Abstract
Background.
Teaching cancer prevention and detection is important in health professional education. It is desirable to select a comprehensive framework for teaching oral cancer (OC) prevention and detection skills.
Methods.
The PRECEDE-PROCEED model was used to design a randomized pretest and posttest study of the OC prevention and detection skills of dental students (n=104). OC knowledge, opinions, and competencies were evaluated.
Results.
Second year students in the intervention group were more competent than those in the control group.
Conclusions.
The novel use of PRECEDE-PROCEED sets a precedent for designing a standardized OC curriculum for a wide range of health professional disciplines.
Training health professional students in the prevention and early detection of disease is an important component of predoctoral education. However, uniform incorporation of prevention and detection content into curricula of health professional schools has not yet occurred.1 In response to this challenge, developmental Objectives 1 through 7 of Healthy People 2010 is to increase the number of health professional schools that include core competencies in health promotion and disease prevention.2 A 4-component Clinical Prevention and Population Health Framework was subsequently developed by the Healthy People Curriculum Task Force. Within this framework is a call for training health professional students in screening and counseling skills.1
A comprehensive disease prevention and detection curriculum for health professional schools should include training in oral cancer prevention and early detection. With a 5-year relative survival rate of 59%, oral cancer is a significant public health concern in the United States. It is anticipated that there will be approximately 30,000 new cases and 7400 deaths in the United States in 2006 attributable to cancers of the oral cavity and pharynx.3 The major risk factor is tobacco use, which accounts for over 75% of oral cancers. Thus, Healthy People 2010 includes 3 objectives to detect oral cancer earlier and to increase the percentage of dentists and physicians who counsel tobacco using patients and encourage nonusers to abstain from starting tobacco use.2 Additionally, the American Cancer Society recommends conducting an oral cancer examination during regular periodic health examinations for individuals aged 20 years and older.4
Despite these national recommendations, studies of dental and medical school curricula confirm insufficient coverage of oral cancer prevention and early detection.5–7 Dental and medical students have reported receiving inadequate training in head and neck examination and tobacco cessation counseling.8–13 Additionally, few dental or medical schools formally evaluate competency in head and neck examination and tobacco cessation counseling, and no state board of dental or medical examiners requires applicants to demonstrate their proficiency in these areas. Only 1 state requires continuing dental education in these areas.14
Oral cancer prevention and early detection can be integrated into the curricula of health professional schools using a comprehensive planning framework. One methodology that is commonly used to design, implement, and evaluate interventions that influence health-related behaviors is the PRECEDE-PROCEED model developed by Green, and Kreuter.15 Components of the model are derived from epidemiology; social, behavioral, and educational sciences; and health administration.
Purpose
The PRECEDE-PROCEED model was used to develop, implement, and evaluate a randomized pretest and posttest study to compare traditional lecture instruction with a problem-based learning (PBL) approach for training dental students in oral cancer prevention and early detection skills. Dental students were chosen as the study population of interest, although this model may be adapted to design oral cancer prevention and detection curricula for other health professions disciplines.
MATERIALS AND METHODS
The PRECEDE-PROCEED model consists of 8 phases: (1) Social Assessment and Situational Analysis, (2) Epidemiological Assessment, (3) Educational and Ecological Assessment, (4) Intervention Alignment, (5) Implementation, (6) Process Evaluation, (7) Impact Evaluation, and (8) Outcome Evaluation. A diagram of the application of PRECEDE-PROCEED to this study is given in Figure 1.
Figure 1.
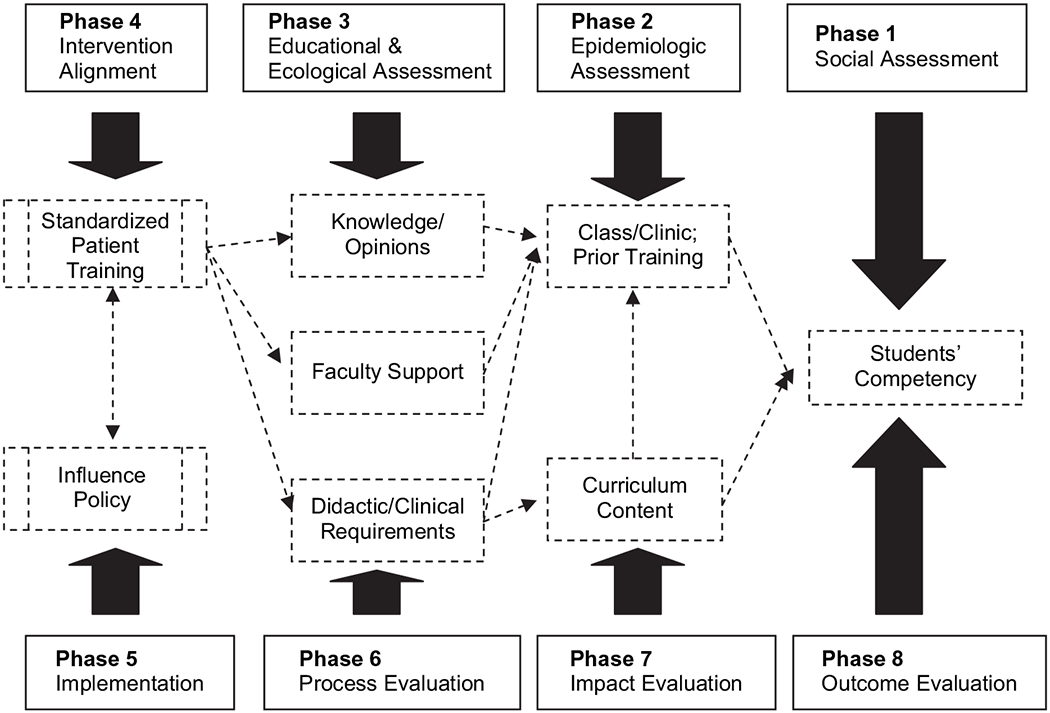
PRECEDE-PROCEED application for designing oral cancer prevention and early detection training for health professional students. Solid boxes and arrows: PRECEDE-PROCEED phases. Dashed boxes and arrows: PRECEDE-PROCEED model application to training health professional students in oral cancer prevention and early detection.
An assessment of the social environment was provided by preliminary studies of dental and medical students in 1 university setting in 2002. Based on the preliminary studies, Phase 2 evaluated the dental school’s curriculum for oral cancer prevention and early detection content. A detailed listing of the curriculum is given in Table 1. In Phase 3, discussion sessions were held with dental faculty members to obtain faculty input regarding ways to improve dental students’ oral cancer prevention and detection skills.
Table 1.
Oral Cancer Prevention and Detection Content at a US Dental School
| Course | Semester | Topics Covered |
|---|---|---|
| 1st Year | Summer | Introduction to oral pathology and oral cancer |
| Nutrition | Fall | The role of fruit and vegetable consumption in the progression of oral cancers |
| Preventive Dentistry | Fall | Oral cancer epidemiology and tobacco cessation training |
| Preventive Periodontics | Fall | Review of medical and dental histories including tobacco and alcohol use assessment; components of an extraoral and intraoral examination |
| Advanced Biochemistry | Spring | The molecular basis of oral cancer |
| 2nd Year | ||
| Oral Medicine | Spring | The types, epidemiology, and location of oral cancers |
| 3rd Year | ||
| Oral Pathology I and II | Fall/Spring | The pathology of oral cancer |
| Junior Periodontics Clinics | Summer/Fall/Spring | Review medical and dental histories, and conduct intraoral and extraoral examination with patients |
| 4th Year | ||
| Clinical Diagnostic Conference | Summer | Establish clinical differential diagnosis for pathologic lesions including various types of oral cancers |
| Senior Periodontics Clinics | Summer/Fall/Spring | Review medical and dental histories, and conduct intraoral and extraoral examination with patients |
In Phases 4 and 5, 1st- and 2nd-year dental students (n = 104) were randomly assigned to either the intervention or control group using a computer-generated random numbers sequence. Students in the control group received usual instruction in oral cancer prevention and detection as determined by the dental curriculum. Those in the intervention group received faculty-facilitated, standardized, patient-based training in addition to the existing curriculum. During this training, groups of students observed dental faculty members demonstrate proper head and neck examination techniques and how to counsel a standardized patient about tobacco use cessation.
All students were measured at baseline and at a 6-month posttest on their oral cancer and tobacco cessation knowledge, opinions and behaviors, and their competency in head and neck examination and tobacco cessation counseling. Knowledge, opinions, and behaviors were measured using a modified version of a self-administered questionnaire designed for physicians and dentists,16–18 and competency was measured with an Objective Structured Clinical Examination (OSCE). Since the mid-1970s, the OSCE has been used to observe and document medical students’ clinical skills in a standardized context.19 The OSCE used for this study portrayed the standardized patient as a current smoker at risk for oral cancer and was pilot-tested with 4th-year dental students (n=8) in August 2005.
The university’s human subjects institutional review board approved this randomized 2-group pretest and posttest study in July 2005. The dental school was designated as the initial study site. Written informed consent was obtained from all student participants, with students and investigators each receiving a copy of the signed consent form.
RESULTS
Phases 6 through 8 comprise the evaluative component of the PRECEDE-PROCEED model. Results of the social assessment indicated that although dental and medical students improved in oral cancer prevention and detection skills as they progressed through school, a greater emphasis should be placed on these issues in the curricula. Similarly, whereas students favored increased training in tobacco cessation education, the majority felt inadequately trained in and uncomfortable providing tobacco cessation counseling and advice to patients.9–11
Following the intervention, change in questionnaire responses and OSCE scores were compared from pretest to posttest between the intervention and control groups. Second-year students in the intervention group received higher OSCE scores than those in the control group. There were no group differences for 1st-year students. Additional study results have been described elsewhere.20
DISCUSSION
Although oral cancer is a significant public health concern, educational research on the oral cancer prevention and early detection skills of health professional students is scarce. This study demonstrated that the PRECEDE-PROCEED theoretical model can be applied as a comprehensive methodology for designing, implementing, and evaluating an oral cancer prevention and early detection intervention. The improved OSCE scores of 2nd-year students indicated that the combination of traditional lecture and PBL can improve students’ oral cancer prevention and detection skills. The skills of 2nd-year students in the intervention group may have been reinforced by observing faculty members demonstrate the head and neck examination and tobacco cessation counseling techniques. The lack of effect for 1st-year students could be attributed to a more limited baseline knowledge and set of skills.
Eva21 acknowledged that research on PBL interventions can be effective when appropriate outcome measures are selected within an optimal research design such as the randomized pretest and posttest design used in this study. Using the PRECEDE-PROCEED model to design an oral cancer prevention and early detection training program is an innovative approach because the model is commonly used to direct interventions for patients, not providers. Additionally, the systematic process of identifying multiple components necessary for achieving the desired outcome allows this methodology to be applied in any health professional discipline or field.
One important aspect of curricular change is that of engaging faculty acceptance and support. Barriers to implementation can be avoided by encouraging faculty participation from the outset. As described in this study, discussion sessions with faculty can yield suggestions for improvement in the existing curriculum content. At the time of this assessment, the dental curriculum was undergoing a major revision, and faculty members were quite supportive of developing an improved oral cancer prevention and detection curriculum. Suggestions from the faculty included having additional instruction for students in proper methods of examination and tobacco cessation counseling and formally evaluating student competency after the 2 preclinical years of school. Sachdeva22 commented that curricular reform and adaptation are more effective when faculty provide expertise toward the development and implementation of new teaching strategies.
Health professional schools have a responsibility to train competent and confident future providers. By assessing the oral cancer prevention and early detection training of health professional students within a theory-based model, educators can apply a scientifically sound approach toward understanding the factors related to students’ examination and counseling skills. Oral cancer prevention and early detection needs to be an integral component of cancer education, and the PRECEDE-PROCEED model can be used to effectively design a standardized curricular model for the health professions disciplines.
Acknowledgments
Supported by the National Institute of Dental and Craniofacial Research F30DE017046-01.
References
- 1.Allan J, Barwick T, Cashman S, et al. Clinical prevention and population health: a curriculum framework for health professions. Am J Prev Med. 2004;27:471–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Healthy People 2010. 2nd ed. Washington, DC: US Government Printing Office, November 2000; 2. [Google Scholar]
- 3.Jemal A, Siegel R, Ward E, et al. Cancer Statistics, 2006. CA Cancer J Clin. 2006;56:106–130. [DOI] [PubMed] [Google Scholar]
- 4.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society Guidelines for the Early Detection of Cancer, 2006. CA Cancer J Clin. 2006;56:11–25. [DOI] [PubMed] [Google Scholar]
- 5.Ahluwalia KP, Yellowitz JA, Goodman HS, Horowitz AM. An assessment of oral cancer prevention curricula in U.S. medical schools. J Cancer Educ. 1998;13:90–95. [DOI] [PubMed] [Google Scholar]
- 6.Rankin KV, Burzynski NJ, Silverman S Jr, Scheetz JP. Cancer curricula in U.S. dental schools. J Cancer Educ. 1999;14:8–12. [DOI] [PubMed] [Google Scholar]
- 7.Tomar SL, Silverman S Jr, Carpenter WM. Oral cancer education training methods: a comparison of self-study and didactic approaches. J Cancer Educ. 1998;13:141–144. [DOI] [PubMed] [Google Scholar]
- 8.Burzynski NJ, Rankin KV, Silverman S Jr, Scheetz JP, Jones DL. Graduating dental students’ perceptions of oral cancer education. J Cancer Educ. 2002;17:83–84. [DOI] [PubMed] [Google Scholar]
- 9.Cannick GF, Horowitz AM, Drury TF, Reed SG, Day TA. Assessing oral cancer knowledge among dental students in South Carolina. J Am Dent Assoc. 2005;136:373–378. [DOI] [PubMed] [Google Scholar]
- 10.Cannick GF, Horowitz AM, Reed SG, Drury TF, Day TA. Opinions of South Carolina dental students toward tobacco intervention. J Public Health Dent. 2006;66:44–48. [DOI] [PubMed] [Google Scholar]
- 11.Reed SG, Grijebovskaya Duffy N, Walters KC, Day TA. Oral cancer knowledge and experience: a survey of South Carolina medical students in 2002. J Cancer Educ. 2005;20:136–142. [DOI] [PubMed] [Google Scholar]
- 12.Rankin KV, Jones DL, McDaniel RK. Oral cancer education in dental schools: survey of Texas dental students. J Cancer Educ. 1996;11:80–83. [DOI] [PubMed] [Google Scholar]
- 13.Yip JK, Hay JL, Ostroff JS, Stewart RK, Cruz GD. Dental students’ attitudes toward smoking cessation guidelines. J Dent Educ. 2000;64:641–650. [PubMed] [Google Scholar]
- 14.Kerr RA, Changrani JG, Gany FM, Cruz GD. An academic dental center grapples with oral cancer disparities: current collaboration and future opportunities. J Dent Educ. 2004;68:531–541. [PMC free article] [PubMed] [Google Scholar]
- 15.Green L, Kreuter M. Health Promotion Planning: An Educational and Ecological Approach. 4th ed. Boston, MA: McGraw-Hill; 2005. [Google Scholar]
- 16.Shenkin JD, Horowitz AM, Drury TF, Kanellis M. Attitudes of pediatric dentists towards tobacco intervention for children and adolescents: a pilot survey. Pediatr Dent. 2003;25:53–60. [PubMed] [Google Scholar]
- 17.Canto MT, Horowitz AM, Drury TF, Goodman HS. Maryland family physicians’ knowledge, opinions, and practices about oral cancer. Oral Oncol. 2002;38:416–424. [DOI] [PubMed] [Google Scholar]
- 18.Horowitz AM, Drury TF, Goodman HS, Yellowitz JA. Oral pharyngeal cancer prevention and early detection: dentists’ opinions and practices. J Am Dent Assoc. 2000;131:453–462. [DOI] [PubMed] [Google Scholar]
- 19.Harden R, Stevenson M, Downie W, Wilson G. Assessment of clinical competence using objective structured examination. Br Med J. 1975;1:447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cannick GR, Horowitz AM, Garr DR, Reed SG, Neville BW, Day TA, Woolson RF, Lackland DT. Journal of Dental Education 2007;71:1203–1209. [PMC free article] [PubMed] [Google Scholar]
- 21.Eva KW. Issues to consider when planning and conducting educational research. J Dent Educ. 2004;68:316–323. [PubMed] [Google Scholar]
- 22.Sachdeva AK. Faculty development and support needed to integrate the learning of prevention in the curricula of medical schools. Acad Med. 2000;75:S35–S42. [DOI] [PubMed] [Google Scholar]


