Summary
The Robson Classification System is recognised as a first step for optimising the use of caesarean section and as a strategy for continuous quality improvement in maternal and newborn health. This Viewpoint provides a detailed account of the strategy adopted and lessons learned from a collaborative initiative to institutionalise the Robson Classification into Pakistan's health system. We developed a training package which emphasised capacity building of senior clinicians to act as master trainers. We also developed a mobile application for data collection and analysis. Training workshops took place in 2020 in a selection of public sector, tertiary-level, teaching hospitals from across the country and data was collected on all births in participating hospitals' obstetric units for a full year. Pakistan is poised for scale-up with the Robson Classification embedded in 57% of Pakistan's public, tertiary, teaching hospitals. A core group of master trainers is positioned in every province, and a robust dataset is available. However, integration into any health system cannot be thought of as a finite project. It requires government commitment, training and an ongoing process with built-in data quality assurance and feedback to clinicians.
Keywords: Robson Classification system, Caesarean section, Maternal health, Newborn health perinatal audit, Robson ten group classification, Continuous quality improvement
Introduction
Pakistan's sharp rise in the rate of caesarean section (CS) from 2.7% in 19901 to 23% in 20182 is causing alarm among public health experts. There is evidence that the rise may not be solely due to medical necessity. Moreover, the rise in the overall rate is masking areas where access to safe CS remains inadequate,3 especially rural areas where maternal and newborn mortality are highest. Pakistan, like many other low-income and middle-income countries (LMICs), now faces a triple burden,4 the coexistence of:
-
(i)
an unmet need for CS–Only 11.5% of rural women had a CS compared to 25.6% of urban women.5
-
(ii)
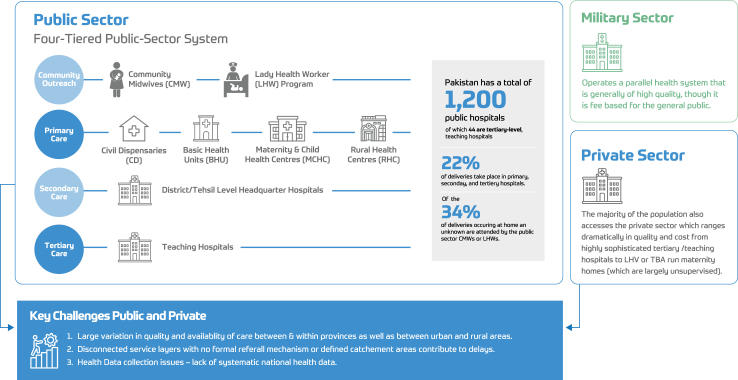
unsafe provision of CS–The three delays pose significant challenges across the country.6 Pakistan's health system is a complex mix of public, private, military and charity-run health services (Fig. 1). The various layers of service provision are disconnected with no formal referral mechanism or delineated catchment areas.7 The public-sector, tertiary, teaching hospitals receive complicated cases from traditional birth attendants (TBA), lady health visitors (LHV) and even advanced facilities in the private-sector who transfer them when they develop complications or cannot pay.1 As a result of the haphazard system, many women reach public-sector hospitals already critically ill and must undergo emergency CS in suboptimal conditions.
-
(iii)
the overuse of CS in certain populations.–A greater likelihood of having a CS is reported among the women with higher income, higher education and women living in urban areas. CS rates ranged from 5.5% in women with lower income to 35.3% in women with higher income.5
Fig. 1.
Pakistan mixed health system.
Pakistan's health system is chronically underfunded, and many programs are donor dependent.8 The situation is compounded by Pakistan's high population growth (fertility rate of 3.45 births per woman),5 worsening economic outlook, frequent natural disasters, the tenuous security situation, and political instability which harms program continuity. Inequalities in access to and quality of care are widespread resulting in disparity in maternal and newborn outcomes.5
Health data collection remains an inexact science in Pakistan; there is a dearth of real-time data on health, and birth and death registries are limited. Maternal and newborn health indicators are not an exception. Most analysis and public policies rely on estimates from the Pakistan Demographic and Health Survey (PDHS). Recognising the need for quality data to inform policies to address the triple burden, Pakistan's Ministry of National Health Services Regulations & Coordination (MoH) looked to global expertise. In 2015, the WHO released a statement recommending the Robson Classification System (RCS)9 as a standard for assessing, monitoring and comparing CS rates10 and began urging for a paradigm shift from striving to achieve a specific national CS rate to “optimising” the use of CS to fit the context.11
The MoH recognised the RCS as the first step towards comprehensive perinatal audit to collect data necessary for continuous quality improvement (CQI) in maternal and newborn care.12 However, despite a wealth of publications reporting RCS data (mainly individual hospital studies), the global literature is lacking in-depth accounts of initiatives to implement it at national level or strategies to address barriers, particularly in LMICs. Hence, stakeholders including MoH, WHO, Women's Health Intervention and Development Initiative (WHI-DI), a Pakistan-based non-governmental organisation (NGO) and Centre for Global Public Health (CGPH) launched a collaborative initiative to institutionalise use of the RCS into Pakistan's health system.
This viewpoint endeavours to add to global literature by describing Pakistan's activities and experience in implementation with a particular emphasis on how barriers were addressed. We hope to provide lessons learned that may be useful to others seeking to utilise the RCS, especially other LMICs.
Implementation strategy
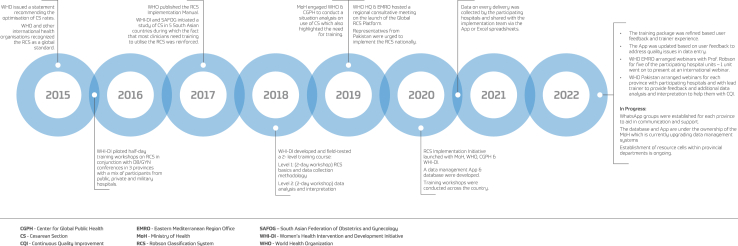
Experience from a previous study in South Asia13 and the situation analysis of Pakistan showed that training is necessary to effectively use the RCS. After extensive piloting and field-testing from 2015 through 2019, a two-level (4 day) course was finalised and formed the basis of the training of trainers (ToT) model developed for this initiative. A custom mobile application (App) was also developed to collect data on each childbirth including data beyond the core RCS variables (see Fig. 2 for a complete list of activities).
Fig. 2.
Timeline of activities.
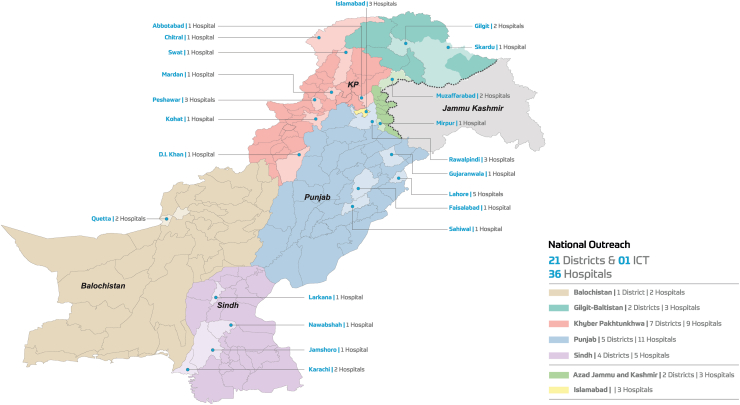
By the end of 2020, 36 public-sector hospitals had been trained across the country (Fig. 3) of which, 25 were tertiary-level, public-sector teaching hospitals (57% of Pakistan's total). Trainees were mainly professors or senior obstetricians-gynaecologists (OB/GYN). The intention was to create a core group of master trainers across the country. The involvement of senior clinicians was intended to strengthen consensus building ensuring adoption within the hospitals. It was also hoped that selecting senior staff would bypass the need to implement a more lengthy, standard ToT model. Participating hospitals collected data on every childbirth in their obstetric unit via a mobile App or manually (using Microsoft Excel spreadsheets). The resulting dataset is a significant step towards addressing Pakistan's lack of real-time data and will allow for myriad analysis. The data is also of sufficient quality that it can be uploaded to the WHO Robson Classification Platform to include Pakistan in the international data-driven dialogue to optimise the use of CS.14
Fig. 3.
Map of hospitals in Pakistan involved in training.
Prior to the initiative, healthcare providers were largely unaware of the RCS or had an incorrect understanding with several erroneously modified versions circulating in Pakistan. The training addressed misconceptions about the appropriateness of CS rates and challenges related to over or underutilisation. Participants also became aware that some of their own clinical practices were not evidence-based. Use of the RCS has been integrated into Pakistan's post-graduate medical curriculum which has had a cascading effect in spreading awareness among junior clinicians. This is expected to have a positive impact on clinical practices in the future.
Challenges and lessons
As a result of Pakistan's initiative, several lessons emerged that will inform Pakistan's scale-up efforts and may be relevant in other LMICs.
Lesson 1. Buy-in, scale-up and sustainability are not automatic; deliberate planning focused on these aspects is essential
Beginning in public-sector hospitals proved efficacious as the MoH was able to streamline logistics and use its authority to encourage participation in the initiative. This allowed for a faster uptake and sufficient progress to inform the next steps. Pakistan is poised for scale-up, but full integration into the health system is still in progress and no mandate for use of the RCS is in place. The situation has been complicated due to the recent surge in political instability (Pakistan has had four changes in government leadership in the last few years, and the original government focal person was transferred midway through the initiative). However, WHO and other stakeholders are collaborating with the MoH to embed the RCS into the National Strategy and Accountability Framework for Quality Reproductive Maternal Newborn Child & Adolescent Health.15 It is important that RCS and other CQI processes are aligned and connected. It is evident that for scale-up and sustainability donor or NGO stakeholders cannot replace commitment from the government.16 Absent an MoH mandate, buy-in of additional public-sector hospitals is unlikely as is the uptake of the RCS by other sector hospitals.
Recommendations
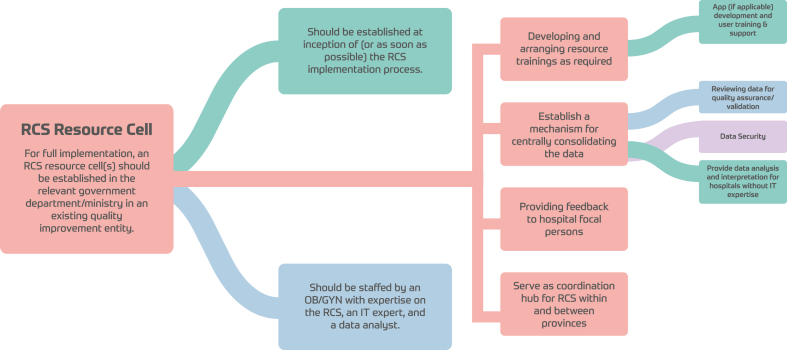
It's crucial that government stakeholders understand and endorse the value of adopting the RCS. At inception of any initiative, hold technical meetings to generate awareness, to define concrete roles and responsibilities, and to map a plan for scale-up and sustainability with all key stakeholders. The roles of donors, UN agencies, or NGOs should be understood as capacity building and support rather than indefinite program management. The team reached a consensus on the need to embed an RCS resource cell within an existing CQI entity in the relevant health departments (Fig. 4). The action-oriented use and report of the RCS should be mandated in every unit that performs CS, and the government should prepare policies or legislation for enforcement. A certification mechanism regulated by the MoH may increase motivation to complete trainings.
Fig. 4.
Robson Classification system resource cell.
Lesson 2. The importance of engaging the right leader in each hospital
Exclusively training senior clinicians had drawbacks including resistance to change or time constraints which impeded some of them in completing the full training or implementing the RCS in their units. Several senior clinicians retired during the initiative leaving untrained junior doctors to take over or letting participation lapse.
Recommendations
The identification of the right person is crucial. Criteria should emphasise selecting candidates based on interest and motivation as well as qualifications and leadership qualities rather than seniority alone since the former are key drivers for successful uptake.17,18 This was shown in Pakistan's case where a small number of interested clinicians have been most successful in terms of data quality and are continuing to share data. Motivation and appreciation within the health unit are fundamental, and incentives (not necessarily financial) can be of help. Junior doctors represent sustainability for the future and should be seriously considered and engaged from the beginning. The data review process can be used to identify participating clinicians who, through their success in submitting accurate data, have demonstrated both interest in the RCS and mastery of concepts thereby making them good candidates for master trainers. Annual progress reviews at national or provincial level that highlight the units/staff that have made the most progress may help to keep implementing teams engaged and motivated.
Lesson 3. Structuring the training to fit the context is crucial
Attempting to teach both the fundamentals of the RCS and the use of a mobile App within the same training workshop did not give participants enough exercise time to master concepts and skills resulting in the need for additional post-training activities. The condensed ToT model was sub-optimal to ensure the “master trainers” were adequately prepared to successfully train their colleagues or juniors.
Recommendations
A modular structure of the training allows the selection of modules to suit the needs of different hospital staff according to their roles. For example, the orientation module should include administrators or heads of departments to ensure buy-in and consensus building. The module on data analysis should include hospital IT staff. Interested senior or middle staff, who will conduct the bulk of data collection and interpretation, should be present for the entirety of the training as should any prospective “master trainers” if a ToT strategy is used. It may be beneficial to adhere to a standard ToT format where only those who demonstrate their ability to further train others should be certified as master trainers.
Lesson 4. Good-quality data collection and analysis is possible but should not be taken for granted
Definitions of several core variables of the RCS are not standardised in Pakistan. For example, criteria used for diagnosis of labour (cervical effacement and dilatation) are not universally agreed upon. The definitions of some terms such as parity and laparotomy are misunderstood which contributed to errors in data collection and incongruous entries such as classifying a patient as nulliparous but with previous CS. Furthermore, adding many variables beyond the core RCS led to increased complexity in collection and analysis and may have eroded the willingness or ability of clinicians to participate.
Recommendations
The decision on collecting outcomes and variables beyond the core set for the basic Robson table should be based on the most common or priority issues and may be introduced in a phased approach. In Pakistan it is important to collect data on maternal and perinatal mortality; so, this was prioritised. To help ensure quality, participants need to understand the impact of errors and misclassification in the final data, and the importance of explicitly agreeing on or understanding definitions cannot be overemphasised. Similarly, unclassified cases are an indicator of data quality and reviewing each case presents an opportunity for improvement.
Lesson 5. Data management technology cannot replace understanding and critical thinking
Even the best designed mobile App is not a substitute for critical thinking of clinicians, having a full understanding of the fundamentals of the RCS, and the implications of their data on developing strategies for CQI. Issues the initiative team encountered can be grouped into three categories:
-
(i)
A lack of consensus on definitions of key terms
For example, classification errors were discovered in both data collection methods because terms such as parity and viability were not specified. Additionally, the term ruptured uterus was not included in the App resulting in laparotomy being incorrectly selected.
-
(ii)
Interface issues
Initially, the App did not allow users to make corrections, nor did it provide alerts for duplicate or contradictory entries (such as a woman being entered as nulliparous but with previous CS). Similarly, careful programming is needed for the criteria to classify each group based on the WHO Robson Implementation Manual19 to avoid patients incorrectly being designated as unclassified. Some users were also confused because they assumed the App had inbuilt capability for statistical analysis.
-
(iii)
Lack of access to requisite technology.
Connectivity issues, especially in remote areas, made consistent use of web-based systems unrealistic, and many hospitals do not have robust (or any) IT support.
Recommendations
Ensure proficiency in manual data collection methods coupled with a working knowledge of how to generate the Robson table from a Microsoft Excel spreadsheet. If the decision is made to pursue an App, the aforementioned government resource cell or an OB/GYN with expertise in the RCS must be engaged from the design phase to ensure it is appropriate for the local context and that all terms are correctly defined within an App. If designed for analysis beyond creation of the basic Robson table, it must also provide data cleaning and sorting options by group, CS indication, etc to avoid the necessity for users to have access to and expertise in specialised statistical software to complete analysis. It is important to note that since the App was the first of its kind, there was a learning curve for both users and App designers. The initiative team sought and incorporated feedback from users and utilised a data review process to improve the App on an ongoing basis.
The way forward
Country-wide institutionalisation of the RCS cannot be thought of as a short-term, finite project. Additional phases are needed to avoid “pilotitis” –the failure of a successful pilot to be scaled-up and become sustainable after donor funding ends.20 Government ownership is crucial to sustain and scale-up the process. Efforts and lessons learned need to be documented and shared. Importantly, even absent a national implementation effort, the RCS can still be used for CQI in individual hospitals or obstetric units. Interested stakeholders can utilise the resources available through the WHO such as the Implementation Manual and Global Platform.
Conclusion
Described in this viewpoint is the ongoing and dynamic nationwide effort to institutionalise the Robson Classification in Pakistan. It is the first step for comprehensive perinatal audit to improve quality of care and provides an important proof of concept for the use of the RCS on a large-scale in an LMIC context. The lessons learned from Pakistan may provide useful insights to other countries or institutions seeking efficient implementation of the RCS.
Contributors
LH, APB, KG and QU conceived the study. KG and ET managed the funds. LH, KG, QU, and ET collaborated on the conception and design of the initiative and its activities. TR, ET and LH developed the data collection tools. ET, QU and TR guided the development of the electronic data collection tool. LH conducted the training of initiative participants. TR conducted training on the electronic data collection tool. QU and ET coordinated and oversaw all training and post-training activities. LH provided follow-up training to participants and quality checked data. KG, LH, ET, QU and TR facilitated webinars of participants. QU and ET held several rounds of discussion with LH, TR, APB, and LW to develop and refine themes. LH, LW, ET, QU, TR and APB conducted the literature review. LH and LW wrote the manuscript. APB provided significant intellectual content and revisions. ET, QU, TR and KG provided revisions and additional information. LH and LW incorporated revisions and wrote the final draft of the manuscript. All authors agreed on the final version of the manuscript.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The current study received technical assistance from the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), World Health Organization, Geneva, Switzerland. The Robson TGCS implementation over the years has received funding from an anonymous donor, Ministry of Foreign Affairs, Norway; Federal Ministry for Economic Cooperation and Development, Germany and WHO internal funds. TR declares funding from Centre for Global Public Health, Pakistan. LH was hired as a consultant to facilitate training of participants and to write the manuscript. Authors declare no other conflicts of interest.
Acknowledgements
Authors thank Mariam Jamal and Bilal Safdar of Butterfly Communications for their assistance in creating the figures.
References
- 1.Mumtaz S., Bahk J., Khang Y.H. Rising trends and inequalities in cesarean section rates in Pakistan: evidence from Pakistan Demographic and Health Surveys, 1990 – 2013. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0186563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute of Population Studies (NIPS) Pakistan and ICF . NIPS and ICF; Islamabad, Pakistan, and Rockville, Maryland, USA: 2019. Pakistan demographic and health Survey 2017-18. [Google Scholar]
- 3.Boatin A.A., Schlotheuber A., Betran A.P., et al. Within country inequalities in caesarean section rates: observational study of 72 low-and-middle income countries. BMJ. 2018;360:55. doi: 10.1136/bmj.k55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Betran A.P., Ye J., Moller A.-B., et al. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-005671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NIPS Pakistan and ICF . NIPS and ICF; Islamabad, Pakistan, and Rockville, Maryland, USA: 2019. Pakistan demographic and health Survey 2017-18. [Google Scholar]
- 6.Hassan L., Woodbury L. 2020. Delays recognized in maternal mortality. [DOI] [Google Scholar]
- 7.Nishtar S. Oxford University Press; 2010. Choked pipes: reforming Pakistan's mixed health system. [PubMed] [Google Scholar]
- 8.National maternal newborn Child health programme Pakistan. https://dynasoft.org/mnch/overview.php
- 9.Robson M. Classification of caeserian sections. Fetal Matern Med Rev. 2001;12(1):23–39. [Google Scholar]
- 10.Betran A.P., Torloni M.R., Zhang J.J., Gülmezoglu A.M., WHO Working Group on Caesarean Section WHO statement on caesarean section rates. BJOG. 2016;123(5):667–670. doi: 10.1111/1471-0528.13526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Betrán A.P., Temmerman M., Kingdon C., et al. Optimising caesarean section use interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392:1358–1368. doi: 10.1016/S0140-6736(18)31927-5. [DOI] [PubMed] [Google Scholar]
- 12.Savchenko J., Ladfors L., Hjertberg L., Hildebrand E., Brismar Wendel S. A step towards better audit: the Robson Ten Group classification system for outcomes other than cesarean section. Acta Obstet Gynecol Scand. 2022;101(7):827–835. doi: 10.1111/aogs.14350. Epub 2022 Mar 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hassan L., Woodbury L., Jamal N., et al. Examining the efficacy to the Robson classification system for optimizing caesarean section rates in South Asia. J South Asian Feder Obst Gynae. 2020;12(6):233–371. [Google Scholar]
- 14.Opiyo N., Torloni M.R., Robson M., et al. WHO's Robson platform for data-sharing on caesarean section rates. Bull World Health Organ. 2022;100(5):352–354. doi: 10.2471/BLT.21.287742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Government of Pakistan . National Strategic and Accountability Framework on Quality of Care for RMNCAH; 2021. Ministry of national health services, Regulations & coordination. [Google Scholar]
- 16.Altaf S. Woodrow Wilson Center Press with Johns Hopkins University Press; 2011. So much aid, so little development: stories from Pakistan. 978-1-4214-0137-9 hardback; 978-1-4214-0138-6 paperback. [Google Scholar]
- 17.Betrán A.P., Vindevoghel N., Souza J.P., Gülmezoglu A.M., Torloni M.R. A systematic review of the Robson classification for caesarean section: what works, doesn't work and how to improve it. PLoS One. 2014;9(6) doi: 10.1371/journal.pone.0097769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zahroh R.I., Kneale D., Sutcliffe K., et al. Interventions targeting healthcare providers to optimise use of caesarean section: a qualitative comparative analysis to identify important intervention features. BMC Health Serv Res. 2022;22(1):1526. doi: 10.1186/s12913-022-08783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . 2017. Robson classification implementation manual.https://www.who.int/publications/i/item/9789241513197 [Google Scholar]
- 20.Chamberlain S., Dutt P., Godfrey A., et al. Ten lessons learnt: scaling and transitioning one of the largest mobile health communication programmes in the world to a national government. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-005341. [DOI] [PMC free article] [PubMed] [Google Scholar]