Abstract
Background:
We evaluate the performance of plastic surgeons in converting National Institutes of Health K grants in early career to R grants intended for established investigators. We also investigate characteristics that may positively predict successful transition from K to R grants.
Methods:
K08, K23, and R01 (or equivalent) grants awarded to plastic surgeons and physicians within the departments of ophthalmology, dermatology, and neurosurgery were collected. Analyses of successful conversion rates from a K to an R grant between plastic surgeons and physicians within the selected departments were performed. Cross-sectional analysis of characteristics among identified plastic surgeons was completed via logistic regression to elucidate possible predictors of successful conversion.
Results:
Comparison of pathway initiation rates demonstrate that plastic surgeons receive significantly fewer K grants relative to the size of their field when compared with other specialties (all P < 0.01). Of the analyzed plastic surgeons, 52.9% successfully converted to an R-series grant within 5.4 years of beginning their K-series grant. Conversion rates were not significantly different between plastic surgeons and physicians within the selected departments. Logistic regression analyses revealed that the time-adjusted mean relative citation ratio of K series–associated publications is a positive predictor of successful conversion (P = 0.047).
Conclusions:
With regard to increasing National Institutes of Health funding via the K-to-R pathway, we believe the field of plastic surgery could benefit from an increased effort to pursue a pathway of K-to-R conversion with a focus on quality over quantity when publishing articles associated with a K-series grant.
Takeaways
Question: How have plastic surgeons fared in converting early-career National Institutes of Health–funded K grants to subsequent R grants and how can they improve?
Findings: Plastic surgeons initiate the K-to-R pathway at a relatively low rate; however, successful conversion rates are on par with other specialties. Time-adjusted mean relative citation ratio of K series–associated publications was found to be a predictor of successful conversion.
Meaning: Promotion of the K-to-R pathway and a focus on quality of research rather than quantity may increase the ability of plastic surgeons to obtain National Institutes of Health grant funding and independent researcher status.
INTRODUCTION
The National Institutes of Health (NIH) provides tens of billions of dollars in research grant funding annually to medical institutions within the United States.1,2 Although these grants are dispersed among physicians in all specialties, plastic surgery is one of the least NIH-funded surgical specialties.3 This limited funding may hinder academic productivity, slow career advancement, and burden future patients by delaying potential improvements to health outcomes. To overcome these hurdles, we must critically analyze and optimize plastic surgeons’ ability to obtain NIH grant funding.
Although many different types of NIH grants exist, the R01 grant is one of the most highly sought after and competitive grants offered by the NIH.4 With an average award rate of approximately 20% in recent years, obtaining an R01 grant serves as an impressive milestone in a researcher’s career.1 Given its competitiveness, many researchers strategically first seek a lower level K-series (eg, K08, K23) grant before pursuing an R01 grant; this commonly utilized strategy is termed the “K-to-R pathway.” The K-to-R pathway serves as a graduated research route whereby researchers first complete a period of mentored research funded through a K-series grant, which are of shorter duration and provide less funding than R01 grants.5 During this time, an early-stage investigator (ESI) builds his or her foundation of research skills and expertise under the guidance of a more established principal investigator (PI).6 Upon successful completion of this initial K-series grant, a researcher hopes to have obtained sufficient knowledge and skill necessary to independently conduct longitudinal research and may then seek further funding via an R01 grant.7 If approved for a subsequent R01 grant, a researcher is deemed to have successfully completed a K-to-R “conversion,” thus graduating them from ESI status to that of independent researcher.
Although previous studies have evaluated use of the K-to-R pathway among other specialties, none have comprehensively analyzed its use by plastic surgeons.8–13 Thus, the present study aims to investigate the use of the K-to-R grant pathway within the field of plastic surgery. We also seek to assess predictors of successful K-to-R grant conversion among plastic surgeons to better guide aspiring clinician-scientists in their pursuit of independent researcher status.
METHODS
The NIH RePORTER database was utilized to identify all K08, K23, R01, and R01 equivalent (DP1, DP2, DP5, R37, R56, RF1, RL1, U01, and R35) grants awarded to plastic surgeons and faculty of ophthalmology, dermatology, and neurosurgery in schools of medicine between 1997 and 2022.14 Given the variability of plastic surgery services as either divisions or departments within US medical institutions, we did not use the NIH RePORTER database’s “department” filter to identify plastic surgeons. Instead, we chose to query the NIH RePORTER database using individual names from the 2023 American Society of Plastic Surgeons (ASPS) membership roster, which comprises 92% of all board-certified plastic surgeons practicing within the United States.15 Given that the ASPS membership roster consists solely of physicians,16 we further chose to limit our search of K-series grants to K08 (Mentored Clinical Scientist Development Award) and K23 (Mentored Patient-Oriented Research Career Development Award) for all department searches, as these grants are exclusively awarded to those with an MD or equivalent degree.5 In doing so, we effectively limited queries of the other departments to only clinician-scientists, as would be expected with the use of our proxy. A combination of computer programming software (Python—pandas 2.0.1, run in PyCharm), manual abstract review, and internet searches were then used to screen and filter each resultant grant.17–19 Grant disbursements were screened to remove duplicate awards and disbursements without an exact name match between the listed primary PI or co-PI and a queried plastic surgeon name. Remaining grant disbursements were then filtered to include only those disbursements verified to have been received by a plastic surgeon as determined by manual abstract review and web search. All collected grants were grouped by specialty for analysis. Plastic surgeon–associated grants were manually categorized by research type (basic science, translational, and clinical) and research area (composite tissue allotransplantation, crania/maxillofacial/head and neck, nerve/peripheral nerve, outcomes, tissue engineering, wounds/scar, and other). Institutional review board approval was not required for this study, as all data were obtained from publicly available sources.
To calculate the relative rates of K-to-R pathway initiation for each specialty group, the 2021 AAMC Physician Specialty Report was utilized to first determine the number of active physicians within plastic surgery, ophthalmology, dermatology, and neurosurgery.20 Pearson chi-square tests were then performed to compare the proportion of plastic surgeons awarded K grants to the proportion of physicians within each of the other specialty groups who were awarded K grants.
Further analysis was conducted to determine each speciality group’s rate of successful K-to-R grant conversion by calculating the proportion of K grant recipients who subsequently obtained an R01 (or equivalent) grant within 5.4 years of their respective K grant start date. This timeframe was chosen based on previously published literature concluding that 5.4 years is the average length of time from receipt of a K grant to subsequent receipt of an R01 (or equivalent) grant.21 Pearson chi-square tests were then used to compare the conversion rate of plastic surgeons to that of the other specialty groups.
A cross-sectional analysis of characteristics specific to the grant recipients and their respective K grant at the time of expected or successful R grant receipt was performed via logistic regression to discern potential predictors of successful conversion for plastic surgeons. A timeline of 2.5 years after completion of the K grant was utilized as the time of expected conversion for these analyses, as this was found to be the average time to conversion among plastic surgeons identified in this study. Grant-specific characteristics were obtained via manual web search and NIH RePORTER query.14 Collection of relative citation ratio (RCR) data and author metrics was performed with the use of iCite.22 The verbiage “K-series-associated publications” refers to peer-reviewed research articles published with data pertaining to the researcher’s K grant project. The term “time-adjusted” refers to our methods of collecting grant-associated publication data in which we included only articles published up until the year before the expected or successful R grant conversion.
Statistical analyses in this study were performed using R. For Pearson chi-square tests, we utilized the chisq.test function from base R.23 Logistic regression analyses were conducted using the “glm” function from the stats package.23
RESULTS
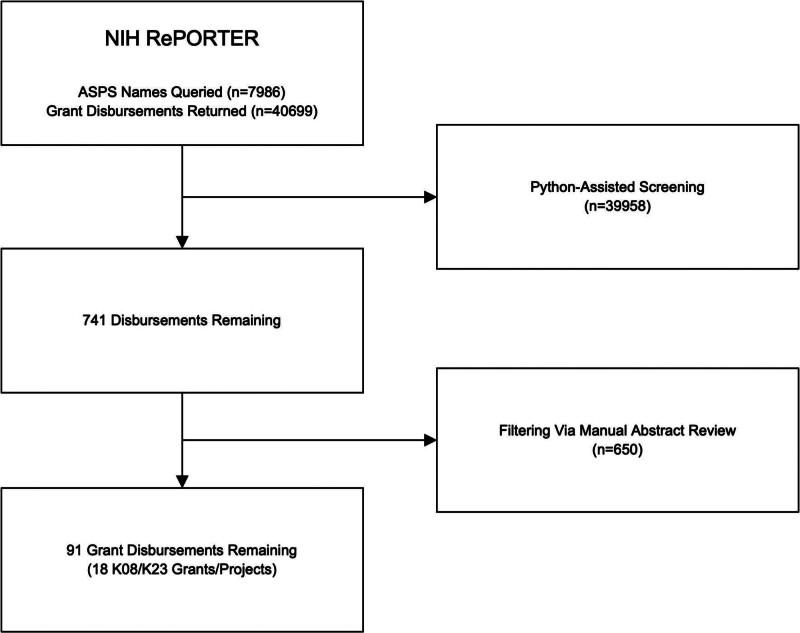
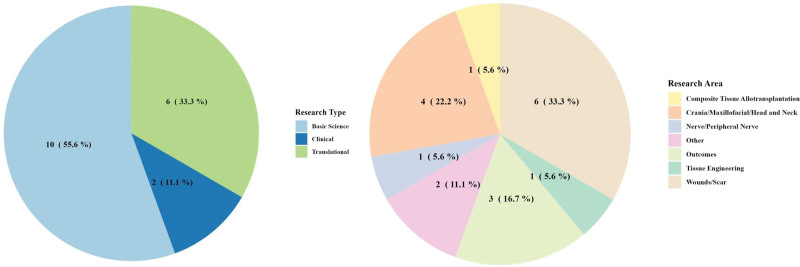
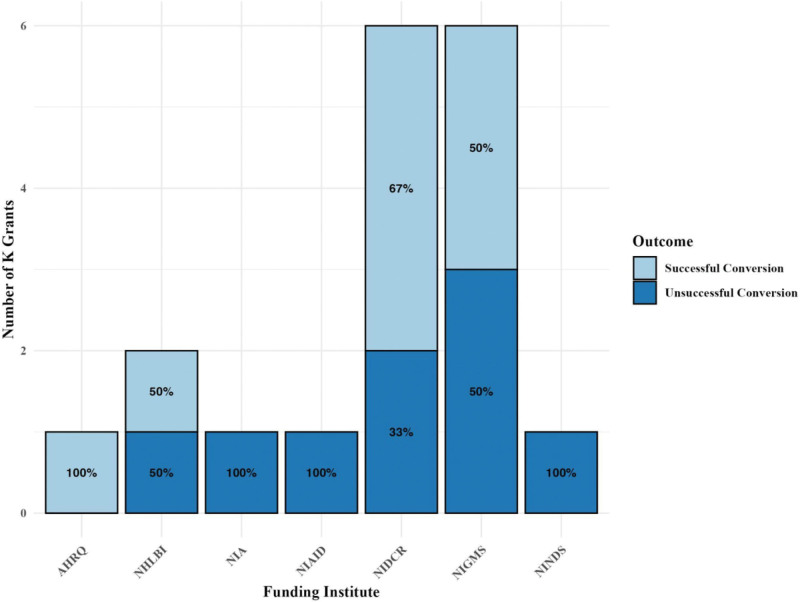
Review of the ASPS membership roster yielded a total of 7986 board-certified plastic surgeons. Initial query of these names within the NIH RePORTER database resulted in a total of 40,699 grant disbursements (Fig. 1). After screening and filtering these grants, we identified a total of 91 grant disbursements corresponding to 18 unique K-series grants received by plastic surgeons. The majority of these grants were classified as basic science projects (Fig. 2A), with the most common area of research being wounds/scar (Fig. 2B). The National Institute of General Medical Sciences and National Institute of Dental and Craniofacial Research were the most common NIH funding institutes that supported the identified grants (Fig. 3).
Fig. 1.
Screening and filtering process of ASPS member grants.
Fig. 2.
Overview of research types and areas in plastic surgeons’ K grants. A, Types of research across identified plastic surgeons’ K grants. B, Areas of research across identified plastic surgeons’ K grants.
Fig. 3.
Funding institutions and centers of identified plastic surgery K grants. AHRQ, Agency for Healthcare Research and Quality; NHLBI, National Heart, Lung, and Blood Institute; NIA, National Institute on Aging; NIAID, National Institute of Allergy and Infectious Disease; NIDCR, National Institute of Dental and Craniofacial Research; NIGMS, National Institute of General Medical Sciences; NINDS, National Institute of Neurological Disorders and Stroke.
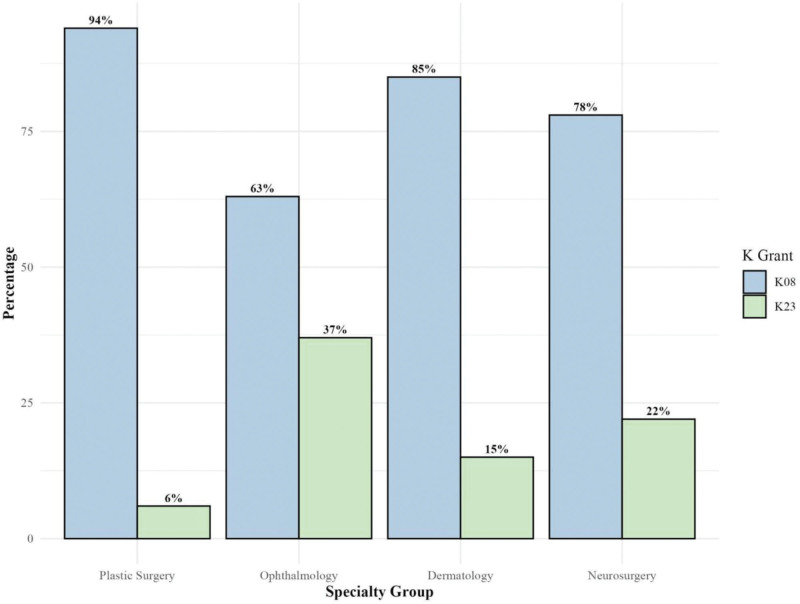
For our comparative analysis of plastic surgeons’ performance with the K-to-R pathway, we identified 17 plastic surgeons, 164 ophthalmologists, 79 dermatologists, and 73 neurosurgeons to be included. A summary of the K grants collected for analysis is depicted in Figure 4. The calculated rates of pathway initiation were found to be 0.2%, 0.9%, 0.6%, and 1.3% within the specialty groups of plastic surgery, ophthalmology, dermatology, and neurosurgery, respectively (Table 1). Pearson chi-square tests comparing rates of pathway initiation revealed that plastic surgeons were significantly less likely to be awarded a K grant when compared with neurosurgeons, ophthalmologists, and dermatologists, independently (all P < 0.01). The calculated rates of successful K-to-R conversion were found to be 52.9%, 47.0%, 58.2%, and 42.5% for the specialty groups of plastic surgery, ophthalmology, dermatology, and neurosurgery, respectively (Table 2). Pearson chi-square analyses comparing rates of successful conversion failed to show statistically significant differences.
Fig. 4.
Percentages of K08 and K23 grants included in analyses by specialty group.
Table 1.
Rates of K-to-R Pathway Initiation by Specialty Group
| Specialty Group | Active Physicians | K Grants (K08, K23) | K-to-R Initiation Rate, % | P |
|---|---|---|---|---|
| Plastic surgery | 7224 | 17 | 0.2 | 1 |
| Ophthalmology | 18,938 | 164 | 0.9 | <0.01 |
| Dermatology | 12,756 | 79 | 0.6 | <0.01 |
| Neurosurgery | 5744 | 73 | 1.3 | <0.01 |
Rates of K-to-R pathway initiation for each specialty group were calculated using the number of identified K grants (K08, K23) per active physician in each specialty.20
Table 2.
Rates of Successful K-to-R Conversion by Specialty Group
| Specialty Group | K Grants (K08, K23) | Subsequent R01 (or Equivalent) Grants | K-to-R Conversion Rate, % | P |
|---|---|---|---|---|
| Plastic surgery | 17 | 9 | 52.9 | 1 |
| Ophthalmology | 164 | 77 | 47.0 | 0.64 |
| Dermatology | 79 | 46 | 58.2 | 0.69 |
| Neurosurgery | 73 | 31 | 42.5 | 0.43 |
Rates of successful K-to-R conversion for each specialty group were calculated as the proportion of subsequent R01 (or equivalent) grants per K grant (K08, K23).
All 18 plastic surgeons were included in our analysis of potential predictors of successful K-to-R conversion. Of these 18 plastic surgeons, nine (50%) were found to have successfully converted to an R01 (or equivalent). (See appendix, Supplemental Digital Content 1, which summarizes the aggregate data of the characteristics collected at the time of expected or successful conversion. http://links.lww.com/PRSGO/D550.) Logistic regression using individual-level characteristic data identified that the time-adjusted mean RCR of K-series-associated publications is a statistically significant predictor of successful conversion (P = 0.047). Analyses of all other gathered individual-level characteristics data failed to show statistical significance.
DISCUSSION
This study provides a critical analysis of plastic surgeon involvement with the graduated K-to-R grant funding pathway over nearly three decades. Our findings demonstrate that relatively few plastic surgeons have initiated the K-to-R grant funding pathway over this time period, but those who do are frequently able to achieve a highly coveted R01 grant.
Comparative analyses of K awardees per active physician in each respective field showed that plastic surgeons had received significantly fewer K08 and K23 grants per active physician when compared with the departments of ophthalmology, dermatology, and neurosurgery. This indicates that plastic surgery has a relative deficiency in receiving initial funding via this mechanism and suggests that the field may benefit from optimization of this stage of K-to-R funding. Further analysis including all applications for K08 and K23 grants could point toward whether the deficiency lies in a lack of attempted pursuit or in a pattern of rejected application for these grants. Unfortunately, rejected applications for both K08 and K23 grants are not made publicly available, so a comprehensive analysis of these grants is not possible.
Comparative analyses of success rates in converting from a mentored K grant to an independent R01 (or equivalent grant) between plastic surgeons and the departments of ophthalmology, dermatology, and neurosurgery failed to show any statistically significant differences. Thus, although the overall NIH funding to plastic surgery may be relatively low, the performance by plastic surgeons in successfully completing the K-to-R pathway, once begun, does not lag behind physicians within other departments.3 This finding, coupled with our finding that plastic surgeons have received fewer K grants per physician, would suggest that a simple increase in the number of plastic surgeons receiving a K08 or K23 grant may directly result in a proportionate increase in R grants and independent researchers relative to other fields.
With this suggestion in mind, we look to current literature to provide practical strategies of increasing ESI research success. A literature review performed by Ransdell et al identified that a lack of mentorship, available time for research, and balance between work and life are major barriers to research development for ESIs.24 In line with these findings, the NIH sourcebook has included a section on training and mentorship, stating that the mentor–mentee relationship is one of the most important factors in performing successful research.25 As such, the most practical strategy that might increase the number of plastic surgeons receiving K08 or K23 grants may be to reinforce mentorship programs focused on improving ESIs technical skills, increasing access to necessary resources and individualizing the support of plastic surgery researchers.
Although an increase in the number of physicians who pursue and begin the K-to-R pathway seems to be a solution to the low NIH funding to plastic surgeons, such an effort would assume that our conversion rates will remain relatively constant and comparable to other specialties. To address this assumption, we sought to also identify characteristics that may predict successful conversion.
The logistic regression analysis of cross-sectional grant recipient characteristics and their respective K grant characteristics demonstrated only one statistically significant predictor of successful conversion for those in plastic surgery—time-adjusted mean RCR of K series–associated publications. Although this is an interesting finding on its own, it is of more interest when we put into perspective that neither the time-adjusted total number of K series–associated publications nor the non-time-adjusted mean RCR of K series–associated publications were found to be positive predictors of success. Being that RCR is a metric proven to be an effective measure of a publication’s impact, our findings reiterate that “quality over quantity” remains as effective guidance for individuals seeking successful conversion—a conclusion we find to be in agreement with the NIH goal to fund projects in a manner so as to “foster fundamental creative discoveries, innovative research strategies, and their applications as a basis to advance significantly the Nation’s capacity to protect and improve health.”26,27 In summary, one should not only work productively throughout their K grant project but focus on publication of work once it has reached a level that it will have maximal impact to other researchers within their field.
In seeking to facilitate grant funding by plastic surgeons utilizing the NIH’s K-to-R funding pathway, we wish to highlight other studies that have addressed the dilemma of securing federal grant funding by plastic surgeons. Although it has been shown that NIH funding is not necessary to publish meaningful works,28 the historically low NIH funding that plastic surgeons receive has been well-documented, and studies taking a closer look at each of the NIH’s many funding mechanisms is not uncommon.3,29–31 Some studies have gathered cross-sectional data from the NIH RePORTER, such as types of grants, rates of approved grants by gender, and other characteristics.3,8–13,29–31 In contrast to these studies, however, we believe our methods allow for a more comprehensive view on NIH funding history by plastic surgeons, as evidenced by discrepancies in the number of sequential K-series and R01 (or equivalent) grant submissions.
There are multiple limitations to this study. First, we were unable to accurately query the NIH RePORTER database for grants awarded to plastic surgeons using the “department” filter, given the significant variability of plastic surgery services as either standalone departments or smaller divisions. However, using the ASPS membership roster as a proxy for NIH RePORTER’s departmental classification of plastic surgery, we were able to effectively identify more than 90% of all board-certified plastic surgeons in the United States. We further mitigated this limitation by restricting K-series queries to K08 and K23 grants for all departments. By maintaining a focus on these grants, specifically, we hoped to make analyses between ASPS members and physicians of other departments more comparable. An additional limitation in this study is the sample size available for analysis with logistic regression. Although more data points would have improved this analysis, we believe the methods of data collection were sufficiently comprehensive, limited most by the size of the field and the history of prior funding.
CONCLUSIONS
This study provides a comparative analysis of rates of successful K-to-R pathway initiation and conversion as well as a starting point in developing a framework that plastic surgeons may utilize to optimize their efforts in receiving NIH funding via this mechanism. Our analysis demonstrates that despite relatively little involvement with this pathway over the past 25 years, plastic surgeons have demonstrated success in advancing from early-career K grants to established investigators holding R grants. The field of plastic surgery may benefit most from an increase in the number of applicants for K grants, and focusing on the quality of publications arising from those awards. Overall NIH funding to plastic surgeons may be improved by continued critical analysis of their performance within all NIH funding mechanisms. Such analysis, coupled with identification of predictors of success, will serve to optimize future funding efforts to plastic surgeons and advance their respective fields of study.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 11 October 2024.
Presented at the American Council of Educators in Plastic Surgery 11th Annual Winter Meeting and the Plastic Surgery Research Council 69th Annual Meeting.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.National Institutes of Health. NIH data book. Available at https://report.nih.gov/nihdatabook/category/10. Accessed March 1, 2023. [Google Scholar]
- 2.Congressional Research Service. National Institutes of Health (NIH) funding: FY1996-FY2023. 2023. Available at https://crsreports.congress.gov/product/pdf/R/R43341/45#:~:text=In%20total%2C%20the%20NIH%20FY2023,until%20the%20end%20of%20FY2025. Accessed May 19, 2024. [Google Scholar]
- 3.Silvestre J, Abbatematteo JM, Chang B, et al. Trends and predictors of National Institutes of Health funding to plastic surgery residency programs. Plast Reconstr Surg. 2017;140:1301–1311. [DOI] [PubMed] [Google Scholar]
- 4.National Institutes of Health. Comparing popular research project grants—R01, R03, and R21. Available at https://www.niaid.nih.gov/grants-contracts/research-project-grants. Accessed March 1, 2023. [Google Scholar]
- 5.K awards: career development. Available at https://www.niddk.nih.gov/research-funding/process/apply/funding-mechanisms/k-awards. Accessed March 1, 2023. [Google Scholar]
- 6.Early stage investigator (ESI) policies. Available at https://grants.nih.gov/policy/early-stage/index.htm. Accessed March 1, 2023. [Google Scholar]
- 7.NIH research project grant program (R01). Available at https://grants.nih.gov/grants/funding/r01.htm. Accessed March 1, 2023. [Google Scholar]
- 8.Jones DR, Mack MJ, Patterson GA, et al. A positive return on investment: research funding by the Thoracic Surgery Foundation for Research and Education (TSFRE). J Thorac Cardiovasc Surg. 2011;141:1103–1106. [DOI] [PubMed] [Google Scholar]
- 9.Rao RC. Success in attaining independent funding among National Institutes of Health K grant awardees in ophthalmology. JAMA Ophthalmol. 2019;137:720. [DOI] [PubMed] [Google Scholar]
- 10.Jagsi R, Motomura AR, Griffith KA, et al. Sex differences in attainment of independent funding by career development awardees. Ann Intern Med. 2009;151:804–811. [DOI] [PubMed] [Google Scholar]
- 11.Narahari AK, Mehaffey JH, Hawkins RB, et al. Cardiothoracic and vascular surgeons achieve high rates of K award conversion into R01 funding. Ann Thorac Surg. 2018;106:602–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nishijima DK, Yadav K, May L, et al. Description and productivity of emergency medicine researchers receiving K23 or K08 mentored research career development awards. Burton J, ed. Acad Emerg Med. 2013;20:611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silvestre J, Hines SM, Chang B, et al. Transition to independent research funding among National Institutes of Health K grant awardees at departments of orthopaedic surgery. J Bone Joint Surg Am. 2021;103:e90. [DOI] [PubMed] [Google Scholar]
- 14.National Institutes of Health. Research portfolio online reporting tools (RePORT). Available at http://projectreporter.nih.gov/reporter.cfm. Accessed March 1, 2023. [Google Scholar]
- 15.American Society of Plastics Surgeons. 2022 ASPS procedural statistics release. 43. Available at https://www.plasticsurgery.org/documents/news/Statistics/2022/plastic-surgery-statistics-report-2022.pdf. Accessed March 1, 2024. [Google Scholar]
- 16.Active membership process. Available at https://www.plasticsurgery.org/for-medical-professionals/join-asps/active-membership-process. Accessed March 1, 2023. [Google Scholar]
- 17.Python Software Foundation. Python language reference, version 3.10. Available at http://www.python.org. Accessed February 4, 2022. [Google Scholar]
- 18.The Pandas Development Team. pandas-dev/pandas: Pandas. 2024. Available at https://zenodo.org/records/10957263. Accessed March 14, 2022. [Google Scholar]
- 19.JetBrains. PyCharm (version 2023.1.2) [Software]. 2023. Available at https://www.jetbrains.com/pycharm/. Accessed June 17, 2023. [Google Scholar]
- 20.American Association of Medical Colleges. Active physicians by sex and specialty, 2021. Available at https://www.aamc.org/data-reports/workforce/data/active-physicians-sex-specialty-2021. Accessed December 1, 2022. [Google Scholar]
- 21.Keswani SS, Short WD, Mehl SC, et al. Defining predictors of successful early career to independent funding conversion among surgeon-scientists. bioRxiv. 2022. [Google Scholar]
- 22.Hutchins BI, Baker KL, Davis MT, et al. The NIH open citation collection: a public access, broad coverage resource. PLoS Biol. 2019;17:e3000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. 2023. Available at https://www.R-project.org/. Accessed March 1, 2023. [Google Scholar]
- 24.Ransdell L, Lane T, Schwartz A, et al. Mentoring new and early-stage investigators and underrepresented minority faculty for research success in health-related fields: an integrative literature review (2010–2020). Int J Environ Res Public Health. 2021;18:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institutes of Health. Mentoring & training. Available at https://oir.nih.gov/sourcebook/mentoring-training. Accessed July 17, 2024. [Google Scholar]
- 26.Hutchins BI, Yuan X, Anderson JM, et al. Relative citation ratio (RCR): a new metric that uses citation rates to measure influence at the article level. Vaux DL, ed. PLoS Biol. 2016;14:e1002541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institutes of Health. About the NIH. Available at https://www.nih.gov/about-nih/what-we-do/nih-almanac/about-nih. Accessed May 23, 2024. [Google Scholar]
- 28.Asserson DB, Janis JE. Majority of most-cited articles in top plastic surgery journals do not receive funding. Aesthet Surg J. 2021;41:NP935–NP938. [DOI] [PubMed] [Google Scholar]
- 29.Silvestre J, Abbatematteo JM, Chang B, et al. The impact of National Institutes of Health funding on scholarly productivity in academic plastic surgery. Plast Reconstr Surg. 2016;137:690–695. [DOI] [PubMed] [Google Scholar]
- 30.Silvestre J, Abbatematteo JM, Serletti JM, et al. National Institutes of Health funding in plastic surgery: a crisis? Plast Reconstr Surg. 2016;138:732–739. [DOI] [PubMed] [Google Scholar]
- 31.Larson KE, Gastman B. Sources of federal funding in plastic and reconstructive surgery research. Plast Reconstr Surg. 2014;133:1289–1294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.