer M.L., Lori J.R. A scoping review on community mobilisation for maternal and child health in sub-Saharan Africa: impact on empowerment. Glob Public Health. 2019;14(3):375–395. doi: 10.1080/17441692.2018.1516228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones R.T., Tusting L.S., Smith H.M.P., et al. The role of the private sector in supporting malaria control in resource development settings. J Infect Dis. 2020;222(Suppl 8):S701–S708. doi: 10.1093/infdis/jiaa488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seidman G., Atun R. Do changes to supply chains and procurement processes yield cost savings and improve availability of pharmaceuticals, vaccines or health products? A systematic review of evidence from low-income and middle-income countries. BMJ Glob Health. 2017;2(2) doi: 10.1136/bmjgh-2016-000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rao V.B., Schellenberg D., Ghani A.C. Overcoming health systems barriers to successful malaria treatment. Trends Parasitol. 2013;29(4):164–180. doi: 10.1016/j.pt.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Potter R., Tesfazghi K., Poyer S., Eliades M.J. Private sector contributions to national malaria surveillance systems in elimination settings: lessons learned from Cambodia, Lao PDR, Myanmar, and Vietnam. Am J Trop Med Hyg. 2023;108(2_Suppl):14–23. doi: 10.4269/ajtmh.22-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith L.A., Jones C., Meek S., Webster J. Review: provider practice and user behavior interventions to improve prompt and effective treatment of malaria: do we know what works? Am J Trop Med Hyg. 2009;80(3):326–335. doi: 10.4269/ajtmh.2009.80.326. [DOI] [PubMed] [Google Scholar]
- 27.Mabona M., Zwane T., Raman J., Kuonza L., Mhlongo B., Phafane P. Evaluation of the malaria case surveillance system in KwaZulu-Natal Province, South Africa, 2022: a focus on DHIS2. Malar J. 2024;23(1):47. doi: 10.1186/s12936-024-04873-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernando D., Wijeyaratne P., Wickremasinghe R., et al. Use of a public-private partnership in malaria elimination efforts in Sri Lanka; a case study. BMC Health Serv Res. 2018;18(1):202. doi: 10.1186/s12913-018-3008-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahi M., Sharma A. India could harness public-private partnerships to achieve malaria elimination. Lancet Reg Health Southeast Asia. 2022;5 doi: 10.1016/j.lansea.2022.100059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wangmo S., Sarkar S., Islam T., Rahman M.H., Landry M. Maintaining essential health services during the pandemic in Bangladesh: the role of primary health care supported by routine health information system. WHO South East Asia J Public Health. 2021;10(Suppl 1):S93–S99. doi: 10.4103/2224-3151.309884. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.