Abstract
Cardiovascular diseases (CVD) and mental health disorders (MHD) are respectively the first and second most prevalent diseases in high-income countries and the two most relevant causes of disability worldwide. The close association between the two conditions has been known for a long time and research has been able to document how the co-morbidity between cardiovascular disorders and mental health disorders is a negative prognostic factor for both conditions. This strong connection and the relevance of the impact of the association have led to define a new branch of cardiology, known as behavioral cardiology. The aim of the new branch is just to study the nexus CVD-MHD in order to prevent or decrease the burden of MHD on CVD and vice versa. This review describes the epidemiological evidence of the relationship between MHD on CVD at the state of the art among clinical research.
Keywords: Cardiovascular disease, myocardial infarction, heart failure, mental health disorders, psychiatric disorder, depressive disorders, bipolar disorder, anxiety disorder, schizophrenia, stress disorders
Introduction
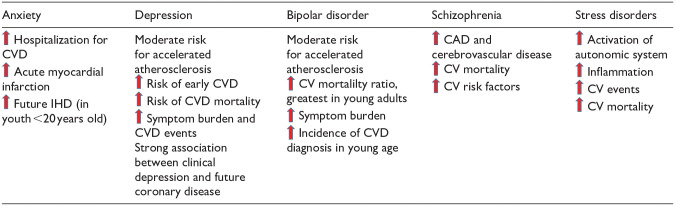
About 10% of adults in Western countries live with an MHD. 1 MHD is a group of medical and psychosomatic conditions characterized by behavioral or cognitive dysfunction that leads to a mid or to relevant psychosocial disability with impairment in social, occupational, and emotional areas. Among MHD the most prevalent in CVD are depressive, bipolar, anxiety disorder, and schizophrenia. 2 People with MHD have a shorter life expectancy respect the general population, and CVD plays a relevant role in the premature deaths of people with MHD.3,4 The excess of cardiovascular disease-related mortality in people with MHD is multifactorial (Table 1).
Table 1.
Prevalence and mortality of cardiovascular disease in patients with psychiatric disorders.
|
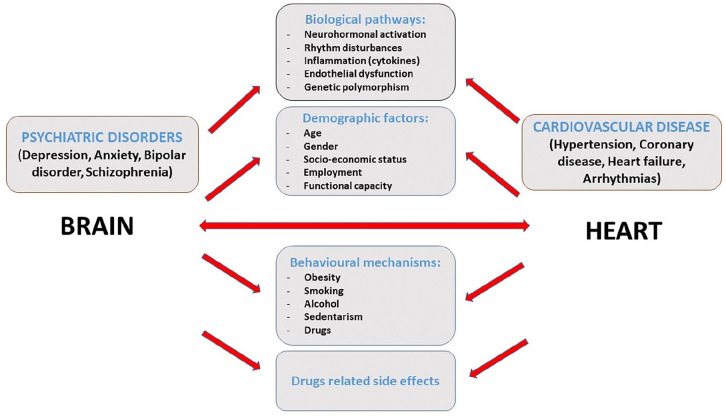
It may be connected to an high prevalence of modifiable cardiovascular risk factors, underestimation of cardiovascular risk and symptoms and therefore cardiovascular pathologies are often undertreated in these patients. Furthermore, many psychotropic medication have important cardiovascular side effects and the same psychiatric pathology. Additionally, it may be related to an increased prevalence of less investigated risk factors such as inflammation, 5 high-risk lipoproteins and insulin resistance. 6 However the relationship of PD and CVD appears to be bidirectional (Figure 1). Acute coronary events and chronic cardiovascular disease as heart failure indeed may promote the onset of mental disorders specifically anxiety disorders, but also mood and schizoaffective disorders have been found. 7
Figure 1.
Relationship between psychiatric disorders & cardiovascular disease.
Depressive disorders
Major Depressive Disorder represents the most prevalent MHD affecting approximately 5% of adults globally. 8 Depressive Disorders are intricate conditions characterized by psychological symptoms, including persistent low mood, feelings of hopelessness, a lack of motivation or interest in activities, and, in severe cases, suicidal ideation. They are also accompanied by physical symptoms such as chronic fatigue, disrupted sleep patterns, and unexplained pains.
The prevalence of Major Depressive Disorders in individuals with CVD varies depending on the impact of CVD on life expectancy and quality of life.9,10 Notably, Major Depressive Disorder is often diagnosed in the aftermath of Acute Myocardial Infarction (AMI) and in the context of Chronic Heart Failure (CHF), with estimated prevalence rates of approximately 15% and 20%, respectively. 11 These prevalence rates are higher compared to those found in the general population, thus a possible causative role of CVD on the onset of depressive disorders was suggested. A shared element between CVD and depressive disorders is autonomic dysfunction characterized by sympathetic nervous system hyperactivity and parasympathetic hypoactivity. Several studies have postulated that in patients with specific genetic predispositions, the autonomic system imbalance induced by CVD may act as a trigger for depression onset.12,13 Concurrently, numerous studies have established a strong association between depressive disorders and the development of CVD, particularly AMI14,15 and Takotsubo syndrome.16,17 A recent study by Sancassiani et al. demonstrated a link between Takotsubo Syndrome and mood disorders, including depression. 16 Individuals with both depressive disorders and CVD often exhibit additional risk factors such as obesity, physical inactivity, smoking, hypertension, and metabolic syndrome. Some of these risk factors may be attributed, at least in part, to the metabolic side effects of various antidepressant medications, including tricyclic antidepressants, Selective Serotonin Reuptake Inhibitors (SSRIs), and serotonin/norepinephrine reuptake inhibitors (SNRIs). The use of these medications is known to be an independent risk factor for CVD. 18 Furthermore, emerging data and preliminary ongoing trials indicate that individuals with depressive disorders, compared to control groups without such disorders, show upregulation of the TNF-alpha and IL-6 pathways and prothrombotic states. These altered pro-inflammatory responses may facilitate the development of atherosclerotic lesions in the arterial system and exacerbate endothelial dysfunction. 19 The multinational case-control INTERHEART study unequivocally establishes that psychosocial factors, such as depressive disorders, represent one of the four most significant contributors to CVD, particularly AMI, independently of the underlying mechanisms. These factors operate in conjunction with the Apolipoprotein B/Apolipoprotein A ratio, smoking, and diabetes. 20 Consequently, the co-occurrence of depressive disorder is a powerful predictor of post-AMI survival and in CHF patients up to two to three fold increase mortality compared to the general population.14–21
Bipolar disorder
Bipolar disorder (BD) is a multisystemic disorder, characterized by depressive and manic episodes interspaced with normal euthymic periods, that lead to extreme fluctuation of a person’s mood, energy, and social relationship. The current lifetime prevalence of BD is around 2% worldwide and about 3%–5% in people with cardiac illnesses. 8 As well as in other MHD, there is a strong relationship between BD and CVD. Patients affected by BP indeed have a higher prevalence of medical conditions which are themselves cardiovascular risk factors such as hypertension, insulin resistance, diabetes, alcoholism, and smoking. 22 Additionally, pharmacotherapy for BP can also increase cardiovascular risk. Both mood stabilizers lithium and valproic acid indeed cause some amount of weight increase according to dosage and duration of therapy. The obesity is an important prognostic factor in BD, in which is associated with a poorer outcome due to a lower therapeutic response to drugs, but also due to the increasing risk of having cardiovascular events. 23 As a result in several studies BP is associated with 1.5 to 2.5 fold increased risk of CVD compared to general population. 24 CVD are also the most common cause of death in people with BP being responsible for 35%–40% of the excess mortality. 25
Anxiety disorder
Anxiety Disorder (AD) is a highly prevalent MHD that significantly impairs daily functioning and overall well-being. The prevalence of AD exhibits regional disparities, ranging from 3.8% to 10.4% in Anglo-Saxon countries and 3.2% to 6.2% in Eastern and Central Europe. The highest prevalence of AD is observed in specific subgroups such as women, young individuals, and those suffering with chronic medical conditions. 26 Clinical presentations of AD encompass a spectrum of cardiorespiratory symptoms, including palpitations, tachycardia, chest discomfort, breathlessness, disorientation, and gastric distress. Additional signs, which might manifest subtly and remain unrecognized, include behavioral (fear of places or circumstances, protection seeking) and cognitive impairment (e.g. catastrophic thinking, thoughts repression). AD exhibits a noteworthy association with CVD. Recent meta-analysis data reveals that 16% of individuals with CVD concurrently experience AD. AD is notably more prevalent in CVD patients compared to the general population, with 50% of CVD patients experiencing concurrent AD and depression. 27 Importantly, AD independently correlates with adverse prognostic outcomes in individuals with preexisting CVD, particularly in the context of CAD. Individuals with AD are approximately twice as likely to face an elevated risk of mortality over the ensuing decade following a Myocardial Infarction (MI). 28 Similarly, in individuals with stable CAD, AD is associated with a twofold higher risk of significant adverse cardiac events over the subsequent 2 years. 29 The exact link connecting AD and CVD is still unknown, but several potential mechanisms have been proposed. The prevailing hypothesis posits that anxiety exerts a sustained influence on the function of the autonomic nervous system. According to this model, AD triggers an excessive activation of the hypothalamic-pituitary-adrenal axis and sympathetic nervous system, resulting in elevated production of plasma catecholamines and endothelial dysfunction. 30 The emotional triggering theory instead, in which the time of association between the two conditions is crucial, is an alternative hypothesis that could underlie contradictory results in epidemiological researches as well as conflicting mechanistic investigations.
Furthermore, acute anxiety is associated with heightened cardiovascular responsiveness to stress, tachycardia, reduced heart rate variability, impaired baroreflex function, and greater variability in ventricular repolarization. 31 Additionally, individuals with AD, as well as other psychiatric disorders, are inclined toward unhealthy lifestyle choices, such as smoking, excessive alcohol consumption, physical inactivity, and poor dietary habits, all of which heighten the risk of developing CVD. 32 Furthermore, CVD initiation and progression may be influenced by a persistent state of inflammation, whose markers consistently elevated in individuals with AD.33,34
Schizophrenia
Schizophrenia is a chronic MHD with negative impact on quality of life, being the seventh disease for years-lost-due-disability. The prevalence of schizophrenia varies between 0.33% and 0.75% globally. Schizophrenia is linked to serious clinical, social, and economic issues as well as a higher chance of dying before expected time. 35 The typical symptoms of Schizophrenia are hallucinations (typically hearing voices), disorganized thinking and delusions.
The clinical course of Schizophrenia is characterized by episodes of psychosis sometimes continuous or relapsing. The disorder typically begin during young adulthood and develop gradually involving social withdrawal and decreased emotional expression. The disorder is frequently chronic, severe, and incapacitating. CVDs is the main cause of death in schizophrenia, even higher than suicide and high-risk behaviors. In a comprehensive metanalysis, schizophrenia was found to be substantially linked to CVD, like CAD and cerebrovascular disease, and to CVD-related mortality. 24 Numerous studies have showed the potential similar pathophysiological factors between schizophrenia and CVD. Genomic association analyses indeed have highlighted genetical and biochemical connections connecting schizophrenia and CVD. Andreassen et al. found 16 novel loci, many of which are connected to CVDs and verified 9 single nucleotide polymorphisms previously related to schizophrenia. 36 A significant component of the rise in risk for CVD can be attributed to the metabolic syndrome, whose prevalence is higher in patients with schizophrenia. Research shows indeed that schizophrenia and metabolic syndrome may also share a variety of pathophysiological characteristics, like mitochondrial malfunction and neuro-inflammation. 37 Furthermore numerous typical and atypical antipsychotic drugs used in the treatment can lead to metabolic syndrome and as a result to a CVD. In addition to metabolic syndrome antipsychotic drugs can lengthen the QRS complex and QT interval leading to arrhythmias, even though the second generation of antipsychotics have a decreased frequency of sudden cardiac death and a decreased risk of pro-arrhythmic episodes compared to the first. 38 In addition to the conventional risk variables utilizing the Framingham heart study formula, the administration of olanzapine, quetiapine, risperidone, and perphenazine increased the incidence of coronary events. 39 Cardiomyopathy and myocarditis brought on by clozapine are also a serious problem. Cardiomyopathy is likely the result of reduced parasympathetic activity and higher adrenergic tone due to clozapine that leads to tachycardia during rest, that whether prolonged can seriously harm the left ventricular (LV) function. According to Rostagno et al. indeed, in 1/3 of subjects who started clozapine, occurs a >5% decline in LV ejection fraction at 1 year. 40 Myocarditis induced by clozapine is instead due to a sudden increase in blood catecholamines that lead to by unknown immunological mechanisms to a severe and potentially fatal cardiac inflammation. 41
Stress disorders
There is growing proof indicating being exposed to long-term stresses on a regular basis and serious psychic trauma may rise the chance of getting CVD and CV death, as people exposed to work-related stress that have a 40% increased risk of CVD. In individuals with pre-existing CVD, chronic stresses are additionally related to a poorer outcome. 42 A correlation between new CV events, CV mortality and post-traumatic stress disorder (PTSD) has been evaluated by several cohort investigations. A recent study on US soldiers found that soldiers gone in war have a noticeably elevated incidence of CV events. There was a higher risk of self-report CHD diagnosis in individuals who have PTSD signs, compared to individuals who did not. 43 A separate research in soldiers without established CHD discovered that individuals with PTSD had greater quantities of coronary calcium with CT, a sign of atherosclerosis. 44 Stress-induced ischemia frequently may not result in chest pain or similar conventional ischemic signs. Myocardial microvascular impairment can be noticed, and it causes unusual sensations including exhaustion and non-specific pain. For these reasons, stress is linked to a greater chance of subsequent CV events and greater risk of death. 45 Maybe a combination of stress-related acute ischemia and atherosclerosis progression are involved in the pathophysiological process. Other physiologic factors, such as heightened activation of the axis that connects the hypothalamus to the pit and the adrenergic system, the autonomic system, and inflammation, might be contributing factors. 46 Regardless of the pathophysiology, stress-related disorders are currently an epidemic poised to grow in the coming years. In this perspective, several evidence have emphasized the importance of physical exercise in reducing stress levels and consequently the associated cardiovascular risks. Recent reviews have summarized these evidence supporting the significant benefits of physical activity in this scenery, emphasizing how this, in combination with mind-body stress therapies such as yoga or behavioral strategies, provides strong benefits in reducing stress levels and fighting the burden of cardiovascular diseases.47,48 However more studies are required to deeply investigate the exactly impact of physical activity on pathophysiology of stress disorders and cardiovascular diseases.
Conclusion
In this review we have described the current evidence suggesting the presence of common pathogenic mechanisms between PD and CVD that often lead to a coexistence of two conditions in the same patient. The relationship appears to be mediated by both behavioral and physiologic mechanisms, including inflammation, alterations in the autonomic nervous system, neurohormonal factors, genetic linkages. A strict control of cardiovascular risk factors and periodic cardiologic visits combined with instrumental tests such as echocardiography could be useful to detect early abnormalities of the systolic and diastolic myocardial function both in primary and secondary prevention of CVD in patients with MHD 49 as well as cardiac and psychological rehabilitation programs could represent a valid tool in people with cardiac diseases to prevent the onset of PD. 50 In summary what is good for the heart is good for the brain and vice versa. 51 However further studies needed to be performed to understand even better the sharing mechanisms between CVD and PD in order to control the mutual influence achieving a reduce of morbidity and mortality related to the twice condition.
Significance for public health
This research investigated the close relationship between cardiovascular diseases and psychiatric disorders, which are the first and second leading causes of illness in industrialized countries, respectively. The significance of this research lies in the fact that a better and increasingly in-depth understanding of the common mechanisms underlying these conditions would enable the development of improve treatments and effective screening methods to improve public health while simultaneously reducing the burden of these two diseases on national healthcare systems.
Acknowledgments
We express thanks to Dr. Iervolino and Dr. Madaudo for their contribution to research and for their valuable advice.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Roberta Montisci  https://orcid.org/0000-0002-7218-6751
https://orcid.org/0000-0002-7218-6751
References
- 1. National Institute of Mental Health Illness 2021, https://www.nimh.nih.gov/health/statics/mental-illness
- 2. Peck MC, Scheffler RM. An analysis of the definitions of mental illness used in state parity laws. Psychiatr Serv 2002; 53(9): 1089–1095. [DOI] [PubMed] [Google Scholar]
- 3. Ringen PA, Engh JA, Birkenaes AB, et al. Increased mortality in schizophrenia due to cardiovascular disease - a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry 2014; 5: 137–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chang CK, Hayes RD, Broadbent M, et al. All-cause mortality among people with serious mental illness (SMI), substance use disorders, and depressive disorders in southeast London: a cohort study. BMC Psychiatry 2010; 10: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sarwar N, Butterworth A, Freitag D, et al. L6R Genetics Consortium Emerging Risk Factors Collaboration. Lancet 2012; 379(9822): 1205–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gans RO. The metabolic syndrome, depression, and cardiovascular disease: interrelated conditions that share pathophysiologic mechanisms. Med Clin North Am 2006; 90(4): 573–591. [DOI] [PubMed] [Google Scholar]
- 7. Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens 2015; 28(11): 1295–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Depression and other common mental disorders: global health estimates, https://www.who.int (2017).
- 9. Colquhoun DM, Bunker SJ, Clarke DM, et al. Screening, referral and treatment for depression in patients with coronary heart disease. Med J Aust 2013; 198(9): 483–484. [DOI] [PubMed] [Google Scholar]
- 10. Cooney MT, Kotseva K, Dudina A, et al. Determinants of risk factor control in subjects with coronary heart disease: a report from the EUROASPIRE III Investigators. Eur J Prev Cardiol 2013; 20(4): 686–691. [DOI] [PubMed] [Google Scholar]
- 11. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006; 48(8): 1527–1537. [DOI] [PubMed] [Google Scholar]
- 12. Frenneaux MP. Autonomic changes in patients with heart failure and in post-myocardial infarction patients. Heart 2004; 90(11): 1248–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stein PK, Carney RM, Freedland KE, et al. Severe depression is associated with markedly reduced heart rate variability in patients with stable coronary heart disease. J Psychosom Res 2000; 48(4-5): 493–500. [DOI] [PubMed] [Google Scholar]
- 14. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J 2006; 27(23): 2763–2774. [DOI] [PubMed] [Google Scholar]
- 15. Wu Q, Kling JM. Depression and the risk of myocardial infarction and coronary death: a meta-analysis of prospective cohort studies. Medicine 2016; 95(6): e2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sancassiani F, Carta MG, Montisci R, et al. Takotsubo syndrome is associated with mood disorders and antidepressants use, not with anxiety and impairment of quality of life due to the psychiatric disorder. Clin Pract Epidemol Ment Health 2018; 14: 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stiermaier T, Walliser A, El-Battrawy I, et al. Happy Heart Syndrome: frequency, characteristics, and outcome of Takotsubo syndrome triggered by positive life events. JACC Heart Fail 2022; 10(7): 459–466. [DOI] [PubMed] [Google Scholar]
- 18. Stapelberg NJ, Neumann DL, Shum DH, et al. A topographical map of the causal network of mechanisms underlying the relationship between major depressive disorder and coronary heart disease. Aust N Z J Psychiatr 2011; 45(5): 351–369. [DOI] [PubMed] [Google Scholar]
- 19. Haapakoski R, Mathieu J, Ebmeier KP, et al. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun 2015; 49: 206–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364(9438): 937–952. [DOI] [PubMed] [Google Scholar]
- 21. Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161(15): 1849–1856. [DOI] [PubMed] [Google Scholar]
- 22. Kupfer DJ. The increasing medical burden in bipolar disorder. JAMA 2005; 293(20): 2528–2530. [DOI] [PubMed] [Google Scholar]
- 23. Fagiolini A, Kupfer DJ, Houck PR, et al. Obesity as a correlate of outcome in patients with bipolar I disorder. Am J Psychiatr 2003; 160(1): 112–117. [DOI] [PubMed] [Google Scholar]
- 24. Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 2017; 16(2): 163–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Miller C, Bauer MS. Excess mortality in bipolar disorders. Curr Psychiatry Rep 2014; 16(11): 499. [DOI] [PubMed] [Google Scholar]
- 26. Remes O, Brayne C, van der Linde R, et al. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav 2016; 6(7): e00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tully PJ, Cosh SM, Baumeister H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. J Psychosom Res 2014; 77(6): 439–448. [DOI] [PubMed] [Google Scholar]
- 28. Roest AM, Zuidersma M, de Jonge P. Myocardial infarction and generalised anxiety disorder: 10-year follow-up. Br J Psychiatry 2012; 200(4): 324–329. [DOI] [PubMed] [Google Scholar]
- 29. Frasure-Smith N, Lespérance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 2008; 65(1): 62–71. [DOI] [PubMed] [Google Scholar]
- 30. Roest AM, Martens EJ, de Jonge P, et al. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010; 56(1): 38–46. [DOI] [PubMed] [Google Scholar]
- 31. Rozanski A, Blumenthal JA, Davidson KW, et al. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005; 45(5): 637–651. [DOI] [PubMed] [Google Scholar]
- 32. Antonogeorgos G, Panagiotakos DB, Pitsavos C, et al. Understanding the role of depression and anxiety on cardiovascular disease risk, using structural equation modeling; the mediating effect of the Mediterranean diet and physical activity: the ATTICA study. Ann Epidemiol 2012; 22(9): 630–637. [DOI] [PubMed] [Google Scholar]
- 33. Ross R. Atherosclerosis’an inflammatory disease. N Engl J Med 1999; 340(2): 115–126. [DOI] [PubMed] [Google Scholar]
- 34. Pitsavos C, Panagiotakos DB, Papageorgiou C, et al. Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study. Atherosclerosis 2006; 185(2): 320–326. [DOI] [PubMed] [Google Scholar]
- 35. National Institute on mental health. Schizophrenia, https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml
- 36. Andreassen OA, Djurovic S, Thompson WK, et al. Improved detection of common variants associated with schizophrenia by leveraging pleiotrophy with cardiovascular-disease risk factors. Am J Hum Genet 2013; 92(2): 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Herbsleb M, Schumann A, Malchow B, et al. Chronotropic incompetence of the heart is associated with exercise intolerance in patients with schizophrenia. Schizophr Res 2018; 197: 162–169. [DOI] [PubMed] [Google Scholar]
- 38. Mitcheson JS, Chen J, Lin M, et al. A structural basis for drug-induced long QT syndrome. Proc Natl Acad Sci USA 2000; 97(22): 12329–12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Daumit GL, Goff DC, Meyer JM, et al. Antipsychotic effects on estimated 10-year coronary heart disease risk in the CATIE schizophrenia study. Schizophr Res 2008; 105(1-3): 175–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rostagno C, Domenichetti S, Gensini GF, et al. Does a subclinical cardiotoxic effect of clozapine exist? Results from a follow-up pilot study. Cardiovasc Hematol Agents Med Chem 2012; 10(2): 148–153. [DOI] [PubMed] [Google Scholar]
- 41. Kilian JG, Kerr K, Lawrence C, et al. Myocarditis and cardiomyopathy associated with clozapine. Lancet 1999; 354(9193): 1841–1845. [DOI] [PubMed] [Google Scholar]
- 42. Steptoe A, Kivimäki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health 2013; 34: 337–354. [DOI] [PubMed] [Google Scholar]
- 43. Crum-Cianflone NF, Bagnell ME, Schaller E, et al. Impact of combat deployment and posttraumatic stress disorder on newly reported coronary heart disease among US active duty and reserve forces. Circulation 2014; 129(18): 1813–1820. [DOI] [PubMed] [Google Scholar]
- 44. Ahmadi N, Hajsadeghi F, Mirshkarlo HB, et al. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol 2011; 108(1): 29–33. [DOI] [PubMed] [Google Scholar]
- 45. Jiang W, Samad Z, Boyle S, et al. Prevalence and clinical characteristics of mental stress-induced myocardial ischemia in patients with coronary heart disease. J Am Coll Cardiol 2013; 61(7): 714–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wood SK, Wood CS, Lombard CM, et al. Inflammatory factors mediate vulnerability to a social stress-induced depressive-like phenotype in passive coping rats. Biol Psychiatry 2015; 78(1): 38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Popovic D, Lavie CJ. Stress, cardiovascular diseases and exercise – a narrative review. Hear Mind 2023; 7(1): 18–24. [Google Scholar]
- 48. Popovic D, Bjelobrk M, Tesic M, et al. Defining the importance of stress reduction in managing cardiovascular disease - the role of exercise. Prog Cardiovasc Dis 2022; 70: 84–93. [DOI] [PubMed] [Google Scholar]
- 49. Montisci R, Cecchetto G, Ruscazio M, et al. Early myocardial dysfunction after chronic use of anabolic androgenic steroids: combined pulsed-wave tissue Doppler imaging and ultrasonic integrated backscatter cyclic variations analysis. J Am Soc Echocardiogr 2010; 23(5): 516–522. [DOI] [PubMed] [Google Scholar]
- 50. Holdgaard A, Eckhardt-Hansen C, Lassen CF, et al. Cognitive-behavioural therapy reduces psychological distress in younger patients with cardiac disease: a randomized trial. Eur Heart J 2023; 44(11): 986–996. [DOI] [PubMed] [Google Scholar]
- 51. O’Keefe EL, O’Keefe JH, Lavie CJ. The intersection of exercise, cognition, and cardiovascular disease. Hear Mind 2023; 7(1): 3–4. [Google Scholar]