Abstract
Purpose:
To explore whether school poverty level and funding modified the effectiveness of an evidence-based Comprehensive School Physical Activity Program called Health Empowers You! implemented in elementary schools in Georgia.
Design:
Secondary data analysis of a multi-level, cluster-randomized controlled trial.
Setting:
40 elementary schools in Georgia in 2018–2019.
Subjects:
4th grade students in Georgia.
Measures:
Intervention schools implemented the Health Empowers You! program to increase school-day physical activity. The outcome was average daily moderate-to-vigorous physical activity, school free-reduced price lunch (FRPL) percentage and per pupil expenditures were effect modifiers.
Analysis:
Separate linear mixed regression models estimated the effect of the intervention on average daily moderate-to-vigorous physical activity, with interaction terms between intervention status and (1) school FRPL percentage or (2) per pupil expenditures.
Results:
The effect of the intervention was significantly higher in schools with higher FRPL percentage (intervention*school % FRPL β (95% CI): .06 (.01, .12)), and was modestly, but not statistically significantly, higher in schools with lower per pupil expenditures.
Conclusion:
Findings support the use of the Health Empowers You! intervention, which was effective in lower income schools, and may potentially reduce disparities in students’ physical activity levels.
Keywords: school-based health interventions, physical activity
Purpose
The World Health Organization 2020 guidelines on physical activity (PA) and sedentary behavior recommend that children should engage in 60 minutes per day of moderate-to-vigorous PA (MVPA), and reduce sedentary behavior.1 Regular PA has important health benefits for children, and evidence suggests that PA in youth may track into adulthood, highlighting its importance in childhood.2,3 Most children in the U.S. do not meet the current recommendations, and increasing the proportion of children who do engage in enough PA is a Healthy People 2030 objective.4 Furthermore, there are known disparities in youth PA levels by race/ethnicity and socioeconomic status.5,6
School-based PA offers a way to increase PA and reduce disparities, as most children spend several hours a day in school.7 The Community Preventive Services Task Force (CPSTF) recommends classroom-based physical activity break interventions as a way to increase physical activity among school-aged children, and the Centers for Disease Control and Prevention encourages schools to have a comprehensive school physical activity program (CSPAP), which includes components to successfully implement PE and PA during and after school.8–10
Despite recommendations to offer school based PA, limited resources in the physical environment, and financial, material, and staff resources have been reported to influence the adoption, implementation, and sustainability of school-based health interventions.11 In the United States, school resources are often tied to school poverty levels, therefore schools with less funding and fewer resources may experience barriers to adopting evidence-based interventions, and be more likely to serve populations who are already less likely to be able to engage in PA.12 For example, Non-Hispanic Black and Hispanic students are more likely to attend schools with higher concentrations of poverty, and fewer opportunities to engage in PA.13 Although studies suggest that school-based PA increases student PA and decreases sedentary behavior, most studies of school-based PA programs do not report differences in results by measures of health equity.8,14 Therefore it is not clear if all schools and students benefit from interventions equally.
The Health Empowers You! program is an evidence-based physical activity intervention that uses a CSPAP approach that has been shown to increase PA opportunities in schools (eg, increase minutes of classroom based exercised) and increase PA levels of elementary school students in Georgia.15–17 However, differences in its effectiveness across student or school characteristics have not been explored. If a CSPAP approach is less effective in low-income schools, scaling up could widen PA disparities. Therefore, this study’s objective was to determine if school poverty level and funding modified the effectiveness of an evidence-based physical activity intervention implemented in elementary schools in Georgia.
Methods
Design
Secondary data analysis of multi-level, cluster randomized control trial.
Sample
Data are from a multi-level, cluster-randomized controlled trial of 40 elementary schools in the Gwinnett County Public Schools system in Georgia (NIH trial registration ID NCT03765047). The trial followed students from 4th through 5th grade over an 18-month intervention period. The study implemented the evidence-based Health Empowers You! program, an intervention designed using a CSPAP approach, aimed at increasing school-day physical activity.10,16 Twenty schools were randomized to receive the Health Empowers You! intervention, and 20 schools were randomized to be control schools. The intervention was implemented during the 2018–2019 school year and fall 2019. The originally scheduled spring 2020 data collection was not completed due to the COVID-19 pandemic and school transition to remote learning. Both the school district and institutional IRB approved the study. Additional study details have been previously published.18,19
Measures
Potential effect modifiers of the intervention were: (1) schools’ percentage of students eligible for free or reduced-price lunch (FRPL), and (2) percentile of per pupil expenditures (PPE) with respect to all Georgia schools. School FRPL percentage was obtained from the school district, and PPE from the Georgia Department of Education (GA DOE). PPE is determined by GA DOE based on an analysis of how federal and state funds are spent by local school systems.
In final models, school FRPL percentage and PPE percentile were modeled continuously. Accelerometer data were used to objectively measure metabolic equivalents (METs), which were used to categorize moderate and vigorous PA (>3 METs). Protocols for accelerometer use have been previously published, but briefly, students wore an ActiGraphwGT3X-BT accelerometer (ActiGraph, Pensacola, FL) for 1 week (5 consecutive school days), at 2 time points (fall/spring) during each of the 2 intervention years.18
Analysis
A single measure of mean daily MVPA minutes was calculated in each semester for students who met a 3-day wear criteria. Average daily minutes of MVPA were calculated for fall and spring of 4th grade (fall 2018 and spring 2019). Only data from the first academic year of the study was analyzed to avoid the effects of summer vacation on students’ PA and maximize exposure to the school setting and intervention. Of the 4936 students enrolled in the study, 4121 (83%) students had complete data on fall and spring MVPA. Missing MVPA data (n = 815) were imputed using multilevel multiple imputation models that included student and school-level demographic characteristics, PA, school-level PA environments, and student academic outcomes.18,20 Twenty imputed datasets were created using the multilevel imputation program Blimp, and results were pooled across the 20 imputed datasets.
Descriptive statistics of students’ and schools’ characteristics were calculated on the complete case data (ie, non-imputed). Linear mixed regression models were used to estimate the effect of the intervention on average daily MVPA. Two-level random intercept models were used to account for school-level clustering of students. Separate models were used for each of the effect modifiers. The outcome variable in our models was spring MVPA with adjustment for fall MVPA. Models examined the effect of the intervention on MVPA, with an interaction term between intervention status and each effect modifier, and adjusted for student sex (male or female). One example model is shown below. All analyses were conducted in R version 4.1.2.
Results
Among the 4121 students with complete data for fall and spring MVPA, 2146 (52%) were in schools assigned to the intervention, and 1975 (48%) were in schools assigned to be control schools (Table 1). Among the intervention group, 22% of students were Black, 30% were Hispanic, 31% were White, and 47% received free or reduced-price lunch. Among the control group, 26% of students were Black, 36% were Hispanic, 21% were White, and 59% were eligible for FRPL. Students in the intervention group spent an average of 23 and 24 minutes/day in MVPA in the fall and spring semesters respectively. Students in the control group spent on average 20 minutes/day in MVPA in both fall and spring. Results from the main analysis of this trial found that the intervention statistically significantly increased MVPA among intervention schools and has been previously published.19 Among the 20 intervention schools, average school FRPL percentage was 51%, and schools were, on average, in the 34th percentile of per pupil expenditures. This was similar between intervention and control schools.
Table 1.
Student and School Characteristics, 4th Graders Enrolled in 40 Schools in Gwinnett County, GA, 2018 – 2019 (n = 4121).a
| Intervention Schoolsb |
Control Schools |
|||
|---|---|---|---|---|
| (n = 2146) |
(n = 1975) |
|||
| Student Characteristics | n | % | n | % |
|
| ||||
| Male | 1063 | 52.1 | 969 | 49.1 |
| Race/ethnicity | ||||
| Asian | 269 | 12.5 | 258 | 13.1 |
| Black | 480 | 22.4 | 504 | 25.5 |
| Hispanic | 639 | 29.8 | 718 | 36.4 |
| Mixed race | 103 | 4.8 | 91 | 4.6 |
| White | 655 | 30.5 | 404 | 20.5 |
| Received free/reduced price lunch | 997 | 46.5 | 1166 | 59.0 |
| Average daily MVPA min (mean, SD)c | ||||
| Fall 2018d | 22.6 | 9.8 | 19.7 | 8.6 |
| Spring 2019e | 24.0 | 10.9 | 19.8 | 9.3 |
|
| ||||
| (n = 20) |
(n = 20) |
|||
| School Characteristics | Mean | SD | Mean | SD |
|
| ||||
| % Male | 51.9 | 3.3 | 50.9 | 5.0 |
| Race/ethnicityf | ||||
| % Asian | 11.9 | 7.5 | 11.2 | 9.1 |
| % Black | 24.9 | 11.1 | 31.0 | 12.4 |
| % Hispanic | 29.4 | 21.4 | 34.9 | 18.2 |
| % Mixed race | 4.5 | 1.6 | 4.3 | 2.0 |
| % White | 29.0 | 19.7 | 18.4 | 15.8 |
| % receiving free/reduced price lunch (FRPL) | 51.0 | 28.2 | 61.1 | 24.7 |
| Avg. percentile of per pupil expendituresg | 34.2 | 16.1 | 36.6 | 19.5 |
Sample with complete data on demographic characteristics and fall and spring MVPA.
Health Empowers You! intervention.
MVPA = moderate-to-vigorous physical activity.
n = 359 missing.
n = 636 missing.
Not mutually exclusive.
Percentile relative to other schools in GA.
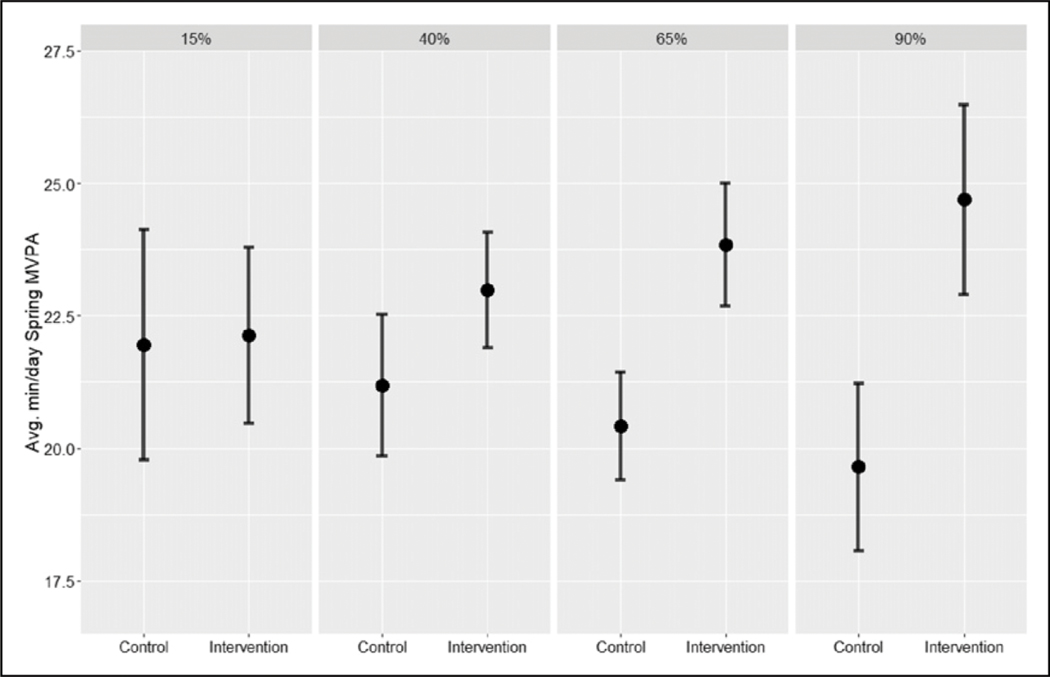
The effect of the intervention significantly differed by school FRPL percentage, wherein the intervention effect was larger as schools’ percentage of FRPL eligible students increased, (βinterv*sch%FRPL = .06; 95% CI = .01, .12) (Table 2). Among schools with 15% FRPL eligibility, students in intervention schools had almost no difference in average daily MVPA compared to those in control schools, while in schools with 80% FRPL eligibility, there was more than a 4-minute difference in average daily MVPA between students in control and intervention schools (Figure 1). PPE was not a statistically significant effect modifier, however examination of interaction plots indicated modest differences by PPE. The intervention had the greatest effect on increased MVPA in schools with lower percentile of per pupil expenditures (data not shown).
Table 2.
Linear Mixed Models of the Effect of the Health Empowers You! Intervention and Average Daily Minutes of MVPAa, With Interaction by School Characteristics, 4th Graders Enrolled in 40 Schools in Gwinnett County, GA, 2018 – 2019 (n = 4936).b, c
| Intervention |
School Characteristic |
Intervention*School Characteristic |
|
|---|---|---|---|
| School Characteristic | β (95% CI) | β (95% CI) | β (95% CI) |
|
| |||
| School % FRPLd | −.80 (−4.28, 2.68) | −.03 (−.07, .01) | .06 (.01, .12) |
| Percentile of per pupil expenditures | 3.92 (.56, 7.27) | .02 (−.03, .08) | −.03 (−.12, .06) |
Spring MVPA adjusted for fall MVPA.
Adjusted for student sex.
Imputed dataset (n = 4936).
FRPL = free- or -reduce-price lunch eligible.
Bold = statistically significant (P < .05).
Figure 1.
Plot of average min/day of MVPAa by Health Empowers You! intervention status and school percentage of free/reduced price lunch eligibility, 4th graders enrolled in 40 schools across Gwinnett County, GA, 2018 – 2019.b
aSpring MVPA, adjusted for fall MVPA.
badjusted for student sex.
Discussion
Overall, these results support the effectiveness of the Health Empowers You! program, indicating the program led to small increases in MVPA, and appeared to have a larger effect among schools with a higher percentage of students eligible for FRPL. Although effect sizes for changes in MVPA were small, they were similar to results from other studies that have implemented CSPAPs and may have meaningful effects at a population level. These results are promising from a health equity perspective, as they suggest that this approach can help decrease the gap in PA levels seen by SES, as well as increase PA among students in general.
The greater intervention effectiveness in lower-income schools could possibly reflect that the students in these schools began with fewer minutes of MVPA on average (see Figure 1). Lower-income schools may have more room to improve, while interventions in higher income schools may be subject to ceiling effects, wherein there may be less room for change because of an already established awareness and ability to improve PA.21
However, school-based PA has been shown to increase student MVPA,22 though a Cochrane Review of school-based PA programs noted that most studies do not tend to report any differences in aspects related to implementation of interventions, such as uptake or adherence, or health equity.14 Recent studies suggest that inadequate facilities and limited resources have been identified as barriers to implementation of PA interventions.23,24 The Health Empowers You! program incorporates all 5 components of the CSPAP model which may make it particularly effective at increasing students’ PA.16 The results suggest that the intervention materials, training, and technical assistance provided to schools and teachers are helpful for increasing PA and that there may be an additional benefit in lower-resource settings. Low-income schools tend to be in lower income neighborhoods, and because most schools are funded from property taxes, these schools often receive less funding.25 Schools with fewer resources and funding may benefit more than others from these supports as the intervention could help address the greater barriers to increasing PA in those schools.13
The focus on equity in schools and PA is important to consider because data suggest that school closures led to reductions in physical activity, BMI increases during the pandemic, particularly among elementary school aged children, and that preexisting disparities in childhood obesity may have widened.26,27 School closures also highlighted disparities in academic achievement, as well as access to healthy food, financial resources, and safe neighborhoods, emphasizing the important role schools can play in shaping childhood health and reducing disparities.28 Furthermore, because PA can help with students’ academic achievement, school PA may offers dual benefits to schools.29
At least 4 limitations of this study should be mentioned. First, the extrapolation of 3–5 days of accelerometer data to a full semester of activity levels may have been less accurate than a longer accelerometer measurement period.30 However, even though at least 4 days of wear time is typically recommended for reliable PA estimates in children, school-day PA is less variable than full-day data, therefore 3 days of wear time in the school context may be valid for school-day PA.30,31 Second, PA was only measured during the school day, therefore we were unable to evaluate the contribution of the intervention to total PA. Third, because the study was shortened due to COVID-19 school closures, longer term effects of school characteristics on MVPA could not be assessed. Finally, a measure of school-day MVPA was not available prior to the start of the intervention so assess baseline levels of PA.
Additional studies in other school districts are warranted to investigate this relationship across different populations and school environments. Future work should also explore what, if any, role school poverty level and funding play in the implementation and adherence to school-based interventions.
SO WHAT?
What is already known about this topic?
Most children do not meet physical activity recommendations. School-based physical activity interventions are an effective way to increase youth physical activity.
What does this article add?
This is one of few studies that examines whether the effectiveness of a school-based PA intervention differs by school free-reduced price lunch (FRPL) percentage, a proxy for schools serving more low-income students.
What are the implications for health promotion practice or research?
This study supports the use of a Comprehensive School Physical Activity Program for increasing physical activity in schools, and particularly in schools with more low-income students who may be less likely to have opportunities to engage in PA.
Acknowledgments
The authors would also like to acknowledge the participating school district and the HealthMPowers staff. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was provided by the Robert Wood Johnson Foundation (ID: 74281), the Ardmore Institute of Health, and the National Heart, Lung, and Blood Institute (Grant No. 1F31HL156426-01A1).
Footnotes
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Washington, DC: Department of Health and Human Services; 2018. [Google Scholar]
- 3.Souilla L, Larsen AC, Juhl CB, Skou ST, Bricca A. Childhood and adolescence physical activity and multimorbidity later in life: a systematic review. J Multimorb Comorb. 2024;14: 26335565241231403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Services UDoHaH. https://health.gov/healthypeople/objectives-and-data/browse-objectives/physical-activity/increase-proportion-children-who-do-enough-aerobic-physical-activity-pa-09 [Google Scholar]
- 5.Armstrong S, Wong CA, Perrin E, Page S, Sibley L, Skinner A. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: findings from the National Health and Nutrition Examination Survey, 2007–2016. JAMA Pediatr. 2018;172(8):732–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gautam N, Dessie G, Rahman MM, Khanam R. Socioeconomic status and health behavior in children and adolescents: a systematic literature review. Front Public Health. 2023;11:1228632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.School health guidelines to promote healthy eating and physical activity. MMWR Recommendations and Reports: MMWR Recomm Rep (Morb Mortal Wkly Rep). 2011;60(RR-5):1–76. [PubMed] [Google Scholar]
- 8.Masini A, Marini S, Gori D, Leoni E, Rochira A, Dallolio L. Evaluation of school-based interventions of active breaks in primary schools: a systematic review and meta-analysis. J Sci Med Sport. 2020;23(4):377–384. [DOI] [PubMed] [Google Scholar]
- 9.Guide to Community Preventive Services. Physical Activity: Classroom-based Physical Activity Break Interventions. Physical Activity: Classroom-Based Physical Activity Break Interventions. https://www.thecommunityguide.org/findings/physical-activity-classroom-based-physical-activity-break-interventions.html (2021). [Google Scholar]
- 10.Comprehensive School Physical Activity Programs: A Guide for Schools. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 11.Fair KN, Solari Williams KD, Warren J, McKyer ELJ, Ory MG. The influence of organizational culture on school-based obesity prevention interventions: a systematic review of the literature. J Sch Health. 2018;88(6):462–473. [DOI] [PubMed] [Google Scholar]
- 12.Saporito S, Sohoni D. Mapping educational inequality: concentrations of poverty among poor and minority students in public schools. Soc Forces. 2007;85(3):1227–1253. [Google Scholar]
- 13.Van Dyke ME, Cheung PC, Franks P, Gazmararian JA. Socioeconomic and racial/ethnic disparities in physical activity environments in Georgia elementary schools. Am J Health Promot. 2018;32(2):453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neil-Sztramko SE, Caldwell H, Dobbins M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2021;2013(2):CD007651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braun HA, Kay CM, Cheung P, Weiss PS, Gazmararian JA. Impact of an elementary school-based intervention on physical activity time and aerobic capacity, Georgia, 2013–2014. Publ Health Rep. 2017;132(2_suppl):24S–32s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyde ET, Gazmararian JA, Barrett-Williams SL, Kay CM. Health Empowers You: impact of a school-based physical activity program in elementary school students, Georgia, 2015–2016. J Sch Health. 2020;90(1):32–38. [DOI] [PubMed] [Google Scholar]
- 17.Cheung P, Franks P, Kramer M, et al. Impact of a Georgia elementary school-based intervention on physical activity opportunities: a quasi-experimental study. J Sci Med Sport. 2019; 22(2):191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boedeker P, Turner L, Calvert H, et al. Study protocol for testing the association between physical activity and academic outcomes utilizing a cluster-randomized trial. Contemp Clin Trials Commun. 2021;21:100747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elish PN, Bryan CS, Boedeker PJ, et al. The longitudinal association between objectively-measured school-day physical activity and academic achievement in US elementary school students. Int J Behav Nutr Phys Activ. 2022;19(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Enders CK, Keller BT, Levy R. A fully conditional specification approach to multilevel imputation of categorical and continuous variables. Psychol Methods. 2018;23(2):298–317. [DOI] [PubMed] [Google Scholar]
- 21.Kumanyika SK, Yancey AK. Physical activity and health equity: evolving the science. Am J Health Promot. 2009;23(6_suppl):S4–S7. [DOI] [PubMed] [Google Scholar]
- 22.Carrasco-Uribarren A, Ortega-Mart´ınez A, Amor-Barbosa M, Cadellans-Arróniz A, Cabanillas-Barea S, Bagur-Calafat MC. Improvement of in-school physical activity with active school-based interventions to interrupt prolonged sitting: a systematic review and meta-analysis. Int J Environ Res Publ Health. 2023; 20(2):1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hanna L, Burns C, O’Neill C, Coughlan E. A systematic review of the implementation and effectiveness of ‘the daily mile’ on markers of children’s health. Int J Environ Res Publ Health. 2023;20(13):6203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig DW, Walker TJ, Cuccaro P, et al. Using the R = MC(2) heuristic to understand barriers to and facilitators of implementing school-based physical activity opportunities: a qualitative study. BMC Publ Health. 2024;24(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Owens A Unequal opportunity: school and neighborhood segregation in the USA. Race Soc Probl. 2020;12(1):29–41. [Google Scholar]
- 26.Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021; 147(5):e2021050123. [DOI] [PubMed] [Google Scholar]
- 27.Camp-Spivey LJ, Newman SD, Stevens RN, Nichols M. “We’ve had to build the plane as we flew It”: impacts of the COVID-19 pandemic on school-based weight management interventions. Child Obes. 2021;17(8):497. [DOI] [PubMed] [Google Scholar]
- 28.Health TLP. Childhood obesity beyond COVID-19. Lancet Public Health. 2021;6(8):e534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barbosa A, Whiting S, Simmonds P, Scotini Moreno R, Mendes R, Breda J. Physical activity and academic achievement: an umbrella review. Int J Environ Res Publ Health. 2020;17(16): 5972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fairclough SJ, Butcher ZH, Stratton G. Whole-day and segmented-day physical activity variability of northwest England school children. Prev Med. 2007;44(5):421–425. [DOI] [PubMed] [Google Scholar]
- 31.Barreira TV, Schuna JM, Tudor-Locke C, et al. Reliability of accelerometer-determined physical activity and sedentary behavior in school-aged children: a 12-country study. Int J Obes Suppl. 2015;5(Suppl 2):S29–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]