Abstract
Elaborating and understanding disparities in the burden of cardiovascular disease attributable to high fasting plasma glucose is important to improve diabetes prevention and promote cardiovascular health. In this study, we pool data on 791,373 people aged 25 years and older from three population-based surveys, and estimate the burden of cardiovascular disease attributable to high fasting plasma glucose between 2010 and 2018 in China by age, sex, region and socio-demographic index. In 2018, an estimated total of 498.61 thousand (95% uncertainty interval 463.93 to 534.12) cardiovascular disease-related deaths are attributable to high fasting plasma glucose in China. High fasting plasma glucose accounts for 1076.09 years of life lost per 100,000 people (95% uncertainty interval 1026.88–1129.04) due to cardiovascular disease in 2018, with substantial variation across provinces. In 2018, the higher age-standardised cardiovascular disease mortality rate attributable to high fasting plasma glucose is observed in the high-middle socio-demographic index region and the middle socio-demographic index region. Nationally, compared to 2010, exposure to high fasting plasma glucose and population aging in 2018 are the primary drivers of increased fasting plasma glucose-related deaths due to cardiovascular disease. Findings of this study emphasize the importance of developing population-specific tailored measures in China and other regions with similar condition.
Subject terms: Epidemiology, Risk factors, Cardiology
Evidence for comprehensive assessment of cardiovascular disease (CVD) burden attributable to high fasting plasma glucose (FPG) in China is limited. Here, the authors show CVD deaths attributable to high FPG varied substantially across China. Exposure to high FPG and population aging were the primary drivers of increased CVD burden.
Introduction
Cardiovascular disease (CVD), with its increasing morbidity and mortality, has become a major threat to the global public health. According to the Global Burden of Disease (GBD) 2019, there was nearly 4.58 million individuals died from CVD in China in 2019, accounting for approximately 43% of all deaths1. Diabetes mellitus has been identified as one of the four main non-communicable disease by China and World Health Organization, and it has shown a continuing increase in prevalence over the past three decades in countries of all income levels2. In 2017, the weighted prevalence of diabetes was 11.2% in China using the WHO criteria, affecting about 129.8 million individuals nationally3. Additionally, previous researches indicated that China has a large population with prediabetes3,4, which represents a large reservoir of individuals at risk of diabetes.
Regarding that high fasting plasma glucose (FPG), defined as a FPG greater than or equal to 4.8–5.4 mmol/L5,6, is increasingly recognised as one of the leading risk factors contributing to the increase in the burden of CVD-related deaths, priority setting for clinical and public health implications requires more information on the CVD burden attributable to high FPG. Also, GBD 2019 estimated that there were 1.07 million deaths were attributed to high FPG in mainland China, and high FPG accounted for 17.5% of the 4 million deaths from CVD5. Moreover, GBD 2015 analysis demonstrated that hyperglycaemia produced a substantial and ever-increasing CVD burden in the Brazil7. Also, a recent study revealed that the burden of diabetes and hyperglycaemia in adults in the Americans has been markedly increasing and expanding8. However, evidence for comprehensive and detailed analyses of the CVD burden attributable to high FPG in other regions, especially in developing countries such as China, is limited. Furthermore, CVD burden caused by high FPG may be further intensified by the population aging, shifts in lifestyle factors, nutrition transition, low physical activity and epidemic of over-weight and obesity. However, previous research did not capture information on the effect of demographic and epidemiologic shift on CVD burden attributable to high FPG in China.
As such, in this study, we aimed to systematically describe the CVD burden attributable to high FPG across China from 2010 to 2018, and reported the decomposes changes in attributable burden into population growth, population aging, risk exposure to FPG, and risk-deleted mortality rates due to CVD. The findings of this study emphasize the importance of developing population-specific tailored measures for diabetes prevention and cardiovascular health promotion in China and other countries or regions with similar condition.
Results
Exposure to FPG levels
Between 2010 and 2018, the overall age-standardised FPG level among adults aged 25 years or older increased from 5.7 mmol/L (95%UI 5.0–6.4) to 5.9 mmol/L (95%UI 5.3–6.5) for men, and from 5.6 mmol/L (95%UI 5.0–6.2) to 5.8 mmol/L (95%UI 5.2–6.4) for women. For most provinces, the age-standardised mean FPG level for both men and women increased from 2010 to 2018 (Supplementary Data 1 and Supplementary Fig S1).
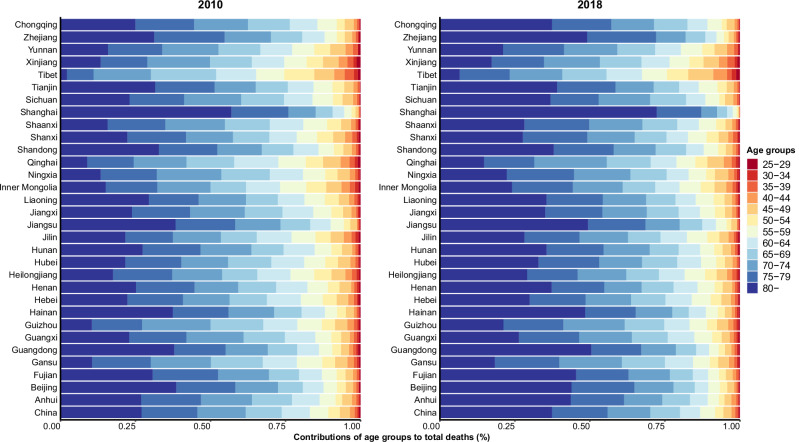
National burden
Nationally, in 2018, the estimated number of CVD-related deaths attributable to high FPG were 498.61 thousand (95%UI 463.93–534.12), with 278.43 thousand (95%UI 257.99–300.08) of these deaths occurring in men and 220.59 thousand (95%UI 194.21–250.18) in women (Table 1, Supplementary Tables S6–S7). The age-standardised CVD mortality rate attributable to high FPG increased by 4.30%, from 40.80 per 100,000 people (95%UI 38.02–43.77) in 2010 to 42.56 per 100,000 (95%UI 39.86–45.33) in 2018, with an EAPC of −0.33 (95%UI −5.33–4.93) (Table 2). Besides, age-specific CVD mortality rates attributable to high FPG increased with increasing age, and this pattern was similar for both men and women (Table 1, Supplementary Tables S6-S7). Compared to 2010, the mortality rates and years of life lost (YLL) rates for CVD attributable to high FPG in 2018 had substantially increased among people ≥80 years, with CVD mortality rates increasing from 481.71 per 100,000 people (95%UI 374.42–596.57) in 2010 to 618.95 per 100,000 people (95%UI 510.53–730.89) in 2018 (Table 1). Moreover, we observed that the gap in CVD mortality attributable to high FPG between men and women had narrowed after the age of 50 in 2018, and even among those over 80, women have higher CVD mortality rate than men (Supplementary Tables S6–S7, and Supplementary Fig S2). In 2010 and 2018, the YLL rates for CVD attributable to high FPG were 907.65 per 100,000 people (95%UI 864.21–949.63) and 1076.09 per 100,000 people (95%UI 1026.88–1129.04), respectively (Table 1). Additionally, the age composition of CVD mortality caused by high FPG suggested a trend toward older ages from 2010 to 2018 (Fig. 1). Compared with men, women had a higher proportion of individuals aged 80 years and older who died of CVD attributable to high FPG in 2010 and 2018, with elderly individuals (≥80 years old) accounting for 38.41% in 2010 and 50.04% in 2018 of CVD deaths attributable to high FPG (Supplementary Figs S3–S4).
Table 1.
Deaths and YLLs for total CVD attributable to high FPG by age in China, 2010–2018 (95%UI)
| 2010 | 2018 | |||||||
|---|---|---|---|---|---|---|---|---|
| Deaths (thousands) | Mortality rate per 100,000 | YLL (thousands) | YLL rate per 100,000 | Deaths (thousands) | Mortality rate per 100,000 | YLL (thousands) | YLL rate per 100,000 | |
| 25–29 | 1.68 (1.33–2.09) | 1.53 (1.21–1.90) | 106.22.1 (84.07–131.93) | 96.7 4 (76.56–120.16) | 1.80 (1.46–2.21) | 1.68 (1.37–2.07) | 113.51 (92.50–139.52) | 106.34 (86.66–130.71) |
| 30–34 | 1.91 (1.54–2.36) | 1.95 (1.57–2.41) | 111.45 (89.47–137.40) | 113.76 (91.32–140.24) | 2.00 (1.66–2.36) | 2.26 (1.88–2.67) | 116.30 (96.47–137.34) | 131.73 (109.27–155.56) |
| 35–39 | 3.36 (2.84–3.91) | 3.11 (2.63–3.62) | 178.86 (151.36–208.50) | 165.58 (140.12–193.03) | 3.98 (3.44–4.54) | 3.76 (3.25–4.29) | 212.21 (183.52–242.03) | 200.15 (173.09–228.28) |
| 40–44 | 5.45 (4.67–6.34) | 5.06 (4.35–5.90) | 263.38 (225.98–306.73) | 244.97 (210.19–285.29) | 6.26 (5.46–7.16) | 5.29 (4.61–6.05) | 302.68 (263.97–346.22) | 255.86 (223.13–292.66) |
| 45–49 | 12.07 (10.63–13.67) | 10.18 (8.97–11.53) | 524.93 (462.45–594.61) | 442.85 (390.14–501.64) | 13.40 (12.05–\14.83) | 10.28 (9.24–11.38) | 582.95 (524.04–645.26) | 447.32 (402.11–495.13) |
| 50–54 | 13.42 (11.91–14.90) | 18.02 (15.99–20.01) | 519.37 (460.77–576.56) | 697.48 (618.79–774.29) | 13.80 (12.52–15.14) | 17.50 (15.88–19.19) | 534.17 (484.72–585.93) | 677.15 (614.46–742.76) |
| 55–59 | 21.75 (19.64–24.14) | 29.25 (26.41–32.46) | 739.14 (667.37–820.19) | 993.94 (897.43–1102.92) | 24.90 (22.85–27.25) | 28.46 (26.11–31.14) | 846.32 (776.43–925.91) | 967.19 (887.32–1058.15) |
| 60–64 | 33.18 (29.87–36.61) | 55.85 (50.28–61.61) | 972.76 (875.67–1073.12) | 1637.31 (1473.89–1806.23) | 33.49 (30.77–36.31) | 50.22 (46.15–54.45) | 981.67 (902.03–1064.32) | 1472.34 (1352.89–1596.29) |
| 65–69 | 42.10 (37.86–46.42) | 102.57 (92.23–113.09) | 1041.39 (936.49–1148.22) | 2536.93 (2281.38–2797.17) | 49.61 (45.02–53.93) | 92.29 (83.76–100.33) | 1227.03 (1113.64–1333.99) | 2282.64 (2071.69–2481.60) |
| 70–74 | 56.79 (51.76–62.72) | 183.77 (167.48–202.93) | 1154.13 (1051.86–1274.48) | 3734.35 (3403.45–4123.76) | 71.01 (65.26–77.63) | 172.06 (158.12–188.09) | 1443.01 (1326.07–1577.45) | 3496.48 (3213.13–3822.22) |
| 75–79 | 65.66 (59.03–73.19) | 287.69 (258.64–320.72) | 1056.69 (950.00–1177.99) | 4630.28 (4162.74–5161.78) | 92.53 (84.27–101.07) | 283.80 (258.47–310.02) | 1489.15 (1356.26–1626.71) | 4567.62 (4160.00–4989.54) |
| ≥80 | 95.24 (74.03–117.95) | 481.71 (374.42–596.57) | 1160.09 (901.72–1436.73) | 5867.62 (4560.82–7266.82) | 186.39 (153.75–220.11) | 618.95 (510.53–730.89) | 2270.46 (1872.76–2681.10) | 7539.35 (6218.73–8902.94) |
| All ages | 352.80 (328.69–378.44) | 40.80 (38.02–43.77) | 7847.76 (7472.13–8210.73) | 907.65 (864.21–949.63) | 498.61 (463.93–534.12) | 53.02 (49.33–56.79) | 10120.38 (9657.55–10618.35) | 1076.09 (1026.88–1129.04) |
YLLs years of life lost, CVD cardiovascular disease, FPG fasting plasma glucose, 95% UI 95% uncertainty intervals.
Table 2.
Total deaths and age-standardised mortality rates due to CVD attributable to high FPG, percentage change, and EAPC by province in China, 2010–2018
| All-age deaths, No. in thousands (95% UI) | Age-standardised mortality rate (95% UI), per 100,000 | ||||||
|---|---|---|---|---|---|---|---|
| 2010 | 2018 | Change, % | 2010 | 2018 | Change,% | EAPC (95%UI) | |
| China | 352.80 (328.69–378.44) | 498.61 (463.93–534.12) | 41.33 | 40.80 (38.02–43.77) | 42.56 (39.86–45.33) | 4.30 | −0.33 (−5.33–4.93) |
| Anhui | 16.54 (12.14–22.08) | 26.63 (18.35–36.33) | 61.02 | 39.15 (28.64–52.48) | 46.46 (33.97–60.62) | 18.66 | 0.94 (−4.93–7.18) |
| Beijing | 5.77 (4.18–7.83) | 7.91 (5.81–10.93) | 37.14 | 48.84 (35.13–66.44) | 42.64 (32.09–57.53) | −12.71 | −2.56 (−5.43–0.41) |
| Fujian | 6.64 (4.53–9.50) | 9.38 (6.65–12.89) | 41.18 | 30.45 (21.44–41.99) | 33.04 (24.50–43.46) | 8.50 | −0.64 (−5.94–4.97) |
| Gansu | 4.94 (3.78–6.26) | 6.77 (5.28–8.62) | 37.06 | 32.51 (24.25–44.44) | 37.25 (27.73–49.02) | 14.58 | 0.46 (−5.69–7.01) |
| Guangdong | 20.29 (13.80–28.36) | 31.65 (20.73–45.92) | 56.00 | 39.34 (27.72–53.64) | 40.22 (28.58–55.72) | 2.25 | −0.11 (−5.58–5.67) |
| Guangxi | 11.86 (8.86–15.88) | 13.74 (10.47–17.70) | 15.81 | 37.39 (28.32–49.07) | 38.26 (30.24–47.96) | 2.34 | −0.06 (−4.43–4.51) |
| Guizhou | 7.03 (5.32–9.13) | 7.55 (5.56–10.11) | 7.33 | 30.64 (23.11–40.06) | 28.85 (21.36–38.35) | −5.85 | −1.78 (−7.92–4.78) |
| Hainan | 2.45 (1.70–3.43) | 3.61 (2.65–4.82) | 47.16 | 46.18 (33.45–62.88) | 54.68 (41.70–70.40) | 18.41 | 0.67 (−5.50–7.25) |
| Hebei | 23.54 (18.87–29.99) | 34.52 (26.52–44.00) | 46.64 | 52.51 (41.48–67.44) | 55.54 (43.53–69.60) | 5.78 | −0.33 (−5.17–4.77) |
| Henan | 31.20 (22.86–43.47) | 44.64 (32.03–58.94) | 43.08 | 52.51 (38.64–72.70) | 61.51 (45.47–79.50) | 17.15 | 0.72 (−4.30–5.99) |
| Heilongjiang | 16.80 (13.21–21.16) | 24.84 (19.85–30.77) | 47.79 | 70.34 (53.97–92.36) | 75.18 (59.99–93.66) | 6.88 | 0.20 (−5.23–5.95) |
| Hubei | 14.17 (10.57–18.89) | 17.46 (12.35–23.86) | 23.17 | 37.89 (27.72–51.76) | 34.30 (24.59–46.57) | −9.47 | −2.05 (−7.05–3.22) |
| Hunan | 14.63 (9.87–19.75) | 19.90 (14.95–26.77) | 36.06 | 32.22 (21.87–43.47) | 32.45 (25.06–42.47) | 0.72 | −0.77 (−6.06–4.80) |
| Jilin | 11.25 (8.90–14.33) | 14.92 (11.78–19.41) | 32.62 | 63.69 (48.89–83.62) | 61.83 (48.80–80.14) | −2.91 | −0.80 (−5.76–4.43) |
| Jiangsu | 18.15 (12.39–25.76) | 26.05 (17.95–36.00) | 43.51 | 28.94 (20.33–40.13) | 31.12 (22.71–41.55) | 7.53 | −0.13 (−5.07–5.06) |
| Jiangxi | 7.96 (5.80–10.59) | 10.04 (7.41–13.50) | 26.10 | 31.43 (22.87–41.91) | 28.85 (21.78–37.87) | −8.23 | −2.04 (−7.34–3.56) |
| Liaoning | 20.92 (15.97–27.24) | 27.74 (20.52–36.99) | 32.58 | 63.11 (47.80–82.52) | 62.59 (47.66–81.70) | −0.83 | −0.83 (−5.65–4.23) |
| Inner Mongolia | 7.95 (6.29–9.85) | 9.87 (7.87–12.20) | 24.12 | 56.44 (43.02–73.09) | 52.68 (41.09–66.65) | −6.66 | −1.58 (−6.96–4.12) |
| Ningxia | 1.10 (0.85–1.44) | 1.54 (1.15–2.02) | 39.92 | 38.05 (27.92–52.75) | 38.55 (27.55–53.51) | 1.32 | −0.49 (−6.76–6.19) |
| Qinghai | 0.82 (0.64–1.04) | 1.38 (1.15–1.65) | 67.34 | 30.98 (23.48–41.56) | 40.96 (33.02–50.33) | 32.23 | 2.65 (−2.96–8.58) |
| Shandong | 33.53 (23.60–46.88) | 50.26 (35.98–69.01) | 49.88 | 47.85 (34.40–65.55) | 49.04 (37.17–64.10) | 2.50 | −0.02 (−4.94–5.16) |
| Shanxi | 9.15 (6.94–11.71) | 12.90 (9.88–17.01) | 41.07 | 46.37 (34.31–60.29) | 46.64 (35.67–61.32) | 0.58 | −0.27 (−5.91–5.72) |
| Shaanxi | 7.64 (5.52–10.68) | 11.33 (8.14–15.19) | 48.36 | 32.75 (22.63–47.87) | 38.47 (27.24–53.05) | 17.45 | 0.38 (−6.84–8.16) |
| Shanghai | 3.72 (2.12–5.97) | 9.07 (5.27–13.84) | 143.77 | 21.16 (12.99–32.32) | 27.07 (17.07–39.22) | 27.89 | 1.21 (−3.66–6.32) |
| Sichuan | 19.19 (14.36–25.86) | 27.81 (20.25–36.31) | 44.95 | 31.17 (23.39–41.74) | 34.39 (25.99–43.66) | 10.34 | 0.12 (−5.25–5.79) |
| Tianjin | 5.53 (4.24–7.30) | 7.08 (5.32–9.29) | 28.05 | 65.61 (50.12–86.73) | 56.12 (42.96–72.52) | −14.46 | −2.67 (−5.91–0.68) |
| Tibet | 0.27 (0.20–0.35) | 0.31 (0.22–0.42) | 14.21 | 22.02 (16.27–29.17) | 20.77 (14.76–28.63) | −5.65 | −1.50 (−7.26–4.60) |
| Xinjiang | 4.65 (3.69–5.72) | 5.71 (4.70–6.95) | 22.82 | 44.64 (34.77–56.55) | 44.54 (35.66–56.00) | −0.22 | −1.16 (−6.53–4.52) |
| Yunnan | 6.63 (4.94–8.86) | 7.96 (6.00–10.43) | 19.99 | 26.02 (19.35–35.00) | 25.01 (19.19–32.18) | −3.87 | −1.41 (−6.45–3.91) |
| Zhejiang | 8.03 (5.37–11.76) | 13.14 (8.85–18.45) | 63.56 | 20.73 (14.50–29.44) | 21.78 (15.63–29.26) | 5.11 | −1.37 (−7.48–5.15) |
| Chongqing | 6.60 (4.78–9.26) | 8.37 (6.03–11.13) | 26.85 | 29.10 (21.21–40.84) | 28.89 (21.35–37.76) | −0.72 | −1.31 (−6.79–4.50) |
CVD cardiovascular disease, FPG fasting plasma glucose, 95% UI 95% uncertainty intervals, EAPC estimated annual percentage change.
Fig. 1. The twelve age groups as percentages of total CVD deaths attributable to high FPG nationally and in 31 provinces in 2010 and 2018.
(CVD: cardiovascular disease; FPG: fasting plasma glucose). Source data are provided as a Source Data file.
For specific causes, ischaemic heart disease was the most important contributor to FPG-related CVD deaths (247.12 thousand [95%UI 224.01–272.48]) in 2018, followed by ischaemic stroke (135.83 thousand [95%UI 121.17–151.16]) and haemorrhagic stroke (115.36 thousand [95%UI 108.74–122.35]) (Table 3). However, we found that the number of haemorrhagic stroke-related deaths attributable to high FPG (103.29 [95%UI 96.91 to 109.75]) in 2010 was higher than that of ischaemic stroke-related deaths attributable to high FPG (83.72 [95%UI 75.23–93.19]) in 2010. Of note, for total CVD and its subtypes, men had a higher mortality burden than women in both 2010 and 2018 (Table 3). Moreover, in 2018, the estimated YLL rates for ischaemic heart disease, ischaemic stroke and haemorrhagic stroke caused by high FPG were 518.95 per 100,000 people (95%UI 487.43–552.79), 266.91 per 100,000 people (95%UI 246.78–289.30) and 288.95 per 100,000 people (95%UI 276.84–301.71) (Supplementary Table S8). Additionally, 13.26% (95%UI 12.34–14.20%) of total deaths attributable to high FPG were related to CVDs in 2018, among which 13.88% (95%UI 12.58–15.31%) were related to ischaemic heart disease, 12.26% (95%UI 10.94–13.65%) were related to ischaemic stroke, and 13.21% (95%UI 12.45–14.01%) were related to haemorrhagic stroke, respectively (Supplementary Tables S9–12).
Table 3.
Number, rate, and age-standardised rate for CVD deaths attributable to high FPG by specific causes and sex in China, 2010–2018 (95%UI)
| 2010 | 2018 | |||||
|---|---|---|---|---|---|---|
| Deaths (thousands) | Mortality rate per 100,000 | Age-standardised mortality rate (95% UI), per 100,000 | Deaths (thousands) | Mortality rate per100,000 | Age-standardised mortality rate (95% UI), per 100,000 | |
| CVD | ||||||
| Total | 352.80 (328.69–378.44) | 40.80 (38.02–43.77) | 40.80 (38.02–43.77) | 498.61 (463.93–534.12) | 53.02 (49.33–56.79) | 42.56 (39.86–45.33) |
| Male | 200.26 (186.05–216.35) | 45.81 (42.56–49.49) | 48.36 (44.68–52.58) | 278.43 (257.99–300.08) | 58.85 (54.53–63.43) | 51.13 (47.44–54.99) |
| Female | 152.62 (134.58–172.26) | 35.70 (31.48–40.30) | 32.98 (29.35–36.91) | 220.59 (194.21–250.18) | 47.20 (41.56–53.53) | 33.88 (30.40–37.79) |
| Ischaemic heart disease | ||||||
| Total | 166.12 (150.43–182.66) | 19.21 (17.40–21.13) | 19.21 (17.40–21.13) | 247.12 (224.01–272.48) | 26.28 (23.82–28.97) | 20.91 (19.15–22.82) |
| Male | 90.38 (82.31–99.93) | 20.68 (18.83–22.86) | 22.04 (19.83–24.55) | 132.18 (119.79–146.36) | 27.94 (25.32–30.94) | 24.36 (22.13–26.90) |
| Female | 75.04 (62.30–89.37) | 17.55 (14.57–20.91) | 16.03 (13.47–18.85) | 114.72 (96.34–137.48) | 24.55 (20.61–29.42) | 17.28 (14.83–20.27) |
| Ischaemic stroke | ||||||
| Total | 83.72(75.23–93.19) | 9.68(8.70–10.78) | 9.68 (8.70–10.78) | 135.83 (121.17–151.16) | 14.44 (12.88–16.07) | 11.34 (10.22–12.55) |
| Male | 46.92(41.91–52.51) | 10.73(9.59–12.01) | 11.45 (10.17–12.97) | 75.87 (67.46–85.73) | 16.04 (14.26–18.12) | 13.65 (12.13–15.41) |
| Female | 36.78(30.45–44.18) | 8.60(7.12–10.33) | 7.92 (6.66–9.40) | 59.92 (49.42–71.36) | 12.82 (10.57–15.27) | 9.08 (7.66–10.61) |
| Haemorrhagic stroke | ||||||
| Total | 103.29(96.91–109.75) | 11.95(11.21–12.69) | 11.95(11.21–12.69) | 115.36(108.74–122.35) | 12.27 (11.56–13.01) | 10.26 (9.74–10.83) |
| Male | 62.87(58.20–67.50) | 14.38(13.31–15.44) | 14.91(13.78–16.05) | 70.06(65.57–74.99) | 14.81 (13.86–15.85) | 13.06 (12.25–13.95) |
| Female | 40.26(36.12–45.40) | 9.42(8.45–10.62) | 8.94(8.10–9.98) | 45.18(40.68–50.21) | 9.67 (8.70–10.74) | 7.46 (6.83–8.14) |
CVD cardiovascular disease, FPG fasting plasma glucose, 95% UI 95% uncertainty intervals.
Regional and provincial burden
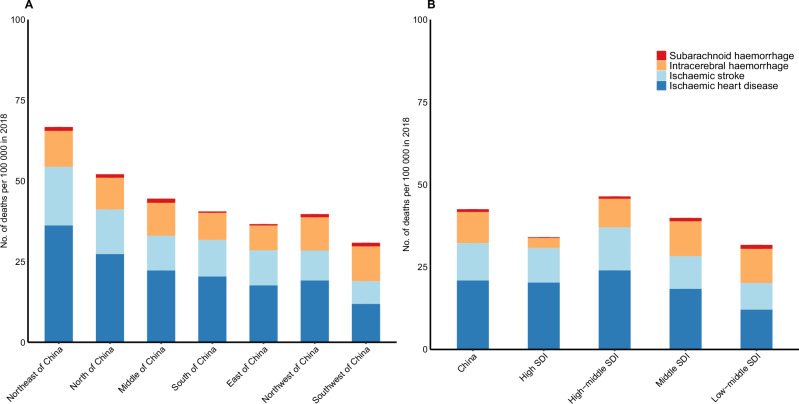
There was substantial geographical heterogeneity in the number of death and age-standardised mortality rate due to CVD and its subtypes attributable to high FPG from 2010 to 2018 (Table 2, Supplementary Tables S13–17). In 2018, the highest age-standardised mortality rate of CVD attributable to high FPG were observed in the northeastern provinces (66.87 per 100,000 people [95%UI 57.89–77.94]) (Fig. 2A). The top three provinces were Heilongjiang (75.18 per 100,000 people [95%UI 59.99–93.66]), Liaoning (62.59 per 100,000 people [95%UI 47.66–81.70]) and Jilin (61.83 per 100,000 people [95%UI 48.80–80.14]). The three provinces with the lowest age-standardised mortality rate due to CVD attributable to high FPG were Tibet (20.77 per 100,000 people [95%UI 14.76–28.63]), Zhejiang (21.78 per 100,000 people [95%UI 15.63–29.26]) and Yunnan (25.01 per 100,000 people [95%UI 19.19–32.18]) (Table 2 and Supplementary Fig S5). YLL for CVD attributable to high FPG were similar with those of deaths (Supplementary Fig S6). Additionally, the number of deaths due to FPG-related CVD progressively increased in all provinces from 2010 to 2018 (Table 2).
Fig. 2. Age-standardised CVD mortality rates attributable to high FPG in seven regions (A) and in territories with low-middle to high SDIs (B).
FPG: fasting plasma glucose; CVD: cardiovascular disease, SDI: sociodemographic index. Source data are provided as a Source Data file.
The contribution of each CVD subtypes to the total CVD burden caused by high FPG also varied considerably at the regional and provincial level (Supplementary Figs S6–S7). Ischaemic heart disease and ischaemic stroke accounted for a higher proportion of total CVD deaths in most regions, however, haemorrhagic stroke accounted for a higher proportion of total CVD deaths than ischaemic stroke in southwest of China. Of the total CVD burden attributable to high FPG, ischaemic heart disease contributed more than 30% in most provinces in 2018. By contrast, haemorrhagic stroke contributed about 64.52% of the total CVD burden attributable to high FPG in Tibet in 2018 (Supplementary Figs S7–S8). There were substantial differences in the population attributable fraction (PAF) of CVD death attributable to high FPG in 2018, ranging from Tibet (5.46% [95%UI 3.93–7.36%]) to Beijing (17.04% [95%UI 12.51–23.53%]) (Supplementary Table S9). The PAFs of CVD subtypes-related deaths attributable to high FPG in 2010 and 2018 for China and its provinces are shown in Supplementary Tables S10–S12.
From 2010 to 2018, we observed that the senior population, particularly those aged 80 and above, accounted for the majority of CVD-related deaths attributable to high FPG (Fig. 1). The oldest distribution of individuals who died of CVD caused by high FPG were observed in Shanghai, Guangdong and Jiangsu in 2018, with elderly individuals aged 80 years and older accounting for 72.11%, 50.27% and 49.25% of CVD-related deaths attributable to high FPG. Furthermore, Tibet had the steepest increase in the proportion of elderly individuals aged 80 years and older who died of CVD attributable to high FPG, accounting for only 3.70% in 2010 versus 6.45% in 2018 (Fig. 1).
The variations in CVD mortality rates attributable to high FPG among SDI regions were non-monotonic (Fig. 2B and Supplementary Table S18). In 2018, the highest age-standardised CVD mortality rate attributable to high FPG was observed in the high-middle SDI region (46.53 per 100,000 people [95%UI 42.45–51.23]), followed by the middle SDI region (39.91 per 100,000 people [95%UI 36.47–43.58]), the high SDI region (34.17 per 100,000 people [95%UI 25.74–42.80]), and the low-middle region (31.91 per 100,000 [95%UI 26.19–38.68]). Overall, the high-middle region exhibited the highest CVD mortality rate compared with those in the other SDI regions in most age groups. However, in the 30–34 age group, the CVD mortality rate was notably higher in the low-middle SDI region (2.68 per 100,000 [95%UI 1.37–4.28]) in 2018, followed by the high-middle region (2.48 per 100,000 [95%UI 1.90–3.13]) and middle SDI region (2.20 per 100,000 [95%UI 1.60–2.83]) (Supplementary Table S18).
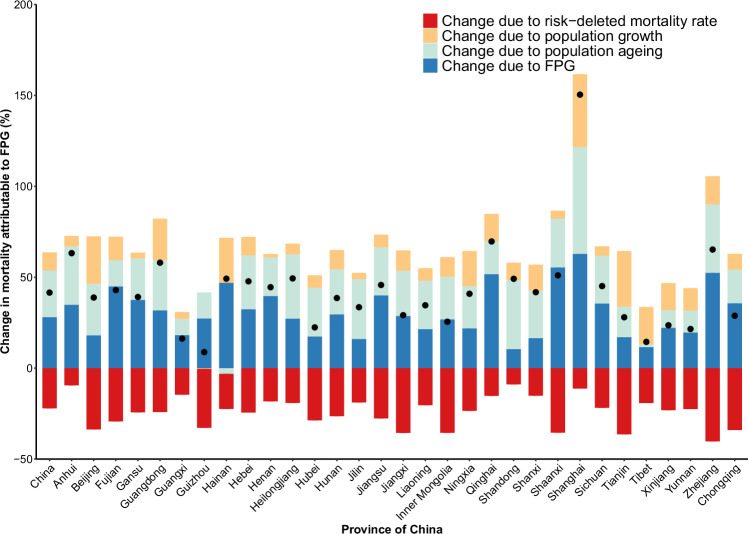
Decomposition analysis of changes in national and provincial mortality
Drivers of changes in CVD deaths attributable to high FPG varied from 2010 to 2018 (Fig. 3). Overall, changes in exposure to high FPG and population aging were the primary drivers of increases in FPG-related deaths due to CVD, which were partially offset by decrease in risk-deleted mortality rate. At provincial level, changes in exposure to high FPG led to increased FPG-related CVD deaths, with a relative contribution that spanned from Shandong (10.40%) to Shanghai (62.81%). Moreover, the impact of population aging on the FPG-related CVD deaths differed markedly by provinces from 2010 to 2018. Population aging accounted for increases in the number of death due to FPG-related CVD for most provinces, especially, Shanghai (58.64%), Shandong (37.95%), and Zhejiang (37.71%). Conversely, for Hainan, population aging contributed to decreasing levels of FPG-related CVD deaths (−3.17%) (Fig. 3).
Fig. 3. Changes in CVD deaths attributable to FPG from 2010 to 2018 by province in China, according to the contributions of population growth, population ageing, exposure to high FPG, and risk-deleted mortality rate.
Black dots indicate the total percent change. FPG: fasting plasma glucose; CVD: cardiovascular disease. Source data are provided as a Source Data file.
Discussions
In 2018, approximately 0.50 million CVD death in adults aged 25 years and older were attributable to high FPG in China, with 0.28 million occurring in men and 0.22 million in women. The CVD mortality burden attributable to high FPG had considerable variations across sex, age group and regions from 2010 to 2018 in China. The age-standardised CVD mortality rate attributable to high FPG was higher in the high-middle SDI region and northeastern China. About 13.26% of CVD-related deaths in 2018 were estimated to be attributable to high FPG. Moreover, nationally, increases in exposure to high FPG and population aging were the primary drivers of increases in FPG-related deaths due to CVD.
To our knowledge, this study is the most recent information on the burden due to CVD attributable to high FPG, based on large-scale nationally representative cross-sectional surveys, which provides comprehensive and comparable data over time in China and its provinces. The CVD burden attributable to high FPG was currently centred in the northeast of China, whereas Tibet had the lowest age-standardised CVD mortality in 2018. This variation might be partly explained by environmental and socioeconomic factors, lifestyles, dietary patterns, and genetic factors. Previous study demonstrated that the Tibetan had significant lower prevalence of diabetes than Han ethnic group3,9. Additionally, to our best knowledge, only one study deriving data from GBD 2019 have assessed the CVD burden (including ischaemic heart disease, stroke, and peripheral arterial disease) attributable to high FPG in China from 1990 to 201910, suggesting that approximately 700.34 million CVD deaths were caused by high FPG in China in 2019, respectively. We observed that the estimated burden of CVD mortality attributable to high FPG in our study was slightly lower than the findings reported in GBD 2019. However, discrepancies in the definition of CVD and the research time window between our study and GBD 2019 render direct comparison challenging, hindering the alignment of the findings on a comparable scale. Nevertheless, this study represented the latest and most comprehensive information on CVD burden attributable to high FPG. Leveraging large-scale nationally representative cross-sectional surveys, this current research established a robust foundation for the precise assessment of FPG levels, facilitating comparability across China and its provinces from 2010 to 2018. The findings offered a comprehensive depiction of CVD burden attributable to high FPG across regions, age groups, and sex, thereby contributing to systematic and reliable evidence aimed at estimating the FPG-attributable burden for CVD and its types in China and other developing countries at the transitioning stage.
We also found that high-middle SDI region, most present in northeast of China and north of China, had the heaviest CVD burden. Previous study based on the global GBD 2019 also showed that the burden of ischaemic heart disease attributable to high FPG was highest in the high-middle SDI11, which was partially consistent with our findings. It is particularly important to note that regions with high socioeconomic status have experienced a remarkable transection toward a western lifestyle over the past four decades, and have more rapid surge in metabolic disorders and related CVD burden12. However, the improvement and development of health facilities is not keeping pace with the rapid urbanization process and economic growth13. Also, covering fewer counties and district in the southwestern region in the Disease Surveillance Point system may also affect the robustness and precision of estimates of the number of deaths due to CVD. Of note, given that the limited capacity to increase spending on health and implementation of effective preventive measures in the less socioeconomic regions, they are expected to experience a large increase in the burden of diabetes and related diseases with the rapid economic growth. Thus, the resultant direct and indirect costs of diabetes and related diseases are estimated to offset some of the gains from economic growth. Additionally, CVD burden caused by high FPG in areas with high SDI has decreased compared with that in high-middle SDI regions, indicating that the burden can be reduced by further broad socioeconomic level.
The findings of this study emphasize the importance of developing population-specific tailored measures for diabetes prevention and management and provide policymakers insights in implementing clinical and public health intervention strategies and appropriate allocation of medical resources. Recent research revealed that although the overall universal health coverage (UHC) in China showed an upward trend from 2003 to 2018 and is expected to reach 80% by 2030, the process in recent years has gradually slowed down, and it is projected that 105.8 million population equivalents will still have no access to UHC by 203014. Inequality in capacity and access to health services explained an important part of the geographical disparities, suggesting that gains can be achieved by effective health promotion and reasonable health resource allocation. Cost-effective and minimal interventions are particularly important in diabetes care for some resource-constrained regions. Additionally, integrating the public health services and clinical diagnosis and treatment of primary health care institutions is crucial to periodically and timely evaluate the disease status and the effectiveness, feasibility and sustainability of alternative management strategies15,16. In line with the context of healthy China 2030 plan17, China has already proposed a range of initiatives to confront the rapid rise of the burden of non-communicable diseases, such as shifting the principle of health care from treatment first to prevention first, and prioritizing prevention and primary care18. Moreover, the Chinese Diabetes Society’s Diabetes Prevention and Management Program (Bluelight Action) from 2010 also be at play in diabetes prevention and improvement of prognosis19. Previous studies indicated that the awareness of diabetes had been improved3,20, which could be attributed to China’s continued efforts. Nonetheless, awareness, treatment and control rates for diabetes remain low, which, coupled with an increase in prevalence, indicates that the health burden of diabetes and related diseases will continue to increase in China. Thus, it is of utmost important to build a strong primary health care health system with good quality of care, which could help to blunt the transition from diabetes prevalence to premature death in some regions.
The findings also showed that population aging accounted for increases in the number of death due to FPG-related CVD for most provinces, especially in Shanghai. It’s estimated that there were approximately 260 million and 190 million residents over 60 and 65, respectively, in 2019 according to the Seventh National Population Census21, demonstrating that the burden of diabetes and its related diseases are expected to increase in China. Given that population aging is in high gear in China, government have planned to integrate the concept of healthy ageing into the processes of socio-economic development22. Therefore, it is important to shift the care model from disease-centred to people-centred and to expand access to health services, especially in field such as geriatrics and rehabilitation23, which is one of the key elements to improve the prevention and management of diabetes and its related diseases.
Moreover, we found that men had higher CVD burden attributable to high FPG than women, which can be partly explained by higher prevalence of smoking, hypertension, and dyslipidemia in men than women24. Also, previous study showed that women had higher awareness, treatment and control rate of diabetes than men, and men had stagnated rates of awareness, treatment, and control, or even declined from 2013 to 20184. Furthermore, similar to the findings of GBD 201925, we found that the sex difference in CVD mortality attributable to high FPG decreased after age 50, and even reversed after age 80. Given that the protective effect of oestrogen on CVD and metabolism may disappear after menopause, combined with a longer life expectancy, the CVD burden caused by high FPG among women could not be ignored. Thus, population-based approaches to improve the awareness of diabetes, and intervene and manage individuals at high risk for diabetes or CVD are also relevant to control the CVD burden caused by high FPG.
Several studies have documented that adiposity, the leading contributing risk factor for diabetes, has increased substantially in prevalence over the past few years in China26,27, which could contribute to the increase of CVD burden related to hyperglycaemia. Moreover, hyperglycaemia-related CVD burden may also be intensified by the large population with prediabetes, changes in dietary profile, smoking, insufficient physical activity and air pollution. Previous evidence based on clinical trials showed that lifestyle interventions can prevent or at least significantly delay diabetes in up to 50% of patients with impaired glucose tolerance28, indicating that identifying individuals with a high risk of diabetes and implementing lifestyle interventions for them is needed. Also, promoting healthy lifestyles and delivering culturally appropriate health education should be effective and cost-saving strategies to confront the ever-increasing burden caused by high FPG, especially for regions or countries with less socio-economical levels.
Limitations
The study has several limitations. First, although the relative risks (RRs) for FPG and related CVDs may differentiate across subpopulations and regions29,30, specific RRs were not available. Second, diet profiles in China, mostly characterized by carbohydrates as a staple food, which can easily lead to an increase in postprandial glucose. In this regard, the CVD burden based on FPG may underestimate the burden of individuals with postprandial hyperglycaemia. Third, some remote and economically- deprived areas lack high-quality data in the Disease Surveillance Point system, which could lead to imprecise estimation of CVD mortality estimates in some provinces. Fourth, we did not utilize all individual information from the three surveys to ascertain the optimal-fit distribution of FPG, owing to constraints in data availability.
In summary, the CVD burden attributable to high FPG varied substantially by age group, sex, and region in China from 2010 to 2018. Approximately 0.50 million CVD deaths were attributed to high FPG in 2018. Overall, changes in exposure to high FPG and population ageing were the primary drivers of increases in FPG-related deaths due to CVD. The findings of this study emphasize the importance of developing population-specific tailored measures for diabetes prevention and management and provide policymakers with evidence for implementing clinical and public health intervention strategies in China and similar countries or regions.
Methods
Ethics and inclusion statement
All data used in this study were aggregated from three previous cross-sectional surveys and did not contain any individually identifiable information. The surveys included the China Chronic Disease and Risk Factor Surveillance (CCDRFS)31, the China National Nutrition Survey (CNNS)32, and the China Hypertension Survey (CHS)33,34, and received ethical approval from the ethical review committee of the National Centre for Chronic and Noncommunicable Disease Control and Prevention, the ethical review committee of the Chinese Centre for Disease Control and Prevention, and the Ethics Committee of Fuwai Hospital, respectively. All participants obtained from these three surveys provided informed consent. Main researchers were included in the research process and are listed as authors where relevant.
Data sources
We obtained data on the fasting plasma glucose levels from three nationally representative surveys, including the CCDRFS, CNNS, and CHS, as described in the Supplementary Methods. Briefly, approximately 791,373 participants aged 25 years and older were recruited from these three national surveys. The data on FPG levels, covering 31 provinces in mainland China, were spread among the years in 2010, 2012, 2013, 2015 and 2018, and 44% of participants were men. We focused on the sex disparity in this study. Sex was used to discuss biological attribute differences throughout this paper, which was determined based on self-reporting. Additionally, data on CVD mortality from 2010 to 2018 at the provincial level were derived from the National Mortality Surveillance System (NMSS), which covers 324 million people, accounting for 24.3% of the country’s population35–37. Underreporting surveys and garbage code redistribution were conducted to ensure the accuracy of CVD mortality estimates in NMSS. More details were provided in Supplementary Methods.
Estimation of exposure to fasting plasma glucose and population attributable fraction
Based on 791,373 participants aged 25 years or older, we used a temporal-spatial hierarchical Bayesian model to comprehensively estimate mean FPG levels by age group and sex for 31 provinces in mainland China from 2010 to 2018, borrowing information across space, time, age as well as covariates for missing data38,39. Specifically, the model included terms that allowed a non-linear time trend, which was specified by a combination of a linear slope and a second order random walk. Besides, we used a cubic spline to allow non-linear age relationship. All analyses were done separately by sex. The model is described in detail in the Supplementary Methods and previous publication40.
GBD comparative risk assessment framework was used to quantify the attributable disease burden of risk factors, which was shown in detail in the Supplementary Methods. Specifically, we quantified the burden of death from CVD and its subtypes attributable to FPG, including ischaemic heart disease, ischaemic stroke, haemorrhagic stroke when there was sufficient evidence of an association according to the World Cancer Research Fund criteria and the GBD 2019 study6,41. The age-specific RRs for each risk factor-disease pair were shown in Supplementary Table S2, which were obtained from GBD 2019. In our main analysis, we estimated the PAF for the CVD by contrasting the risk of the FPG distribution with the expected risk of the theoretical-minimum-risk exposure level (TMREL). Consistent with the GBD 2019 study5, TMREL is a level of FPG that minimises risk at the population level and captures the maximum attributable burden (4.8–5.4 mmol/L). In this study, we used high FPG as a risk factor to calculate the CVD burden attributable to high FPG (only available for adults aged 25 years or older), which was also consistent with previous studies5,10. The PAF attributable to high FPG was calculated using the following formula, assuming that the distribution of the FPG was normal:
| 1 |
where is the relative risk as a function of exposure level x, CVD subtypes (o), age group (a), and sex (s). is the distribution of FPG in the age group (a), sex (s), province (p), and year (t); l is the minimum exposure level and m is the maximum exposure level.
CVD mortality burden attributable to high FPG
Findings were reported by 31 geographical units in mainland China, including 22 provinces, five autonomous regions, and four municipalities. YLLs owing to premature mortality were calculated as the death numbers multiplied by standard life expectancy at the age that death occurred1. The details about YLL computation were presented in the Supplementary Methods. Deaths and YLLs for CVD attributable to high FPG were computed by multiplying age-, sex-, province-, year-, and cause-specific PAFs by the estimated deaths and YLLs for the same strata. Age-standardised FPG level, mortality rate and YLL rate for CVD attributable to high FPG were standardised to the population in 2010 census to adjust demographic differences using direct standardization (Supplementary Table S4).
Other definitions and analytical approaches
The estimated annual percentage change (EAPC) was computed to quantify the trends of FPG-related CVD mortality burden within a specific time interval. We assumed a natural logarithm of age-standardised rates to fit a linear regression model: , where is equal to the natural logarithm of age-standardised rates, indicates a constant, is the positive or negative changing trends, year stands for the calendar year, is the error term. EAPC can be calculated based on the following equation:42 In addition, We divided 31 provinces in relation to different indicators, including socio-demographic index (SDI) and seven regions (northeast China, north China, east China, central China, south China, northwest China, and southwest China, Supplementary Table S5). SDI is a composite indicator based on total fertility rate (age <25 years), income per person, and years of educational attainment (for those aged ≥15 years) (Supplementary Table S5)5.
Additionally, we conducted decomposition analyses to quantify the drivers of change in the death numbers for CVD caused by high FPG based on methods developed by Das Gupta43. Specifically, we decomposed the change in CVD deaths caused by high FPG from 2010 to 2018 into four explanatory components: change in population growth; change in population structure by sex; change in risk exposure to FPG; and change in risk-deleted mortality rates for CVD, which correspond to the four terms shown in the below44:
| 2 |
where is the total CVD deaths attributable to FPG at year ; is the population size in the sex (s), province (p), and year (t); is the proportion of the population in the age group; is the CVD mortality rate in the absence of the FPG, which is calculated by multiplied CVD mortality rate by for a given age group (a), sex (s), province (p) and year (t); and is the ratio of attributable burden to the underlying rate defined as .
We reported the 95% uncertainty intervals (UIs) for the FPG levels and cause-specific burden estimates by running 1000 draws of each step of the estimation process from a Monte Carlo simulation approach. All analyses, unless otherwise stated, were done with SAS 9.4. The temporal-spatial hierarchical Bayesian model and graphs were done with R 4.2.0.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
This study was supported by the National High Level Hospital Clinical Research Funding (2022-GSP-GG-3, Z.W.), the National Key Research and Development Program of China (2018YFC1315303, Z.W.), China National Science & Technology Pillar Program (2011BAI11B01, Z.W.) and Project Entrusted by the National Health Commission of the People’s Republic of China (NHC2020-609, Z.W.). The funders were not involved in the collection, analysis, or interpretation of data, writing of this report, or decision to submit the article for publication. The funders played no role in determining the study design, data collection, or analysis methods employed, in our decision to publish, or in preparing the paper. The authors thank the contributions that have been made by the China Chronic Disease and Risk Factor Surveillance group, the China Nation Nutrition Survey group, the China Hypertension Survey group, and the local sites in the collaborative network in the realms of study operations. We thank the GBD 2019 for providing the relative risks of ischaemic heart disease and stroke deaths used in this study.
Author contributions
Z.W. and M.Zhou. contributed to the conceive and design of the study. X.C. conducted the data analysis and prepared the first draft. Z.Z., Z.H., R.G., X.Y., X.P., Y.F. and M.Zhang. were involved in data preparation and verification. X.C. and Y.T. performed the statistical analysis and data interpretation. Z.Z., L.W., X.W., C.Z., P.Y., Y.H., M.Zhou. and Z.W. provided important comments on the manuscript. Z.W., M.Zhou. and X.C. had full access to all the data in the study and final responsibility for the decision to submit for publication.
Peer review
Peer review information
Nature Communications thanks Theo Vos, and the other, anonymous, reviewers for their contribution to the peer review of this work. A peer review file is available.
Data availability
The “minimum dataset” that are necessary to interpret, verify and extend the research in the article, can be found within the manuscript and its supplementary information. Age-sex-specific relative risks and theoretical minimum risk exposure level were available from Global burden of disease 2019 study (10.1016/S0140-6736(20)30752-2). The original datasets generated or analysed, or both, and the raw data for fasting plasma glucose levels and CVD deaths are available under restricted access due to data privacy laws according to Chinese regulations, access can be obtained by submitting a collaboration request including information on the institution and a brief description of the project to wangzengwu@foxmail.com. An answer can be expected within 30 d. If the collaboration request is accepted, a data access agreement will be necessary and appropriate authorisations from the competent administrative authorities may be needed. In accordance with existing regulations, no personal identification data will be accessible. Source data are provided with this paper.
Code availability
The code that supports the findings of this study is available upon request (send requests to wangzengwu@foxmail.com)”.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Maigeng Zhou, Zengwu Wang.
Contributor Information
Maigeng Zhou, Email: zhoumaigeng@ncncd.chinacdc.cn.
Zengwu Wang, Email: wangzengwu@foxmail.com.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-024-53236-y.
References
- 1.Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet396, 1204–1222 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collaboration, N. C. D. R. F. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet387, 1513–1530 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li, Y. et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ369, m997 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang, L. et al. Prevalence and Treatment of Diabetes in China, 2013-2018. JAMA326, 2498–2506 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray, C. J. L. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet396, 1223–1249 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh, G. M. et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One8, e65174 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duncan, B. B. et al. The burden of diabetes and hyperglycemia in Brazil-past and present: findings from the Global Burden of Disease Study 2015. Diabetol. Metab. Syndr.9, 18 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collaborators, G. B. D. D. i. t. A. Burden of diabetes and hyperglycaemia in adults in the Americas, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Diabetes Endocrinol.10, 655–667 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang, L. et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA317, 2515–2523 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong, L. et al. Burden of cardiovascular diseases attributable to diabetes among Chinese adults from 1990 to 2019. Chin. Gen. Pract.27, 1380–1386 (2024).
- 11.Wang, W. et al. Global Burden of Disease Study 2019 suggests that metabolic risk factors are the leading drivers of the burden of ischemic heart disease. Cell Metab.33, 1943–1956.e1942 (2021). [DOI] [PubMed] [Google Scholar]
- 12.Li, Y. et al. Time trends of dietary and lifestyle factors and their potential impact on diabetes burden in China. Diabetes Care40, 1685–1694 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gong, P. et al. Urbanisation and health in China. Lancet379, 843–852 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou, Y. et al. Universal health coverage in China: a serial national cross-sectional study of surveys from 2003 to 2018. Lancet Public Health7, e1051–e1063 (2022). [DOI] [PubMed] [Google Scholar]
- 15.Li, X. et al. The primary health-care system in China. Lancet390, 2584–2594 (2017). [DOI] [PubMed] [Google Scholar]
- 16.Li, X. et al. Quality of primary health care in China: challenges and recommendations. Lancet395, 1802–1812 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CPC Central Committee and State Council. The plan for “Healthy China 2030”, https://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (2016).
- 18.Lancet Public, The H. Public health in China: achievements and future challenges. Lancet Public Health3, e456 (2018). [DOI] [PubMed] [Google Scholar]
- 19.Chan, J. C., Zhang, Y. & Ning, G. Diabetes in China: a societal solution for a personal challenge. Lancet Diabetes Endocrinol.2, 969–979 (2014). [DOI] [PubMed] [Google Scholar]
- 20.Yang, W. et al. Prevalence of diabetes among men and women in China. N. Engl. J. Med362, 1090–1101 (2010). [DOI] [PubMed] [Google Scholar]
- 21.National Bureau of Statistics of China. China Statistical Yearbook–2020. (China Statistics Press; Beijing, China, 2020).
- 22.The “14th Five-Year Plan for Healthy Aging”. http://www.gov.cn/zhengce/zhengceku/2022-03/01/content_5676342.htm. (2022).
- 23.Chen, X. et al. The path to healthy ageing in China: a Peking University-Lancet Commission. Lancet400, 1967–2006 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teufel, F. et al. Body-mass index and diabetes risk in 57 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 685 616 adults. Lancet398, 238–248 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu, Y. et al. Global disease burden of stroke attributable to high fasting plasma glucose in 204 countries and territories from 1990 to 2019: An analysis of the Global Burden of Disease Study. J. Diabetes14, 495–513 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang, L. et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet398, 53–63 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang, Y., Zhao, L., Gao, L., Pan, A. & Xue, H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol.9, 446–461 (2021). [DOI] [PubMed] [Google Scholar]
- 28.Yoon, U., Kwok, L. L. & Magkidis, A. Efficacy of lifestyle interventions in reducing diabetes incidence in patients with impaired glucose tolerance: a systematic review of randomized controlled trials. Metabolism62, 303–314 (2013). [DOI] [PubMed] [Google Scholar]
- 29.Howard, G. et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med173, 46–51 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lacey, B. et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob. Health6, e641–e649 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang, M. et al. Data Resource Profile: China Chronic Disease and Risk Factor Surveillance (CCDRFS). Int J. Epidemiol.51, e1–e8 (2021). [DOI] [PubMed] [Google Scholar]
- 32.He, Y. et al. Data Resource Profile: China National Nutrition Surveys. Int J. Epidemiol.48, 368–368f (2019). [DOI] [PubMed] [Google Scholar]
- 33.Wang, Z. et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J. Cardiol.174, 721–723 (2014). [DOI] [PubMed] [Google Scholar]
- 34.Wang, Z. et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012-2015. Circulation137, 2344–2356 (2018). [DOI] [PubMed] [Google Scholar]
- 35.Zhou, M. et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet394, 1145–1158 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qi, J. et al. National and subnational trends in cancer burden in China, 2005-20: an analysis of national mortality surveillance data. Lancet Public Health8, e943–e955 (2023). [DOI] [PubMed] [Google Scholar]
- 37.Wang, W. et al. Mortality and years of life lost of cardiovascular diseases in China, 2005-2020: Empirical evidence from national mortality surveillance system. Int J. Cardiol.340, 105–112 (2021). [DOI] [PubMed] [Google Scholar]
- 38.Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet380, 2224–2260 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finucane, M. M. et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet377, 557–567 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cao, X. et al. The burden of cardiovascular disease attributable to high systolic blood pressure across China, 2005-18: a population-based study. Lancet Public Health7, e1027–e1040 (2022). [DOI] [PubMed] [Google Scholar]
- 41.Wiseman, M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc. Nutr. Soc.67, 253–256 (2008). [DOI] [PubMed] [Google Scholar]
- 42.Hankey, B. F. et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control11, 31–35 (2000). [DOI] [PubMed] [Google Scholar]
- 43.Das Gupta P. Standardization and decomposition of rates: A user’s manual. [PubMed]
- 44.G. B. D. Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet388, 1659–1724 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The “minimum dataset” that are necessary to interpret, verify and extend the research in the article, can be found within the manuscript and its supplementary information. Age-sex-specific relative risks and theoretical minimum risk exposure level were available from Global burden of disease 2019 study (10.1016/S0140-6736(20)30752-2). The original datasets generated or analysed, or both, and the raw data for fasting plasma glucose levels and CVD deaths are available under restricted access due to data privacy laws according to Chinese regulations, access can be obtained by submitting a collaboration request including information on the institution and a brief description of the project to wangzengwu@foxmail.com. An answer can be expected within 30 d. If the collaboration request is accepted, a data access agreement will be necessary and appropriate authorisations from the competent administrative authorities may be needed. In accordance with existing regulations, no personal identification data will be accessible. Source data are provided with this paper.
The code that supports the findings of this study is available upon request (send requests to wangzengwu@foxmail.com)”.