Abstract
Background:
The number of hip arthroscopies performed in the United States has grown significantly over the past several decades, with evolving indications and emerging techniques.
Purposes:
To (1) examine the evolution of hip arthroscopy at 3 tertiary referral centers between 1988 and 2022 and (2) quantify trends in patient demographics and procedures performed.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective analysis was performed of all patients undergoing hip arthroscopy at 3 academic centers between 1988 and 2022. Demographic data were collected using standardized forms and operative notes, and intraoperative images were manually reviewed for each patient to determine the specific procedures performed at the time of the hip arthroscopy. Surgical procedures were plotted over time to evaluate trends. Patients were divided into 3 time periods for comparison: early hip arthroscopy from 1988 to 2008, 2009 (the time of the first labral repair in our cohort) to 2015, and 2016 to 2022.
Results:
A total of 3000 patients (age, 35.7 ± 13.8 years; age range, 10-89 years; female sex, 2109 (70.3%); body mass index, 27.4 ± 6.3 kg/m2) underwent arthroscopic hip procedures between 1988 and 2022. The mean number of cases increased from a mean of 3.2 per year in 1988-2008 to 285.9 per year in 2016-2022 (P < .001). Labral treatment at the time of primary hip arthroscopy evolved from 100% debridement and 0% repair in 1988-2008 to 5.0% debridement, 94.0% repair, and 1.0% labral reconstruction in 2016-2022 (P < .001). Cam resection increased from 4.1% in 1988-2008 to 86.9% in 2016-2022 (P < .001). By 2022, 45 out of 325 cases (13.8%) were revisions. The rate of capsular repair at the time of primary hip arthroscopy increased from 0.0% in 1988-2008 up to 81.0% in 2016-2022.
Conclusion:
There has been a significant growth of hip arthroscopy volumes as well as a significant transition from use as a tool for diagnosis and labral debridement to procedures restoring native anatomy including labral repair, cam resection, capsular repair, periacetabular osteotomy, and gluteal repair.
Keywords: hip/pelvis/thigh, hip arthroscopy, hip: femoroacetabular impingement, groin pain, osteotomy, acetabular labrum repair, cam resection, pincer resection, capsular repair, psoas fractional lengthening
Despite the dramatic rise in popularity over the past 2 decades, hip arthroscopy is over a century in the making. 32 The first arthroscopes were descendants of 19th-century endoscopes, with Nordentoft proposing the use of such a device in the evaluation of meniscal lesions in 1912 in Denmark. Subsequently, Takagi performed the first cadaveric knee arthroscopy in 1918. 18 Burman performed the first cadaveric hip arthroscopy in 1931, 5 but due to the depth of the hip joint and challenges accessing and visualizing the central compartment, arthroscopy of the hip lagged behind that of the shoulder and knee, with the author stating, “It is manifestly impossible to insert a needle between the head of the femur and acetabulum. One cannot, therefore, hope to see the acetabular fossa with its outlying horseshoe-shaped fibrocartilage.” Takagi's student, Watanabe, 35 continued to make advancements in arthroscopic designs and techniques throughout the 1940s and 1950s. However, hip arthroscopy was not performed on a living patient until 1986 when Suzuki et al 34 published a series of diagnostic arthroscopies in 8 hips. This was shortly followed in 1987 by a report by Glick et al 16 on the innovative use of traction and lateral positioning to reliably enter and instrument the central compartment.
Though one of the first reported therapeutic uses of hip arthroscopy was loose body removal in the early 1990s performed by Byrd, 6 arthroscopy remained primarily a diagnostic tool throughout the next decade. An increased understanding of acetabular labral tears and femoroacetabular impingement syndrome (FAIS) as sources of hip pain and the described association between FAIS and hip osteoarthritis led to a renewed interest in therapeutic applications of hip arthroscopy.30,38 The diagnosis of FAIS has increased over time as the understanding of this condition evolves. 38 The incidence of FAIS is reported at up to 54.4 per 100,000 person-years,17,30 and this number has increased over time. Similarly, the treatment of FAIS has evolved over time. Since Ganz et al 14 first described the association between FAIS and hip osteoarthritis in 2003, hip arthroscopy has seen a rapid growth in surgical case volume and an expanding breadth of indications and surgical techniques.25,32 Better instrumentation, including the application of the 70° arthroscope, improved suture anchors and passing devices, and high-speed burrs made labral repair and acetabular and femoral osteochondroplasty (cam resection) reliable options for the treatment of labral pathology and FAIS. Renewed interest throughout the 2010s and a rapidly expanding body of supportive evidence led to further application of arthroscopic techniques to a variety of indications including labral tears in the setting of borderline acetabular dysplasia, labral reconstruction, iliopsoas impingement, and gluteal tears.4,21,26,36 Furthermore, the role of the capsulotomy and repair or lack thereof has evolved over time from excision in the early years of hip arthroscopy, to capsulotomy without repair in the early 2000s, and finally, to capsular repair, which increasingly has become standard practice. 12
While outcomes of various evolving hip arthroscopic techniques have been individually published, to date there is no published granular investigation quantifying the evolution and relative volumes of hip arthroscopic procedures such as labral treatment and capsular management over time. This is of clinical importance as we evaluate available case series; define modern, contemporary hip arthroscopy; and contrast it against historical techniques. The historical context and current trends are important to establish to identify and quantify areas of ongoing innovation in the field of hip arthroscopy. Therefore, the purposes of this study were to (1) examine the evolution of hip arthroscopy at 3 tertiary referral centers between 1988 and 2022 and (2) quantify trends in patient demographics as well as procedures performed.
Methods
A retrospective analysis was performed of all patients who underwent hip arthroscopy at 3 academic tertiary referral centers between 1988 and 2022. The 3 centers included in the study are academic hospitals with specialized surgeons involved in training residents and fellows. While the surgeon training and expertise varied early in the study due to the new nature of hip arthroscopy, all procedures in the modern era were performed by orthopaedic sports medicine fellowship–trained surgeons. All patients who underwent hip arthroscopy for any reason were identified by searching the electronic medical record for Current Procedural Terminology codes related to hip arthroscopy. Each patient record was manually reviewed to ensure hip arthroscopy was performed. Any patients who did not undergo hip arthroscopy were excluded, which mostly consisted of patients who underwent only open surgical procedures about the hip. Demographic data including age, sex, and body mass index (BMI) at the time of surgery were collected via chart review. Operative notes and imaging were manually reviewed for each patient to determine the specific procedures performed at the time of the hip arthroscopy. Arthroscopic procedures included diagnostic arthroscopy, labral debridement, labral repair, labral reconstruction, capsular repair, cam resection, fractional iliopsoas lengthening, loose body removal, ligamentum teres debridement, trochanteric bursectomy, and abductor repair. Arthroscopic procedures performed on prosthetic hips (ie, fractional iliopsoas lengthening for symptomatic iliopsoas tendinitis) were included as were extra-articular procedures alongside interventions such as isolated arthroscopic gluteus medius and minimus repair. Rates of pincer resection were not evaluated due to the inherent challenge of retrospectively determining and differentiating acetabular rim preparation at the time of labral repair from rim preparation with coincident measured rim resection with the goal of modifying lateral coverage. Simultaneous open procedures such as periacetabular osteotomy (PAO) were also documented on standardized study collection forms. For each case, it was noted if the procedure embodied a primary or revision hip arthroscopy. True primary hip arthroscopies were defined as a first-time intra-articular hip arthroscopy in a native hip including central compartment access. Revision hip arthroscopy was defined as a repeat intra-articular hip arthroscopy after a prior intra-articular hip arthroscopy. Patients who underwent isolated (peripheral compartment) iliopsoas fractional lengthening (ie, in the setting of a prosthetic hip), isolated trochanteric bursectomy, or gluteus medius and minimus repair were analyzed separately.
Graphs demonstrating trends in procedures over time were created for each procedure. Additionally, patients were split into 3 time periods for statistical comparison. Time period 1 consisted of the prelabral repair era and included all patients before 2009 when the first acetabular labral repair was performed at our institution. The labral repair era included all patients between 2009 and 2022. The labral repair era was split into 2 equal time periods: time period 2 between 2009 and 2015 and time period 3 between 2016 and 2022, which also coincided with increasing recognition of capsular importance and capsular repair. Data were summarized and reported using standard descriptive statistics, including means and standard deviations for continuous variables, with counts and percentages for categorical data. Demographics and surgical procedures were compared for the 3 time periods using analysis of variance for continuous variables and chi-square or Fisher exact tests for categorical variables. The alpha level was set at .05 for statistical significance. All statistical analyses were performed using SAS Studio software (version 3.81 (Basic Edition); SAS Institute).
Results
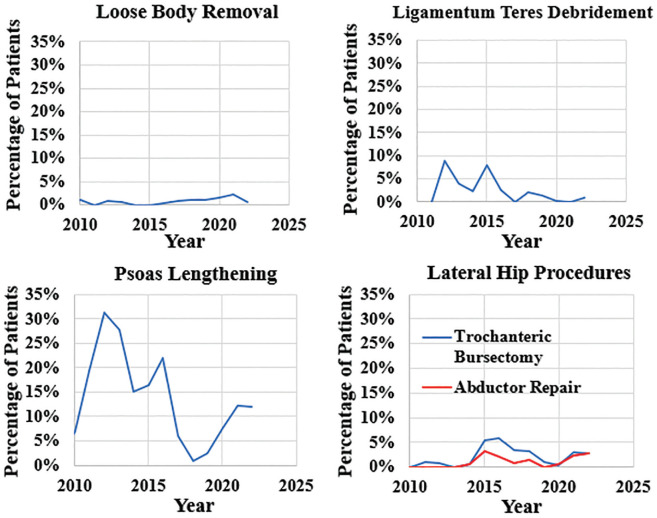
A total of 3000 patients (age, 35.7 ± 13.8 years; age range, 10-89 years; female sex, 2109 [70.3%]; BMI, 27.4 ± 6.3 kg/m2) underwent arthroscopic hip procedures at the 3 institutions between 1988 and 2022. No patients underwent simultaneous bilateral hip arthroscopy. Of the 3000 patients, 2265 underwent surgery at Mayo Clinic Minnesota, 553 at Mayo Clinic Arizona, and 182 at Mayo Clinic Florida. The first hip arthroscopy in this cohort was performed at Mayo Clinic Minnesota in 1988 for diagnostic purposes in a patient with hip pain refractory to conservative management. A labral tear was identified at the time of arthroscopy, and the surgeon converted to an open arthrotomy and resected the involved labrum. Subsequently, during the prelabral repair era between 1988 and 2008, 51 patients underwent arthroscopic hip procedures. Of these, 49 (96.1%) were true primary hip arthroscopies, 1 was an arthroscopic trochanteric bursectomy and iliotibial band release, and 1 was a revision total hip arthroplasty (THA) in which hip arthroscopy was used to assist with a portion of the cement removal. Of the 51 total hip arthroscopies performed from 1988-2008, 13 (26.5%) were diagnostic only. Of the 49 true primary hip arthroscopies, 30 (61.2%) had labral debridement (all were arthroscopic except for the first which was performed after conversion to open arthrotomy in 1991), 2 (4.1%) had arthroscopic cam resections, and 1 (2.0%) had a psoas fractional lengthening (Table 1). The number of cases per year increased from 3.2 ± 4.6 per year in 1988-2008 to 135.4 ± 66.9 in 2009-2015 and 285.9 ± 49.9 in 2016-2022 (P < .001). The first hip arthroscopy at Mayo Clinic Arizona was performed in 2007, and the first case at Mayo Clinic Florida was in 2008. Overall case volume increased steadily between 2010 and 2022, with a peak volume of 369 cases in 2021 (Figure 1). Increased case volume was accompanied by an increase in the volume of revision hip arthroscopy. The first revision arthroscopy in the present study was performed in 2009, and by 2022 45 out of 325 cases (13.8%) were revisions.
Table 1.
Trends in Age, Sex, and Surgical Procedures Between 1988 and 2022 a
| Prelabral Repair Era | Labral Repair Era | P | ||
|---|---|---|---|---|
| 1988-2008 | 2009-2015 | 2016-2022 | ||
| (n = 51) | (n = 948) | (n = 2001) | ||
| No. of cases per y | 3.2 ± 4.6 | 135.4 ± 66.9 | 285.9 ± 49.9 | <.001 |
| Age, y | 40.1 ± 14.6 | 37.1 ± 13.9 | 34.9 ± 13.6 | <.001 |
| Female | 34 (66.7) | 672 (70.9) | 1406 (70.3) | .79 |
| Body mass index, kg/m2 | 24.7 ± 3.4 | 26.5 ± 6.1 | 28.1 ± 6.4 | <.001 |
| True primary hip arthroscopy | 49/51 (96.1) | 873/948 (92.1) | 1701/2001 (85.0) | <.001 |
| Labral procedure | 30/49 (61.2) | 775/873 (88.8) | 1638/1701 (96.3) | <.001 |
| Labral debridement | 30/30 (100.0) | 179/775 (23.1) | 82/1638 (5.0) | <.001 |
| Labral repair | 0/30 (0.0) | 590/775 (76.1) | 1540/1638 (94.0) | <.001 |
| Labral reconstruction | 0/30 (0.0) | 6/775 (0.01) | 16/1638 (1.0) | .37 |
| Capsulotomy | 48/51 (97.9) | 873/873 (100.0) | 1699/1701 (99.9) | .01 |
| Capsular repair | 0/48 (0.0) | 349/873 (39.9) | 1377/1699 (81.0) | <.001 |
| Cam resection | 2/49 (4.1) | 718/873 (82.2) | 1479/1701 (86.9) | <.001 |
| Psoas lengthening | 1/49 (2.0) | 162/873 (18.6) | 151/1701 (8.9) | <.001 |
| Revision hip arthroscopy | 0/51 (0.0) | 61/948 (6.4) | 216/2001 (10.8) | <.001 |
| Labral procedure | 0/0 (n/a) | 42/61 (68.8) | 189/216 (87.5) | <.001 |
| Labral debridement | 0/0 (n/a) | 18/61 (42.9) | 12/189 (6.3) | <.001 |
| Labral repair | 0/0 (n/a) | 22/61 (52.4) | 171/189 (90.5) | <.001 |
| Labral reconstruction | 0/0 (n/a) | 2/61 (4.8) | 6/189 (3.2) | .61 |
| Capsulotomy | 0/0 (n/a) | 59/61 (96.7) | 216/216 (100.0) | .06 |
| Capsular repair | 0/0 (n/a) | 29/59 (49.2) | 198/216 (91.7) | <.001 |
| Cam resection | 0/0 (n/a) | 38/61 (62.3) | 160/216 (74.1) | .07 |
| Psoas lengthening | 0/0 (n/a) | 21/61 (34.4) | 58/216 (26.9) | .25 |
| Diagnostic only | 13/51 (26.5) | 24/948 (2.5) | 20/2001 (0.1) | <.001 |
| Conversion to open | 3/13 (23.1) | 1/24 (4.2) | 0/20 (0.0) | .12 |
| Diagnostic before PAO | 0/13 (0.0) | 20/24 (83.3) | 16/20 (80.0) | <.001 |
| Conversion to THA | 0/13 (0.0) | 2/24 (8.3) | 0/20 (0.0) | .89 |
| No intervention | 7/13 (53.8) | 1/24 (4.2) | 3/20 (15.0) | .01 |
| Other | 3/13 (23.1) | 0/24 (0.0) | 1/20 (5.0) | .12 |
| Arthroscopy with extra-articular procedures | 1/51 (1.9) | 115/948 (12.1) | 367/2001 (18.3) | <.001 |
| Psoas lengthening in THA | 0/51 (0.0) | 4/948 (0.4) | 63/2001 (3.1) | <.001 |
| Periacetabular osteotomy | 0/51 (0.0) | 85/948 (8.9) | 218/2001 (10.9) | .04 |
| Trochanteric bursectomy | 1/51 (1.9) | 17/948 (1.8) | 55/2001 (2.7) | .28 |
| Abductor repair | 0/51 (0.0) | 9/948 (0.9) | 31/2001 (1.5) | .39 |
Values are presented as n (%) or mean ± SD. n/a, not applicable; PAO, periacetabular osteotomy; THA, total hip arthroplasty.
Figure 1.
Trends in case volume. True primary cases were primary intra-articular hip arthroscopies. Revision included repeat intra-articular hip arthroscopy in the setting of prior intra-articular hip arthroscopy. Psoas only in prosthetic hips refers to patients who received either iliopsoas release or fractional lengthening in the setting of a native hip. The lateral procedure only included patients who underwent isolated arthroscopic trochanteric bursectomy or abductor repair. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
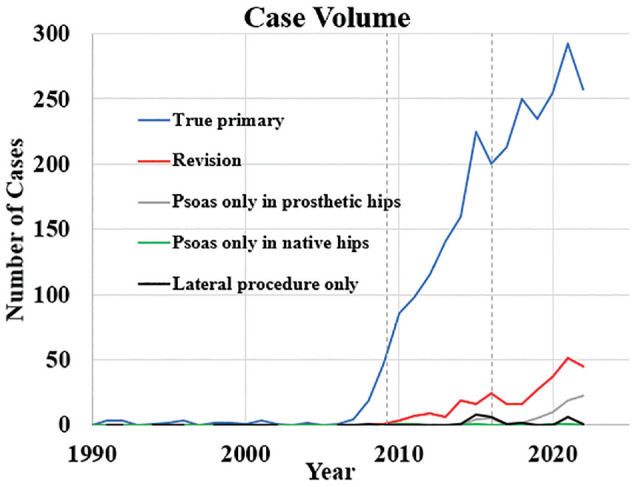
Over the course of the study period, the mean age of patients undergoing hip arthroscopy decreased from 40.1 ± 14.6 in 1988-2008 to 34.9 ± 13.6 in 2016-2022 (P < .001) (Table 1 and Figure 2) whereas there was no significant change in the percentage of female patients (P = .79). The mean BMI increased over time from 24.7 kg/m2 in time period 1 to 28.1 kg/m2 in time period 3 (P < .001).
Figure 2.
Trends in patient age and body mass index (BMI). BMI is reported in kg/m2. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
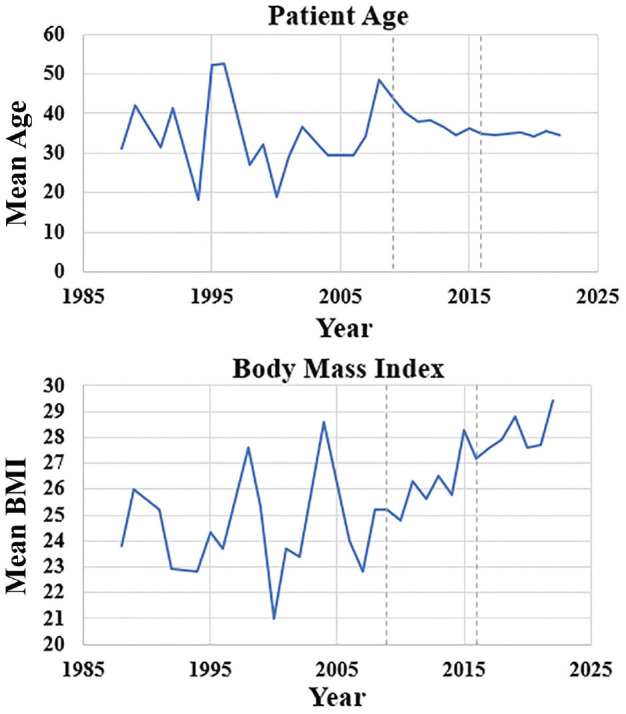
While labral debridement was initially the treatment of choice for labral tears at the time of primary hip arthroscopy early in the study period, labral repair surpassed debridement as the more common procedure in 2010 (58% repair versus 42% debridement in 2010) and continued to be the most common procedure for labral tears through 2022. By the 2016-2022 time period, 94.0% of labral procedures performed at the time of primary hip arthroscopy were labral repairs as compared with 0.0% in 1988-2008 and 76.1% in 2009-2015 (P < .001) (Table 1 and Figure 3). Of note, the first labral reconstruction in the study period was performed in 2014. The peak number of labral reconstructions per year in the study period was 7 (3.2%) in 2016. Similar trends were present for revision hip arthroscopy. Labral procedures at the time of revision transitioned from 42.9% debridement, 52.4% repair, and 4.8% reconstruction in time period 2 to 6.3% debridement, 90.5% repair, and 3.2% reconstruction by time period 3 (P < .001).
Figure 3.
Trends in labral treatment in true primary hip arthroscopies by year. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
The proportion of procedures including cam resection and capsular repair both increased significantly over the study period. The volume of arthroscopic cam resection has increased from 2 cases in 2008 to a peak of 296 cases in 2021. In 2022, 83% of arthroscopic hip surgeries in our study included a cam resection. In true primary hip arthroscopies, the rate of cam resection increased from 4.1% of patients in time period 1 to 86.9% in time period 3 (P < .001) (Table 1 and Figure 4).
Figure 4.
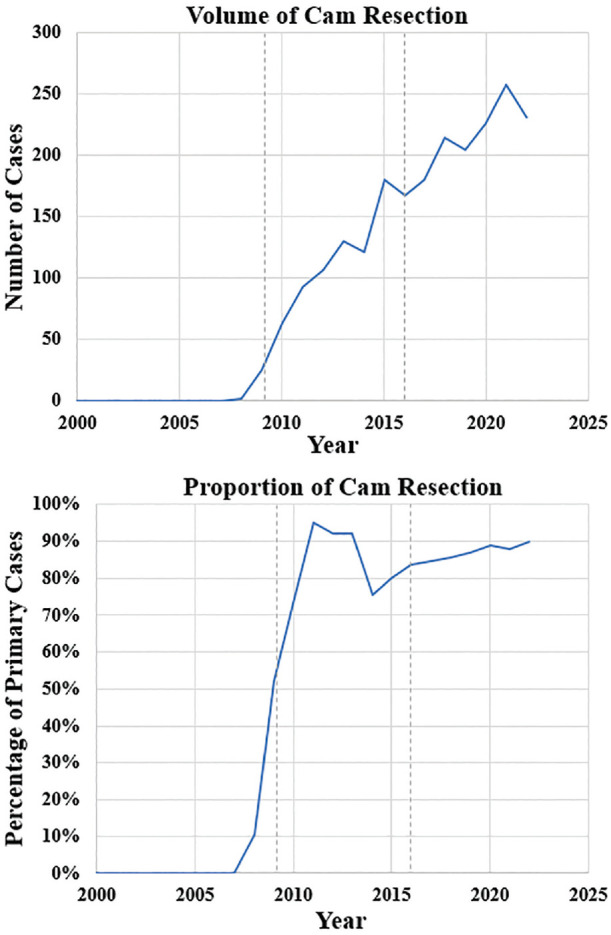
Trends in cam deformity treatment in true primary hip arthroscopies by year. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
Similarly, capsular repair increased from 0.0% of capsulotomies in primary hip arthroscopies in time period 1 to 81.0% in time period 3 (P < .001) (Table 1 and Figure 5). Of note, this includes the presence of a prospective randomized study of capsular repair versus nonrepair that enrolled patients between 2018 and 2020. In revision hip arthroscopy, the rate of capsular repair similarly increased from 49.2% in time period 2 to 91.7% in time period 3.
Figure 5.
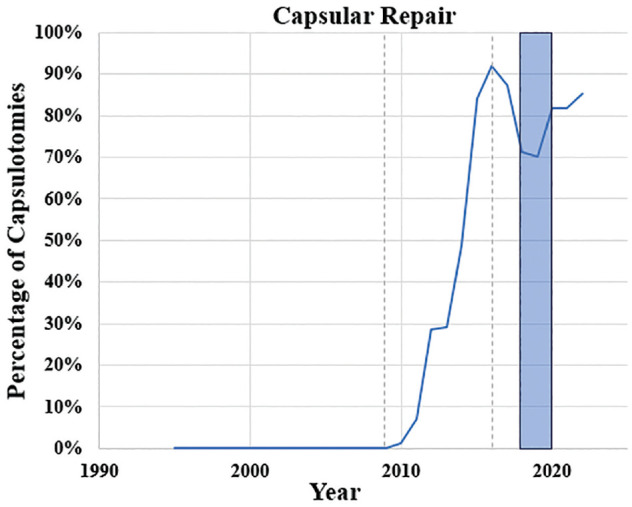
Trends in percentage of capsulotomies repaired in true primary hip arthroscopies by year. The blue shaded region represents the years 2018 to 2020, during which a percentage of patients were randomized to a noncapsular repair group for a clinical trial. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
The first arthroscopic iliopsoas release in the setting of a THA was performed at our institution in 2015 (Figure 1). The rate has increased over time with 19 cases (5.1%) in 2021 and 22 cases (6.8%) in 2022 performed on prosthetic hips. Only 5 native hips in the study cohort underwent isolated iliopsoas lengthening without a concomitant intra-articular hip procedure, and each of these was a revision hip arthroscopy in patients with prior intra-articular arthroscopic hip procedures. Similarly, isolated lateral procedures (ie, arthroscopic gluteus medius and minimus repair or trochanteric bursectomy without intra-articular access) were only performed 26 times throughout the study period; 16 (61.5%) of these occurred in time period 3.
The first simultaneous hip arthroscopy and PAO at our institution was performed in 2012. The volume of concomitant PAOs increased throughout the study period from 0 cases in the first 14 years to a peak of 45 cases (19.6%) in 2017 (Figure 6). Of hip arthroscopies in time period 3, 10.9% were performed at the time of a concurrent PAO.
Figure 6.
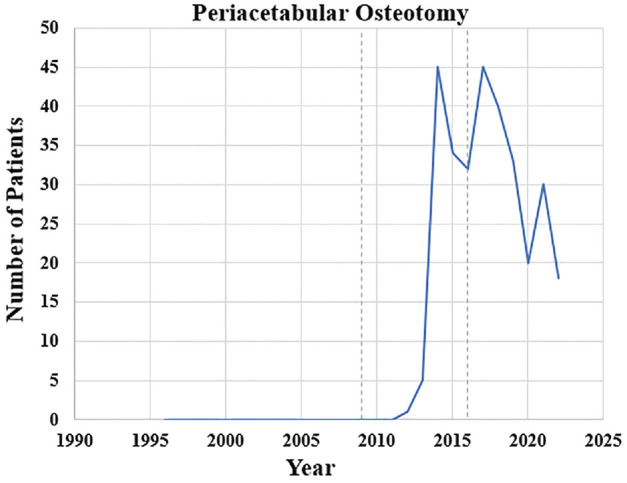
Trends in volume of simultaneous hip arthroscopy and periacetabular osteotomy by year. The dotted vertical lines denote the separation of time periods at 2009 and 2016.
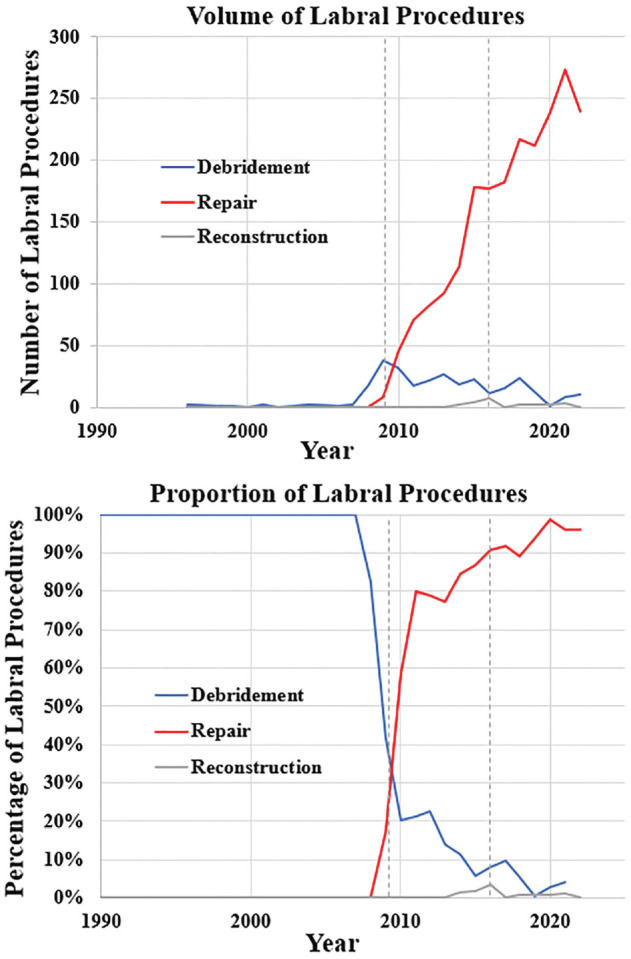
Additional arthroscopic hip procedure trends over time are shown in Figure 7. The rate of iliopsoas fractional lengthening or release at the time of true primary hip arthroscopy reached a peak of 31.3% in 2012. In the era of labral repair, the rate of loose body removal has remained relatively low at approximately 2% per year. Lateral hip procedures such as trochanteric bursectomy and arthroscopic abductor repair may be performed at the time of intra-articular hip arthroscopy or as an isolated procedure. The first trochanteric bursectomy was performed in 2008 and the first arthroscopic abductor repair was performed in 2014. In 2022, 9 patients (2.8%) each underwent arthroscopic trochanteric bursectomy and abductor repair. Of these, 8 were performed concomitantly with other intra-articular (central compartment) arthroscopic hip procedures.
Figure 7.
Trends in proportion of loose body removal, ligamentum teres debridement, iliopsoas release or fractional lengthening, and lateral hip procedures in true primary hip arthroscopies by year.
Discussion
The purpose of this study was to examine the evolution of hip arthroscopy at 3 tertiary referral centers from 1988 to 2022 and to quantify trends in patient demographics and procedures performed. The main findings of this study are the exponential growth of arthroscopy over the study period and a significant transition from initial use for diagnosis and labral debridement to procedures restoring native anatomy including labral repair, cam resection, and capsular repair. Demographically, there has been an overall decrease in mean patient age undergoing arthroscopy and an overall significant increase in BMI over time, mimicking the general population. Our findings are clinically relevant in that they are the first to quantify the evolution of hip arthroscopy procedures over time in a granular manner, demonstrating its evolution from diagnostic and palliative procedures to its current state as a high-volume intervention aiming to restore and optimize hip anatomy.
The overall volume of arthroscopic hip procedures at the 3 institutions studied increased significantly over the course of the study period, from a mean of 3 cases per year in 1988-2008 to a mean of 286 cases per year in 2016-2022. This trend is similar to prior reports including a 600% increase in hip arthroscopy from 2006 to 2010, 3 a 365% increase from 2004 to 2009, 23 and an 85% increase from 2011 to 2018. 39 During this time, we observed no substantial change in the number of male versus female patients undergoing hip arthroscopy, with approximately 70% of patients throughout all time periods analyzed being female, which is consistent with prior literature. 39 While hip arthroscopy was primarily used as a diagnostic procedure at our centers throughout the 1990s, the first therapeutic arthroscopic hip procedure in our cohort was a labral debridement in 1991. This was 1 year following the first reported therapeutic arthroscopic hip procedure, which was loose body removal performed by Byrd in 1990. 6 Of note, the labral debridement in our study and Byrd's loose body removal comprised therapeutic, but nonrestorative, procedures. The rate of therapeutic procedures in our cohort increased dramatically following the recognition of FAIS as an etiology of hip osteoarthritis, championed by Ganz and colleagues in 2003. 14 Since then, the treatment of FAIS has greatly increased in the literature and in our study population, likely due to improved recognition.17,30
The first cam resection in our cohort occurred in 2008, 16 years after the first arthroscopic hip procedure among the 3 institutions studied. The volume of arthroscopic cam resection has increased from 2 cases in 2008 to a peak of 296 cases in 2021. In 2022, 83% of arthroscopic hip surgeries in our study included a cam resection. This closely mirrors the large database study by Gillinov et al 15 in which cam resection comprised 81% of arthroscopic hip procedures. The rapid rise in cam resection followed reports of favorable outcomes for the procedure, including the 2009 study by Byrd and Jones 7 that demonstrated significant improvements in patient-reported outcomes and low rates of conversion to THA. Cam resection may be especially beneficial as cam deformities have been shown to have an association with labral tears as well as early, mechanically driven osteoarthritic changes particularly in adolescent patients. 37
Before 2009, only 61% of patients in our cohort underwent labral procedures at the time of primary hip arthroscopy, all of which consisted of labral debridement. The first labral repair in our cohort occurred in 2009. Soon thereafter, labral repair surpassed debridement as the most common labral procedure at the time of hip arthroscopy, with labral procedures consisting of 58% repair versus 42% debridement in 2010. A 2014 study by Krych et al 19 demonstrated overall modest results for isolated labral debridement and another study by the same lead author demonstrated overall superior outcomes of labral repair as compared with debridement in a randomized controlled trial with 32-month mean follow-up. 20 Biomechanical data continue to emerge regarding the structural role of the labrum and its contribution to hip stability, which may play a role in current labral-preserving philosophies. 29 Labral reconstruction has gained popularity in recent years for managing complex, extensive labral tears, especially in the setting of revision hip arthroscopy with irreparable (recurrent) labral tears. Bodendorfer et al 2 reported similar outcomes for labral repair and labral reconstruction in their cohort of primary hip arthroscopies. In our study, 30 patients underwent labral reconstruction. Eight of these (26.7%) were performed at the time of revision hip arthroscopy. At our institution, labral repair remains significantly more common than labral reconstruction, comprising 96% of all labral procedures performed in 2022. To date, the relative indications of repair, augmentation, and reconstruction remain to be further defined, particularly as they relate to long-term, randomized prospective outcomes.
The importance of capsular preservation and repair has become a topic of increasing interest in contemporary hip arthroscopy. While patient-reported outcomes may be improved in patients with complete capsular closure, 11 other studies have demonstrated healing of (small) unrepaired capsulotomies on magnetic resonance imaging by 24 weeks postoperatively and no clinically relevant superiority over unrepaired capsulotomies.10,33 In our study, rates of capsular repair increased significantly over time, with 0% repair between 1988 and 2008 and subsequently 81% of patients with primary hip arthroscopy undergoing repair between 2016 and 2022.
With the recognition of hip dysplasia as a risk factor for early hip osteoarthritis, rates of PAO have increased over the past decade. Intra-articular pathologies such as labral tears and acetabular chondral lesions are common in the setting of hip dysplasia. 8 Therefore, addressing these issues at the time of PAO is important for optimization of hip preservation. Hip arthroscopy and PAO can be done concomitantly or as staged procedures. 24 The first combined PAO and hip arthroscopy at our center was performed in 2012, and the peak volume occurred in 2017 with 45 cases. Ruzbarsky et al 31 demonstrated improvements in patient-reported outcomes and arthroplasty-free survival in patients who underwent single-stage combined hip arthroscopy and PAO. Another study by Wyles et al 36 demonstrated similar outcomes for hip arthroscopy versus limited open arthrotomy for addressing intra-articular pathology at the time of PAO. Although patient-reported outcomes and rates of open arthrotomy were beyond the scope of our current study, the rate of combined hip arthroscopy and PAO increased significantly over the study period, with 11% of patients between 2016 and 2022 undergoing a simultaneous hip arthroscopy and PAO (P = .04), highlighting the evolution of comprehensive intra- and periarticular management of dysplasia over time.
Several additional procedures including iliopsoas fractional lengthening and arthroscopic abductor repair became more common throughout the time period analyzed. Iliopsoas fractional lengthening and arthroscopic abductor repair may both be performed independently or in combination with intra-articular arthroscopic hip procedures. 28 Psoas fractional lengthening is useful for the treatment of symptomatic internal snapping hip and iliopsoas impingement. 13 Perets et al 27 reported approximately 92% resolution of painful snapping in athletes who underwent psoas fractional lengthening. While patients who undergo iliopsoas tenotomy have been reported to have lower patient-reported outcomes compared with patients without tenotomy, iliopsoas fractional lengthening preserves a portion of the iliopsoas muscle-tendon complex and has been shown to improve symptomatic iliopsoas impingement.9,22 Psoas fractional lengthening may also be an option for patients with painful snapping or impingement following THA. In our study, 460 arthroscopic iliopsoas fractional lengthenings were performed, with 67 (14.6%) occurring in the setting of a prosthetic hip. Additional extracapsular procedures such as arthroscopic trochanteric bursectomy and abductor repair were also performed at our center during the study period. The first arthroscopic abductor repair at our center occurred in 2014, with a mean of 5 cases per year performed over the past 5 years. Recent studies have demonstrated similar excellent results for both open and arthroscopic abductor repair. 1 To date, relative indications of arthroscopic versus open abductor repair continue to evolve.
Limitations
Our study must be viewed considering certain important limitations. First, it had the limitations inherent to retrospective studies including a potential for missing cases, incomplete operative data, and heterogeneity of the definitions of certain procedures over the long study period. However, our institutional database prospectively documents surgical information and is available for case-by-case review including intraoperative images, thus mitigating this risk. Additionally, patient-reported outcomes and the effects of evolving indications and techniques are beyond the scope of the current study and not reported. Last, the volume of specific surgical procedures may have been affected by institutional variables such as surgeon experience and specialization as well as the fact that clinical trials intermittently dictated when certain procedures would be performed at our institution during the study period, such as was the case for hip capsular repair in the 2018-2020 time period during which we were actively enrolling patients in a randomized trial investigating capsular repair.
Conclusion
There has been a significant growth of hip arthroscopy volumes as well as a transition from its use as a diagnostic tool with labral debridement to its application for therapeutic procedures restoring native anatomy including labral repair, cam resection, capsular repair, concurrent PAO, and gluteus medius repair.
Footnotes
Final revision submitted February 20, 2024; accepted March 18, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: Support from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund. M.M.C. has received education payments from Arthrex and Team 1, consulting fees from Arthrex, and royalties from Arthrex. K.J.E. has received education payments from Goode Surgical and nonconsulting fees from Arthrex. A.J.K. has received a grant from DJO; consulting fees from Arthrex, JRF Ortho, and Responsive Arthroscopy; nonconsulting fees from Arthrex; royalties from Arthrex; and honoraria from JRF Ortho and MTF Biologics. B.A.L. has received consulting fees from Arthrex and Smith & Nephew; nonconsulting fees from Arthrex, Smith & Nephew, and Linvatec; and royalties from Arthrex. M.H. has received financial or material support from Elsevier; education payments from Arthrex, Foundation Medical, Medwest Associates, and Smith & Nephew; consulting fees from Vericel, DJO, and Moximed; royalties from Elsevier; honoraria from Encore Medical; and hospitality payments from Orthalign, Stryker, and Medical Device Business Services. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Mayo Clinic (PR08-002259-15).
ORCID iDs: Aaron J. Krych  https://orcid.org/0000-0003-3248-8007
https://orcid.org/0000-0003-3248-8007
Mario Hevesi  https://orcid.org/0000-0001-6208-878X
https://orcid.org/0000-0001-6208-878X
References
- 1. Alpaugh K, Chilelli BJ, Xu S, Martin SD. Outcomes after primary open or endoscopic abductor tendon repair in the hip: a systematic review of the literature. Arthroscopy. 2015;31(3):530-540. doi: 10.1016/j.arthro.2014.09.001 [DOI] [PubMed] [Google Scholar]
- 2. Bodendorfer BM, Alter TD, Carreira DS, et al. Multicenter outcomes after primary hip arthroscopy: a comparative analysis of two-year outcomes after labral repair, segmental labral reconstruction, or circumferential labral reconstruction. Arthroscopy. 2022;38(2):352-361. doi: 10.1016/j.arthro.2021.05.013 [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Chan V, Valone FH, III, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8):140-143. doi: 10.1016/j.arth.2013.02.039 [DOI] [PubMed] [Google Scholar]
- 4. Bryan AJ, Poehling-Monaghan K, Krych AJ, Levy BA, Trousdale RT, Sierra RJ. Factors associated with failure of hip arthroscopy in patients with hip dysplasia. Orthopedics. 2018;41(2):e234-e239. doi: 10.3928/01477447-20180123-02 [DOI] [PubMed] [Google Scholar]
- 5. Burman MS. Arthroscopy or the direct visualization of joints: an experimental cadaver study. J Bone Joint Surg Am. 1931;13(4):669-695. [DOI] [PubMed] [Google Scholar]
- 6. Byrd JT. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10(3):275-280. doi: 10.1016/s0749-8063(05)80111-2 [DOI] [PubMed] [Google Scholar]
- 7. Byrd JT, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739-746. doi: 10.1007/s11999-008-0659-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014;472(2):674-680. doi: 10.1007/s11999-013-3140-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Domb BG, Maldonado DR. Editorial commentary: indiscriminate iliopsoas tenotomy may cause complications—with tight indications and transbursal lengthening, we may avoid them. Arthroscopy. 2021;37(7):2149-2151. doi: 10.1016/j.arthro.2021.04.065 [DOI] [PubMed] [Google Scholar]
- 10. Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31(4):643-650. doi: 10.1016/j.arthro.2014.10.014 [DOI] [PubMed] [Google Scholar]
- 11. Economopoulos KJ, Chhabra A, Kweon C. Prospective randomized comparison of capsular management techniques during hip arthroscopy. Am J Sports Med. 2020;48(2):395-402. doi: 10.1177/0363546519894301 [DOI] [PubMed] [Google Scholar]
- 12. Ekhtiari S, de Sa D, Haldane CE, et al. Hip arthroscopic capsulotomy techniques and capsular management strategies: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):9-23. doi: 10.1007/s00167-016-4411-8 [DOI] [PubMed] [Google Scholar]
- 13. El Bitar YF, Stake CE, Dunne KF, Botser IB, Domb BG. Arthroscopic iliopsoas fractional lengthening for internal snapping of the hip: clinical outcomes with a minimum 2-year follow-up. Am J Sports Med. 2014;42(7):1696-1703. doi: 10.1177/0363546514531037 [DOI] [PubMed] [Google Scholar]
- 14. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. doi: 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 15. Gillinov SM, Kim DN, Moran J, et al. Low rates of 5-year secondary surgery and postoperative complications after primary hip arthroscopy in more than 30,000 patients. Arthroscopy. 2023;39(7):1639-1648. doi: 10.1016/j.arthro.2023.01.100 [DOI] [PubMed] [Google Scholar]
- 16. Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy. 1987;3(1):4-12. doi: 10.1016/s0749-8063(87)80003-8 [DOI] [PubMed] [Google Scholar]
- 17. Hale RF, Melugin HP, Zhou J, et al. Incidence of femoroacetabular impingement and surgical management trends over time. Am J Sports Med. 2021;49(1):35-41. doi: 10.1177/0363546520970914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jackson RW. From the scalpel to the scope: the history of arthroscopy. In: Jackson RW, ed. Baylor University Medical Center Proceedings. Vol 9. Taylor & Francis; 1996:77-79. [Google Scholar]
- 19. Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA. Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):763-767. doi: 10.1007/s00167-014-2872-1 [DOI] [PubMed] [Google Scholar]
- 20. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53. doi: 10.1016/j.arthro.2012.07.011 [DOI] [PubMed] [Google Scholar]
- 21. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32(3):750-755. doi: 10.1016/j.arth.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 22. Matsuda D, Kivlan BR, Nho SJ, et al. Tenotomy for iliopsoas pathology is infrequently performed and associated with poorer outcomes in hips undergoing arthroscopy for femoroacetabular impingement. Arthroscopy. 2021;37(7):2140-2148. doi: 10.1016/j.arthro.2021.02.018 [DOI] [PubMed] [Google Scholar]
- 23. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661-665. doi: 10.1016/j.arthro.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 24. Orner CA, Haws BE, Reuter J, Kenney R, Cook PC, Giordano BD. Patient-reported outcomes are similar in the first 2 years after staged versus combined hip arthroscopy and periacetabular osteotomy for hip dysplasia. Arthroscopy. 2023;39(8):1857-1865. doi: 10.1016/j.arthro.2023.02.017 [DOI] [PubMed] [Google Scholar]
- 25. Palmer AJ, Malak TT, Broomfield J, et al. Past and projected temporal trends in arthroscopic hip surgery in England between 2002 and 2013. BMJ Open Sport Exerc Med. 2016;2(1):e000082. doi: 10.1136/bmjsem-2015-000082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Patel KA, Collins MS, Cazan BA, Krych AJ, Levy BA, Hartigan DE. Iliopsoas release in hip arthroscopy: assessment of muscle atrophy. Orthopedics. 2020;43(3):e171-e176. doi: 10.3928/01477447-20200314-06 [DOI] [PubMed] [Google Scholar]
- 27. Perets I, Hartigan DE, Chaharbakhshi EO, Ashberg L, Mu B, Domb BG. Clinical outcomes and return to sport in competitive athletes undergoing arthroscopic iliopsoas fractional lengthening compared with a matched control group without iliopsoas fractional lengthening. Arthroscopy. 2018;34(2):456-463. doi: 10.1016/j.arthro.2017.08.292 [DOI] [PubMed] [Google Scholar]
- 28. Perets I, Rybalko D, Mu BH, Friedman A, Morgenstern DR, Domb BG. Hip arthroscopy: extra-articular procedures. Hip Int. 2019;29(4):346-354. doi: 10.1177/1120700019840729 [DOI] [PubMed] [Google Scholar]
- 29. Riff AJ, Kunze KN, Movassaghi K, et al. Systematic review of hip arthroscopy for femoroacetabular impingement: the importance of labral repair and capsular closure. Arthroscopy. 2019;35(2):646-656.e3. doi: 10.1016/j.arthro.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 30. Röling MA, Mathijssen NM, Bloem RM. Incidence of symptomatic femoroacetabular impingement in the general population: a prospective registration study. J Hip Preserv Surg. 2016;3(3):203-207. doi: 10.1093/jhps/hnw009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ruzbarsky JJ, Comfort SM, Rutledge JC, et al. Improved functional outcomes of combined hip arthroscopy and periacetabular osteotomy at minimum 2-year follow-up. Arthroscopy. 2024;40(2):352-358. doi: 10.1016/j.arthro.2023.06.034 [DOI] [PubMed] [Google Scholar]
- 32. Shukla S, Pettit M, Kumar KHS, Khanduja V. History of hip arthroscopy. J Arthrosc Surg Sports Med. 2020;1(1):73-80. doi: 10.25259/JASSM_21_2020 [DOI] [Google Scholar]
- 33. Strickland CD, Kraeutler MJ, Brick MJ, et al. MRI evaluation of repaired versus unrepaired interportal capsulotomy in simultaneous bilateral hip arthroscopy: a double-blind, randomized controlled trial. J Bone Joint Surg Am. 2018;100(2):91-98. doi: 10.2106/JBJS.17.00365 [DOI] [PubMed] [Google Scholar]
- 34. Suzuki S, Awaya G, Okada Y, Maekawa M, Ikeda T, Tada H. Arthroscopic diagnosis of ruptured acetabular labrum. Acta Orthop Scand. 1986;57(6):513-515. doi: 10.3109/17453678609014781 [DOI] [PubMed] [Google Scholar]
- 35. Watanabe M. Memories of the early days of arthroscopy. Arthroscopy. 1986;2(4):209-214. doi: 10.1016/s0749-8063(86)80073-1 [DOI] [PubMed] [Google Scholar]
- 36. Wyles CC, Hevesi M, Bartels DW, Larson DR, Sierra RJ, Trousdale RT. Arthroscopy and arthrotomy to address intra-articular pathology during PAO for hip dysplasia demonstrates similar short-term outcomes. J Hip Preserv Surg. 2018;5(3):282-295. doi: 10.1093/jhps/hny022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wyles CC, Norambuena GA, Howe BM, et al. Cam deformities and limited hip range of motion are associated with early osteoarthritic changes in adolescent athletes: a prospective matched cohort study. Am J Sports Med. 2017;45(13):3036-3043. doi: 10.1177/0363546517719460 [DOI] [PubMed] [Google Scholar]
- 38. Zhou J, Melugin HP, Hale RF, et al. The prevalence of radiographic findings of structural hip deformities for femoroacetabular impingement in patients with hip pain. Am J Sports Med. 2020;48(3):647-653. doi: 10.1177/0363546519896355 [DOI] [PubMed] [Google Scholar]
- 39. Zusmanovich M, Haselman W, Serrano B, Banffy M. The incidence of hip arthroscopy in patients with femoroacetabular impingement syndrome and labral pathology increased by 85% between 2011 and 2018 in the United States. Arthroscopy. 2022;38(1):82-87. doi: 10.1016/j.arthro.2021.04.049 [DOI] [PubMed] [Google Scholar]