Abstract
Background
Anti-seizure medications (ASMs) are the primary therapeutic mode to control seizures in patients with epilepsy. Adherence to the medications is critical to achieving the goals of epilepsy therapy. However, the cost of the medications and the interrupted availability of ASMs contribute to non-adherence to epilepsy treatment. Therefore, this study aimed to assess ASM adherence and its association with self-reported medication availability and affordability.
Objective
To assess whether self-reported availability and affordability of Anti-seizure medications affect medication adherence among Epileptic Patients at Eka Kotebe General Hospital, Addis Ababa, Ethiopia, from January 13, 2023 to March 23, 2023.
Methods
A hospital-based analytical cross-sectional study was conducted among 357 epileptic patients using the Consecutive sampling method in Eka Kotebe General Hospital, Addis Ababa, Ethiopia. ASM adherence was measured using a self-report 3items questionnaire focusing on medication use patterns of patients from their last visit to the current visit. Statistical packages for Social Sciences 26.0 version statistical software cleaned, coded and analyzed the collected data. Binary logistic regression was fitted, and P-values less than 0.05 were considered to have statistical significance.
Result
The prevalence of ASM adherence was 55.2% with 95% CI (50.1%; 60.2%). About two-thirds (61.3%) of patients in this study had limited access to the ASMs or could not afford the medications. Self-reported availability of ASMs (AOR = 2.01, 95% CI = 1.01, 3.98) was significantly associated with ASM adherence. Self-reported affordability of ASMs was associated with ASM adherence in the Bivariate logistic regression analysis; however, when adjusted for other covariates in the multivariable logistic regression, no significant association was observed (p = 0.674).
Conclusion and recommendation
Only about half of the epileptic patients adhered to ASMs at Eka Kotebe General Hospital. Self-reported availability of ASMs was an essential factor. Improving access to ASMs is critical to improving adherence and management of epilepsy.
Introduction
Medication adherence is the extent to which individuals take their medications as prescribed with respect to dosage and dosage intervals [1]. In both developed and developing countries, non-adherence to medication remains a significant concern for healthcare providers as well as patients because of its adverse consequences on therapeutic outcomes. It is significant, especially in chronic illnesses involving complex and long-term medical regimens [2].
Epilepsy is a common chronic neurological disease of the brain affecting 50 million people worldwide, of whom 40 million are estimated to live in developing countries [3]. Anti-seizure medications (ASMs) are the mainstay of long-term epilepsy treatment, and they are 70% effective at reducing epileptic attacks in adults [4]. However, about 90% of epileptic patients in developing countries are not receiving appropriate treatment due to cultural attitudes, lack of prioritization, poor healthcare system, and inadequate supply of anti-seizure medications (ASMs) [5].
In Ethiopia, epilepsy is often mistakenly seen as a form of mental illness by the Community and is usually treated by psychiatrists and psychiatric nurses. The most prescribed Anti-seizure medications are phenobarbitone, phenytoin, and sometimes carbamazepine and sodium Valproate.
A study in Western countries revealed an adherence rate of 71% in the US [6] and 59% in the UK [7]. The result was not different in Gondar, Ethiopia (70.8%) [8] and Jimma, Ethiopia (58.5%) [9]. On the other hand, the report was higher in India (98.6%) [10] and Palestine (85.3%) [11]. However, a lower adherence rate was found in China 51.9% [12], Nigeria (32.6%) [13], and South Africa (54.6%) [14].
The consequence of ASM nonadherence behavior has been associated with poor seizure control, increased morbidity and mortality along with increased time of hospitalization, worsened patient outcomes, poor quality of life, and increased healthcare cost. ASM nonadherence will also lead to an increase in the burden of inpatient and emergency department services; moreover, it also affects the family members socially, economically, and psychologically [15].
Availability and affordability of ASMs are poor and act as a barrier to accessing treatment for epilepsy in low and middle-income countries [16]. In most low-income countries, access to medicines remains very low. The availability and affordability of medications are two key factors that affect patients’ access to treatment. A study of the availability and prices of ASMs in southern Vietnam showed that only 57% of the public and private pharmacies surveyed had ASMs available [17]. A second study conducted in Zambia found that nearly one-half of the government, private, and nongovernmental organization (NGO) pharmacies surveyed did not carry ASMs [18]. There is a failure to explore these factors, particularly in Ethiopia.
A study done in Bangui, Central African Republic, on the Problem of accessibility to anti-seizure medications for patients who have epilepsy, shows that the lack of trained personnel, the inadequacy of pharmaceutical structures, the insufficient availability of anti-seizure medications, and their very high cost are factors limiting the accessibility of anti-seizure medications for epileptic patients [19].
This study aimed to evaluate medication availability and affordability from the patient’s point of view. This allows for a more direct assessment of the role of these factors in adherence. However, the studies and tools developed thus far were from a system perspective. Hence, this study aims to assess the association of self-reported medication availability and affordability with medication adherence. In addition, ASM adherence was also assessed to fill the gaps in epilepsy treatment.
Methodology
Study design and period
A hospital-based Analytical cross-sectional study with internal comparison was conducted from January 13, 2023 to March 23, 2023.
Study setting
The study was conducted at Eka Kotebe General Hospital, located in the eastern part of Addis Ababa, the capital city of Ethiopia. Eka Kotebe General Hospital was established as an extension of Amanuel Mental Specialized Hospital until April 2020, when it became a stand-alone federal hospital. The hospital has a dedicated clinic for patients with epilepsy. There were about 2478 epileptic patients who had regular follow-ups in a year at the outpatient department, and on average, 200 epilepsy patients have follow-ups at the hospital. Patients pay for the services they get from the hospital and for purchasing ASMs, except those who use CBHI (community-based health insurance). The hospital also gives psychiatric services at the outpatient level. In addition, the hospital has served as a dedicated inpatient COVID treatment center.
Source population
Adult epileptic patients who have been on treatment with one or more anti-seizure medications and who had follow-ups at the outpatient units during the study period.
Study population
We selected adult epileptic patients who have been on treatment with one or more anti-seizure medications and who had follow-up at the outpatient units during the study period, fulfilling the inclusion criteria.
Inclusion criteria
Adult Epileptic Patients (age≥18 years) who had a follow-up in the hospital for at least three months and received ASMs at the last visit were eligible for the study. Patients with general severe medical conditions and unable to communicate were excluded.
Sample size and sampling technique
The sample size for the first objective was determined using a single population proportion formula considering the following assumptions (z = 1.96, d = 0.05, and P = 65%) [20]. Second, an attempt was made to calculate the sample size by considering the association of medication availability and affordability with adherence using Open Epi version 2.3.1. Finally, the sample size we obtained from the first objective was the largest and was taken as our final sample. By considering a non-response rate of 10%, the final estimated sample size was 385.
Consecutive sampling was used to recruit samples for the study each day of the data collection process until the desired sample size was obtained.
Data collection tool and procedures
Data was collected using a structured questionnaire translated into a local language (Amharic) and pre-tested. Trained nurses interviewed volunteer participants face-to-face during their follow-up clinic visits. The data was collected after explaining the purpose of the study to the participants and earning informed written consent. The patient interview aimed to gather information related to sociodemographic, clinical factors, psychosocial factors, self-reported medication availability, affordability, and adherence. Their medical records were reviewed for the type of seizure and prescribed ASMs.
Adherence of epileptic patients to their ASMs was assessed using a self-reported questionnaire; in this study, a 3 items questionnaire focusing on medication use patterns of patients from their last visit to the current visit was used. Patients were asked 3questions: “Did you forget to take your medicine since your last visit?” “In the past two weeks, were there any days you did not take your medicine?” and “Did you take all your medicine yesterday?” The response choices were yes/no, and a response “no” was rated as “1,” and a “yes” response as “0,” except for item 3. For item 3, a response “yes” was rated as “1” and “no” as “0”. The total score ranges from 0 to 3, with scores of </ = 1, 1 to <3, and 3 reflecting low, medium, and high adherence, respectively. For data analysis, scores were categorized into two, scores <3 were assigned as non-adherent, and those who scored 3 were assigned as adherent.
Data quality control
To ensure the data quality, a data collection tool was prepared after reviewing the literature related to the study. Data was collected by 4 BSC nurses who know about epilepsy and a supervisor. A thorough training was given by the principal investigator about the general objective of the study and the contents of the questionnaire. The questionnaire was pre-tested a week before the data collection started on 10% of the sample size at Eka Kotebe General Hospital Outpatient units. After a thorough and deep review of inputs obtained during the pre-test, the final tool was developed with some modifications. The pre-tested patients were excluded from the analysis. Data collectors were supervised daily, and the supervisor and principal investigator checked the filled questionnaires daily.
Data analysis
The gathered quantitative data was cleaned, arranged, coded, and then analyzed through statistical packages for social sciences (SPSS) version 26.0 statistical Software. Categorical variables were expressed by percentage and frequency, whereas numerical variables were present by median with Inter Quartile range (IQR).
The association between the independent variables and Adherence to ASMs was analyzed using a binary logistic regression model. Bivariate binary logistic regression was run at a 25% significance level to screen out potentially significant independent variables. A multivariable binary logistic regression model was run by including the significant independent variables from the bivariate binary logistic regression model. To measure the presence and strength of association between the independent variables and adherence to ASMs, adjusted odds ratio (AOR), P-value, and 95% CI for AOR were calculated separately for self-reported availability and affordability of ASMs. Since the ORs were not different, in the final model, the two variables were considered together, and variables with a P-value of ≤ 0.05 were considered significantly associated with adherence to ASMs.
Operational definitions
Adherence
In this study, adherence was measured using a self-report 3-item questionnaire focusing on medication use patterns of patients from their last visit to the current visit, the items were taken from Morisky Medication Adherence Scale-8.
Self-reported medication availability
In this study, medication availability was measured from the patient’s perspective based on their ability to obtain their medication in the same facility where treatment was given, a nearby facility, or near their residence. Accordingly, Medication Availability was assigned as “Available” if patients were able to gain medications in the same or nearby health facility where they received care or near their residency and others were categorized as “Unavailable”.
Self-reported medication affordability
In this study, medication affordability was assigned as “Affordable” if patients could pay for medications with no difficulty or gain medications free and others were categorized as “Unaffordable”.
ASM (Anti-seizure medications)
ASMs are the primary medications used to control seizures in epileptic patients. In the study setting, the most prescribed anti-seizure medications are phenobarbitone, phenytoin, and sometimes carbamazepine and sodium valproate. In this study, the number of ASMs used by patients was classified as monotherapy if participants took a single drug and poly-therapy, if the participants took more than one anti-seizure medication.
Social support
Social support is the physical and emotional comfort given to you by your family, friends, co-workers, and others. It is the knowledge that you are part of a community of people who love and care for you, value you, and think well of you. In this study, social support was assessed using a Likert scale with a single question: “Is someone available to help you if you need help?”.
Financial support
In this study, financial support was assessed using a single question: “Do you get financial support from relatives, organizations, or anybody else when needed?”.
Ethical consideration
The research and ethical review board of the Addis Continental Institute of Public Health granted ethical clearance and approval of the study. Following the approval, Eka Kotebe General Hospital Institutional Review Board (IRB) obtained official permission. Before data collection, informed written consent was obtained from the study participants. Individuals were told that they had a right to withdraw from the study at any time, and this would not affect the service they got from the hospital. Confidentiality was ensured during the patient interviews and the review of charts.
Results
Socio-demographic characteristics
A total of 357 participants participated in the study, with a response rate of 92.7%. From this, 111 (31.1%) of the respondents were 25–34 years old. More than half of the study participants (61.1%) were single and 184 (51.5%) were males. Regarding educational status, the majority of the study participants had primary and secondary school, 95 (26.6%) and 109(30.5%), respectively. Around two-thirds of the study participants were unemployed, 191 (53.5%) were living in Addis Ababa, and nearly a third were within the same sub-city. The median (IQR) family size of the participants was 4 (3, 5) (Table 1).
Table 1. Socio-demographic characteristics of adult Epileptic patients in Eka Kotebe General Hospital, Ethiopia, 2023 (n = 357).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Family size (Median, IQR) | 4 (3,5) | ||
| Age(Year) | 18–24 | 94 | 26.3 |
| 25–34 | 111 | 31.1 | |
| 35–44 | 78 | 21.8 | |
| ≥ 45 | 74 | 20.7 | |
| Sex | Female | 173 | 48.5 |
| Male | 184 | 51.5 | |
| Marital Status | Single | 218 | 61.1 |
| Married | 139 | 38.9 | |
| Educational Status | No formal education | 80 | 22.4 |
| Primary education (1–8) | 95 | 26.6 | |
| Secondary education (9–12) | 109 | 30.5 | |
| College and above | 73 | 20.4 | |
| Usual place of residence | Within the same sub-city | 109 | 30.5 |
| Addis Ababa | 191 | 53.5 | |
| Outside Addis Ababa | 57 | 16 | |
| Employment Status | Gainfully Employed | 130 | 36.4 |
| Unemployed | 227 | 63.6 | |
| Social Support | Not often | 87 | 24.4 |
| Sometimes | 152 | 42.6 | |
| Often | 118 | 33.1 | |
| Financial support | No | 181 | 71.5 |
| Yes | 72 | 28.5 |
The majority of the respondents, 181(71.5%), had no financial support, and 118 (33.1%) thought they had someone around to help them often when they needed help. (Table 1).
Clinical factors for anti-seizure medication adherence
Among the study participants, the majority of the patients, 279 (78.2%), were diagnosed with a Generalized type of seizure, and more than half, 227(63.6%) of the participants were on monotherapy. The median (IQR) age for the onset of the illness of the participants was 17(10, 24) years, and about slightly two-thirds, 223(62.5%), of the participants had a duration of illness of greater than/equal to 11 years. While co-morbidity was found in less than a fifth of the participants and a small number, 17(4.8%) of the participants had an adverse effect that prompted them to stop taking medication since their last visit (Table 2).
Table 2. Clinical factors for anti-seizure medication adherence among adult Epileptic patients at Eka Kotebe General Hospital, Ethiopia, 2023 (n = 357).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Age of onset of Epilepsy (Year) (Median, IQR) | 17(10,24) | ||
| Duration of illness (in Years) | <5 years | 48 | 13.4 |
| 6–10 years | 82 | 23 | |
| >11 years | 223 | 62.5 | |
| Types of Seizure | Generalized | 279 | 78.2 |
| Focal | 66 | 18.5 | |
| Unclassified | 12 | 3.4 | |
| Number of ASMs | Monotherapy | 227 | 63.6 |
| Polytherapy | 130 | 36.4 | |
| History of Adverse effects of ASMs that prompt to stop taking medication | No | 283 | 79.3 |
| Yes | 74 | 20.7 | |
| History of Adverse effects of ASMs that prompt to stop taking medication since the last visit | No | 340 | 95.2 |
| Yes | 17 | 4.8 | |
| Comorbidity | No | 308 | 86.3 |
| Yes | 49 | 13.7 |
Comorbidity refers to a non-communicable disease that requires a long-term medication, such as Diabetes, hypertension, cardiac illness, renal disease, psychiatric disorders or other health conditions.
Prevalence of adherence to ASMs and self-reported medication availability and affordability among adult Epileptic patients
The prevalence of ASM adherence was 55.2% with 95% CI (50.1%; 60.2%). In this study, self-reported availability and affordability of ASMs were found to be 80.1% and 53.2% respectively (Table 3).
Table 3. Prevalence of adherence to ASMs and self-reported medication availability and affordability among adult Epileptic patients at Eka Kotebe General Hospital, Ethiopia, 2023 (n = 357).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Adherence to ASMs | Non-Adherent | 160 | 44.8 |
| Adherent | 197 | 55.2 | |
| Self-reported Availability of ASMs | Unavailable | 71 | 19.9 |
| Available | 286 | 80.1 | |
| Self-reported Affordability of ASMs | Unaffordable | 167 | 46.8 |
| Affordable | 190 | 53.2 |
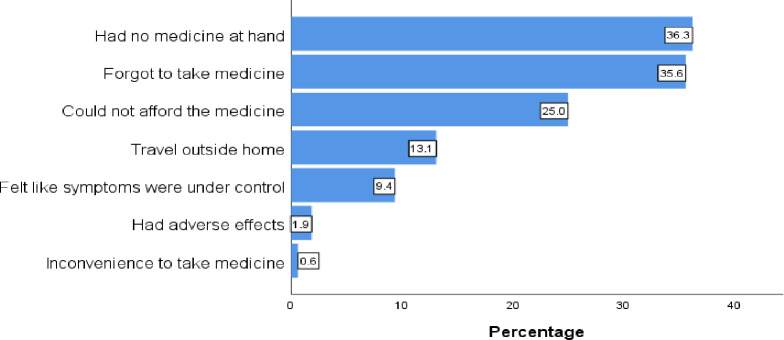
The unavailability of the medications at hand 36.3% and forgetfulness to take medicine 35.6%, were the most common reasons for medication nonadherence, followed by medication unaffordability 25%, and travel outside the home 13.1% was the least reasons for medication non-adherence (Fig 1).
Fig 1. Reasons for ASMs non-adherence at Eka Kotebe General Hospital, Ethiopia, 2023 (n = 357).
Association of self-reported medication availability and affordability with anti-seizure medication adherence among people with epilepsy
In the bivariate binary logistic regression, educational status, number of ASMs, and self-reported affordability of ASMs were significantly associated with adherence to ASMs. However, on the multivariable binary logistic regression model, after adjusting for the covariates, Patients who finished secondary school, were educated up to college level and above, Number of ASMs, and self-reported Availability of ASMs were found to have a statistically significant relationship with adherence to ASMs at 5% level of significance.
Accordingly, after adjusting for other covariates, the odds of being adherent to ASMs among those with secondary education were 2.2 times higher as compared to those with no formal education (AOR = 2.21, 95% CI = 1.07, 4.56, p-value = 0.032). Similarly, the odds of adherent to ASMs were 2.6 times higher for those educated up to college level and above than those with no formal education (AOR = 2.61, 95% CI = 1.08, 6.30, p-value = 0.032). Regarding self-reported availability of ASMs, the odds of being adherent to ASMs were two times higher among those who reported the medications available as compared with those who reported unavailable (AOR = 2.01, 95% CI = 1.01,3.98, p-value = 0.046). On the other hand, the odds of being adherent to ASMs were 45% less for those on polytherapy than those on monotherapy (AOR = 0.55, 95% CI = 0.32, 0.96, p-value = 0.035). In bivariate logistic regression analysis, self-reported affordability of ASMs was associated with ASM adherence (COR = 1.59, CI = 1.04, 2.42, P-Value = 0.031); however, when adjusted for other covariates in the multivariable logistic regression, no significant association was observed (p = 0.674) (Table 4).
Table 4. Bivariate and multivariate analysis of variables associated with ASM adherence (n = 357).
| Variables | Category | Adherence to ASMs | COR (95% CI) | P-Value | AOR (95% CI) | P-Value | |
|---|---|---|---|---|---|---|---|
| Adherent (n) | Non-adherent (n) | ||||||
| Age (years) | 18–24 | 53 | 41 | 1 | 1 | ||
| 25–34 | 60 | 51 | 0.91 (0.52–1.58) | 0.738 | 1.14(0.55–2.35) | 0.729 | |
| 35–44 | 43 | 35 | 0.95 (0.52–1.74) | 0.869 | 0.99(0.46–2.13) | 0.969 | |
| ≥ 45 | 41 | 33 | 0.96 (0.52–1.78) | 0.899 | 0.95 (0.42–2.18) | 0.910 | |
| Sex | Female | 96 | 77 | 1 | 1 | ||
| Male | 101 | 83 | 0.98(0.64–1.48) | 0.909 | 0.88(0.52–1.49) | 0.637 | |
| Educational Status | No formal education | 37 | 43 | 1 | 1 | ||
| Primary education (1–8) | 45 | 50 | 1.05(0.58–1.90) | 0.883 | 1.10 (0.53–2.30) | 0.795 | |
| Secondary education (9–12) | 68 | 41 | 1.93(1.07–3.46) | 0.028 | 2.21 (1.07–4.56) | 0.032 * | |
| College and above | 47 | 26 | 2.10(1.10–4.03) | 0.025 | 2.61 (1.08–6.30) | 0.032 * | |
| Number of Anti-seizure medications | Monotherapy | 138 | 89 | 1 | 1 | ||
| Polytherapy | 59 | 71 | 0.54(0.35–0.83) | 0.005 | 0.55 (0.32–0.96) | 0.035 * | |
| Comorbidity | No | 171 | 137 | 1 | 1 | ||
| Yes | 26 | 23 | 0.91(0.50–1.66) | 0.748 | 0.78 (0.34–1.80) | 0.557 | |
| Self-reported Availability of ASMs | Unavailable | 35 | 36 | 1 | 1 | ||
| Available | 162 | 124 | 1.34 (0.80–2.26) | 0.266 | 2.01 (1.01–3.98) | 0.046 * | |
| Self-reported Affordability of ASMs | Unaffordable | 82 | 85 | 1 | 1 | ||
| Affordable | 115 | 75 | 1.59(1.04–2.42) | 0.031 | 1.13 (0.64–2.01) | 0.674 | |
| Financial Support | No | 92 | 89 | 1 | 1 | ||
| Yes | 38 | 34 | 1.08(0.63–1.87) | 0.780 | 0.93 (0.52–1.68) | 0.819 | |
* Statistically Significant at P<0.05
Discussion
Findings of adherence in this study showed that less than two-thirds (55.2%; 95% CI (50.1%-60.2%) of the study participants were adherent to anti-seizure medications. Globally, the adherence rate ranges between 33 and 99% [6, 8, 10, 12, 13].
The prevalence of adherence to anti-seizure medications in this study was in line with a cross-sectional study conducted in Addis Ababa (52.4%) [21], Jimma (58.5%) [9], and Nigeria (55.5%) [22]. However, it was lower than the study done in Gondar, Ethiopia (61.5%) [23], Southwestern Ethiopia (63.5%) [24], and India (72.3%) [25]. The probable reason for these discrepancies could be the differences in the methodology used for assessing adherence rate and the study design. For example, a prospective observational study was employed in the study from southwestern Ethiopia, and adherence was assessed by the Hill–Bone compliance to the high blood pressure therapy scale [24], but the current study employed a cross-sectional study design, and adherence was assessed using self-report questions taken from a validated MMAS 8. The other reason could be due to the socio-demographic characteristics of the study participants as well as the study area.
On the other hand, the findings of this study were higher than the studies done in Brazil and Nigeria, which were (33.8%) [26] and (31.6%) [13], respectively, and this difference was probably due to the difference in ASMs multidrug treatment. For instance, 71.1% of people with epilepsy in Brazil and 85% in Nigeria were on multiple ASM treatment, while in the current study, only 36.4% of people with epilepsy were in poly-ASM treatment.
The most common reasons for missing doses in this study were the unavailability of the medications at hand (36.3%) followed by forgetfulness to take medicine (35.6%), which is supported by the findings of studies in Amanuel Mental Specialized Hospital, Ethiopia [27], Jimma Ethiopia [24] and Nigeria [22].
In this study, factors found to have a significant association with adherence to ASMs were higher educational status, self-reported availability of ASMs, and being on poly-therapy. This study revealed the odds of being adherent to ASMs were 2.6 times higher for those who were educated up to college level and above than those with no formal education. This result aligns with the study conducted in India [28]. This might be due to patients who are more educated might question their health care providers about their disease and its medications, might be more aware of the disease progression and follow the prescription and instructions as told Whereas, those who are less educated in our setting might prefer other alternative traditional practices at home than proper medication follow up.
Besides, Patients taking combination drugs were less likely to Adhere. Poly-therapy increases the potential for drug-drug interactions, results in failure to evaluate the individual drugs may affect compliance and is associated with a higher cost of medication and the necessity for therapeutic drug monitoring [29]. Our study revealed the odds of being adherent to ASMs were 45% less for those on poly-therapy as compared with those who were on monotherapy. Similar studies found a negative association between the complexity of medication and patient adherence [22, 28]. Regarding self-reported availability of ASMs, the odds of being adherent to ASMs were two times higher among those who reported the medications available as compared with those who reported unavailable. This finding was supported by the study from Jimma, Ethiopia [24], and India [28].
In bivariate logistic regression analysis, self-reported affordability of ASMs was associated with ASM adherence. This finding was supported by a study from South Western Ethiopia [30]. The possible justification was that patients who got their medication out of pocket would sometimes cease to purchase their medications, and those who got free will continue their medications in whatever circumstances.
By contrast, the patient’s adherence to their medication did not show a significant association with age and gender. This result is in line with the findings in Gondar, Ethiopia [23], Nigeria [22], and India [28]. This may indicate that ASM adherence in our context is affected more by the availability of the drugs rather than the demographic characteristics of the patients.
This study has a few limitations. First, it was a cross-sectional study with no prospective follow-up period. As a result, it may be subjected to recall bias. Second, a self-reported measure of adherence, which is prone to social desirability bias, was used to measure adherence. Third, it was conducted in a single setting, which makes it difficult to generalize.
Conclusion and recommendation
In conclusion, overall, only about half of the patients adhered to Anti-seizure medications at Eka Kotebe General Hospital. The self-reported availability of ASMs was significantly associated with adherence to anti-seizure medications. Improving access to ASMs is critical to improving adherence and management of epilepsy. A large-scale study is highly recommended to fully understand the factors contributing to ASM adherence in Ethiopia.
Supporting information
(PDF)
(PDF)
Acknowledgments
We thank the patients for their consent to participate in this study and their patience during the interview. We also appreciate the staff of Eka Kotebe General Hospital for their cooperation and support throughout the data collection process.
Abbreviations
- AOR
Adjusted Odds Ratio
- ASMs
Anti-Seizure Medications
- CBHI
Community-Based Health Insurance
- CI
Confidence Interval
- COR
Crudes Odds Ratio
- IQR
Inter Quartile Range
- IRB
Institutional Review Board
- OR
Odds ratio
- SPSS
Statistical Package for Social Sciences
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication Compliance and Persistence: Terminology and Definitions. Value in Health. 2008. Jan;11(1):44–7. doi: 10.1111/j.1524-4733.2007.00213.x [DOI] [PubMed] [Google Scholar]
- 2.Gottlieb H. Medication nonadherence: finding solutions to a costly medical problem CME. Drug Benefit Trends [Internet]. (12(6):57–62, 2000). Available from: http://www.medscape.com/SCP/DBT/2000/v12.n06/d1206.01.gott/d1206.01.gott-01.html [Google Scholar]
- 3.Organization WH. Neurological disorders: public health challenges. World Health Organization; 2006. [Google Scholar]
- 4.Kwan P, Brodie MJ. Early Identification of Refractory Epilepsy. N Engl J Med. 2000. Feb 3;342(5):314–9. doi: 10.1056/NEJM200002033420503 [DOI] [PubMed] [Google Scholar]
- 5.Scott RA, Lhatoo SD, Sander JW. The treatment of epilepsy in developing countries: where do we go from here? Bulletin of the World Health Organization. 2001;79(4):344–51. [PMC free article] [PubMed] [Google Scholar]
- 6.Hovinga CA, Asato MR, Manjunath R, Wheless JW, Phelps SJ, Sheth RD, et al. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: Survey of patients with epilepsy and physicians. Epilepsy & Behavior. 2008. Aug;13(2):316–22. doi: 10.1016/j.yebeh.2008.03.009 [DOI] [PubMed] [Google Scholar]
- 7.Jones RM, Butler JA, Thomas VA, Peveler RC, Prevett M. Adherence to treatment in patients with epilepsy: Associations with seizure control and illness beliefs. Seizure. 2006. Oct;15(7):504–8. doi: 10.1016/j.seizure.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 8.Teferra A, Alemayehu W. Patient non-compliance with drug regimens for chronic diseases in northwest Ethiopia. Ethiopian Journal of Health Development. 2001;15(3):185–92. [Google Scholar]
- 9.Getachew H, Dekema N, Awol S, Abdi A, Mohammed M. Medication adherence in epilepsy and potential risk factors associated with non adherence in tertiary care teaching hospital in southwest Ethiopia. Gaziantep Med J. 2014;20(1):59. [Google Scholar]
- 10.Sebastian J, Adepu R, Keshava BS, Harsha S. Assessment of antiepileptic drugs usage in a South Indian tertiary care teaching hospital. Neurology Asia. 2013;18(2). [Google Scholar]
- 11.Sweileh WM, Ihbesheh MS, Jarar IS, Taha ASA, Sawalha AF, Zyoud SH, et al. Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsy & Behavior. 2011. Jul;21(3):301–5. doi: 10.1016/j.yebeh.2011.04.011 [DOI] [PubMed] [Google Scholar]
- 12.Liu J, Liu Z, Ding H, Yang X. Adherence to treatment and influencing factors in a sample of Chinese epilepsy patients. Epileptic Disorders. 2013. Sep;15(3):289–94. doi: 10.1684/epd.2013.0588 [DOI] [PubMed] [Google Scholar]
- 13.Johnbull OS, Farounbi B, Adeleye AO, Ogunrin O, Uche AP. Evaluation of Factors Influencing Medication Adherence in Patients with Epilepsy in Rural Communities of Kaduna State, Nigeria. NM. 2011;02(04):299–305. [Google Scholar]
- 14.Egenasi C, Steinberg W, Raubenheimer J. Beliefs about medication, medication adherence and seizure control among adult epilepsy patients in Kimberley, South Africa. South African Family Practice. 2015. Sep 3;57(5):326–32. [Google Scholar]
- 15.Getnet A, Woldeyohannes SM, Bekana L, Mekonen T, Fekadu W, Menberu M, et al. Antiepileptic Drug Nonadherence and Its Predictors among People with Epilepsy. Behavioural Neurology. 2016;2016:1–6. doi: 10.1155/2016/3189108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cameron A, Bansal A, Dua T, Hill SR, Moshe SL, Mantel‐Teeuwisse AK, et al. Mapping the availability, price, and affordability of antiepileptic drugs in 46 countries. Epilepsia. 2012. Jun;53(6):962–9. doi: 10.1111/j.1528-1167.2012.03446.x [DOI] [PubMed] [Google Scholar]
- 17.Mac TL, Le VT, Vu AN, Preux P, Ratsimbazafy V. AEDs Availability and Professional Practices in Delivery Outlets in a City Center in Southern Vietnam. Epilepsia. 2006. Feb;47(2):330–4. doi: 10.1111/j.1528-1167.2006.00425.x [DOI] [PubMed] [Google Scholar]
- 18.Chomba EN, Kansembe H, Mbewe E, Ndubani P, Birbeck GL, Haworth A, et al. The Current Availability of Antiepileptic Drugs in Zambia: Implications for the ILAE/WHO “Out of the Shadows” Campaign. The American Journal of Tropical Medicine and Hygiene. 2010. Sep 1;83(3):571–4. doi: 10.4269/ajtmh.2010.10-0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.YANGATIMBI E. Problem of accessibility to antiepileptic drugs for patients suffering from epilepsy in Bangui. Central African Republic. African & Middle East Epilepsy Journal. 2020;9(6). [Google Scholar]
- 20.Berhe T, Mulatu HA. Anti-epileptic drug utilization pattern and control of seizure among patients with epilepsy at two tertiary hospitals in Addis Ababa, Ethiopia. Vol. 1, Received: 16 December 2021 Accepted: 31 December 2021 Published: 24 January 2022. MJH; 2021. [Google Scholar]
- 21.Molla S, Demissie H, Ayele BA, Tsehayneh F, Ali S, Zenebe G. Factors associated with antiepileptic drug adherence in epileptic patients at a tertiary care center in Ethiopia: A cross sectional study. African Journal of Neurological Sciences. 2021;40(2):3–10. [Google Scholar]
- 22.Ejeliogu EU, Courage A. Prevalence and factors associated with non-adherence to antiepileptic drugs among children with epilepsy in Jos, Nigeria. Nig J Paed. 2020. Aug 6;47(3):240–5. [Google Scholar]
- 23.Tilahun M, Habte N, Mekonnen K, Srahbzu M, Ayelegne D. Nonadherence to Antiepileptic Medications and Its Determinants among Epileptic Patients at the University of Gondar Referral Hospital, Gondar, Ethiopia, 2019: An Institutional-Based Cross-Sectional Study. de Carvalho M, editor. Neurology Research International. 2020. Oct 28;2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bayane YB, Senbeta BS. Pattern of anti-epileptic medications nonadherence and associated factors at ambulatory clinic of Jimma Medical Center, Southwestern Ethiopia: A prospective observational study. SAGE Open Medicine. 2023. Jan;11:205031212311608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gurumurthy R, Chanda K, Sarma G. An evaluation of factors affecting adherence to antiepileptic drugs in patients with epilepsy: a cross-sectional study. smedj. 2017. Feb;58(2):98–102. doi: 10.11622/smedj.2016022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferrari CMM, de Sousa RMC, Castro LHM. Factors associated with treatment non-adherence in patients with epilepsy in Brazil. Seizure. 2013. Jun;22(5):384–9. doi: 10.1016/j.seizure.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 27.Shumet S, Wondie M, Ayano G, Asfaw H, Kassew T, Mesafint G. Antiepileptic Drug Adherence and Its Associated Factors among Epilepsy Patients on Follow-ups at Amanuel Mental Specialized Hospital, Ethiopia. Ethiopian Journal of Health Sciences. 2022;32(5):913–22. doi: 10.4314/ejhs.v32i5.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Govil N, Chahal S, Gupta N, Kaloti AS, Nadda A, Singh P. Factors Associated with Poor Antiepileptic Drugs Adherence in Below Poverty Line Persons with Epilepsy: A Cross-Sectional Study. JNRP. 2021. Jan 29;12:95–101. doi: 10.1055/s-0040-1721200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ArulKumaran KSG, Palanisamy S, Rajasekaran A. A study on drug use evaluation of anti-epileptics at a multispecialty tertiary care teaching hospital. Int J Pharm Tech Res. 2009;1(4):1541–7. [Google Scholar]
- 30.Bereda G, Bereda G. Determination of the Factors Leading To Non Adherence with Anti-Epileptic Medication in Psychiatric Ambulatory Follow up Patients of Mettu Karl Referral Hospital, South Western, Ethiopia: A Prospective Cross Sectional Study. South Western, Ethiopia: A Prospective Cross Sectional Study J Basic ClinPharma. 2021;12(4):51–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.