Abstract
Background:
Sleep is influenced by the environments that we experience while awake and while asleep. Neighborhood walkability has been linked with chronic disease and lifestyle factors, such as physical activity; however, evidence for the association between walkability and sleep is mixed. Extant studies assign walkability based on residential addresses, which does not account for mobility. We examined the association between walkability and sleep in the Nurses’ Health Study 3 (NHS3) Mobile Health Substudy (MHS).
Methods:
From 2018 to 2020, individuals in the United States-based NHS3 prospective cohort participated in the MHS, in which minute-level global positioning systems (GPS) data and objective sleep duration and efficiency measures were collected via a custom smartphone application and Fitbit, respectively, for four 7-day periods across a year to capture seasonal variability. Census tract walkability was calculated by summing z-scores of population density (2015–2019 American Community Survey), business density (2018 Infogroup), and intersection density (2018 TIGER/Line road shapefiles). We ran generalized additive mixed models with penalized splines to estimate the association between walkability and sleep, adjusting for individual-level covariates as well as GPS-based exposure to environmental and contextual factors.
Results:
The average main sleep period duration was 7.9 hours and the mean sleep efficiency was 93%. For both sleep duration and sleep efficiency, we did not observe an association with daily average walkability exposure.
Conclusion:
In this study of women across the United States, we found that daily GPS-based neighborhood walkability exposure during wake time was not associated with objective wearable-derived sleep duration or sleep efficiency.
Keywords: Walkability, Sleep, Wearables, Mobile health, Built environment, Global positioning system
What this study adds:
Walkability, which is the presence of environmental features that increase the propensity for walking, is a built environment exposure that may impact sleep; however, there is no consensus in the current literature. Prior studies assign walkability exposure using residential addresses, which captures a limited representation of a person’s true exposure to walkable environments. In this study, we used fine-scale time-activity data from smartphone global positioning systems (GPS) to assess walkability exposure, and we objectively measured sleep using consumer-wearable devices. Incorporating these mobile health data streams (e.g. minute-level GPS, wearables) into this epidemiologic study, we investigated associations between walkability and sleep.
Introduction
Sleep is an integral process to human health; sleep’s role in repair and recovery is essential to cognition, performance, and mental health and key in the maintenance of physical and cardiometabolic health.1,2 Effects of suboptimal sleep on the human body range from short-term health consequences that impact day-to-day quality of life to increased risk of several chronic diseases including cardiovascular disease and several cancers.3–5 Insufficient sleep is modulated by a variety of individual-level risk factors that relate to socioeconomic status, health behaviors, and overall health status, but there is also evidence that environmental and contextual exposures may impact the risk of suboptimal sleep; the ubiquity of these exposures motivate further studies to better understand how these exposures are related to sleep.6,7
Environmental exposures that shape one’s sleeping environment as well as exposures that are experienced during wake time that precedes sleep can impact sleep.8–10 Built environment factors, such as light-at-night (LAN), neighborhood greenspace, and walkability, are of particular interest due to their modifiability and previous links with sleep.11–14 Neighborhood walkability, which is broadly defined by the presence of features that increase propensity for human walking, is hypothesized to be linked to sleep through the mechanism of increased physical activity.15
The relationship between neighborhood walkability and sleep outcomes is not fully elucidated; it is hypothesized that higher walkability exposure leads to higher physical activity, which promotes sleep health via the facilitation of melatonin production, stress reduction, and improvement of mood.16,17 However, there are mixed findings in the current literature with some evidence supporting an association between walkability and sleep, but not all.13,18,19 Difficulty in accounting for correlated environmental coexposures such as LAN and noise may contribute to the lack of consensus on this association. Additionally, extant studies have relied on the assignment of walkability exposure based on residential address locations, which does not account for time spent away from the home. Using minute-level global positioning systems (GPS) data to derive walkability exposure and objectively measured sleep data that was collected over a year-long period for each participant, we investigated associations between walkability and sleep duration and efficiency in the Nurses’ Health Study 3 (NHS3) Mobile Health Substudy (MHS).
Methods
Nurses’ Health Study 3 Mobile Health Substudy
The NHS3 is an open prospective cohort study of male and female nurses and nursing students, with participants in both the United States and Canada. Enrollment for NHS3 began in 2010 for female participants and in 2018 for male participants, all born in 1965 or later. NHS3 is internet based, with survey modules on health and health behaviors sent to participants on personalized timelines based on enrollment date, with a new questionnaire sent to each participant approximately every 6 months.20
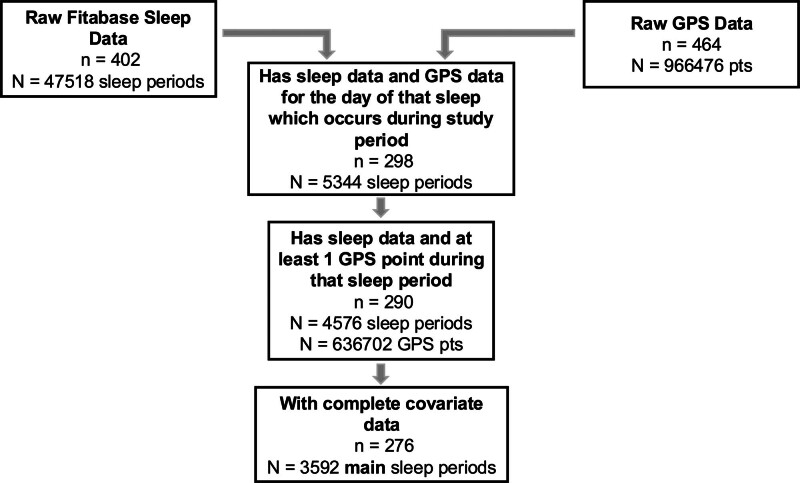
The MHS within NHS3 began in 2018. This study was approved by the Institutional Review Board at Brigham and Women’s Hospital and Harvard Pilgrim Health Care Institute (Boston, MA). At the time of enrollment, we selected participants who had completed at least four questionnaires, had reported no doctor-diagnosed sleep disorder, and had a smartphone running iOS. A total of 511 participants consented and were asked to download a custom smartphone application that passively collected GPS location. They were also provided Fitbit (San Francisco, CA) wearable devices to objectively measure physical activity and sleep outcomes including duration and efficiency.21 A range of devices were used throughout the study period, including the Fitbit Charge HR, Fitbit Charge 2, and Fitbit Charge 3. Participants were followed for a year, with four separate periods of 7-day long data collection, spaced 3 months apart, to capture seasonal variation. Of the participants enrolled in the MHS, 402 had sleep data collected and 464 had at least 1 day of GPS data. After restricting to participants who had simultaneous GPS and sleep data, there were 290 participants and 4576 sleep periods. Once we removed the 462 nonmain sleep periods (i.e., naps) as well as restricted to observations with complete (i.e., no missingness) environmental exposure and covariate data, there were 276 participants and 3952 main sleep periods (Figure 1).
Figure 1.
Deriving the analytic dataset of 276 participants and 3592 main sleep periods from the NHS3 Mobile Health Substudy’s GPS data and Fitbit sleep data.
Sleep
Sleep data measured by the Fitbit devices were downloaded from Fitabase (San Diego, CA). Due to the use of different devices, we have sleep period observations in our dataset estimated from two Fitbit algorithms, “Stages” and “Classic.” Main sleep periods, as classified by the Fitbit device, were included in this analysis; they are the sleep periods of the longest duration and are classified for distinction from naps. For each sleep period, data on duration (in minutes) and efficiency (percentage of time asleep relative to time in bed, calculated as 100 × minutes asleep/[time in bed − minutes after wakeup]) were derived by Fitbit. We additionally conducted analyses with the sleep measures operationalized as categorical outcomes, to estimate the risk of high and low sleep duration and efficiency. Specifically, we categorized sleep duration as optimal (7–9 hours, reference), less than 7 hours, and more than 9 hours. Sleep efficiency was categorized as optimal (85%–96%, reference), low efficiency (less than 85%), and high efficiency (over 96%).
Exposure
GPS data were collected via a custom smartphone application developed for the study, which identified the latitude and longitude of the smartphone every 10 minutes. These GPS points provided data on the locations of participants throughout the study period, which were used for exposure assessment. To ensure the accuracy of GPS data in the analytic dataset, a restriction criteria of minimum 65-m horizontal accuracy was applied. Using the timestamp of GPS points and the times of the sleep records recorded by the Fitbit device, each GPS point was classified as occurring during wake or sleep; this was used to assign environmental exposures accordingly. Wake exposures were assigned based on the daily main wake period preceding each main sleep (i.e., sleep periods beginning after midnight were assigned the previous day’s exposure).
The walkability exposure used in this analysis draws on the framework by Rundle et al, which was optimized to examine the relationships between walkability and physical activity; the calculation of this walkability index for the United States has been described elsewhere.22,23 Briefly, walkability exposure was calculated by summing the z-scores of three elements: population density, business density, and intersection density. A higher walkability score is indicative of an area that encourages active transport versus driving. Population density was calculated by using population data from 2015 to 2019 American Community Survey 5-year estimates and 2010 Census Bureau shapefiles.24 The geospatial 2018 Infogroup US Historical Business Dataset, which contains geocoded addresses of all businesses across the United States, was used to calculate business density.25 For intersection density, intersection counts were calculated with road data from 2019 Tiger/Line shape files of all roads with the interstates removed.26 The resulting walkability exposure is spatially resolved at the census tract level. We joined this walkability exposure to all the GPS points for each participant. By cross-referencing the date and time of each GPS point with the timing of sleep records measured by Fitbit, we calculated the daily mean walkability exposure during wake.
Covariates
Sociodemographic information including age, marital status, employment status, and education and behavioral health information such as alcohol consumption and prevalence of health outcomes including depression were ascertained on the NHS3 baseline survey. We also utilized a covariate for whether the sleep period occurred on a weekend or weekday, based on the day of the wake period. Shiftwork was ascertained from a survey deployed via the smartphone application that participants filled out after each week-long GPS/sleep data collection period, which asked if they had done any shiftwork (and if so, on which days); for sensitivity analyses regarding shiftwork, all sleep periods on dates with reported shiftwork and dates following the shiftwork within that week-long data collection period were considered impacted by shiftwork and excluded in a sensitivity analysis. Data on sleep in nonmain sleep periods (i.e., naps) were collected from the Fitbit; we operationalized a naps variable by classifying main sleep periods on the same day a nap had also occurred (for main sleep periods occurring after midnight, naps on the previous calendar date were included) and excluded these in a sensitivity analysis.
For environmental exposure covariates, the same method described earlier for assignment using GPS data was applied. For LAN, Stray Light Corrected Nighttime Day/Night Band Composites data from NASA’s Visible Infrared Imaging Radiometer Suite was utilized, which has a monthly 500-m spatiotemporal resolution; this was temporally matched to the month of each GPS point.27 For noise, we used 270-m resolution time-aggregated (2000–2014) anthropogenic median A-weighted decibel noise data provided by the National Park Service; for GPS points occurring between 7 am and 7 pm, daytime noise levels were assigned, while GPS points occurring between 7 pm and 7 am were assigned nighttime noise levels.28 For temperature, we matched the date of the GPS point with mean daily temperature data at an 800-m spatial resolution from Parameter-elevation Regressions on Independent Slopes Model.29 For neighborhood socioeconomic status (SES), the Census tract level exposure calculated for the Nurses’ Health Study cohorts was used; it is a composite score of z-standardized components representing education, employment, housing, wealth, racial composition, and density for which higher scores represent higher neighborhood SES.30 Data from the 2010 Census were used. For greenness, we extracted the seasonal Normalized Difference Vegetation Index, which is a satellite measure of photosynthetically active vegetation, at a 30-m resolution, and matched to the season and year of each GPS point.31 Normalized Difference Vegetation Index has a range of −1 to 1, with negative values representing water, zero representing barren rock and soil, and values greater than zero representing vegetation. Consistent with other studies of greenness, we set negative values to zero, resulting in a range of values between zero and one. For the environmental exposure covariates, the periods (sleep vs. wake) used for exposure assignment were as follows: LAN, noise, and outdoor temperature during sleep; neighborhood SES and greenness during wake.
Statistical analysis
All statistical analyses were conducted in R 4.2.0 (Vienna, Austria). To estimate the association between daily mean walkability exposure during wake and sleep outcomes, we used generalized additive mixed models with a random intercept for individuals. Both duration, in minutes, and efficiency, in percent, were modeled continuously. We tested for nonlinearity in all dose responses by evaluating the effective degrees of freedom assigned by penalized splines from the R package mgcv.32 To account for the correlation between observations on adjacent days, we used an autoregressive correlation structure. In basic models, we adjusted for age (years). In fully adjusted models, we additionally adjusted for race (White/non-White), marital status (ever/never married), education (advanced degree yes/no), employment (yes/no), alcohol consumption (≥1 drink per day yes/no), season (Spring/Summer/Fall/Winter), weekend versus weekday, LAN, noise, outdoor temperature, neighborhood SES, and greenness (each continuous). We estimated the expected difference in sleep duration and efficiency associated with an interquartile range (IQR) increase in daily walkability exposure during the wake.
We also conducted analyses with sleep duration and efficiency measures as categorical outcomes for which the middle category (7–9 hours for duration, 85%–96% for efficiency) was considered optimal and used as the referent group. To estimate the odds of higher and lower levels of sleep duration and efficiency, we used mixed effects logistic regression models on subsets of the analytic dataset including the referent group and the level of interest; for instance, to estimate the odds of higher sleep duration, we ran logistic regression models on the subset of observations from the referent group and the high duration group. To account for correlations between repeated measures within an individual, as well as that of observations from the same data collection week, we included random intercepts for participant/collection week. This subsetted logistic regression approach has been shown to be comparable to the results of a multinomial logistic regression and permitted us to assess nonlinear dose responses.33
We conducted sensitivity analyses to examine the robustness of our results to alternative modeling choices. To determine if shiftwork may have impacted associations, we removed sleep periods for which shiftwork was reported and the sleep periods that followed a date of shiftwork within a data collection week. To determine if naps may have modified associations, we also ran models restricted to sleep periods on dates for which no naps occurred. To ensure our estimation of the association was not impacted by the combination of Fitbit algorithms used, we also ran models restricted to sleep observations from only the newer “Stages” algorithm. Finally, to evaluate if depression would potentially alter associations between walkability and sleep, we also ran a sensitivity analysis restricting participants who did not self-report doctor-diagnosed depression at enrollment.
Results
Participants in the NHS3 MHS were all female, majority White race, and employed with roughly equivalent representation across geographic regions (Table 1). The average age of participants was 39.6 years old (SD, 7.1). Participants had an average sleep duration of 7.9 hours (SD, 1.6) and an average sleep efficiency of 92.6% (SD, 8.0%). On average, each participant had 13 recorded sleep periods during the study period, with a mean of five sleep periods in each of the quarterly data collection weeks. Across the included sleep periods, the average walkability exposure of the wake period preceding sleep was 0.5 (SD, 2.8). The demographics of the participants included in the analysis did not differ meaningfully from demographics of those who provided Fitbit sleep data or of those who consented (eTable 1; http://links.lww.com/EE/A308).
Table 1.
Characteristics of the 276 female participants and 3592 sleep periods of the Nurses’ Health Study 3 Mobile Health Substudy with paired sleep and GPS data available
| Participant characteristic | Mean (SD) |
|---|---|
| Age (years) | 39.58 (7.10) |
| n (%) | |
| Advanced degree (% yes) | 71 (25.7) |
| Employed (% yes) | 260 (94.2) |
| Married (% yes) | 170 (61.6) |
| Race (% White) | 264 (95.7) |
| Depression (% yes) | 86 (31.2) |
| Region (%) | |
| Midwest | 66 (23.9) |
| Northeast | 64 (23.2) |
| South | 77 (27.9) |
| West | 69 (25.0) |
| Alcohol consumption (% ≥1 drink/day) | 6 (2.2) |
| Sleep period characteristic | Mean (SD) |
| Duration (hours) | 7.94 (1.61) |
| Efficiency (%) | 92.62 (8.00) |
| Greenness exposure during wake (NDVI) | 0.28 (0.16) |
| Walkability exposure during wake | 0.46 (2.75) |
| LAN exposure during sleep (nanoWatts/cm2/sr) | 25.29 (27.83) |
| Noise exposure during sleep (L50, dBA) | 44.68 (4.24) |
| Neighborhood SES exposure during wake | 1.95 (2.96) |
| Outdoor temperature exposure during sleep (°C) | 14.08 (9.11) |
| Duration (%) | n (%) |
| <7 hours | 794 (22.1) |
| 7–9 hours | 1,988 (55.3) |
| >9 hours | 810 (22.6) |
| Efficiency (%) | |
| <85% | 204 (5.7) |
| 85%–96% | 1,999 (55.7) |
| 96%–100% | 1,389 (38.7) |
| Season (%) | |
| Fall | 810 (22.6) |
| Spring | 810 (22.6) |
| Summer | 1,068 (29.7) |
| Winter | 904 (25.2) |
| Day of week (% weekends) | 1,006 (28.0) |
Advanced degree is a binary variable indicating whether the participant has a master’s degree in nursing or higher. Marital status is a binary variable for either never married or ever married (married, widowed, and divorced). Depression is self-reported diagnosis.
NDVI indicates Normalized Difference Vegetation Index.
Associations between walkability and sleep duration did not deviate from linearity. In our basic model, a one IQR increase in walkability exposure was associated with a 2.64 minute shorter sleep duration (95% confidence interval [CI]: −5.53, 0.25); after additionally adjusting for demographic variables, temporal variables, and environmental coexposures, the association was attenuated to a 1.77 minute shorter (95% CI: −4.99, 1.46) sleep duration (Table 2). In categorical analyses, compared to those who slept 7–9 hours, the odds ratio (OR) for each IQR increase in daily walkability exposure and low sleep duration (< 7h) was 1.03 (95% CI: 0.94, 1.13); meanwhile, for high sleep duration (>9 hours), the OR was 0.96 (95% CI: 0.86, 1.06).
Table 2.
Association between an IQR increase in walkability exposure on sleep duration and efficiency among 276 participants and 3592 sleep periods of the Nurses’ Health Study 3 Mobile Health Substudy
| Effect estimate (minutes) (95% CI) | ||||
|---|---|---|---|---|
| Continuous models | Basica | Adjustedb | ||
| Duration | −2.64 (−5.53, 0.25) | −1.77 (−4.99, 1.46) | ||
| Odds ratio (95% CI) | ||||
| Categorical models | n participant | n sleep | Basica | Adjustedb |
| Duration (7–9 hours referent) | ||||
| Low duration (<7 hours) | 272 | 2,782 | 1.04 (0.96, 1.13) | 1.03 (0.94, 1.13) |
| High duration (>9 hours) | 270 | 2,798 | 0.95 (0.87, 1.03) | 0.96 (0.88, 1.06) |
| Efficiency (85%–96% referent) | ||||
| Low efficiency (<85%) | 258 | 2,203 | 0.88 (0.62, 1.25) | 0.96 (0.66, 1.40) |
| High efficiency (>96%) | 263 | 3,388 | 1.05 (0.97, 1.14) | 1.06 (0.97, 1.16) |
Adjusted for age.
Adjusted for age, education, employment, alcohol consumption, marital status, race, season, weekend versus weekday, light-at-night exposure during sleep, noise exposure during sleep, temperature exposure during sleep, greenness exposure during wake, and neighborhood SES exposure during wake.
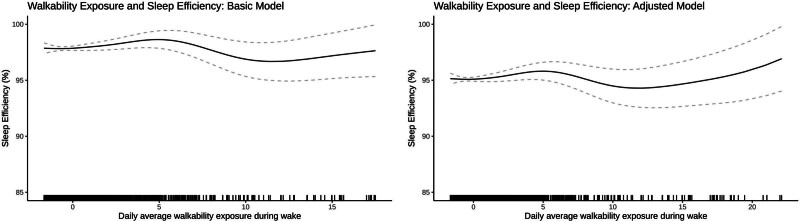
For sleep efficiency, due to evidence of nonlinearity, we modeled the continuous association with a penalized spline. Both the basic age-adjusted and fully adjusted models had a similar shape, with 5.1 and 4.6 effective degrees of freedom, respectively, but little evidence of an association between most levels of walkability and efficiency (Figure 2). In categorical analyses, the ORs for low (<85%) and high sleep efficiency (>96%) were 0.96 (95% CI: 0.66, 1.40) and 1.06 (95% CI: 0.97, 1.16), respectively (Table 2). All results were robust in sensitivity analyses (eTable 2 and eAppendix 1; http://links.lww.com/EE/A308).
Figure 2.
Associations between walkability exposure and sleep efficiency (%) among 276 participants and 3592 sleep periods of the Nurses’ Health Study 3 Mobile Health Substudy. Splines were restricted to predicted values ≤100% to retain interpretability.
Discussion
In our study of GPS-derived walkability exposure and sleep outcomes in the NHS3 MHS, we did not find evidence of associations between walkability and sleep duration, or sleep efficiency. Across models of continuous and categorical sleep duration and sleep efficiency, we observed null associations with walkability. We conducted several sensitivity analyses to account for if factors relating to sleep such as naps, shiftwork, and depression as well as the way sleep, estimated via the Fitbit algorithm may have impacted our findings; however, the associations remained stable. This study is the first to assess the association between walkability and sleep using objective sleep data collected with repeated measures across seasons with nationwide geographic dispersion and activity space for exposure assessment.
Prior studies of walkability and sleep duration have shown inconsistent findings; one study showed suggestive positive associations while another found negative associations.13,19 In contrast to the multiple 1-week data collection periods year-round in this study, each of these previous studies utilized data from single week-long periods. Our null findings are consistent with results reported in other previous studies.13,18,19
Differences in reported associations between walkability and sleep may reflect differences in how walkability scores are calculated.34 Prior studies looking at the connection between walkability and sleep have used a variety of measures including the nationwide Street Smart Walk Score or combinations of quantitative and qualitative measures of walkability on more local street-segment levels in specific neighborhoods.13,18,19 A related version of the walkability exposure metric employed in this study has been previously shown to be associated with physical activity in other cohorts of healthy adults, in addition to being associated with increased Fitbit-measured physical activity in this NHS3 MHS when assigned using GPS time-activity data to assign exposure.22,23,35
The demographic composition of the NHS3 MHS is largely early-middle-aged married White and educated women. Relative to prior studies of walkability and sleep, which were conducted in predominantly non-White and low-income cohorts such as the Multiethnic Atherosclerosis Study and the Pittsburgh Hill/Homewood Eating, Shopping, and Health Study, this study’s population is less generalizable to disadvantaged populations, due to differences in exposure distributions and potential confounders. The Fitbit-measured average sleep duration and efficiency in this cohort are comparable to longitudinal Fitbit measurements of sleep outcomes among free-living, healthy adults in other studies.36
This study has limitations. Walkability was assessed at Census tract spatial resolution; in accordance with the modifiable areal unit problem, there is possible bias due to the aggregated nature and arbitrary spatial size and shape of Census tracts. Additionally, walkability was calculated using three components, but other contextual aspects of walkability such as neighborhood safety (e.g., crime), presence of public transportation, and public spaces like parks that could influence behavior and sleep were not incorporated.37 As a study population, the NHS3 MHS may have limited generalizability due to its predominantly White and middle-to-high SES demographics. The lack of association between walkability and sleep in this population may reflect its relative affluence and homogenous racial composition. Studies conducted in more sociodemographically diverse populations are needed to determine whether these patterns hold. With respect to outcome assessment, research-grade accelerometry is still regarded as preferable over Fitbit devices for assessing sleep in free-living conditions, particularly due to the proprietary nature of their algorithms. However, the Fitbit devices used in the study have been validated against research-standard measures of accelerometry or polysomnography, with reports of small differences in both sleep duration and sleep efficiency in healthy populations, of discrepancies of at most 11 minutes and 8%, respectively.38–40 Additionally, due to their lower cost, Fitbits are more scalable for large-scale studies and are less prone to bias than subjective sleep measures.41
This study also has several strengths. To our knowledge, this study is the first to use GPS time-activity data and longitudinal objectively measured sleep outcomes to assess the relationship between neighborhood walkability and sleep. In contrast to prior work that largely relies on residential assignment of walkability, being able to account for mobility with minute-level GPS data across an individual’s activity space enabled us to reduce exposure measurement error by capturing both residential and nonresidential exposures.42 Additionally, the leveraging of fine temporal scale GPS data for exposure assessment enabled clear delineation of exposure during the wake period. With regards to confounding by environmental coexposures, we utilized available environmental exposure data, on the same spatial scale as the main exposure, to control for salient factors such as LAN and noise that may be correlated with both walkability and sleep.
In summary, we found that in this study GPS-derived walkability exposure was not associated with objectively measured sleep duration and efficiency in this nationwide cohort of women in the United States. In addition to contributing to the body of mixed evidence in the literature on walkability and sleep, this study illustrates the possibilities of integrating mobile health technologies such as smartphone GPS and wearables to interrogate the relationship between sleep and the built environment.
Conflicts of interest statement
The authors declare that they have no conflicts of interest with regard to the content of this report.
ACKNOWLEDGMENTS
We would like to thank the staff and participants of the Nurses’ Health Study 3, without whom this study would not have been possible.
Supplementary Material
Footnotes
Published online 10 October 2024
Funding for the cohort and these analyses came from National Institutes of Health grants U01 HL145386, R24 ES028521, R00 CA201542, P30 ES000002, and F31 ES035252.
The data used in our analyses are not publicly available due to privacy reasons. Researchers interested in obtaining access to NHS data and computing code should submit an external collaborator form (https://nurseshealthstudy.org/researchers).
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
References
- 1.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19:56–59. [DOI] [PubMed] [Google Scholar]
- 2.Zielinski MR, McKenna JT, McCarley RW. Functions and mechanisms of sleep. AIMS Neurosci. 2016;3:67–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grandner MA. Epidemiology of insufficient sleep and poor sleep quality. In: Sleep and Health. Elsevier; 2019:11–20. [Google Scholar]
- 4.Luyster FS, Strollo PJ, Zee PC, Walsh JK; Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep: a health imperative. Sleep. 2012;35:727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zee PC, Turek FW. Sleep and health: everywhere and in both directions. Arch Intern Med. 2006;166:1686–1688. [DOI] [PubMed] [Google Scholar]
- 6.Bobba B, Bacaro V, Crocetti E. Embedded in contexts: a systematic review of the longitudinal associations between contextual factors and sleep. Adolesc Res Rev. 2023;8:403–422. [Google Scholar]
- 7.Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev. 2016;25:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Billings ME, Hale L, Johnson DA. Physical and social environment relationship with sleep health and disorders. Chest. 2020;157:1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson CL, Gaston SA. Chapter 8 - The impact of environmental exposures on sleep. In: Grandner MA, ed. Sleep and Health. Academic Press; 2019:85–103. [Google Scholar]
- 10.Liu J, Ghastine L, Um P, Rovit E, Wu T. Environmental exposures and sleep outcomes: a review of evidence, potential mechanisms, and implications. Environ Res. 2021;196:110406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Astell-Burt T, Feng X, Kolt GS. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259 319 Australians. BMJ Open. 2013;3:e003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grigsby-Toussaint DS, Turi KN, Krupa M, Williams NJ, Pandi-Perumal SR, Jean-Louis G. Sleep insufficiency and the natural environment: results from the US behavioral risk factor surveillance system survey. Prev Med. 2015;78:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson DA, Hirsch JA, Moore KA, Redline S, Diez Roux AV. Associations between the built environment and objective measures of sleep. Am J Epidemiol. 2018;187:941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo YS, Song JY, Joo EY, et al. Outdoor artificial light at night, obesity, and sleep health: cross-sectional analysis in the KoGES study. Chronobiol Int. 2016;33:301–314. [DOI] [PubMed] [Google Scholar]
- 15.Lo RH. Walkability: what is it? J Urban. 2009;2:145–166. [Google Scholar]
- 16.Alnawwar MA, Alraddadi MI, Algethmi RA, Salem GA, Salem MA, Alharbi AA. The effect of physical activity on sleep quality and sleep disorder: a systematic review. Cureus. 2023;15:e43595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Philbrook LE, El-Sheikh M. Associations between neighborhood context, physical activity, and sleep in adolescents. Sleep Health. 2016;2:205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim B, Troxel WM, Dubowitz T, et al. Neighborhood built environments and sleep health: a longitudinal study in low-income and predominantly African-American neighborhoods. Am J Epidemiol. 2023;192:736–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Troxel WM, DeSantis A, Richardson AS, et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2018;41:zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bao Y, Bertoia ML, Lenart EB, et al. Origin, methods, and evolution of the three nurses’ health studies. Am J Public Health. 2016;106:1573–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fore R, Hart JE, Choirat C, et al. Embedding mobile health technology into the Nurses’ Health Study 3 to study behavioral risk factors for cancer. Cancer Epidemiol Biomarkers Prev. 2020;29:736–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rundle AG, Chen Y, Quinn JW, et al. Development of a neighborhood walkability index for studying neighborhood physical activity contexts in communities across the U.S. over the past three decades. J Urban Health. 2019;96:583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilt G, Roscoe C, Hu C, et al. Associations between minute-level smartphone-derived exposure to walkability and consumer wearable-derived physical activity in the US-based Nurses’ Health Study 3 Cohort 2018-2020. ISEE Conference Abstracts; 2022;2022(1). [Google Scholar]
- 24.US Census Bureau. American Community Survey 2015-2019 5-Year Data Release. 2020. Available at: https://www.census.gov/newsroom/press-kits/2020/acs-5-year.html. Accessed 25 August 2023. [Google Scholar]
- 25.Infogroup. Infogroup US Historical Business Data. 2016. doi:10.7910/DVN/PNOFKI
- 26.US Census Bureau. TIGER/Line Shapefiles. 2020. Available at: https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html. Accessed 15 February 2022. [Google Scholar]
- 27.Elvidge CD, Baugh K, Zhizhin M, Hsu FC, Ghosh T. VIIRS night-time lights. Int J Remote Sens. 2017;38:5860–5879. [Google Scholar]
- 28.Mennitt D, Sherrill K, Fristrup K. A geospatial model of ambient sound pressure levels in the contiguous United States. J Acoust Soc Am. 2014;135:2746–2764. [DOI] [PubMed] [Google Scholar]
- 29.Luzio MD, Johnson GL, Daly C, Eischeid JK, Arnold JG. Constructing retrospective gridded daily precipitation and temperature datasets for the conterminous United States. J Appl Meteorol Climatol. 2008;47:475–497. [Google Scholar]
- 30.DeVille NV, Iyer HS, Holland I, et al. Neighborhood socioeconomic status and mortality in the Nurses’ Health Study (NHS) and the Nurses’ Health Study II (NHSII). Environ Epidemiol. 2022;7:e235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Measuring Vegetation (NDVI & EVI). 2000. Available at: https://earthobservatory.nasa.gov/features/MeasuringVegetation/measuring_vegetation_2.php. Accessed 18 March 2022. [Google Scholar]
- 32.Wood SN. Generalized Additive Models: An Introduction with R. 2nd ed. CRC Press/Taylor & Francis Group; 2017. [Google Scholar]
- 33.Begg CB, Gray R. Calculation of polychotomous logistic regression parameters using individualized regressions. Biometrika. 1984;71:11–18. [Google Scholar]
- 34.Hajna S, Ross NA, Brazeau AS, Bélisle P, Joseph L, Dasgupta K. Associations between neighbourhood walkability and daily steps in adults: a systematic review and meta-analysis. BMC Public Health. 2015;15:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilt GE, Roscoe CJ, Hu CR, et al. Minute level smartphone derived exposure to greenness and consumer wearable derived physical activity in a cohort of US women. Environ Res. 2023;237:116864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perez-Macias JM, Jimison H, Korhonen I, Pavel M. Comparative assessment of sleep quality estimates using home monitoring technology. In: 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA. 2014:4979–4982. [DOI] [PubMed] [Google Scholar]
- 37.Roscoe C, Hu CR, Villeneuve PJ. Invited perspective: studying walkability and cancer incidence—a step in the right direction. Environ Health Perspect. 2023;131:101301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Performance assessment of new-generation Fitbit technology in deriving sleep parameters and stages. Chronobiol Int. 2020;37:47–59. [DOI] [PubMed] [Google Scholar]
- 39.Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Accuracy of wristband Fitbit models in assessing sleep: systematic review and meta-analysis. J Med Internet Res. 2019;21:e16273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menghini L, Yuksel D, Goldstone A, Baker FC, de Zambotti M. Performance of Fitbit Charge 3 against polysomnography in measuring sleep in adolescent boys and girls. Chronobiol Int. 2021;38:1010–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilt GE, Roscoe C, Hu CR, et al. Examining exposure differences between residential and smartphone mobility-based greenness in a cohort of the Nurses’ Health Study. Environ Health Perspect. 2023;131:117701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.