Abstract
Background:
Breast reduction, the seventh most performed plastic surgery globally, has witnessed a significant increase in procedures over recent years. Various techniques exist, each with its advantages and complications, emphasizing the critical role of preoperative marking. Although existing literature focuses on different reduction mammaplasty techniques, limited attention is given to surgical preoperative marking. This study introduces a “mosque tower” pattern combined with a superomedial pedicle, aiming to minimize complications and standardize the design based on individualized factors such as patient characteristics and predicted breast reduction weight.
Methods:
The retrospective case series includes 103 women who underwent reduction mammaplasty between 2017 and 2020. Surgical marking is described, and complications are recorded. The study categorizes breasts into three groups based on key-hole dimensions, correlating them with predicted resection weight. Statistical analysis establishes a rationale formula for selecting key-hole size.
Results:
A total of 175 breasts were reduced in 103 women with an average follow-up of 29.8 months. The mean resection weight was 883 g per breast (range: 490–2531). A complication rate of 8% was observed, with only 2.8% experiencing wound breakdown, notably lower than reported rates in other studies. Key-hole dimension as a predicting variable was correlated significantly with resection weight.
Conclusions:
The mosque tower pattern proves to be an effective, safe, and reproducible method for preoperative marking in reduction mammaplasty. The study emphasizes the importance of individualized planning to achieve satisfactory results, particularly for surgeons in their early practice.
Takeaways
Question: Is it possible to standardize the marking for a safe reduction mammaplasty?
Findings: A total of 175 breasts were reduced in 103 women, using a mosque tower pattern for surgical marking and a septum-superomedial technique. A complication rate of 8% was observed, with only 2.8% experiencing wound breakdown.
Meaning: The mosque tower pattern proves to be a safe and reproducible method for preoperative marking in reduction mammaplasty.
INTRODUCTION
Breast reduction is the seventh most performed procedure by plastic surgeons worldwide and, according to the 2019 International Society of Aesthetic Plastic Surgery statistics, it showed a 12.3% increase over the number of procedures performed in 2018 and even a 41.9% increase compared to 2015.1
Reduction mammaplasty not only helps women to resolve physical symptoms and functional limitations,2–5 such as relief of pain and improved ability to participate in physical activity, but has also been shown to significantly enhance self-image and self-confidence and reduce the emotional strain produced by related anxiety and depression.6–12
The aim of reduction mammaplasty surgery is to create an appropriately sized breast of good shape, with longevity of outcome. During the procedure, it is essential to reposition the nipple-areola complex (NAC) in an anatomically correct position; maintain the vascular support and the skin sensation to the NAC; and remove the excessive skin, ensuring a tension-free closure.13,14
So far, several breast reduction techniques using a different combination of skin patterns and pedicle design as well as suction or ultrasound-assisted lipectomy and free nipple grafting have been described,15 each with its own advantages and complications. Specifically, delayed wound healing represents the most prevalent postoperative complication after reduction mammoplasty, and it has shown associations with factors such as breast resection volume, smoking, and advanced age.16–18 The choice of pedicle also plays a crucial role in postoperative complications, as the pedicle’s direction influences the location and weight of tissue resection, as well as the blood supply to the remaining breast tissue and NAC. Research has also explored the impact of the skin incision on postoperative complications in reduction mammoplasty. Indeed, a meta-analysis comparing complications between vertical scar and inverted T scar reduction techniques revealed a significantly lower overall incidence of complications with the vertical scar methods.19
Given these premises, the search of literature yields several articles that focus on the different reduction mammaplasty techniques, mainly comparing the different pedicles. Nevertheless, very few articles focus on surgical preoperative marking, though it represents the first skill young surgeons and physicians in training are asked to understand and learn.
The current study was designed to develop a method to accurately perform the preoperative marking of reduction mammaplasty using a mosque tower pattern combined with a superomedial pedicle, trying to minimize complications and to standardize the design on an individualized basis according to the patient and the predicted breast reduction weight.
MATERIALS AND METHODS
Patient Selection
The study was designed as a retrospective case series of prospectively collected data. All patients who underwent reduction mammaplasty between January 2017 and December 2020 were identified from our institution’s digital database. Inclusion criteria were women who (1) were candidates for bilateral reduction mammaplasty for symptomatic breast hypertrophy and (2) were candidates for unilateral reduction mammaplasty for contralateral breast symmetrization after breast cancer surgery. Exclusion criteria were women who (1) were candidates for reduction mammaplasty and free nipple graft (Toreck procedure), (2) had a secondary breast reduction procedure, and (3) had clinical or radiological evidence of a suspicious breast lump.
Preoperative details recorded on the day of admission for surgery were age, body mass index (BMI), smoking status, sternal notch-to-nipple distance (NTN), and nipple-to-inframammary fold (IMF) distance, both in centimeters. Physical examination was performed for all patients preoperatively, and all women underwent preoperative mammography.
This study was conducted according to the Declaration of Helsinki and its later amendments. A signed consent form was obtained from all the patients who participated in the study before surgery. The work has been reported in line with Strengthening the Reporting of Observational Studies in Epidemiology guidelines. No donor or funder had a role in the design or conduct of the study, the collection or analyses of the data, or the preparation of the article.
Marking and Surgical Technique
The patients are marked in the standing position. The mid sternal line, the meridian line (starting from the mid clavicular point 6.5–8 cm from the sternal notch down to the IMF) and the IMF line are drawn.
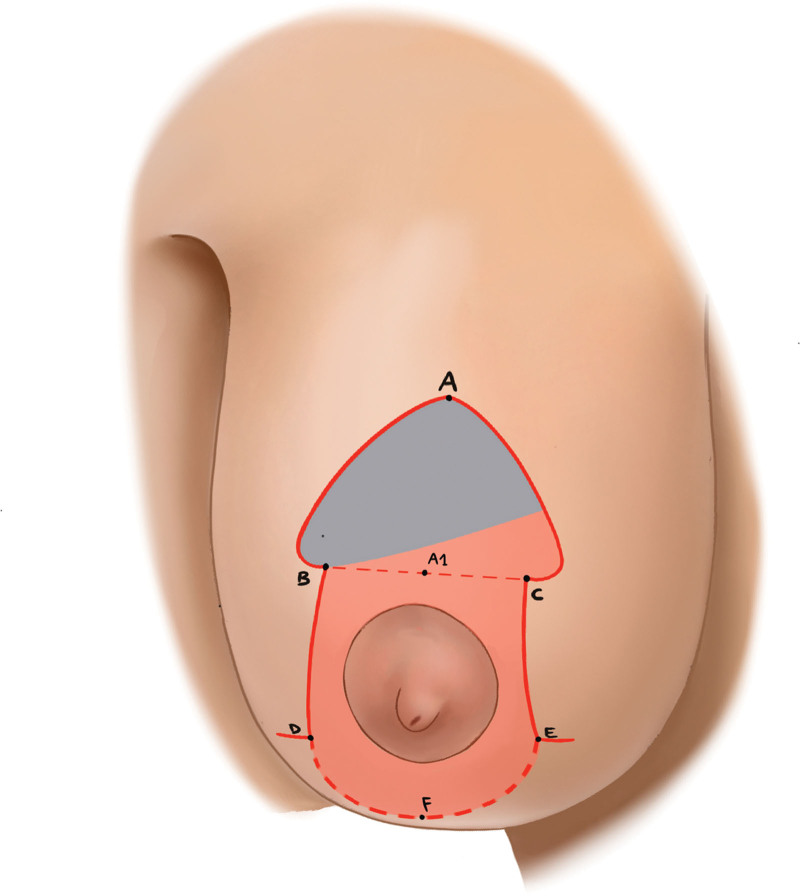
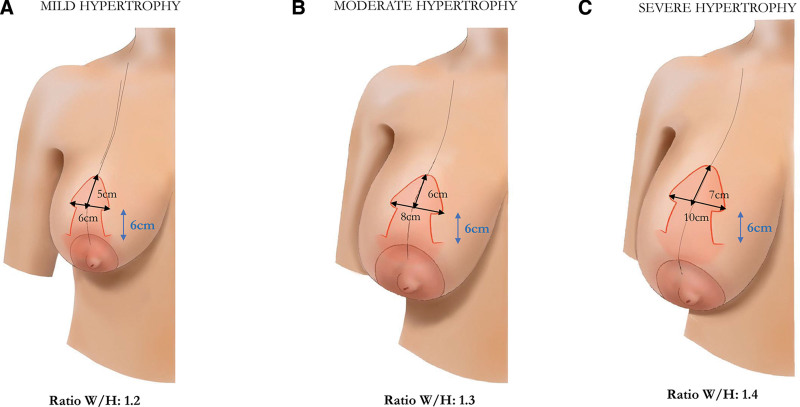
The skin pattern is drawn customized for each patient, and it is schematized in Figure 1. The Pitanguy point, namely, the position of the new NAC, is determined by placing the index finger, slightly lower the IMF and is marked on the breast on the meridian line.20 The new superior border of the areola (point A) is outlined approximately 2 cm over this marking. Along the breast meridian, starting from point A at a distance of 5, 6, or 7 cm, depending on the degree of breast ptosis, point A′ is positioned. At this level, a line is drawn orthogonal to the breast meridian, measuring 6, 8, or 10 cm, depending on breast hypertrophy. Points B and C correspond to the edges of this line. Point A is joined to points B and C on each side. The resulting triangular profile, with a base width of 6, 8, or 10 cm and a height of 5, 6, or 7 cm, is then smoothed to a curvilinear profile, wider at the base, to avoid creating acute angles and make it suitable for suturing to the areola, which has a circular profile. The resulting periareolar marking is drawn free-hand as a mosque-shaped pattern (Fig. 2).
Fig. 1.
Schematic drawing showing the mosque tower–shaped pattern for reduction mammaplasty. The new superior border of the areola (point A) is outlined approximately 2 cm over the Pitanguy point along the breast meridian. Along the same line, starting from point A at a distance of 5, 6, or 7 cm, depending on the degree of breast ptosis, point A is positioned. At this level, a line is drawn orthogonal to the breast meridian (dotted line), measuring 6, 8, or 10 cm, depending on breast hypertrophy. Points B and C correspond to the edges of this line. Point A is joined to points B and C on each side. Two vertical lines, measuring 6 cm, are traced caudally on each side, extending from points B and C toward the IMF (points D and E). The pedicle supplying the NAC (septum-superomedial) is marked in red superiorly with a line from two-thirds of the A–C distance toward point B and inferiorly with a U-shaped lined which surrounds the areola before ending at the base of the medial vertical line (from points D to E) and corresponds to the area that will be de-epithelialized. The wedge of skin and glandular tissue that will be removed is marked.
Fig. 2.
Schematic drawings showing the dimensions of the mosque-shaped skin marking according to breast hypertrophy and ptosis. A, Mild hypertrophy. B, Moderate hypertrophy. C, Severe hypertrophy.
Two vertical lines, measuring 6 cm, are traced caudally on each side, extending from the lower limit of the new areolar opening (points B and C) toward the IMF (points D and E). These will correspond to the pillars length. As a whole, the skin marking of the mosque-shaped dome and the vertical pillars has been called the masque tower pattern.
The pedicle supplying the NAC (septum-superomedial) is marked superiorly with a line from two-thirds of the A–C distance toward point B and inferiorly with a U-shaped line which surrounds the areola before ending at the base of the medial vertical line (from points D to E).
The operation is performed under general anesthesia with the patient in supine position and a marginal reverse Trendelenburg position. The principle is that the majority of the reduction comes from the inferolateral portion of the breast, preserving the maximally vascularized central pyramidal flap to carry the NAC vascularization and innervation.
The new NAC size is marked using a 42-mm-diameter nipple marker. The marked pedicle is de-epithelialized. A wedge of skin and glandular tissue is excised inside the mosque-shaped pattern above the areola to provide a new space to lift the NAC. A wide undermining is performed in the upper quadrants of the breast to create enough space to accommodate the breast tissue that will be lifted. The septum-superomedial pedicle is harvested, keeping superficial the curved incision from B to D to preserve the lateral neurovascular bundle. Two Monocryl 2-0 stay sutures are placed between the new areolar opening and the areola at the 12 and 6 o’clock positions (points A and B–C). Stay sutures offer several advantages at this stage: traction of the sutures toward the zenith gives a three-dimensional perspective of the new breast, which favors size estimation between both breasts and helps during pillar closure. The medial and lateral pillars are shaped. Three deep Vicryl sutures to provide breast conization and improve breast projection are positioned. [See Video 1 (online), which displays the preoperative skin marking.]
Video 1. which displays the preoperative skin marking.
A setup suture is placed joining points D and E with point F along the breast meridian at the IMF, creating the skin flap’s T junction. The horizontal transversal parenchyma excision of the inferior quadrants is planned and marked at this point according to each patient’s needs (on-demand). The breast is initially incised at the level of the IMF. The horizontal excision is performed: the median portion first and then the lateral and medial ones, taking care to first de-epithelialize the medial and lateral triangles to create two inferior dermal slings. With the patient in a semi-upright position, the medial triangular dermal flap is sutured to the lateral aspect of the pectoralis muscle fascia, and the lateral triangular dermal flap to the chest wall at the same level as the medial triangle to complete the dermal suspensory hammock.21 [See Video 2 (online), which displays the steps of horizontal parenchyma excision. Breast conization and harvest and set of the lateral inferior dermal flap are shown.]
Video 2. which displays the steps of horizontal parenchyma excision. Breast conization and harvest and set of the lateral inferior dermal flap are shown.
To reduce the stress between the areola edge and the outer breast tegument circumference, areola closure is performed through a Prolene 3-0 interlocking suture.22 Care is taken to dip the knot into povidone-iodine and carefully bury it under adequate soft tissue, held in position with a single overlying small caliber resorbable suture.
Considering the characteristics of the technique with no skin undermining, drains usually could not be used. When drains are used, they should be removed when the output is less than 25–30 mL in 24 hours. Because bacteria are present in breast ducts, we think it is appropriate to administer an antibiotic prophylaxis (cefazolin 2 g) that, for large breast reductions in patient with higher BMI (>30 kg/m2), can be continued postoperatively.23 Patients are asked to wear a surgical brassiere for at least 1 month after surgery to provide good support.
Study Hypothesis and Data Analysis
The senior author has refined the technique described earlier for the preparatory marking empirically, based on the breast size and the predicted breast volume to be removed. In view of optimization of the procedure, designed to make the most possible repetitive and standard marking, the breasts were separated into three groups according to the key-hole size and, specifically, on the basis of two variable dimensions: the width (W) of the base and the vertical height (H) dimension of the mosque dome:
Group A: base width: 6 cm; vertical height: 5 cm (ratio W/H: 1.2).
Group B: base width: 8 cm; vertical height: 6 cm (ratio W/H: 1.3).
Group C: base width: 10 cm; vertical height: 7 cm (ratio W/H: 1.4).
The weight of the breast tissue resected was recorded for each breast intraoperatively. The charts of the patients were reviewed for early and late postoperative complications.
Statistical analysis was performed using the IBM SPSS Statistics, version 25. Data were analyzed with multiple regression analysis separately on each breast with the key-hole dimensions as a dependent variable and the resected breast weight as an independent variable. The hypothesis was to establish a reliable “rationale” formula for choosing the key-hole size from the predicted resection weight.
RESULTS
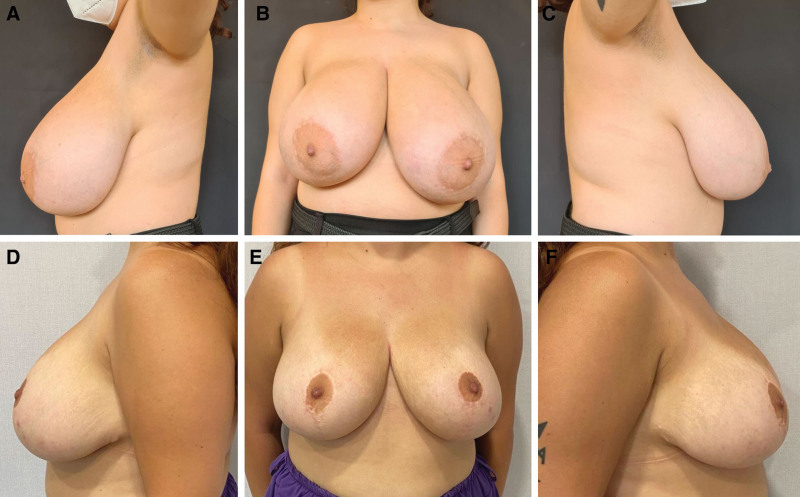
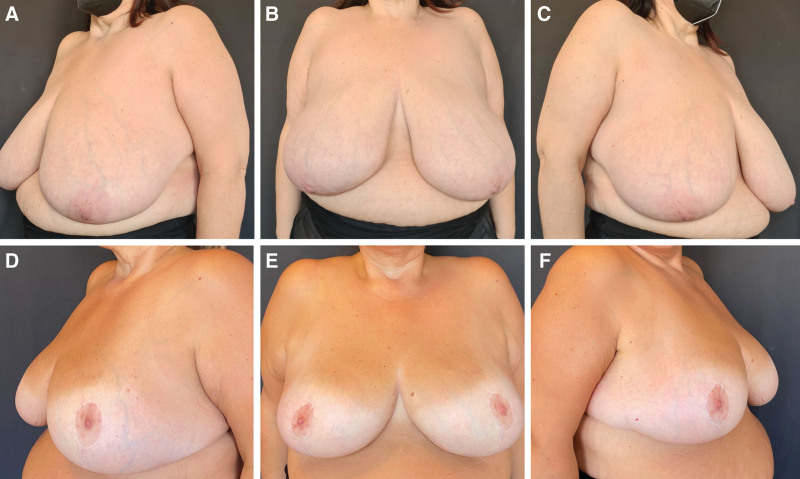
A total of 175 breasts were reduced in 103 women, with an average follow-up time of 29.8 months (range: 12–54 mo). Indications for surgery were symptomatic breast hypertrophy in 72 women and contralateral breast symmetrization after breast cancer surgery in 31 patients. The mean age of the patients was 41.2 years (range: 25–66 y) and the majority of them (73.8%) had a BMI of 30 kg/m2 or less. The mean sternal NTN distance was 31.11 cm (SD: 4.68 cm; range: 24–41.2 cm). The mean resection weight was 883 g per breast (range: 490–2531). The sample size was composed as follows: group A, 37 breasts; group B, 81 breasts; and group C, 57 breasts (Figs. 3, 4). The demographic and surgical data are listed in Table 1. [See figure, Supplemental Digital Content 1, which displays a 54-year-old patient affected by breast ptosis and mild breast hypertrophy (panels above). Preoperative marking was performed according to group A key-hole dimensions. Intraoperative resection weight was on average 380 g per side. Postoperative pictures at 48 months of follow-up (panels below), http://links.lww.com/PRSGO/D552.]
Fig. 3.
Clinical case, group B. A-C, 42-year-old patient affected by breast ptosis and moderate breast hypertrophy. Preoperative marking was performed according to group B key-hole dimensions. Intraoperative resection weight was on average 620 g per side. D-F, Postoperative pictures at 40 months of follow-up.
Fig. 4.
Clinical case, group C. A-C, 55-year-old patient affected by breast ptosis and severe breast hypertrophy. Preoperative marking was performed according to group C key-hole dimensions. Intraoperative resection weight was on average 870 g per side. D-F, Postoperative pictures at 44 months of follow-up.
Table 1.
Patient Data
| Mean or Count | SD or % | Range | |
|---|---|---|---|
| Patient characteristics | |||
| Age, y | 41.2 | 14.83 | 25–66 |
| Smoking status | |||
| Nonsmoker | 75 | 72.8% | — |
| Smoker | 28 | 27.2% | — |
| BMI, kg/m2 | 28.18 | 3.2 | 22–35 |
| <25 | 18 | 17.47% | |
| 25–30 | 58 | 56.31% | |
| >30 | 27 | 26,21% | |
| Indication for surgery | |||
| Symptomatic breast hypertrophy | 72 | 69.9% | — |
| Contralateral breast symmetrization | 31 | 30.1% | — |
| NTN distance, cm | 31.11 | 4.68 | 24–41.2 |
| <30 | 96 | 54.86% | — |
| >30 | 79 | 45.14% | |
| Surgical outcomes | |||
| Tissue removed (tot), g | |||
| <500 | 55 | 31.4 | |
| 500–800 | 91 | 52 | |
| >800 | 29 | 16.6 | |
| Follow-up, mo | 29.8 | 9.8 | 12–54 |
Within 1 month after the operation, minor complications occurred in nine patients and 15 breasts, for a total complication rate of 8%. No major complications and no further complications occurred in the remaining follow-up months. Five women out of the nine were smokers. A total of five breasts (2.8%) in three women had wound dehiscence, of which four were treated by conservative therapy and dressing change, and the remaining one needed surgical revision. A total of 25% of the wound problems were located at the T-junction. Surgical site infection occurred in five breasts (2.8%), treated with antibiotics. Only a single breast (1.5%) presented partial NAC necrosis. No removed tissue showed malignancy (Table 2). The lower pole arc length (distance from lower areolar border to IMF) was measured intraoperatively at 6 ± 0.5 cm (average ± SD). At 24 months, the lower pole arc length was 6.8 ± 0.7 cm, representing an average increase of 13.3% ± 4%. At the latest follow-up, no revisional procedures were performed.
Table 2.
Surgical Complications
| Complications | No. Breasts (175) | Percentage |
|---|---|---|
| Areola widening or distortion | 18 | 10.2 |
| Weak nipple sensation (6 mo) | 2 | 1.1 |
| Loss of the NAC | 1 (partial) | 0.5 |
| Fat necrosis | 1 | 0.5 |
| Seroma requiring drainage | 0 | 0 |
| Hematoma | 2 | 1.1 |
| Delayed healing | 5 | 2.8 |
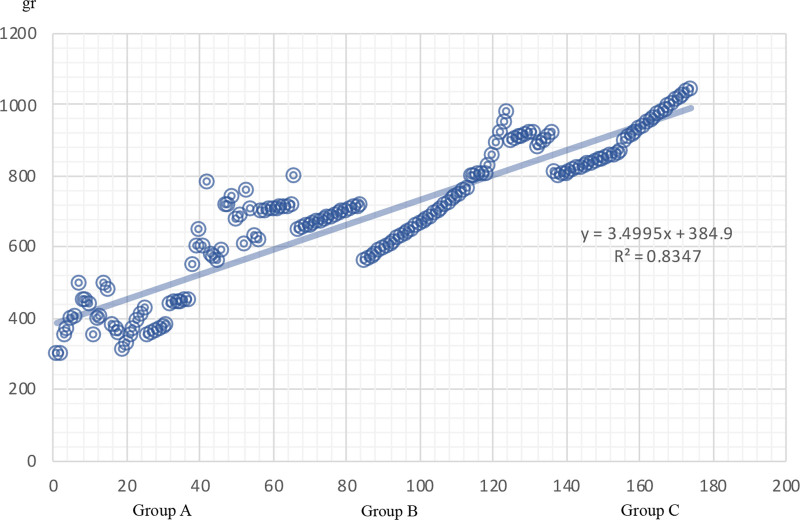
Key-hole dimension as a predicting variable was correlated significantly with resection weight (Pearson correlation coefficient = 0.08099). Specifically, group A was correlated with a resection weight less than 500 g, group B with a resection weight of 500–800 g, and group C with a resection weight greater than 800 g (Fig. 5).
Fig. 5.
Correlation between predicted weight removed according to preoperative surgical marking (x axis) and postoperative weight removed (y axis) expressed in grams. The graph shows the positive correlation between the key-hole dimension and the resection weight.
DISCUSSION
Several different vascular pedicles and skin incisions have been described for reduction mammoplasty. Different methods may be more optimal for certain patients, and thus, a pedicle selection and skin excision pattern should be always considered independently. In this setting, the authors are not debating about NAC pedicle selection, as a septum-superomedial pedicle technique with simultaneous preservation of the breast septum24 (SSM mammaplasty) has become the preferred method of reduction mammaplasty at our institution.25,26 The SSM technique has been noted to ensure adequate vascularity of the NAC, to decrease operation time and to provide better cosmetic durability with less bottoming out or pseudoptosis and fuller medial volume.25–28
Conversely, the authors aimed to focus on a “new skin pattern” and the related preoperative skin marking, on the one hand, providing a guide for preoperative planning according to the breasts’ ptosis and hypertrophy, and on the other hand, trying to minimize the occurrence of complications.
Regarding the first objective, the senior author has sought to standardize a free-hand marking approach and to convert it in numbers, firmly believing that standard Wise-pattern templates do not accommodate individual patients’ needs and fail to consider potential asymmetries.29,30 The mosque dome areolar marking can also be adapted to the different sizes of breasts without influencing the circular shape of the areola.31
The marking and the described technique could resemble the breast reduction mainly described by Hall-Findlay32 for the shape of the new areola opening and the vertical orientation of the vertical lines, which do not extend out laterally and medially. Nevertheless, they differ for a variety of reasons which represent the described technique’s novelty features.
First, the size of the mosque-shaped areola opening is not standard. The variability in the design itself (what we have termed as ratio) is intended to adapt to the patient’s anthropometric measurements and to the degree of breast hypertrophy and ptosis. Indeed, the results of the regression analysis confirmed the existence of a correlation between the dimensions of the skin marked incision pattern and the amount of tissue to be resected. If surgeons then want to calibrate the reduction of breast parenchyma also in relation to the patient’s requirements, the described preoperative marking enables them to do that. The dimensions of the mosque-shaped pattern must be respected in their ratios, but it is possible to modulate the extent of resection in the lower pole (on-demand intraoperatively). The authors find it useful in this case to have an approximate preoperative understanding of the extent of tissue removal, making patient consultation and communication more transparent. Moreover, it fits with the ongoing debate in research on identifying a method that can predict the final cup size, an area that still lacks a singular consensus in the literature, with many methods proposed, mainly based on anthropomorphic measurements which are limited by diverse female physiognomy.30,33,34 With a view to simplifying the procedure, the marking is entirely performed preoperatively in the upright position, including the periareolar one, to manage any asymmetry rather than leaving this step to the intraoperatory phase with the risk of position bias.
Second, the vertical lines are drawn vertically oriented parallel to each other, without converging to the nipple, as in the Bisemberg maneuver. The Bisemberg maneuver makes the preoperative marking fully operator-dependent with the possibility to change according to individual experience and strengths. The authors’ technical choice makes the marking reproducible and has the rationale of keeping the tension at the T joint at minimum level. The length of the vertical lines is fixed at 6 cm considering that they tend to elongate over time. As for the presented case series, an average elongation of 13.3% ± 4% was observed at 24 months of follow-up.
Third, the location of the parenchyma excision differs between the authors’ technique and the mammaplasty described by Hall-Findlay. The parenchyma excision is not circumvertical. Indeed, the orientation of the pedicle is superomedial and not purely medial. Furthermore, the Wuringer septum is preserved to maintain three vascular sources for the CAC, making the technique suitable for severe hypertrophic and ptotic breasts. With an incision limited exclusively to the dermal layer on the lateral side (from B to D), the lateral neurovascular bundle for the CAC is also preserved.19,35 The resulting NAC pedicle is lifted without rotation into its new position, as if it were an auto-augmentation, filling the upper quadrants of the breast and reducing the risk of areola congestion. This is an additional advantage of the presented technique. (See Supplemental Digital Content 1, http://links.lww.com/PRSGO/D552.)
The breast tissue is first removed inside the mosque-shaped pattern above the areola and then horizontally in the lower ptotic quadrants of the breast after breast conization. An additional difference is that the authors do not mark preoperatively the horizontal excision according to a standard pattern, but they still perform it at the end of the procedure, marking an area that is customized for each patient (on-demand). And, in any case, breast conization is always performed before the horizontal breast excision to precisely calibrate the amount of breast tissue that needs to be removed in the lower quadrants and best balance any breast asymmetries.
Regarding the second objective, connected to the first, the skin pattern is one of the factors that can explain the onset of certain postoperative complications, especially those related to wound dehiscence, along with other known risk factors.19 Current literature has demonstrated complication rates in reduction mammoplasty to vary significantly (range from 4% to 63%).18 Complications are reported to be most commonly minor and related to delayed wound healing. The wound complications have been reported to occur commonly at the point of greatest stress or tension on the closure. Especially in the inferior pedicle with inverted T skin incision, the tension lies to the skin over the breast parenchyma to maintain the desired shape. Furthermore, in the superomedial pedicle technique combined with inverted T incision, the main support is glandular, but the closure of skin flaps at a single point creates excess tension and possibility for wound breakdown at that point. The skin pattern presented by the authors has been modified compared with the classical Wise pattern to make the marking of the vertical pillars effectively oriented in a more vertical longitudinal axis, decreasing the tension on the T-junction point. The results of the presented study showed an incidence of wound breakdown of 4%, of which only 25% were located at the T-junction, data relatively lower compared with those reported in other studies18 (wound healing problems located at tripod zone in 35% of superomedial pedicle and 37% of inferior pedicle patients). Certain intraoperative strategies may further contribute to the decrease of wound-related complications, such as the creation of the inferior triangular dermal slings. The use of dermal flaps as a hammock contributes to supporting the more cranially positioned glandular tissue, reducing the tension on the T-junction but also protecting against lower pole lengthening with a stable result over time.21 Indeed, at the latest follow-up, no revisional procedure for the correction of breast pseudoptosis has been performed. Inferior dermal slings have been demonstrated to be useful, especially in the presence of risk factors generally associated with worse outcomes (weight loss, multiparity, and bad skin quality).
To avoid another common minor complication of the procedure, namely areola widening, an interlocking suture22 is always performed. The reason is to reduce the stress between the areola edge and the outer breast tegument circumference because of the inevitable discrepancy between the areola diameter and the outer edge of the wound circumference. The circular inset does not usually need to be revised at the time of closure. A minimal irregularity of the areola profile could result, but it can be treated with dermopigmentation.
As a final consideration, as the mammaplasty is the result of a combination of the choice of the NAC pedicle and the skin marking, the described preoperative skin marking can be theoretically applied with other NAC pedicles, such as the inferior one. The rationale behind some of the skin marking choices (mosque dome rather than standard Wise pattern, vertically oriented pillars) are intrinsic to the marking itself and not to the chosen pedicle.
CONCLUSIONS
Breast marking determines the amount of skin and breast tissue to be removed. The mosque tower pattern for the preoperative marking in reduction mammaplasty appears to be an easy, safe, and reproducible method for surgical planning, adaptable to various grades of breast hypertrophy and ptosis. Certain intraoperative strategies along with adequate preoperative markings can thoroughly help to simplify a breast reduction and achieve satisfactory results, especially for trainees or surgeons in the early days of their practice.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 11 October 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Viscardi JA, Oranges CM, Schaefer DJ, et al. Reduction mammoplasty: a ten-year retrospective review of the omega resection pattern technique. J Clin Med. 2021;10:4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boschert MT, Barone CM, Puckett CL. Outcome analysis of reduction mammaplasty. Plast Reconstr Surg. 1996;98:451–454. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez F, Walton RL, Shafer B, et al. Reduction mammaplasty improves symptoms of macromastia. Plast Reconstr Surg. 1993;91:1270–1276. [DOI] [PubMed] [Google Scholar]
- 4.Rogliani M, Gentile P, Labardi L, et al. Improvement of physical and psychological symptoms after breast reduction. J Plast Reconstr Aesthet Surg. 2009;62:1647–1649. [DOI] [PubMed] [Google Scholar]
- 5.Collins ED, Kerrigan CL, Kim M, et al. The effectiveness of surgical and nonsurgical interventions in relieving the symptoms of macromastia. Plast Reconstr Surg. 2002;109:1556–1566. [DOI] [PubMed] [Google Scholar]
- 6.Strong B, Hall-Findlay EJ. How does volume of resection relate to symptom relief for reduction mammaplasty patients? Ann Plast Surg. 2015;75:376–382. [DOI] [PubMed] [Google Scholar]
- 7.Spector JA, Karp NS. Reduction mammaplasty: a significant improvement at any size. Plast Reconstr Surg. 2007;120:845–850. [DOI] [PubMed] [Google Scholar]
- 8.Hernanz F, Fidalgo M, Muñoz P, et al. Impact of reduction mammoplasty on the quality of life of obese patients suffering from symptomatic macromastia: a descriptive cohort study. J Plast Reconstr Aesthet Surg. 2016;69:e168–e173. [DOI] [PubMed] [Google Scholar]
- 9.Iwuagwu OC, Stanley PW, Platt AJ, et al. Effects of bilateral breast reduction on anxiety and depression: results of a prospective randomised trial. Scand J Plast Reconstr Surg Hand Surg. 2006;40:19–23. [DOI] [PubMed] [Google Scholar]
- 10.Saariniemi KM, Joukamaa M, Raitasalo R, et al. Breast reduction alleviates depression and anxiety and restores self-esteem: a prospective randomised clinical trial. Scand J Plast Reconstr Surg Hand Surg. 2009;43:320–324. [DOI] [PubMed] [Google Scholar]
- 11.Romeo M, Cuccia G, Zirilli A, et al. Reduction mammaplasty and related impact on psychosexual function. J Plast Reconstr Aesthet Surg. 2010;63:2112–2116. [DOI] [PubMed] [Google Scholar]
- 12.Mello AA, Domingos NAM, Miyazaki MC. Improvement in quality of life and self-esteem after breast reduction surgery. Aesthetic Plast Surg. 2010;34:59–64. [DOI] [PubMed] [Google Scholar]
- 13.Wong C, Vucovich M, Rohrich R. Mastopexy and reduction mammoplasty pedicles and skin resection patterns. Plast Reconstr Surg Glob Open. 2014;2:e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greco R, Noone B. Evidence-based medicine: reduction mammaplasty. Plast Reconstr Surg. 2017;139:230e–239e. [DOI] [PubMed] [Google Scholar]
- 15.Purohit S. Reduction mammoplasty. Indian J Plast Surg. 2008;41:S64–S79. [PMC free article] [PubMed] [Google Scholar]
- 16.Simpson AM, Donato DP, Kwok AC, et al. Predictors of complications following breast reduction surgery: a National Surgical Quality Improvement Program study of 16,812 cases. J Plast Reconstr Aesthet Surg. 2019;72:43–51. [DOI] [PubMed] [Google Scholar]
- 17.Winter R, Haug I, Lebo P, et al. Standardizing the complication rate after breast reduction using the Clavien-Dindo classification. Surgery. 2017;161:1430–1435. [DOI] [PubMed] [Google Scholar]
- 18.Palve J, Kuuskeri M, Luukkaala T, et al. Predictive risk factors of complications in reduction mammoplasty-analysis of three different pedicles. Gland Surg. 2022;11:1309–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z, Qian B, Wang Z, et al. Vertical scar versus inverted-T scar reduction mammaplasty: a meta-analysis and systematic review. Aesthetic Plast Surg. 2021;45:1385–1396. [DOI] [PubMed] [Google Scholar]
- 20.Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20:78–85. [DOI] [PubMed] [Google Scholar]
- 21.Watfa W, Zaugg P, Baudoin J, et al. Dermal triangular flaps to prevent pseudoptosis in mastopexy surgery: the hammock technique. Plast Reconstr Surg Glob Open. 2019;7:e2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hammond DC, Khuthaila DK, Kim J. The interlocking Gore-Tex suture for control of areolar diameter and shape. Plast Reconstr Surg. 2007;119:804–809. [DOI] [PubMed] [Google Scholar]
- 23.Shortt R, Cooper MJ, Farrokhyar F, et al. Meta-analysis of antibiotic prophylaxis in breast reduction surgery. Plastic Surg (Oakv). 2014;22:91–94. [PMC free article] [PubMed] [Google Scholar]
- 24.Würinger E, Mader N, Posch E, et al. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101:1486–1493. [DOI] [PubMed] [Google Scholar]
- 25.Bucaria V, Elia R, Maruccia M, et al. Why choose the septum-supero-medial (SSM)-based mammaplasty in patients with severe breast ptosis: an anatomical point of view. Aesthetic Plast Surg. 2018;42:1439–1446. [DOI] [PubMed] [Google Scholar]
- 26.Giudice G, Maruccia M, Vestita M, et al. The medial-central septum based mammaplasty: a reliable technique to preserve nipple-areola complex sensitivity in post bariatric patients. Breast J. 2019;25:590–596. [DOI] [PubMed] [Google Scholar]
- 27.DeLong MR, Chang I, Farajzadeh M, et al. The central mound pedicle: a safe and effective technique for reduction mammaplasty. Plast Reconstr Surg. 2020;146:725–733. [DOI] [PubMed] [Google Scholar]
- 28.Bauermeister AJ, Gill K, Zuriarrain A, et al. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72:410–418. [DOI] [PubMed] [Google Scholar]
- 29.Tenna S, Cogliandro A, Cagli B, et al. Breast hypertrophy and asymmetry: a retrospective study on a sample of 344 consecutive patients. Acta Chir Plast. 2012;54:9–12. [PubMed] [Google Scholar]
- 30.Descamps MJL, Landau AG, Lazarus D, et al. A formula determining resection weights for reduction mammaplasty. Plast Reconstr Surg. 2008;121:397–400. [DOI] [PubMed] [Google Scholar]
- 31.Paloma V, Samper A, Sanz J. A simple device for marking the areola in Lejour’s mammaplasty. Plast Reconstr Surg. 1998;102:2134–5; discussion 2136. [DOI] [PubMed] [Google Scholar]
- 32.Hall-Findlay EJ. Vertical breast reduction. Semin Plast Surg. 2004;18:211–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sommer NZ, Zook EG, Verhulst SJ. The prediction of breast reduction weight. Plast Reconstr Surg. 2002;109:506–511. [DOI] [PubMed] [Google Scholar]
- 34.Kececi Y, Sir E. Prediction of resection weight in reduction mammaplasty based on anthropometric measurements. Breast Care (Basel). 2014;9:41–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cruz-Korchin N, Korchin L. Vertical versus wise pattern breast reduction: patient satisfaction, revision rates, and complications. Plast Reconstr Surg. 2003;112:1573–8; discussion 1579. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.